Abstract
Background
The introduction of non-VKA oral anticoagulants (NOACs) has changed the landscape of preventing thromboembolism events in many countries. However, the prescription trends of oral anticoagulant (OAC) in China are still unclear, which were evaluated in this study through data extracted and summarized from 5 major cities as representatives.
Methods
This study was designed as a time-series study which was based on pharmacy prescription data. Analysis was performed on yearly aggregated visits and expenditure. The results were also stratified by indications and specialties.
Results
A total of 189,006 prescriptions of 67 hospitals in 6 years were included in the study. The average growth rates of overall visit and expenditure of OAC were 15.8 and 57.5%, respectively. The share of warfarin decreased and NOACs had taken 92% of cost, covering 28% of patients in 2017. The more frequently used NOACs were rivaroxaban and dabigatran. The use of OAC was differed by indication and specialty.
Conclusion
The use of NOACs was found increasing rapidly in both visits and cost, sharing a majority of cost with a minority of patients. Attentions should be paid on the rational use of NOACs.
Similar content being viewed by others
Background
Thromboembolism events associated with atrial fibrillation (AF) and venous thromboembolism are leading causes of morbidity and mortality all over the world [1, 2]. Warfarin, the primary Vitamin K antagonist (VKA) in the market, has been the unique oral anticoagulant (OAC) for stroke prevention for decades. However, the introduction of non-VKA oral anticoagulants (NOACs) has changed the landscape of preventing thromboembolism events in many countries [3,4,5,6,7]. In China, three NOACs (rivaroxaban, dabigatran and apixaban) were approved sequentially for clinical use since 2009. Considering the high price of NOACs in China, the cost-utility of NOACs should be carefully re-evaluated [8]. It can be foreseen that there is a great demand of NOACs in China due to the high burden of diseases needing anticoagulation therapy [9, 10]. However, the prescription trends of oral anticoagulant in China are still unclear, which were evaluated in this study through data extracted and summarized from 5 major cities as representatives.
Methods
Study design
This study was designed as a time-series study which was based on pharmacy prescription data and was run under the guide of the statement of Reporting of Studies Conducted using Routinely-collected Data (RECORD statement) [11].
Data collection
The prescriptions were extracted from database of Hospital Prescription Analysis Corporation Program of China [12]. The database contained participated hospitals’ prescription information of 40 random days per year. All outpatient OAC prescriptions were included from hospitals locating in 5 major regions of China (Beijing, Shanghai, Hangzhou, Guangzhou and Chengdu). These 5 cities locate in the north, east, south and west of China respectively, covering a wide area and having a total population of more than 800 million, thus the data were nationally representative. The prescriptions from hospitals which did not participate the program continuously between 2012 and 2017 were excluded. The prescription data included unique prescription code and patients’ code, sex, age, date, location and hospital code, diagnosis, drug generic name and price of drugs. Data with missing field was not included for the calculation involving the missed field.
Sample size was not estimated before data extraction. All prescriptions met the inclusion criteria were included since excessive data could be handled by software easily. It should be noted that this study included prescriptions on specific days and didn’t follow up the same patient group over the study period.
Primary measurements and data processing
Our primary analysis units were treatment visit and expenditure, and the definition of treatment visit is an ambulatory OAC prescription prescribed, no matter the prescription is the first or renewal. The total expenditure was calculated by add up all the prices of OACs together. The cost per visit was obtained by dividing total expenditure by visits. The study was limited to patients receiving warfarin and 3 NOACs (rivaroxaban, dabigatran and apixaban), aged more than 18. Analysis was performed on yearly aggregated visits and expenditure. The results were also be analyzed by indications and specialties. It should be noted that when assessing OAC use by indication, the retrieved prescriptions cannot clearly distinguish valvular and non-valvular AF.
Statistical analysis
Trends in proportions will be tested by log-linear analysis. Other trends will be analyzed by Mann-Kendall trend test. All the statistical analysis will be run in R(3.5.0).
Results
Characteristics of prescriptions
The data cleaning process was shown in Fig. 1. As shown in Table 1, a total of 189,006 prescriptions of 67 hospitals in 6 years were included in the study. In all the included prescriptions, 48.7% were of male. The age ranged from 18 to 117, with an average age of 56.
Overall trends of oral anticoagulant use and expenditure
The overall OAC use increased from 21,435 visits in 2012 to 44,653 visits in 2017, driven by an average growth rate of 15.8% per year (P < 0.05). Among all the visits, the percent of patients receiving warfarin declined from about 98% in 2012 to about 72% in 2017 (P < 0.05).
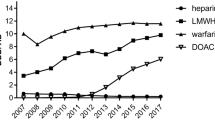
While the total expenditure of OAC seemed to increase more rapidly at an average growth rate of 57.5%. The average cost per visit of OAC kept on increasing during the study period (P < 0.05), but the average cost of warfarin remained constant (P > 0.05) and of NOACs even decreased (P < 0.05). However, the average cost of NOACs at 2017 was about 30 times than the cost of warfarin (Fig. 2). While the percent of cost of warfarin declined with a bigger extent. Warfarin had taken a share of cost at 8% in 2017 and NOACs had taken 92% of cost, covering 28% of patients. The more frequently used NOACs were rivaroxaban and dabigatran, while apixaban took a minimal share of NOACs.
The overall trends of ambulatory anticoagulant use and expenditure in 67 hospitals from 5 cities of China. a: Trends of yearly total visits; b: Trends of yearly total cost; c: Trends of average cost per visit of warfarin, NOACs and OAC; d: Trends of percentage of visits taking different OAC; e: Trends of percentage of cost taking different OAC
OAC use by indication
Four diseases, AF, pneumonia embolism (PE), deep vein thromboembolism (DVT) and joint replacement, which need anticoagulation therapy were selected and analyzed for OAC use (Fig. 3). For AF and PE, the most prescribed OAC was warfarin. The visits of AF patients receiving warfarin kept increasing, while which of PE remained constant in the recent years. For patients with DVT, the use of rivaroxaban increased rapidly, and the visits of rivaroxaban user exceed warfarin in 2017. For joint replacement patients, the use of rivaroxaban was close to warfarin at the beginning of study duration and then became the major used OAC at the end of the study gradually. Rivaroxaban was the most frequently prescribed NOAC except in AF patients. Apixaban was rarely prescribed.
OAC use by specialty
The use of OAC was stratified by specialties (Fig. 4). The orthopedists seemed to embrace NOACs in the first place by whom rivaroxaban was the most frequently prescribed, and the use of apixaban increased but also took a minor portion. Cardiothoracic surgeons remained using warfarin as a major option during the 6 years and the portion of NOACs was small. Warfarin used by cardiologists and neurologists decreased but still took the major proportion. The use of rivaroxaban and dabigatran were increasing rapidly in the recent years, and dabigatran was more than rivaroxaban.
Discussion
The trends of OAC used by patients in 5 major cities of China were investigated through pharmacy prescription data in this study. It could be found that the number of patients receiving OAC and the total cost of OAC both increased rapidly. The percentage of patients who receiving warfarin kept on decreasing, but warfarin was still the most frequently prescribed OAC. Although NOACs took a minor portion in patient number, it became the major component of OAC cost.
The trends of OAC use in China, decreased warfarin and increased NOACs, was similar to other countries. According to the experience of these countries, the use of NOACs will still increase in next several years. For patients who are not able to monitor international normalized ratio (INR) frequently or reach a stable INR, it would be beneficial to switch warfarin to NOACs [13]. However, switching from warfarin to NOACs may bring no benefit to patients who had stable anticoagulation [14]. Holding a small number of patients, NOACs have revealed a higher average cost per patient and occupied a larger part of total cost in OAC nowadays. The average cost of NOAC declined during the study period, that may due to the increased use of a cheaper NOAC, dabigatran. However, the prices of NOAC were much higher than that of warfarin. The increasing use of NOACs had elevated the average cost of OAC. It will exert more pressure on both patients and health insurance system, therefore NOACs should be used after balancing the benefit, risk and cost carefully [15].
As the first NOAC applied to AF patients, rivaroxaban was the most popular at one time, however, rivaroxaban’s market share had been surpassed by dabigatran in recent years. This may due to the accumulated clinical evidences, which showing the priority of dabigatran over rivaroxaban in AF patients [16,17,18]. By contrast, rivaroxaban strengthened the market in joint replacement patients. It was the first NOAC approved for thromboprophylaxis in patients undergoing joint replacement surgery and was recommended by guidelines [19]. The use of apixaban was rare in China. Orthopedists had rich experience in rivaroxaban and would not switch to apixaban without clinical evidence of superiority. Higher price and more frequent dosing were both apixaban’s shortages [20]. More unfortunately, apixaban has not been approved for AF by Chinese government yet.
The choice of OAC differed among specialists. Orthopedists were the first and most widely embracing group of NOACs which may due to the early approval for orthopedic indication and less NOACs contraindication in these patients. NOACs were only suitable for non-valvular AF patients, thus the cardiothoracic surgeons had the lowest rate of NOAC use.
There are still some limitations of this study. The prescription data didn’t provide the outcomes of anticoagulation therapy. Patients who need but have not received OAC can not be included. The source data were from hospitals which participated in the program and sampling bias may exist. The cost for warfarin only includes the drug cost. Additional cost for taking warfarin, such as monitoring of INR, was not included.
Conclusion
The use of NOACs was found increasing rapidly in both visits and cost, sharing a majority of cost with a minority of patients. Patients and health insurance system have to face the rapid growth of anticoagulation expenditure. Cost-utility study of NOACs is needed for drug provider, consumer and policy maker. Attentions should be paid on the rational use of NOACs for no benefit of switching to NOACs in warfarin stable anticoagulation patients.
Availability of data and materials
The datasets analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- AF:
-
Atrial fibrillation
- DVT:
-
Deep vein thromboembolism
- NOAC:
-
Non-Vitamin K oral anticoagulant
- OAC:
-
Oral anticoagulant
- PE:
-
Pneumonia embolism
References
Chugh SS, Havmoeller R, Narayanan K, Singh D, Rienstra M, Benjamin EJ, et al. Worldwide epidemiology of atrial fibrillation. Circulation. 2014;129:837–47.
Morillo R, Jiménez D, Aibar MÁ, Mastroiacovo D, Wells PS, Sampériz Á, et al. DVT management and outcome trends, 2001 to 2014. Chest. 2016;150:374–83.
Kirley K, Qato DM, Kornfield R, Stafford RS, Caleb AG. National trends in oral anticoagulant use in the United States, 2007 to 2011. Circ Cardiovasc Qual Outcomes. 2012;5:615–21.
Barnes GD, Lucas E, Alexander GC, Goldberger ZD. National trends in ambulatory oral anticoagulant use. Am J Med. 2015;128:1300–5.
Weitz JI, Semchuk W, Turpie AGG, Fisher WD, Kong C, Ciaccia A, et al. Trends in prescribing Oral anticoagulants in Canada, 2008-2014. Clin Ther. 2015;37:2506–14.
Staerk L, Fosbøl EL, Gadsbøll K, Sindet-Pedersen C, Pallisgaard JL, Lamberts M, et al. Non-vitamin K antagonist oral anticoagulation usage according to age among patients with atrial fibrillation: temporal trends 2011-2015 in Denmark. Sci Rep. 2016;6:31447.
Elewa H, Alhaddad A, Al-Rawi S, Nounou A, Mahmoud H, Singh R. Trends in oral anticoagulant use in Qatar: a 5-year experience. J Thromb Thrombolysis. 2017;43:411–6.
Kumana CR, Cheung BMY, Siu DCW, Tse HF, Lauder IJ. Non-vitamin K Oral anticoagulants versus warfarin for patients with atrial fibrillation: absolute benefit and harm assessments yield novel insights. Cardiovasc Ther. 2016;34:100–6.
Luo Q, Xie J, Han Q, Tang C, Chen X, Wu L, et al. Prevalence of venous thromboembolic events and diagnostic performance of the wells score and revised Geneva scores for pulmonary embolism in patients with interstitial lung disease: a prospective study. Hear Lung Circ. 2014;23:778–85.
Guo Y, Tian Y, Wang H, Si Q, Wang Y, Lip GYH. Prevalence, incidence, and lifetime risk of atrial fibrillation in China: new insights into the global burden of atrial fibrillation. Chest. 2015;147:109–19.
Benchimol EI, Smeeth L, Guttmann A, Harron K, Moher D, Petersen I, et al. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) Statement. PLoS Med. 2015;12:e1001885.
Han G, Yu Z, Ma K. Current status of parenteral nutrition and enteral nutrition application: an assessment of nutritional prescriptions from 59 hospitals in the People’s republic of China. Ther Clin Risk Manag. 2015;11:201–7.
Amin A, Deitelzweig S, Jing Y, Makenbaeva D, Wiederkehr D, Lin J, et al. Estimation of the impact of warfarin’s time-in-therapeutic range on stroke and major bleeding rates and its influence on the medical cost avoidance associated with novel oral anticoagulant use-learnings from ARISTOTLE, ROCKET-AF, and RE-LY trials. J Thromb Thrombolysis. 2014;38:150–9.
Verdecchia P, Angeli F, Aita A, Bartolini C, Reboldi G. Why switch from warfarin to NOACs? Intern Emerg Med. 2016;11:289–93.
Wang Y, Bajorek B. New oral anticoagulants in practice: pharmacological and practical considerations. Am J Cardiovasc Drugs. 2014;14:175–89.
Bai Y, Deng H, Shantsila A, Lip GYH. Rivaroxaban versus Dabigatran or warfarin in real-world studies of stroke prevention in atrial fibrillation: systematic review and meta-analysis. Stroke. 2017;48:970–6.
Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361:1139–51.
Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, Hacke W, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365:883–91.
Falck-Ytter Y, Francis CW, Johanson NA, Curley C, Dahl OE, Schulman S, et al. Prevention of VTE in orthopedic surgery patients: Antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012;141:e278s–325s.
Yan X, Gu X, Xu Z, Lin H, Wu B. Cost-effectiveness of different strategies for the prevention of venous thromboembolism after Total hip replacement in China. Adv Ther. 2017;34:466–80.
Acknowledgements
The authors would thank Hospital Prescription Analysis Corporation Program of China for collecting and providing the data.
Funding
This work was funded by Zhejiang Traditional Medicine Administration, China (2016ZQ027). The funder played no role in the study.
Author information
Authors and Affiliations
Contributions
Conceptualization, Z.Y.; methodology, Z.Y.; validation, L.Y., C.S. and Y.Z.; formal analysis, Z.Y., L.Y. and C.S.; investigation, L.Y. and C.S.; resources, Z.Y.; data curation, Z.Y.; writing—original draft preparation, L.Y. and C.S.; writing—review and editing, Z.Y.; visualization, L.Y. and C.S.. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The board of Ethic Committee of Sir Run Run Shaw Hospital, College of Medicine, Zhejiang University had reviewed the study protocol and confirmed that formal ethic approval was not required because this study only involved prescription data from a database. Informed consent was also waived by the ethic committee (Reference number: KEYAN20190628–23). Permission was obtained to access the database and the data used was de-identified upon data collection.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yu, Z., Yu, L. & Shan, C. Trends of ambulatory oral anticoagulant prescription in five major cities of China, 2012–2017. BMC Health Serv Res 20, 209 (2020). https://doi.org/10.1186/s12913-020-5072-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-020-5072-3