Abstract
Background
Multiple Sclerosis (MS) is a chronic inflammatory, demyelinating and neurodegenerative disease that in many cases produces disability, having a high impact in patients’ lives, reducing significantly their quality of life. The aim of this study was to agree on a set of proposals to improve the current management of MS within the Spanish National Health System (SNHS) and apply the Social Return on Investment (SROI) method to measure the potential social impact these proposals would create.
Methods
A Multidisciplinary Working Team of nine experts, with representation from the main stakeholders regarding MS, was set up to agree on a set of proposals to improve the management of MS. A forecast SROI analysis was carried out, with a one-year timeframe. Data sources included an expert consultation, a narrative literature review and a survey to 532 MS patients. We estimated the required investment of a hypothetical implementation, as well as the potential social value that it could create. We calculated outcomes in monetary units and we measured intangible outcomes through financial proxies.
Results
The proposed ideal approach revealed that there are still unmet needs related to MS that can be addressed within the SNHS. Investment would amount to 148 million € and social return to 272 million €, so each euro invested could yield almost €2 of social return.
Conclusions
This study could guide health interventions, resulting in money savings for the SNHS and increases in patients’ quality of life.
Similar content being viewed by others
Background
Multiple sclerosis (MS) is the most disabling neurological disease in young adults, which causes significant limitations in patients’ personal, family, social, and work life [1,2,3].
The prevalence of MS in Spain has increased in recent decades from 53 patients per 100,000 inhabitants in 1994 [4], to 125 cases per 100,000 inhabitants in 2008 [5]. At present, the European Multiple Sclerosis Platform estimates that there are approximately 47,000 adult patients in Spain [6]. In parallel, an increase in incidence has been detected, with an annual average per 100,000 inhabitants of 5.3 cases between 1998 and 2003 [7], and 5.8 cases between 2008 and 2014 [8].
As with other chronic diseases, patients with MS have a high incidence of co-morbidities [9, 10], that can affect the illness by delaying diagnosis, accelerating disability, worsening quality of life, and increasing mortality [11,12,13,14]. Spanish patients with MS have an average of 5.0 ± 3.0 co-morbidities, the most frequent being depression (32.4%) and metabolic diseases such as dyslipidemia (31.1%), arterial hypertension (23.0%), obesity (22.5%), and diabetes mellitus (7.7%). In addition, 9% have chronic obstructive pulmonary disease, and 6.3% have asthma [15].
The disability derived from these factors contributes to the deterioration of health-related quality of life (HRQoL) of patients with MS [16, 17]. In 2017, Spanish patients, via the EuroQol-5 Dimensions (EQ-5D) questionnaire, reported pain and discomfort (63%), problems in carrying out daily activities (62%), anxiety / depression (55%), mobility difficulties (54%), and self-care problems (26%) [18]. Only 45% of patients with MS of working age were employed or self-employed and, among those employed, 72% felt that MS affected their productivity, mainly due to fatigue (64%), difficulty thinking (29%), moodiness (27%), mobility (25%), and pain (20%) [18].
MS also impacts the HRQoL of their informal caregivers: 20.6% have symptoms of depression, 10.6% perceive their family as dysfunctional, and 9.4% receive little social support [19]. Likewise, patient’s progressive increase in cognitive deficit causes a higher incidence of depressive symptoms in caregivers, further contributing to the deterioration of the family environment [20].
The healthcare needs of patients with MS depend on the symptoms, the degree of disability, and the existence of co-morbidities [1, 10]. Since it is a chronic disorder, care must include patients as well as their relatives and caregivers [21].
The early diagnosis of MS has been identified as one of the main needs: in Spain, the average onset age of the first symptoms is 31.4 years, while the average age at the time of diagnosis is 33.6 years [8]. Accordingly, a diagnostic delay of more than 2 years is estimated [8, 22]. Furthermore, the twenty-first Century Steering Group, comprising patients and healthcare professionals, detected unmet MS health needs regarding symptom management, treatment access, patient access to information, and communication between patients and health professionals [23].
The Social Return on Investment (SROI) method, developed in 1996 by the Roberts Enterprise Development Fund, aimed to account for the social value of interventions, offering a framework to measure returns that do not have a market value but possess an intrinsic value (e.g. emotional well-being of patients or satisfaction with the healthcare system) [24, 25]. The current SROI method further includes principles and processes typically used in evaluations of economic and financial return on investment [26]. The SROI method has not been applied to the management of MS previously, however, the methodology has been used in the area of neurology [27, 28], as well as other areas such as dermatology, cardiology, rheumatology, and oncology within the SNHS [29,30,31,32,33], and other health-related areas in other countries (nephrology [34], old age [35, 36], or maternity [37, 38], among others [39, 40]).
Thus, the objective of this study was twofold: first, to agree on a set of proposals that contribute to the ideal approach to MS in the Spanish National Health System (SNHS) and, secondly, to analyse the potential social value that would be created after its implementation.
Methods
The project was developed according to the following phases (Fig. 1):
-
Phase 1 (initial): description of the current approach to MS in the SNHS, as well as the affectation suffered by MS patients as a starting point for the study to be performed.
-
Phase 2 (first objective, ideal approach): definition of proposals contributing to the ideal approach to MS in the SNHS.
-
Phase 3 (second objective, social return on investment [SROI] analysis): analysis of the SROI of the hypothetical implementation of the previous proposals, based on the principles and stages proposed by the SROI guide [41].
The following data sources, which were developed by the authors for the purposes of this study, were used:
-
1.
Narrative literature review.
Scientific articles, official data and, to a lesser extent, grey literature (mainly news and websites regarding MS) was reviewed.
The review helped establish the current approach to MS in the initial phase of the Project and provided information for the analysis phase.
-
2.
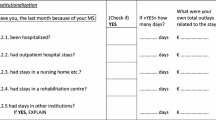
Survey of patients with MS.
A survey was conducted on 532 adult patients with MS living in Spain, through an on-line electronic questionnaire, between June and July 2017. An English translation of the questionnaire can be found in the Additional file 1.
The results provided information about the needs and HRQoL of patients with MS in the initial phase of the Project, as well as quantitative information for the analysis phase to carry out calculations.
-
3.
Expert consultation.
A Multidisciplinary Working Team (MWT) of 9 experts was set up, with representation from the main stakeholders regarding MS: 2 from neurology, 1 from primary care medicine, 1 from specialist nursing, 1 from hospital pharmacy, 1 from physiotherapy, 1 from social work, 1 from association of patients, and 1 patient with MS.
Three of the nine experts participated as an Advisory Committee in establishing the current approach to MS (starting point), and together with the rest of the experts, agreed on a set of proposals aimed at achieving the ideal approach to MS (first objective). Subsequently, the MWT assessed the impact of each proposal on each life areas of the MS patient, which helped establish the potential returns of each proposal.
In order to identify an ideal approach to the management of MS, an 8-h meeting with the MWT was held. In this meeting, three work subgroups were organised according to the individual perspective of the experts: medicine (neurology and primary care), other health professionals (specialist nursing, hospital pharmacy and physiotherapy) and patients (social work, patients association, and patient).
Each group had a predetermined time to internally discuss the most relevant proposals for the ideal approach to MS. Thereafter, proposals were shared with the rest of the groups via a spokesperson. The proposals were discussed and collected around three categories that were previously established by the Advisory Committee: diagnosis, relapsing-remitting MS, and progressive forms of MS (which encompass primarily progressive MS and secondarily progressive MS).
Next, the MWT was asked to rate the proposals individually according to the importance they considered each proposal to have for an ideal approach to MS, on a scale from 0 (“not important”) to 10 (“maximum importance”). Finally, based on the basic principle of the economy of resource scarcity, the 6 proposals with the highest average score in each area were selected.
Regarding the second objective, the forecast type SROI method was applied, with a one-year timeframe. In order to determine investment, the SNHS perspective was used, while impact was determined from a social perspective. The analysis combined both qualitative and quantitative methodologies, as dictated by the SROI guide [41].
The qualitative analysis implied understanding how the set of proposals put forward by the MWT would create social value after its hypothetical implementation, that is, the process by which each investment would generate a return, which is called the Theory of Change according to the SROI method [41].
The identification of these processes was based, first, on the opinion of the MWT that assessed the importance of each proposal in various areas of the patient’s life and, in turn, on the literature review.
The quantitative analysis focused on the process of calculating investment, return, and impact. In order to calculate the investment, the activities necessary to implement each proposal, the necessary resources, and the cost associated with those resources were first identified. Thereafter, these resources were multiplied by their unit prices. Resources, be they medical or non-medical, material or human, were quantified (in number and cost) from the literature review, official data, public prices of health services of each of the Spanish autonomous regions, and market prices. No financial value was given to the time considered for patients and their caregivers, since they are the main beneficiaries of the project, following the current SROI methodology convention [41].
Return was calculated by identifying the potential consequences of each proposal in clinical, welfare, economic, and social terms. Returns, be they tangible or intangible, positive or negative, were identified from the expert opinion of the MWT, and from the literature review, official data, public prices of health services of each of the Spanish autonomous regions and market prices. The increase or decrease in the burden of care that informal caregivers would assume was quantified using the substitution cost method, which consists of allocating the cost of hiring a professional caregiver for the time spent for informal care. Moreover, losses or gains in labour productivity were measured using the human capital method, assigning the average wage cost lost/earned as a consequence of the proposal. The intangible returns (those that do not have a market price) were quantified by assigning financial proxies such as revealed preferences (for example, the proxy of being well informed could be equivalent to the fee paid by the partners of an association of patients) or declared preferences (for example, the willingness to pay to improve their emotional state declared by patients with MS in the survey).
To adjust the total impact of the return, the deadweight (percentage of the return that would have been obtained without the proposal), the attribution (percentage of the return resulting from other activities independent from the proposal), the displacement (percentage of the return that would have displaced another return), and the drop-off (percentage of return deterioration over time)Footnote 1were deducted. Information on adjustment factors was obtained from literature review, survey to MS patients, and expert opinion.
Prices were updated to euros from 2017 according to the corresponding Consumer Price Index [42]. Regarding missing data, some assumptions based on expert opinion and literature were made, such as the average number of extra medical visits required, the average needed time for every medical visit, or the number of neurologists to be trained in specialized MS units, among others.
All calculations were based on the prevalence reported by the MS Barometer 2015 [6], updated to the population figures of 2017 (47,084 patients with MS in Spain) and an incidence of 2701 patients according to published data [8]. We assumed the entire population of MS patients would adhere to the set of proposals. Spain is geographically divided into 17 autonomous communities with decentralized management of health services, hence some proposals here presented may already have been implemented in some regional health services, but not in others.
The SROI ratio was calculated by dividing the total estimated impact by the estimated necessary investment, and so the analysis can be summarised in one sentence: “for each euro invested, a social return of X euros would be obtained”. Any ratio greater than 1 is positive.
Figure 2 explains the process of calculating the investment, the return, the impact and the SROI ratio.
Finally, a sensitivity analysis was carried out, by varying the variables that included some type of assumption (Table 1). Thus, two alternative scenarios (best and worst) were considered as the reference case, following expert opinion.
Due to the type of study, no clinical research ethical committee approval was required.
Results
Consensus for an ideal approach to MS
A total of 18 proposals were obtained to contribute to an ideal approach to MS within the SNHS (Table 2).
The main returns derived from the implementation of the diagnostic area proposals would be to avoid diagnostic errors, reduce the time of diagnosis, delay the evolution of the disability, improve the degree of knowledge of the patient about the disease, and reduce the emotional burden of the patient.
Regarding the area of relapsing-remitting MS, the main returns would be to avoid unnecessary visits to the neurology department, reduce relapses or outbreaks, improve treatment adherence, reduce disease progression, and improve emotional status, autonomy, quality of life, and the self-care of patients.
Finally, the proposals of the area of the progressive forms of MS would help avoid unnecessary neurology department visits, improve labour protection linked to MS, reduce outbreaks and costs per patient thanks to early treatment, and improve the quality of life, motor status, fatigue, family relationships, and the emotional state of patients.
From a global point of view, the improvement of the quality of life of the patient and the efficient use of health resources would imply that the patient did not have to lose hours of work for medical assistance and that the burden for informal caregivers would decrease. However, the proposals that involve completing more visits or medical tests would mean an increase in labour productivity losses, as well as in the care burden of their informal caregivers.
Table 3 shows the main stakeholders of each proposal, the objective sought, and the associated returns.
Impact of the proposals for the ideal approach to MS
The total amount of resources invested by all the stakeholders in the set of proposals for the ideal approach to MS would amount to 148.35 million euros. Most of the investment would focus on the areas of the progressive forms of MS (52.4%) and relapsing-remitting MS (43.3%), followed by the diagnostic area (4.3%).
The total social value that would be generated after the implementation of this set of proposals would amount to 271.94 million euros: 53.3% in the area of relapsing-remitting MS, 41.1% in the area of the progressive forms of MS, and 5.6% in the area of diagnosis.
This implies that for every euro invested in the set of proposals included in the Project, 1.83 euros of social value would be generated. Of these, 74.2% would correspond to tangible returns, while 25.8% would be intangible and would include aspects such as the subjective experience of the patient to avoid an outbreak, the improvement of their emotional well-being or the burden of informal care. Figure 3. shows the social value that would be created by each area analysed while distinguishing the type of return.
The sensitivity analysis revealed that, under the assumptions considered, the potential social value would range from 1.59 euros to 2.15 euros for each euro invested (Table 4).
Figure 4 shows the ratio variation according to each variable included in the sensitivity analysis.
SROI ratio according to the variation of each variable included in the sensitivity analysis. Notes: Assumption 1. Percentage of disability reduction from moderate to mild in the incident patients, consequence of the reduction in the time to diagnosis; Assumption 2 Percentage of disability reduction from severe to moderate in the incident patients, consequence of the reduction in the time to diagnosis; Assumption 3 Percentage of cross-consultations avoided in neurology after direct consultation between Primary Care and Specialised Care professionals; Assumption 4. Percentage reduction of informal care hours, as a result of a better follow-up of patients and the slowing down of the progression of their illness; Assumption 5. Decrease in the percentage of patients who do not work because of MS; Assumption 6. Percentage of untreated SPMS patients, who could be treated
Discussion
This study presents a set of proposals for improving the MS approach in the SNHS, as well as the evaluation of the potential social value that they would generate after its implementation.
Some of the proposals presented here had been previously collected, based on the chronic and complex nature of patients with MS and the specialised and continuous care they require [43, 44]. The first strength of the study would therefore be the confirmation of the needs already detected, based on the MWT consensus. However, in Spain, autonomous regions have autonomy in health management, so there may be different realities with regard to MS care [45]. Addressing these differences is a challenge to achieve equality in access to healthcare and ensure good health for the entire population and for patients with MS in particular. In this regard, the National Institute for Health and Care Excellence (NICE) in the United Kingdom proposes to evaluate health interventions from a dual approach of efficiency and equality that aims to ensure that all relevant benefits are taken into account (medical and non-medical and community), to help local authorities (and other organisations interested in improving the health of people) to better judge whether a public health intervention represents good value for money [46]. In addition, the inclusion of the perspective of patients within the MWT provides added value to the proposed set of measures and legitimises their implementation [47].
The results of the present study showed that a social value would be generated for patients with MS primarily, but also for their informal caregivers and the SNHS itself. In addition, said social value would be, in economic terms, almost twice the investment required for its implementation, with a ratio of 1:1.83 euros. However, we must keep in mind that this ratio is an abbreviated form of expressing all the potential social value. Hence, it is advisable to present it along with the rest of the information, mainly the theory of change [41].
Another strength of this study is the use of a mixed methodology, which includes both qualitative and quantitative analyses. The former refers to the theory of change, which explains and documents how an investment results in a certain impact. The latter is the process of quantitative analysis of investment and impact, which accounts for a broader concept of value that includes intangible aspects. In this phase, although it is impossible to maintain total objectivity, the provisions of the SROI guide were accurately and transparently followed [41].
The SROI method has hardly been used to evaluate different interventions in the area of public health, and never in relation to MS [37, 39, 40, 48, 49]. The challenge is not only to assess the current situation and create value around the management of patients with MS, but also to reflect on how decision making is performed in the SNHS and how the challenge of sustainability and efficiency is faced, since cutting back on health benefits represents a false economy [40].
This method poses the need to face the complexity of health care through knowledge. The traditional economic evaluation is based fundamentally on financial measurements that leave out a type of value that cannot be measured in this way. The SROI method focuses more on social value or impact than on expenditure, showing a broader type of value, and supports the collating of more comprehensive information on any intervention. The SROI method is not a substitute for other types of economic evaluation but potentially offers a more complete picture of outcomes which may support healthcare-related decision making.
This study is not without its limitations. First, there is no standardisation for the measurement of the social value inherent to health interventions. Second, in order to measure a broader concept of value, financial proxies were used to monetise that which does not have a market price. In this process, the subjective component is inevitable since two different experts could yield different results. Third, as it is a forecast study, its calculations, despite being referenced, are based on hypothetical scenarios. Therefore, the challenge remains to evaluate the real impact of these proposals once they are implemented and analyse the possible differences between both analyses. Fourth, having adopted a one-year timeframe may have biased the overview of the long-term impact of proposals. Since a forecast study implies unavoidable imprecision in data (estimated investment and return), having chosen a broader timeframe would have implied a higher imprecision. Finally, we assumed the entire population of MS patients would adhere to the set of proposals, but the whole adherence may be compromised due to proposals that demand time and effort from patients and caregivers (such as extra medical visits or tests). This might result in a lower SROI ratio which is hard to calculate as further studies about adherence to plans, in addition to treatments, are needed.
Conclusions
The results of the present study show how patients with MS could improve their HRQoL while the SNHS could improve the efficiency of its health interventions. On the other hand, the proposals raised here could also generate impact outside the scope of MS and benefit, for example, patients with other illnesses, or health professionals. Although these impacts have not been quantified due to the magnitude of the study, the potential social value could be even greater.
Availability of data and materials
The datasets used and/or analysed during the current study, and data associated to the narrative review and patient survey are available from the corresponding author on reasonable request.
Notes
The drop-off applies only to SROI analysis with a timeframe of more than 1 year.
Ley 14/2007, de 3 de julio, de Investigación biomédica. Boletín Oficial del Estado. Madrid, 4 de julio de 2007, núm. 159, pp. 28826–28,848.
Ley 41/2002, de 14 de noviembre, básica reguladora de la autonomía del paciente y de derechos y obligaciones en materia de información y documentación clínica. Boletín Oficial del Estado. Madrid, 15 de noviembre de 2002, núm. 274, pp. 40126–40,132.
Abbreviations
- CSUR:
-
Reference Centres, Services and Units
- EQ-5D:
-
EuroQol-5 Dimensions
- HRQoL:
-
Health-related quality of life
- MRI:
-
Magnetic resonance imaging
- MS:
-
Multiple sclerosis
- MWT:
-
Multidisciplinary Working Group
- NICE:
-
National Institute for Health and Care Excellence
- PC:
-
Primary care
- PCM:
-
Medicine / Primary care physician
- PFMS:
-
Progressive forms of MS
- PPMS:
-
Primarily progressive MS
- RRMS:
-
Relapsing-relapsing MS
- SC:
-
Specialised care
- SNHS:
-
Spanish National Health System
- SPMS:
-
Secondary Progressive MS
- SROI:
-
Social return on investment
References
Ministerio de Sanidad, Servicios Sociales e Igualdad. Estrategia en Enfermedades Neurodegenerativas del Sistema Nacional de Salud. Madrid: Ministerio de Sanidad, Servicios Sociales e Igualdad; 2016. http://www.mscbs.gob.es/organizacion/sns/planCalidadSNS/pdf/Est_Neurodegenerativas_APROBADA_C_INTERTERRITORIAL.pdf. Accessed 24 Aug 2017.
Déniz Cáceres A, Saavedra P, Marrero I. Predicción del grado de minusvalía en pacientes con esclerosis múltiple. Rehabilitación. 2011;45:301–7.
Servicio Canario de Salud. Guía de actuación en pacientes con esclerosis múltiple. In: Gobierno de Canarias; 2016. http://www3.gobiernodecanarias.org/sanidad/scs/contenidoGenerico.jsp?idDocument=aeab11ca-a4c8-11e6-acfb-b7af34d5e321&idCarpeta=a91550f4-75d0-11e2-bc0c-6512fc1bab5e. Accessed 24 Jan 2018.
Fernández O, Luque G, San Román C, Bravo M, Dean G. The prevalence of multiple sclerosis in the Sanitary District of Vélez-Málaga, southern Spain. Neurology. 1994;44(3 Pt 1):425–9.
Fernández O, Fernández V, Guerrero M, León A, López-Madrona JC, Alonso A, et al. Multiple sclerosis prevalence in Malaga, southern Spain estimated by the capture-recapture method. Mult Scler J Lond. 2012;18:372–6.
European Multiple Sclerosis Platform. MS Barometer 2015. In: Raising the voice of people with MS; 2015. http://www.emsp.org/wp-content/uploads/2017/02/BAROMETER-2015-Final-10.05.2017.pdf. Accessed 31 Jul 2017.
Ares B, Prieto JM, Lema M, Dapena D, Arias M, Noya M. Prevalence of multiple sclerosis in Santiago de Compostela (Galicia, Spain). Mult Scler Clin Lab Res Lond. 2007;13:262–4.
Carreón-Guarnizo E, Andreu-Reinón ME, Cerdán-Sánchez MC, Carrasco-Torres R, Hernández-Clares R, Prieto-Valiente L, et al. Prevalencia de la esclerosis múltiple en la Región de Murcia. Rev Neurol. 2016;62:396–402.
Marrie RA, Cohen J, Stuve O, Trojano M, Sørensen PS, Reingold S, et al. A systematic review of the incidence and prevalence of comorbidity in multiple sclerosis: overview. Mult Scler Houndmills Basingstoke Engl. 2015;21:263–81.
Marrie RA. Comorbidity in multiple sclerosis: implications for patient care. Nat Rev Neurol. 2017;13:375.
Marck CH, Neate SL, Taylor KL, Weiland TJ, Jelinek GA. Prevalence of comorbidities, Overweight and Obesity in an International Sample of People with Multiple Sclerosis and Associations with Modifiable Lifestyle Factors. PLoS One. 2016;11:e0148573.
Marrie RA, Elliott L, Marriott J, Cossoy M, Blanchard J, Leung S, et al. Effect of comorbidity on mortality in multiple sclerosis. Neurology. 2015;85:240–7.
Thormann A, Sørensen PS, Koch-Henriksen N, Laursen B, Magyari M. Comorbidity in multiple sclerosis is associated with diagnostic delays and increased mortality. Neurology. 2017;89:1668–75.
Marrie RA, Horwitz R, Cutter G, Tyry T, Campagnolo D, Vollmer T. Comorbidity delays diagnosis and increases disability at diagnosis in MS. Neurology. 2009;72:117–24.
Sicras-Mainar A, Ruíz-Beato E, Navarro-Artieda R, Maurino J. Comorbidity and metabolic syndrome in patients with multiple sclerosis from Asturias and Catalonia, Spain. BMC Neurol. 2017;17:134.
Jones E, Pike J, Marshall T, Ye X. Quantifying the relationship between increased disability and health care resource utilization, quality of life, work productivity, health care costs in patients with multiple sclerosis in the US. BMC Health Serv Res. 2016;16:294.
Kobelt G, Thompson A, Berg J, Gannedahl M, Eriksson J, Group MS, et al. New insights into the burden and costs of multiple sclerosis in Europe. Mult Scler J. 2017;23:1123–36.
Oreja-Guevara C, Kobelt G, Berg J, Capsa D, Eriksson J, Platform EMS. New insights into the burden and costs of multiple sclerosis in Europe: results for Spain. Mult Scler J. 2017;23(Suppl 2):166–78.
Meca-Lallana J, Mendibe M, Hernández-Clares R, Caminero AB, Mallada-Frechin J, Dávila-Gonzalez P, et al. Predictors of burden and depression among caregivers of relapsing-remitting MS patients in Spain: MS feeling study. Neurodegener Dis Manag. 2016;6:277–87.
Labiano-Fontcuberta A, Mitchell AJ, Moreno-García S, Benito-León J. Anxiety and depressive symptoms in caregivers of multiple sclerosis patients: the role of information processing speed impairment. J Neurol Sci. 2015;349:220–5.
Oreja-Guevara C, Miralles A, García-Caballero J, Noval S, Gabaldón L, Esteban-Vasallo MD, et al. Diseño de una vía clínica para la atención a los pacientes con esclerosis múltiple. Neurología. 2010;25:156–62.
Fernández O, Fernández V, Arbizu T, Izquierdo G, Bosca I, Arroyo R, et al. Characteristics of multiple sclerosis at onset and delay of diagnosis and treatment in Spain (the novo study). J Neurol. 2010;257:1500–7.
Rieckmann P, Centonze D, Elovaara I, Giovannoni G, Havrdová E, Kesselring J, et al. Unmet needs, burden of treatment, and patient engagement in multiple sclerosis: a combined perspective from the MS in the 21st century steering group. Mult Scler Relat Disord. 2018;19:153–60.
Emerson J, Cabaj M. Social return on investment. Mak Waves. 2000;11:10–4.
Narrillos H. Economía Social. Valoración y medición de la inversión social (método SROI). Madrid: Ecobook; 2012.
Tuan MT. Measuring and/or estimating social value creation: insights into eight integrated cost approaches. 2008. http://cmapspublic.ihmc.us/rid=1LHK87JH8-F72NL0-2R6P/WWL-report-measuring-estimating-social-value-creation%5B1%5D.pdf. Accessed 8 Feb 2016.
Willis E, Semple AC, de Waal H. Quantifying the benefits of peer support for people with dementia: a social return on investment (SROI) study. Dement Lond Engl. 2018;17:266–78.
Jones C, Edwards RT, Windle G, Dementia, team I research, others. Social return on investment analysis of an art group for people with dementia Lancet 2014;384:S43.
Merino M, Ivanova Y, Gómez-García T, Hidalgo-Vega Á, Díaz González F. García de Vicuña R, et al. Proyecto SROI-AR Impacto clínico, asistencial, económico y social del abordaje ideal de la artritis reumatoide en comparación con el abordaje actual. Madrid: Fundación Weber; 2019. http://weber.org.es/wp-content/uploads/2019/04/Informe_completo_SROI_Lilly_AAFF-1.pdf.
González A, Ivanova Y, Jiménez M, Merino M, Hidalgo Á, Alfonso S, et al. Retorno Social de la Inversión de un abordaje ideal de la psoriasis. Instituto Max Weber: Majadahonda, Madrid; 2016.
Durán Piñeiro G, Sánchez Carreira MC, Peña Gil C, Paredes-Galán E, Gómez Ruíz R, Lado Sestayo R, et al. El retorno económico y social de la e-interconsulta de cardiología en el área de Vigo. ICEDE Work Pap Ser ISSN 2254–7487. 2015;11:1–28.
de Castro Carpeño J, Fírvida Pérez JL, Lianes Barragán P, Cobo Dols MÁ, Gil Gil JM, Carrato Mena A, et al. Cuantificando el beneficio de la sustitución por vinorelbina oral en los pacientes susceptibles de tratamiento con vinorelbina. Estudio del retorno social de la inversión. Rev Esp Econ Salud. 2018;13:336–53.
Merino M, Jiménez M, Manito N, Casariego E, Ivanova Y, González-Domínguez A, et al. The social return on investment of a new approach to heart failure in the Spanish National Health System. ESC Heart Fail. 2020;n/a n/a. https://doi.org/10.1002/ehf2.12535.
Lophongpanit P, Tongsiri S, Thongprasert N. Social return on investment for patient treated by continuous ambulatory peritoneal Dialysis: a case study in Ubon Ratchathani Province, Thailand. Clin Outcomes Res. 2019;11:569–78.
Jones RB, Ashurst EJ, Atkey J, Duffy B. Older people going online: its value and before-after evaluation of volunteer support. J Med Internet Res. 2015;17. https://doi.org/10.2196/jmir.3943.
Scharlach AE. Estimating the value of volunteer-assisted community-based aging services: a case example. Home Health Care Serv Q. 2015;34:46–65.
Goudet S, Griffiths PL, Wainaina CW, Macharia TN, Wekesah FM, Wanjohi M, et al. Social value of a nutritional counselling and support program for breastfeeding in urban poor settings, Nairobi. BMC Public Health. 2018;18:424.
Banke-Thomas A, Madaj B, Kumar S, Ameh C, van den Broek N. Assessing value-for-money in maternal and newborn health. BMJ Glob Health. 2017;2. https://doi.org/10.1136/bmjgh-2017-000310.
Banke-Thomas AO, Madaj B, Charles A, van den Broek N. Social return on investment (SROI) methodology to account for value for money of public health interventions: a systematic review. BMC Public Health. 2015;15:582–95.
Masters R, Anwar E, Collins B, Cookson R, Capewell S. Return on investment of public health interventions: a systematic review. J Epidemiol Community Health. 2017;71:827–34.
Nicholls J, Lawlor E, Neitzert E, Goodspeed T. A guide to social return on investment. UK: The SROI Network. Accounting for Value; 2012. http://www.socialvalueuk.org/app/uploads/2016/03/The%20Guide%20to%20Social%20Return%20on%20Investment%202015.pdf
Instituto Nacional de Estadística. Índice de Precios de Consumo. Base 2016. Índices nacionales: general y de grupos ECOICOP. [Data file]. Retrieved from http://www.ine.es/jaxiT3/Tabla.htm?t=22553&L=0. Accessed 26 July 2017.
Sociedad Española de Neurología. Plan Estratégico Nacional para el Tratamiento Integral de las Enfermedades Neurológicas II (Pentien II). Madrid: SEN; 2016. https://issuu.com/senmadrid/docs/pentien_ii. Accessed 2 Feb 2018
Berger T, Adamczyk-Sowa M, Csépány T, Fazekas F, Hojs Fabjan T, Horáková D, et al. Management of multiple sclerosis patients in central European countries: current needs and potential solutions. Ther Adv Neurol Disord. 2018;11. https://doi.org/10.1177/1756286418759189.
Urbanos-Garrido R. La desigualdad en el acceso a las prestaciones sanitarias. Propuestas para lograr la equidad. Gac Sanit. 2016;30:25–30.
National Institute for Health and Care Excellence. How NICE measures value for money in relation to public health interventions. London: National Institute for Health and Care Excellence; 2013. https://www.nice.org.uk/Media/Default/guidance/LGB10-Briefing-20150126.pdf. Accessed 12 Jul 2018
Rieckmann P, Boyko A, Centonze D, Elovaara I, Giovannoni G, Havrdová E, et al. Achieving patient engagement in multiple sclerosis: a perspective from the multiple sclerosis in the 21st century steering group. Mult Scler Relat Disord. 2015;4:202–18.
Laing CM, Moules NJ. Social return on investment: a new approach to understanding and advocating for value in healthcare. JONA J Nurs Adm. 2017;47:623–8.
Dyakova M, Hamelmann C, Bellis MA, Besnier E, Grey CNB, Ashton K, et al. Investment for health and well-being: a review of the social return on investment from public health policies to support implementing the sustainable development goals by building on health 2020. WHO Regional Office for Europe: Copenhagen; 2017. http://www.ncbi.nlm.nih.gov/books/NBK453553/. Accessed 13 Jun 2018
Acknowledgements
We would like to thank Esclerosis Múltiple España and all MS patients who participated in answering the survey. Likewise, we would also like to thank the group of experts for their participation in the consensus on the set of proposals for the improvement to the MS approach: Dr. Pablo G. Baz Rodríguez (National coordinator of the SEMERGEN Neurology Working Group), Mrs. Guadalupe Piñeiro Corrales (Head of the Hospital Pharmacy Service, University Hospital of Vigo, Pontevedra), Mrs. María Valdivia García (nurse at the Fundación Madrid contra la EM), Mrs. Irene Bartolomé Gómez (physiotherapist at the Fundación Madrid contra la EM), Mrs. Laia Miralles Roca (social worker at the Fundación de Esclerosis Múltiple, Barcelona), and Ainhoa Ruiz del Agua (patient with MS, Bilbao).
Funding
This study was supported by ROCHE FARMA, SA. Authors working at ROCHE FARMA participated in the design of the study, the interpretation of the results and approved the final manuscript, as stated in the Authors’ contributions section.
Author information
Authors and Affiliations
Contributions
ERB, AHV and MM designed the study. TGG, MJ and MM participated in the analysis of data. EMT, OFF, PCR, ERB, EEP, RME, TGG, MJ, AHG and MM participated in the interpretation of data. MM drafted the manuscript. All authors substantively revised and approved the final manuscript.
Authors’ information
Not applicable.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The present study conforms with the ethical principles of the Declaration of Helsinki. This study did not require approval by any ethics committee as according to the Spanish law (“Ley 14/2007, de 3 de julio, de Investigación biomédica”), research projects carried out on human beings or their biological material have to be approved by a Research Ethics Committee, excluding observational studies where any patient treatment or intervention is modified.Footnote 2 Moreover, according to the Spanish law (“Ley 41/2002, de 14 de noviembre, básica reguladora de la autonomía del paciente y de derechos y obligaciones en materia de información y documentación clínica el consentimiento informado”), the informed consent has to be signed only when the activity of the study can affect patient’s health status.Footnote 3 Since our study is observational and patient data were obtained using an online anonymous survey, it was not necessary for patients to sign an informed consent in this study.
Consent for publication
Not applicable.
Competing interests
EM has received honoraria as consultant in advisory boards, and as chairperson or lecturer in meetings, and has also participated in clinical trials and other research projects promoted by Bayer, Biogen-Idec, Merck-Serono, Teva, Novartis, Almirall, Sanofi-Genzyme, Actelion and Roche. OF have received honoraria as consultant in advisory boards, and as chairmen or lecturer in meetings, and has also participated in clinical trials and other research projects promoted by Bayer, Biogen-Idec, Merck-Serono, Teva, Novartis, Allergan, Almirall, Sanofi-Genzyme and Roche. The rest of authors have no conflicting interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1.
Patient survey.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Moral Torres, E., Fernández Fernández, Ó., Carrascal Rueda, P. et al. Social value of a set of proposals for the ideal approach of multiple sclerosis within the Spanish National Health System: a social return on investment study. BMC Health Serv Res 20, 84 (2020). https://doi.org/10.1186/s12913-020-4946-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-020-4946-8