Abstract
Background
Health system science (HSS) encompasses both core and cross-cutting domains that emphasize the complex interplay of care delivery, finances, teamwork, and clinical practice that impact care quality and safety in health care. Although HSS skills are required during residency training for physicians, current HSS didactics have less emphasis on hands-on practice and experiential learning. Medical simulation can allow for experiential participation and reflection in a controlled environment. Our goal was to develop and pilot three simulation scenarios as part of an educational module for resident physicians that incorporated core and cross-cutting HSS domains.
Methods
Each scenario included a brief didactic, an interactive simulation in small-group breakout rooms, and a structured debriefing. The case scenario topics consisted of educational leadership, quality and safety, and implementation science. Learners from four residency programs (psychiatry, emergency medicine, orthopedics, ophthalmology) participated January – March 2021.
Results
A total of 95 resident physicians received our curricular module, and nearly all (95%) participants who completed a post-session survey reported perceived learning gains. Emotional reactions to the session were positive especially regarding the interactive role-play format. Recommendations for improvement included participation from non-physician professions and tailoring of scenarios for specific disciplines/role. Knowledge transfer included use of multiple stakeholder perspectives and effective negotiation by considering power/social structures.
Conclusions
The simulation-based scenarios can be feasibly applied for learner groups across different residency training programs. Simulations were conducted in a virtual learning environment, but future work can include in-person and actor-based simulations to further enhance emotional reactions and the reality of the case scenarios.
Similar content being viewed by others
Background
The Accreditation Council for Graduate Medical Education (ACGME) has incorporated multiple competencies related to health systems science in residency training to highlight the importance of understanding complexities of systems in delivering effective and safe patient care [1]. Core competencies in practice-based improvement and system-based practice are important components of health systems science (HSS) [2].
Several reports have identified deficits among newly trained physicians in leadership skills for HSS [3]. One challenge to teaching HSS is that it encompasses multiple competencies in health care delivery, financing, communication skills, team-based care, population health, and the attainment of patient safety and quality, which can then be further divided to identify core and cross-cutting domains [4]. Within our institution, some ad-hoc didactic lectures and apprenticeship-type electives in healthcare administration are being conducted within several disciplines for resident physicians, but no site-wide formal training in HSS is currently in place. Experts have called for radical transformation and redesign of educational curricula that prepare trainees to lead executive teams and address challenges in rapidly evolving systems of care [2].
Curricula that have been developed in HSS within undergraduate medical education focuses on content knowledge and didactics, but less on experiential learning [5]. Although resident physicians are constantly placed in real-life situations that include many cross cutting HSS domains, they are rarely debriefed post-event or viewed through an HSS lens [6]. Simulation-based medical education is a tool that incorporates structured, skill-building learning experiences and has been used to teach physicians communication and non-technical skills. Simulation helps activate learners’ emotional or affective states, allowing for development of cognitive and communication skills necessary in clinical practice through an immersive and psychologically safe environment that ultimately leads to significant improvement in patient safety [7]. Studies have demonstrated feasibility in simulation to target healthcare organizational leadership and systems science for executives and managers [8]. Although case-based curricula for patient safety and quality improvement that involve discussions and simulation likely exist locally at various institutions, no standardized or widely used curricula for HSS that incorporates simulation currently exist for graduate medical education.
In this innovation report, we describe the implementation of a structured curricular module consisting of three simulation-based clinical case scenarios for resident physicians across four residency programs that integrate core and cross-cutting competencies in HSS using realistic situations that can occur in healthcare settings.
Methods
Theoretical background and curricular design
To address the complexity of teaching HSS, we used an instructional and evaluation approach that was grounded and aligned to Self-Determination Theory (SDT) [9]. SDT emphasizes that learners' engagement and learning outcomes are directly related to their relationships with each other, perceived competence in a content area, and autonomy regarding their engagement. Our educational innovation reflects SDT by scaffolding participants’ knowledge throughout each curricular case scenario by incorporating a clear structure for respectful interactions amongst learner groups and allowing for a high degree of autonomy in how individuals enacted their role. SDT builds on the benefits of simulation-based learning by providing a more direct emotional connection to the learning materials and a setting for practicing interpersonal dynamics in a controlled environment. SDT also pairs with our evaluation approach, which explores participants’ perceived learning gains, specific changes in their understanding, and value of session components. Feedback provided by volunteer participants early in the design process was used to inform changes for subsequent workshop iterations (See Fig. 1).
Using this SDT-based approach, we embedded HSS core domains as well as cross-cutting domains to develop three interdisciplinary team-based case scenarios: 1) Implementation Science, 2) Education Leadership, and 3) Quality and Safety (see Additional file 1: Appendix 1). Each scenario detailed a clinical challenge with a specific systems-based clinical issue that participant teams are tasked to address. Residents had assigned roles within the scenario exercise that they portrayed and acted out during the simulation. We selected clinical contexts that would have applicability and familiarity across disciplines and training backgrounds. Scenario summaries and corresponding HSS domains are listed in Table 1. We initially included a fourth scenario focusing on health informatics and telemedicine but opted to drop it from the curriculum due to low level of interest from our graduate medical educational leadership.
Participant recruitment
Residency program directors at Yale School of Medicine were contacted by one of the authors (LL) requesting to have resident physicians participate as part of their core didactics. Directors of four residency programs representing procedural and non-procedural specialties (emergency medicine, adult psychiatry, ophthalmology, and orthopedic surgery) voiced interest given lack of formal training within their existing curricula and agreed to have their residents from across postgraduate years participate in the HSS curriculum as part of their programs’ core didactic series. Residents from all postgraduate years (PGY) 1–5 provided verbal consent for participation prior to the start of the simulation. This educational intervention was approved and deemed exempt by the Yale University Institutional Review Board. The institutional review board approved use of verbal consent for participation in the study given that the research presents no more than minimal risk of harm to subjects.
Simulation sessions
We conducted the modules in a virtual learning environment using Zoom videoconferencing. Each session lasted two hours and included a ten-minute didactic that provided a conceptual framework of the main content topic. These ten-minute didactics incorporated the main teaching points highlighted in Table 1 and contained basic content knowledge that the participants could incorporate into the simulation activity. Participants were also provided anticipatory guidance on the simulation activity in a pre-briefing prior to the start of the simulation activity. This pre-briefing established expectations and for the learners including ground rules of engagement through role enactment within the exercise and the importance of psychological safety. After the pre-briefing, participants were divided into groups of four to six, in the form of a “breakout room,” where they participated in a 30-min tabletop simulation with designated roles. Each participant received a detailed description of the systems science problem at hand as well as the background and relevant goals of their assigned role within the simulation. When possible, a facilitator was present to answer questions and record observations of the activity to inform the larger group debriefing. Immediately following completion of the simulation, participants returned to a common room for a structured large group debriefing led by one of the study authors.
Evaluation
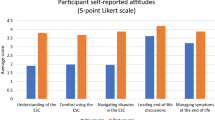
Our evaluation approach reflected a developmental phase of applying HSS curricular content into graduate medical education, as no standardized approach has been well-established to evaluate the effectiveness of HSS curricula. At the start of each session, participants were asked about their prior experience with the session content via an electronic survey to identify the perceived needs by the specific learner group undergoing the simulation-based case scenario. At the end of each session, participants were asked to complete an anonymous post-intervention survey-based evaluation. The evaluation incorporated a core set of Likert-scale and qualitative questions that was adapted to apply to all three case scenarios (See Additional file 2: Appendix 2). We calculated means and standard deviations for responses to each survey question, percentage positive responses (inclusive of responses with 3, 4 and 5 on the Likert scale). Narrative free-text survey responses were collected and coded using directed content analysis techniques [12] to derive recurrent themes.
Curricular and evaluation iteration
In building the three simulation modules, several iterations occurred to the curricula, debriefing approach, and evaluation early on the design phase. These included limiting the total number of roles and group sizes incorporated into simulation, as higher numbers of roles made it difficult to administratively manage the small group breakout room simulations. In addition, volunteer participants who helped with piloting and testing of the modules provided early feedback that they received the most benefit from the simulation and debriefing portions, so the didactic portion was shortened to highlight the key content information needed to participate in the simulation. Surveys were developed using an iterative refinement process led by a psychometric expert (co-author MB) and tested on a group of volunteer resident learners prior to formal launch.
Results
A total of 95 resident physicians across postgraduate years (PGY 1–5) representing > 95% of all emergency medicine (n = 41), psychiatry (n = 24), ophthalmology (n = 12), and orthopedic surgery (n = 18) trainees at our institution participated in our curricular modules between January to March 2021. We conducted each of the three scenarios with residents from two different specialties. In the needs assessment survey responses (n = 95), the majority of participants responded “not at all” to “moderate” when asked about familiarity with the session content (72%), prior training (93%), and experience implementing structural changes (94%). This pattern indicated a clear need and room for growth among participants on the HSS topics covered in all three case scenarios.
Table 2 describes demographic data of our post-session survey respondents (n = 66, 69.5% response rate). Table 3 summarizes results from our post-session survey, which consisted of mostly positive feedback. There were not major differences in responses between participants from different specialties that attended the same scenarios. Coded qualitative responses resulted in three overarching themes (see Table 4). Emotions and reactions to the session (Theme 1) were positive overall, especially with regards to the interactive role-play format allowing for immersion within a health system science context. Recommendations for improving feasibility and applicability of the module (Theme 2) included participation from non-physician professions, distillation of core concepts with a post-session handout, tailoring of scenarios for specific disciplines/roles, and more directed support from facilitators during the breakout. Participants also described specific instances of knowledge application and transfer to the bedside (Theme 3) via incorporation of multiple stakeholder perspectives, effective negotiation by considering power/social structures, and enactment of system change using incentivization that considers downstream impacts on frontline staff.
Implications for practice
In this innovation report, we developed simulation-based case scenarios to teach core and cross-cutting domains in HSS that were feasibly applied to residents in both medical and surgical subspecialties. We found that participants reported limited knowledge and familiarity with HSS topics, despite ACGME requirements. This may be due to the fact that (1) the content is not currently being taught in a structured way, and (2) HSS skills require an experiential method like simulation to effectively grasp, similar to other non-technical skills (e.g., end-of-life discussion, leadership and communication) [13]. We also found that participants reported that they most preferred the simulation-based portion of the module. Qualitative feedback from learners remarked on the challenges and gratification of developing rapid team cohesion to solve a health system challenge within the breakout format, mimicking the skills needed to effectively coordinate disparate stakeholders in temporary or ad-hoc groups [14]. Our pilot implementation was supported by a small foundation grant which allowed for a part-time research associate to administer and organize the sessions and some dedicated effort by a simulation specialist to lead the debriefings. Attempts to pilot similar curricula at other organizations may benefit from dedicated finances to similarly provide administrative support and simulation expertise for optimal outcomes.
Important next steps for the work include expansion and testing of the modules to additional specialties. In addition, the simulation module format may serve as a template for additional modules to be developed covering more content areas in HSS. Further piloting of the entire set of modules in each specialty residency cohort will be able to assess specialty-specific needs and content applicability. Our sessions incorporated trainees across multiple years of training level within the same session, which did not appear to hinder learning. In fact, some residents remarked positively on how the assignment of roles within the breakout often subverted the usual professional hierarchy amongst participants (i.e., a more junior resident would act as medical director while a chief resident would act as a nurse) which added humor and novelty to the experience.
The simulation modules were created using a virtual learning environment due to social distancing requirements at time of implementation and attempts at accommodating disparate trainee schedules, but participants remarked on some challenges to engaging with each other during the breakout session via the Zoom videoconferencing format. A future direction may be to use in-person tabletop sessions and actors to augment psychological realism of interpersonal interactions that occur during simulation. Additional approaches to evaluation, including incorporating assessments such as a situational judgment test and additional surveys to assess long-term impact post-residency can be developed and used to more carefully assess learner knowledge and application into clinical practice. In our next step of implementation, we aim to integrate our module within an institution-wide chief resident forum to target learners who are most likely to have jobs that include HSS in their day-to-day work after graduation and pilot our scenarios in other nearby institutions.
Conclusions
In conclusion, we found that interactive, simulation-based learning modules in HSS were feasible to develop and apply to diverse physician trainee cohorts. Our evaluation showed that residents expressed lack of baseline content knowledge on multiple topics in health systems science, and that learning about core and cross-cutting domains using simulation-based modules produced perceived learning gains related to systems-based practice and care quality and was valued by participants.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
ACGME. ACGME Common Program Requirements (Residency). 2020.
Gonzalo JD, Wolpaw T, Wolpaw D. Curricular Transformation in Health Systems Science: The Need for Global Change. Acad Med. 2018;93(10):1431–3.
Crosson FJ, Leu J, Roemer BM. Ross MN Gaps In Residency Training Should Be Addressed To Better Prepare Doctors For A Twenty-First-Century Delivery System. Health Aff. 2011;30(11):2142–8.
Gonzalo JD, Dekhtyar M, Starr SR, et al. Health Systems Science Curricula in Undergraduate Medical Education: Identifying and Defining a Potential Curricular Framework. Acad Med. 2017;92(1):123–31.
Gonzalo JD, Caverzagie KJ, Hawkins RE, Lawson L, Wolpaw DR, Chang A. Concerns and Responses for Integrating Health Systems Science Into Medical Education. Acad Med. 2018;93(6):843–9.
Crosson FJ, Leu J, Roemer BM, Ross MN. Gaps In Residency Training Should Be Addressed To Better Prepare Doctors For A Twenty-First-Century Delivery System. Health Aff (Millwood). 2011;30(11):2142–8.
McGaghie WC, Draycott TJ, Dunn WF, Lopez CM, Stefanidis D. Evaluating the impact of simulation on translational patient outcomes. Simul Healthc. 2011;6(Suppl):S42-47.
Cook DA. How much evidence does it take? A cumulative meta-analysis of outcomes of simulation-based education. Med Educ. 2014;48(8):750–60.
Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000;55(1):68–78.
Aarons GA, Hurlburt M, Horwitz SM. Advancing a Conceptual Model of Evidence-Based Practice Implementation in Public Service Sectors. Adm Policy Ment Health. 2011;38(1):4–23.
Sebenius JK. BATNAs in Negotiation: Common Errors and Three Kinds of “No.” Negot J. 2017;33(2):89–99.
Hsieh H-F, Shannon SE. Three Approaches to Qualitative Content Analysis. Qual Health Res. 2016;15(9):1277–88.
Nicksa GA, Anderson C, Fidler R, Stewart L. Innovative Approach Using Interprofessional Simulation to Educate Surgical Residents in Technical and Nontechnical Skills in High-Risk Clinical Scenarios. JAMA Surgery. 2015;150(3):201–7.
Valentine MA, Edmondson AC. Team Scaffolds: How Mesolevel Structures Enable Role-Based Coordination in Temporary Groups. Organ Sci. 2015;26(2):405–22.
Acknowledgements
We would like to acknowledge the additional support of Yale Center for Medical Simulation staff member Joy Grabow, simulation supervisor, for her work in coordinating this educational module as well as her acting as the standardized patient during the simulation.
Funding
Dr. Luming Li received support from the 2020 AMA Accelerating Change in Medical Education Innovation Grant Program for this project. Dr. Wong is supported by the Robert E. Leet and Clara Guthrie Patterson Trust Mentored Research Award, the National Center for Advancing Translational Science (1 KL2 TR001862-01), the National Institute for Mental Health (1 K23 K23MH126366-01A1), and the Agency for Healthcare Research and Quality (1 R01 HS28340-01). Dr. Ray is supported by the National Institute of Minority Health and Health Disparities (1 R01 MD014853-01A1) and the Agency for Healthcare Research and Quality (1 R01 HS28340-01).
Author information
Authors and Affiliations
Contributions
LL, JMR, MB, and AHW conceived and designed the study; LL, JMR, MB, WK, and AHW performed data collection, analysis, and interpretation of the data. SJH and JC performed external review and auditing of data collection and analysis. All authors drafted and contributed to critical revisions of the article. LL takes responsibility for the paper as a whole. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study received ethical approval from the Yale University human investigation committee as an exempt study (HIC# 2000029226, October 20, 2020). All methods were performed in accordance with the relevant guidelines and regulations. The Yale University Institutional Review Board approved use of verbal consent for participation in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Appendix 1. Case Scenarios.
Additional file 2:
Appendix 2. Post-survey template items
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, L., Ray, J.M., Bathgate, M. et al. Implementation of simulation-based health systems science modules for resident physicians. BMC Med Educ 22, 584 (2022). https://doi.org/10.1186/s12909-022-03627-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12909-022-03627-w