Abstract
Background
Three-dimensional (3D) printing technology enables the translation of 2-dimensional (2D) medical imaging into a physical replica of a patient’s individual anatomy and may enhance the understanding of congenital heart defects (CHD). We aimed to evaluate the usefulness of a spectrum of 3D-printed models in teaching CHD to medical students.
Results
We performed a prospective, randomized educational procedure to teach fifth year medical students four CHDs (atrial septal defect (ASD, n = 74), ventricular septal defect (VSD, n = 50), coarctation of aorta (CoA, n = 118) and tetralogy of Fallot (ToF, n = 105)). Students were randomized into printing groups or control groups. All students received the same 20 min lecture with projected digital 2D images. The printing groups also manipulated 3D printed models during the lecture. Both groups answered an objective survey (Multiple-choice questionnaire) twice, pre- and post-test, and completed a post-lecture subjective survey.
Three hundred forty-seven students were included and both teaching groups for each CHD were comparable in age, sex and pre-test score. Overall, objective knowledge improved after the lecture and was higher in the printing group compared to the control group (16.3 ± 2.6 vs 14.8 ± 2.8 out of 20, p < 0.0001). Similar results were observed for each CHD (p = 0.0001 ASD group; p = 0.002 VSD group; p = 0.0005 CoA group; p = 0.003 ToF group). Students’ opinion of their understanding of CHDs was higher in the printing group compared to the control group (respectively 4.2 ± 0.5 vs 3.8 ± 0.4 out of 5, p < 0.0001).
Conclusion
The use of 3D printed models in CHD lectures improve both objective knowledge and learner satisfaction for medical students. The practice should be mainstreamed.
Similar content being viewed by others
Introduction
Congenital heart defects (CHD) are a leading cause of morbidity in pediatric patients and is an emerging field in adult medicine. Therefore, the anatomy and pathophysiology of CHD is an integral and increasingly important part of medical education [1]. Two-dimensional (2D) representations are the mainstream method of teaching CHD. The ability to translate these 2D images into 3-dimensional (3D) representations of the defect is critical to the understanding, diagnosis, and management of underlying disease. Individuals vary in their ability to deduce 3D spatial relationships from 2D imaging [2]. Since the first stereolithography technique used by Charles Hull in 1983, the method of transforming digital models into physical objects has been one of the main disruptive technologies in the first two decades of the twenty-first century. In healthcare, 3D printing is being widely adopted in many areas, from creating bioprosthetics, to improving surgical planning and as an educational tool [3,4,5,6]. 3D models provide a unique support for the comprehension of simple to more complex cardiac malformations. Compared to other tissue engineering scaffolds, 3D printing has the advantages of relatively low production costs and accurate generation of an anatomical structure in a short time [7]. In order to create 3D printed heart and blood vessel models, multiple imaging techniques might be used to obtain a volumetric representation of the heart, such as computed tomography (CT), 3D echocardiography and cardiac magnetic resonance imaging [8].
Few studies have evaluated the usefulness of 3D printed heart models to teach CHD to medical students, and most of the research has focused on learners satisfaction or has often analysed a single CHD with a small student sample [9,10,11,12]. Moreover, studies have reported heterogeneous conclusions with regards to learners’ knowledge acquisition after teaching with 3D printed heart models, regardless of the disease complexity.
We aimed to evaluate the usefulness of 3D printed models in teaching medical students four CHD, using a randomized controlled trial design.
Method
Creating 3D printed models
This study was approved by the Institutional Review Board at the Toulouse University Hospital Affiliated with Toulouse University Paul Sabatier School of Medicine in the form of modified teaching method study. All methods were performed in accordance with the relevant guidelines and regulations.
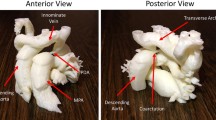
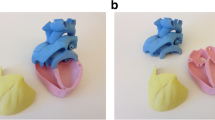
We conducted a retrospective search for extractable DICOM files of cardiac CT and 3D echocardiography performed in our hospital over the past year in routine follow-up of CHD. Based on the quality, after anonymization, we selected four CT exams of coarctation of the aorta (CoA): one neonatal case, one infant, one stent-repaired CoA, and one aortic hypoplasia; four CT exams of ventricular septal defect (VSD): one perimembranous VSD, one inlet VSD, one outlet VSD without malalignment, one outlet VSD with malalignment; two CT exams and one 3D echocardiography of atrial septal defect (ASD): two different ostium secundum ASDs and one sinus venosus ASD; and two CT exams of Tetralogy of Fallot (ToF) (Fig. 1 and S1 ToF, S2 neonatal aortic hypoplasia, S3 VSD: 3D PDF). These four CHDs are among the most common and are included in the French medical program. We used Mimics and 3-Matic (Materialise HQ, Leuven, Belgium) software for segmentation and to generate the final real scale 3D virtual model exported as an STL file. STL files were finally printed with a Stream 20 pro printer (Volumic, France) and biodegradable polylactic acid (PLA) filament. For the ASD model from echocardiography data, image was acquired by 3D transesophageal echocardiography in 3D zoom mode using the EPIQ system (version 7C, Philips Medical Systems, Andover, MA) and an X8-2t phased array transducer. All models were printed in duplicate for a total of 26 models. The mean period time needed to segmentate models was around 15 min for ASD and CoA, 30 min for VSD and 60 min for ToF. The mean period time to print the models were 30 min for ASD, and 150 min for ToF, CoA and VSD.
Study population and intervention
Fifth year medical students from the Paul Sabatier University of Toulouse faculty of medicine were anonymously included. In France, medical degree is validated at the end of the 6th year corresponding to a MBBS. The paediatric module was shared with gynaecology, orthopaedic, and rheumatology and clinical practice was provided during 1 month after a 1 month of full lecture. All students attended lectures on CHD as part of the standard academic training. Different students attended additional 20-min lectures for one of the following CHD: CoA, VSD, ASD and ToF. Lectures were held on separate days by the same teacher and so each learner attended only one lecture for one of the four different CHD.
For each 20-min CHD lecture, students were randomized into two groups; one was the intervention group (printing) and the other a control group (control). Both groups attended the same lecture in two separate sessions which consisted of standard slides and projected two-dimensional models on anatomy, physiopathology and the diagnosis and management of CHD. After an initial description of each printed model, students in the printing group had the possibility during all the lecture to freely analyze and manipulate 3D printed models for the CHD presented by sharing models and passing them around during the lectures. Students were also free to ask question about the models during the lecture.
Acquisition evaluation
To evaluate knowledge acquisition, each student answered the same multiple-choice test twice, pre- and post-lecture, on the respective CHD with a maximal score of 20 points corresponding to 20 true or false questions. Questionnaires assessed knowledge acquisition on anatomy, pathophysiology and overall management. Questionnaires were made by PA, CK, and AG and met the faculty’s end-of-year exam validation criteria. In the post-lecture test, we also included three more 5-point Likert scale (1 to 5: 1 = strongly disagree, 5 = strongly agree) questions to assess self-rating of acquired general knowledge and knowledge on the diagnosis and treatment of CHD. The participants in the printing group were also asked to rate their satisfaction with the 3D printed models as a teaching tool, and to use a 5-point Likert scale to indicate whether this helped them to understand the presented CHD. An example of the post-test questionnaire including the objective and subjective questionnaire is provided (S4 and S5: supplementary method).
Analysis
Quantitative variables are expressed as mean ± standard deviation (SD). Normally distributed continuous variables were compared with t tests and non-normally distributed variables were compared with Mann-Whitney tests. Normality was assessed by the Shapiro-Wilk normality test. Changes in subjective survey scores were compared with t tests or Mann-Whitney tests in terms of the normality distribution. Knowledge ratings from the ‘pre-’ and ‘post’-intervention survey were analysed using a paired test for each CHD or a Wilcoxon matched-pairs signed rank test if the distribution was not normal. Increases in scores were assessed by subtracting the pre-test score from the post-test score. The printing group was then compared to the control group with a t test.
P-values < 0.05 were considered statistically significant. Statistical analysis was carried out using GraphPad Prism 9 (GraphPad Software, Inc., San Diego, CA).
Results
We enrolled 347 students including 74 in the ASD group (55.4% in the printing group), 50 in the VSD group (50% in the printing group), 118 in the CoA group (55% in the printing group), and 105 in the ToF group (49.5% in the printing group). The model/student ratio was 1/7 for ASD, 1/3 for VSD, 1/8 for CoA, and 1/13 for ToF.
The two teaching groups for each CHD were comparable in age, gender and pre-test score (Table 1).
Overall, there was no difference in the pre-lecture tests between printing and control groups, with a median global score of 11.8 ± 2.4 out of a maximal score of 20 for the control group and 11.6 ± 2.5 out of 20 for the printing group (p = 0.46) (Fig. 2). Knowledge improved in both groups after the lecture but was higher in the printing group than the control group (16.3 ± 2.6 vs 14.8 ± 2.8 out of 20, p < 0.0001). The increase in score was higher in the printing group than the control group (4.5 ± 0.4 vs 3.2 ± 0.5, p = 0.001).
Similarly, for each CHD group, no difference in the baseline objective test scores was observed, and all groups improved after the lecture. The post-lecture scores were significantly higher for the printing group than for the control group, regardless of the CHD (p = 0.0001 in the ASD group; p = 0.002 in the VSD group; p = 0.0005 in the CoA group; p = 0.003 in the ToF group), (Fig. 3). The increase in score was also higher for each CHD in the printing group (Table 2).
In the post-lecture subjective 5-point Likert scale evaluation, the students learning through 3D printed models scored higher in their self-reported understanding of the CHDs, their diagnostic modalities and treatment options (Fig. 4). For all CHDs combined, the mean 5-point Likert scale was 3.8 ± 0.4 out of 5 for control groups versus 4.2 ± 0.5 for printing groups (p < 0.0001).
Students’ self-reported understanding of CHDs, their diagnostic modalities and treatment options: boxplot of means of three 5-point Likert scale items according to the CHD (ASD, VSD, CoA, and ToF). ASD: Atrial septal defect; CoA: Coarctation of the aorta; CHD: Congenital heart defects; ToF: Tetralogy of Fallot; VSD: Ventricular septal defect
Most of the students strongly agreed that learning CHD through 3D printed models was more useful than through projected images. The score was approximately 4 out of 5 on the 5-point Likert scale regardless of the CHD (Fig. 5).
Discussion
The main strength of this study is that it evaluated several types of CHD and demonstrated that teaching through 3D printed models improves students’ objective performance in post-lecture scores for each CHD. Moreover, students in the 3D printing group reported a subjective improvement in the understanding of the CHDs, their diagnostic modalities and treatment option with this teaching method compared to a standard lecture. Therefore, the feedback from participants was generally positive and enthusiastic with a higher satisfaction score when 3D printing was involved.
Previous studies reported variable results using different methodologies among medical students or paediatric residents. Based on an objective questionnaire, Su et al. [13] found that 3rd year medical students taught with 3D printed heart models demonstrated a significant improvement in structural conceptualization of VSD compared to a control group. Three-dimensional printed models of vascular rings have also been shown to benefit residents learning about CHD [11]. Nevertheless, Loke et al. found no improvement in factual knowledge acquisition with the use of 3D ToF models for second year residents [14].
Most of the previous studies only reported student opinion rather than objective measures of their learning [10, 15], while only a few used a control group like us [13, 14]. Non-randomization and subjective assessment made the results of these studies less convincing and so strengthen our results. In our study knowledge was enhanced among fifth year medical students in all groups, including the ToF group. We also found no difference regarding the complexity of CHD, while recently Smerling et al. found a correlation [16]. They studied only 45 1st year medical students using a self-reported knowledge survey during a CHD workshop where all students had four different stations (Video, 2D, specimen and 3D), which makes an objective comparison difficult. Nevertheless, they also noted an increase in knowledge regarding all defects.
For decades, heart specimens have been incredibly useful in providing physical 3D samples of heart defects for medical education. Studies suggest no disadvantages to using 3D printed heart models compared to cadaveric specimens, which demonstrates at least equivalent educational outcomes [16, 17]. However, the limited availability, durability and reproducibility of cadaveric heart specimens makes it difficult to spread them and reinforces the interest of 3D printed models to teach CHD. Recently, the Archiving Working Group of the International Society for Nomenclature of Paediatric and Congenital Heart Disease recommends generating 3D digital images of cadaveric heart specimens for printing [18]. From a recent medical educational meta-analysis the 3D printing group had better accuracy and shorter answering time when compared with conventional models (including specimens, plastic products, and 2D anatomical pictures) [19].
The first step towards using 3D printed models in medical education would be to establish local 3D libraries. However, recently some authors have promoted a 3D Heart Library to disseminate validated 3D models through an open-access platform as a peer-reviewed subset of content on the National Institutes of Health 3D Print Exchange [4]. In our experience, models can be easily created from CT scans and 3D echocardiography performed in routine patient follow-up. Several versions of software are available to perform the segmentation and modelling processes. These models are durable and the cost of a printed model is affordable when a 3D printer is already available [7]. The translation of medical imaging data into 3D printed models requires knowledge of anatomy, pathology, imaging physics and engineering concepts related to 3D printing. Therefore, models are most likely to be created by a team.
The impact of teaching with 3D heart models could also be assessed in other situations and has been used to enhance congenital heart critical care via simulation training of multidisciplinary intensive care teams [20].
The recent SARS-CoV-2 pandemic has seen the confirmation of more than 100 million cases at the time of writing, resulting in the imposition of rigorous public health measures such as a quarantine [21, 22]. New interactive forms of virtual teaching have been developed and seem effective and could include virtual-reality or digital 3D PDF files. Beyond the negative effect on students’ mental well-being, technical challenges, confidentiality issues, reduced student engagement, and a lack of assessment have been described [23, 24]. Despite the impact of COVID-19 on medical education, hands-on experience that is provided in a safe environment with 3D printed models should be encouraged.
Limitations of our study include the high specificity of the population, which makes these results difficult to extrapolate to all medical and healthcare professionals. Nonetheless, other researchers have found similar results in populations with highly variable degrees of prior knowledge on CHD [12, 13]. Additionally, we only evaluated the usefulness of 3D printed models for teaching a limited group of simple or moderate CHDs. This is mainly due to our population’s limited prior knowledge of CHD. Therefore, complex CHD such as double outlet right ventricle could not be assessed.
Additionally, we did not test the long-term increase in knowledge to assess knowledge retention. Therefore, we cannot predict whether the positive effects of learning from these models are sustained over a longer period of time.
Finally, 3D printed models do not necessarily provide a good representation of all aspects of heart anatomy and physiology since valve tissue is often poorly recreated. Verbal explanation and guidance remain fundamental for the model.
Conclusion
3D printed CHD models are a useful resource for teaching in medical schools improving significantly CHD knowledge acquisition for medical students. These findings re-emphasize the role of these models considering the range of CHD severities, and promote the use of this technology in teaching CHD to medical students.
Availability of data and materials
Additional data and materials can be made available upon request to the corresponding author.
Abbreviations
- 2D:
-
Two-dimensional
- 3D:
-
Three-dimensional
- ASD:
-
Atrial septal defect
- CoA:
-
Coarctation of the aorta
- CHD:
-
Congenital heart defects
- CT:
-
Computed tomography
- ToF:
-
Tetralogy of Fallot
- VSD:
-
Ventricular septal defect
References
Baumgartner H, De Backer J, Babu-Narayan SV, Budts W, Chessa M, Diller G-P, et al. 2020 ESC guidelines for the management of adult congenital heart disease: the task force for the management of adult congenital heart disease of the European Society of Cardiology (ESC). Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Adult Congenital Heart Disease (ISACHD). Eur Heart J. 2021;42(6):563–645. https://doi.org/10.1093/eurheartj/ehaa554.
Hoyek N, Collet C, Rastello O, Fargier P, Thiriet P, Guillot A. Enhancement of mental rotation abilities and its effect on anatomy learning. Teach Learn Med. 2009;21(3):201–6. https://doi.org/10.1080/10401330903014178.
Hadeed K, Acar P, Dulac Y, Cuttone F, Alacoque X, Karsenty C. Cardiac 3D printing for better understanding of congenital heart disease. Arch Cardiovasc Dis. 2018;111(1):1–4. https://doi.org/10.1016/j.acvd.2017.10.001.
Bramlet M, Olivieri L, Farooqi K, Ripley B, Coakley M. Impact of three-dimensional printing on the study and treatment of congenital heart disease. Circ Res. 2017;120(6):904–7.
Valverde I, Gomez-Ciriza G, Hussain T, Suarez-Mejias C, Velasco-Forte MN, Byrne N, et al. Three-dimensional printed models for surgical planning of complex congenital heart defects: an international multicentre study. Eur J Cardiothorac Surg. 2017;52(6):1139–48. https://doi.org/10.1093/ejcts/ezx208.
Valverde I. Three-dimensional printed cardiac models: applications in the field of medical education, cardiovascular surgery, and structural heart interventions. Rev Espanola Cardiol Engl Ed. 2017;70(4):282–91. https://doi.org/10.1016/j.recesp.2016.09.043.
McMenamin PG, Quayle MR, McHenry CR, Adams JW. The production of anatomical teaching resources using three-dimensional (3D) printing technology. Anat Sci Educ. 2014;7(6):479–86. https://doi.org/10.1002/ase.1475.
Acar P, Hadeed K, Dulac Y. Advances in 3D echocardiography: from foetus to printing. Arch Cardiovasc Dis. 2016;109(2):84–6. https://doi.org/10.1016/j.acvd.2015.09.004.
Biglino G, Capelli C, Wray J, Schievano S, Leaver L-K, Khambadkone S, et al. 3D-manufactured patient-specific models of congenital heart defects for communication in clinical practice: feasibility and acceptability. BMJ Open. 2015;5(4):e007165. https://doi.org/10.1136/bmjopen-2014-007165.
Costello JP, Olivieri LJ, Su L, Krieger A, Alfares F, Thabit O, et al. Incorporating three-dimensional printing into a simulation-based congenital heart disease and critical care training curriculum for resident physicians. Congenit Heart Dis. 2015;10(2):185–90. https://doi.org/10.1111/chd.12238.
Jones TW, Seckeler MD. Use of 3D models of vascular rings and slings to improve resident education. Congenit Heart Dis. 2017;12(5):578–82. https://doi.org/10.1111/chd.12486.
White SC, Sedler J, Jones TW, Seckeler M. Utility of three-dimensional models in resident education on simple and complex intracardiac congenital heart defects. Congenit Heart Dis. 2018;13(6):1045–9. https://doi.org/10.1111/chd.12673.
Su W, Xiao Y, He S, Huang P, Deng X. Three-dimensional printing models in congenital heart disease education for medical students: a controlled comparative study. BMC Med Educ. 2018;18(1):178. https://doi.org/10.1186/s12909-018-1293-0.
Loke Y-H, Harahsheh AS, Krieger A, Olivieri LJ. Usage of 3D models of tetralogy of Fallot for medical education: impact on learning congenital heart disease. BMC Med Educ. 2017;17(1):54. https://doi.org/10.1186/s12909-017-0889-0.
Costello JP, Olivieri LJ, Krieger A, Thabit O, Marshall MB, Yoo S-J, et al. Utilizing three-dimensional printing technology to assess the feasibility of high-fidelity synthetic ventricular septal defect models for simulation in medical education. World J Pediatr Congenit Heart Surg. 2014;5(3):421–6. https://doi.org/10.1177/2150135114528721.
Smerling J, Marboe CC, Lefkowitch JH, Pavlicova M, Bacha E, Einstein AJ, et al. Utility of 3D printed cardiac models for medical student education in congenital heart disease: across a spectrum of disease severity. Pediatr Cardiol. 2019;40(6):1258–65. https://doi.org/10.1007/s00246-019-02146-8.
Lim KHA, Loo ZY, Goldie SJ, Adams JW, McMenamin PG. Use of 3D printed models in medical education: a randomized control trial comparing 3D prints versus cadaveric materials for learning external cardiac anatomy. Anat Sci Educ. 2016;9(3):213–21. https://doi.org/10.1002/ase.1573.
Seslar SP, Shepard CW, Giroud JM, Aiello VD, Cook AC, Spicer DE, et al. Lost treasures: a plea for the systematic preservation of cadaveric heart specimens through three-dimensional digital imaging. Cardiol Young. 2015;25(8):1457–9. https://doi.org/10.1017/S1047951115002589.
Ye Z, Dun A, Jiang H, Nie C, Zhao S, Wang T, et al. The role of 3D printed models in the teaching of human anatomy: a systematic review and meta-analysis. BMC Med Educ. 2020;20(1):335. https://doi.org/10.1186/s12909-020-02242-x.
Olivieri LJ, Su L, Hynes CF, Krieger A, Alfares FA, Ramakrishnan K, et al. ‘Just-in-time’ simulation training using 3-D printed cardiac models after congenital cardiac surgery. World J Pediatr Congenit Heart Surg. 2016;7(2):164–8. https://doi.org/10.1177/2150135115623961.
Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–33. https://doi.org/10.1056/NEJMoa2001017.
COVID-19 Map - Johns Hopkins coronavirus resource center [Internet]. [cited 2021 Jan 5]. Available from: https://coronavirus.jhu.edu/map.html
Wilcha R-J. Effectiveness of virtual medical teaching during the COVID-19 crisis: systematic review. JMIR Med Educ. 2020;6(2):e20963. https://doi.org/10.2196/20963.
Alsoufi A, Alsuyihili A, Msherghi A, Elhadi A, Atiyah H, Ashini A, et al. Impact of the COVID-19 pandemic on medical education: medical students’ knowledge, attitudes, and practices regarding electronic learning. PLoS One. 2020;15(11):e0242905. https://doi.org/10.1371/journal.pone.0242905.
Acknowledgements
None.
Funding
There was no funding for the study.
Author information
Authors and Affiliations
Contributions
Conceived and designed the analysis: PA, KH, AG, CK. Collected the data: AG, YD, CK, RV, BD. Contributed data or analysis tools: AG, YD, JB, KH, RV, BD, CD, PV. Performed the analysis: AG, CK, KH, SH. Wrote the paper: CK. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Institutional Review Board at the Toulouse University Hospital Affiliated with Toulouse University Paul Sabatier School of Medicine in the form of modified teaching method study. Considering the nature of the study, written consent from each individual participating in the study was waived by the IRB (Comité d’Ethique de la Recherche, Hôtel-Dieu, Direction de la Recherche Médicale et Innovation, Hopitaux de Toulouse).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: S1.
3D-PDF of tetralogy of Fallot: feel free to crop and navigate into the model.
Additional file 2: S2.
3D-PDF of neonatal aortic hypoplasia: feel free to crop and navigate into the model.
Additional file 3: S3.
3D-PDF of ventricular septal defect: feel free to crop and navigate into the model.
Additional file 4: S4.
The post-test questionnaire for tetralogy of Fallot including the objective and subjective questionnaire.
Additional file 5: S5.
The post-test questionnaire for ventricular septal defect including the objective and subjective questionnaire.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Karsenty, C., Guitarte, A., Dulac, Y. et al. The usefulness of 3D printed heart models for medical student education in congenital heart disease. BMC Med Educ 21, 480 (2021). https://doi.org/10.1186/s12909-021-02917-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12909-021-02917-z