Abstract
Background
In Ethiopia, the leaves of Syzygium guineense have been found useful for the prevention and cure of malaria, and demonstrated antiplasmodial activity in vitro. Nevertheless, no scientific study has been conducted to confirm its antimalarial activity in vivo. Therefore, the objective of the study was to evaluate the antimalarial effect of Syzygium guineense leaf extract in mice.
Methods
Inoculation of the study mice was carried out by using the malaria parasite, Plasmodium berghei. The plant extract was prepared at 200, 400 and 600 mg/kg. Chloroquine and distilled water was administered to the positive and negative control groups respectively. Parameters like parasitaemia, survival time and body weight were determined following standard tests (4-day suppressive, Rane’s and repository tests).
Results
Syzygium guineense crude leaf extract displayed considerable (p < 0.05) parasite suppression at doses of 600 and 400 mg/kg in a 4-day suppressive test with chemosuppressive value of 59.39 and 49.09% respectively. S. guineense crude leaf extract also showed dose-dependent schizontocidal activity in both the repository and curative tests. The extract also prevented body weight loss and prolonged survival date of mice significantly (P < 0.05) at the highest dose employed in the study. Qualitative chemical assay for S. guineense methanolic leaf extract revealed that the plant is endowed with different plant secondary metabolites exemplified by terpenoids, alkaloids, triterpenes, flavonoids, anthraquinones, tannins, glycosides, saponins and phenols.
Conclusion
Syzygium guineense leaf extract possess antimalarial activity in mice. The test substance was found to be safe with no observable signs of toxicity in the study mice. The results of the present work confirmed the in vitro antiplasmodial finding and traditional claims in vivo in mice. Therefore, Syzygium guineense could be regarded as a potential source to develop safe, effective and affordable antimalarial agent.
Similar content being viewed by others
Background
Regardless of intensive efforts to get rid of malaria, the infection remains to be among the top health problems in Ethiopia [1]. Malaria, though widespread in tropical Africa, the healthcare coverage of the continent in general and the rural areas in particular is still inadequate. People dwelling in this area have time tested experiences regarding medicinal plants. As a result, people in the countryside, wholly or partially, use medicinal plants for prevention as well as cure of various disease conditions especially malaria. People give predilection to use herbal remedies due to the fact that traditional healers are easily accessible and generally respected by the community. This could be also a result of inadequate knowledge of the rural people regarding the modern healthcare institutions coupled with their belief in herbal remedies as being more affordable, safer and effective compared to the modern medicine [1–3].
In Ethiopia, malaria is the major cause of morbidity and mortality, with approximately 5–10 million cases per year. The disease causes not less than 60,000 deaths every year and accounts for about 17% of outpatient visits to health organizations, 8% of admissions and 29% of inpatient deaths [4, 5]. Furthermore, P. falciparum malaria parasite has recently developed resistance to almost all of the currently available medications used to treat the infection [6–8].
Syzygium guineense is a large evergreen flowering plant (family Myrtaceae). The plant is found widespread in the regions of Australia, Asia and Africa including Ethiopia [9].
Historically, antimalarial drug therapy is closely associated with traditionally used medicinal plants contributing like quinine; the first plant derived natural product (identified from Cinchona bark) is still employed in antimalarial therapy. Phytochemical compounds such as alkaloids, also found in the leaves of S. guineense, are commonly implicated for their antiplasmodial activity of many plants including Cinchona tree from which quinine, the first antimalarial drug, was isolated [10, 11]. In Ethiopia, leaf decoction of S. guineense is being used traditionally to treat malaria [12, 13].
Other secondary metabolites present in S. guineense implicated for their antimalarial activity include: Terpenoids [14–16], Phenols [17], Anthraquinones [18, 19], and Flavonoids [20]. S. guineense leaves are also recognized by their immunomodulatory [21], anti-oxidant, and anti-inflammatory properties [22].
Furthermore; the members of the genus Syzygium are well recognized for their antimicrobial, anti-inflammatory, antimalarial and larvicidal effect in mosquito vector [23]. The family Myrtaceae [24] and different species of Syzygium have shown promising antimalarial activity in vitro [25].
Despite the plant being endowed with the aforementioned secondary metabolites known for their antimalarial activity and in vitro claims, information regarding its in vivo antimalarial efficacy is extremely lacking. Therefore, this study was aimed in evaluating the traditional claim as well as reported in vitro efficacy of S. guineense in vivo in mice.
Methods
Collection and identification of the plant material
The fresh leaves of S. guineense (Wild) D.C. were collected near the town of Gondar in North Gondar administrative zone, Ethiopia, in February 2015. S. guineense as a potential medicinal plant was selected depending on the evidence provided by herbalists in Northwest Ethiopia. The antimalarial plant S. guineense was kindly authenticated by a taxonomist at the Ethiopian National Herbarium, Addis Ababa University and the Voucher specimen (voucher number ST02/2015) deposited for future reference.
Experimental animals
Albino mice of either sex (25–30 g) were used for this study. All the study mice were sustained under standard environment (Temperature of 22 ± 3 °C, Relative Humidity of 50–70% and 12 h light/dark cycle), with food and water ad libitum. Mice were allowed to adapt themselves to the experimental environment for 7 days prior to the initiation of the actual experiment. All the experimental protocols were evaluated and approved by the institutional review board of the university.
Parasite isolate
For the in vivo evaluation of S. guineense leaf extract, chloroquine sensitive P. berghei ANKA strain was used. The malaria parasite, P. berghei, was kindly provided by Ethiopian Health and Nutrition Research Institute (EHNRI) and was sustained by serial passage of blood from infected mice to non-infected ones on weekly basis.
Extraction procedure
Fresh matured leaves of S. guineense (Wild) D.C. were collected, washed, air dried under shade and grinded using mortar and pestle to coarse powder. A total of 400 g powder was extracted by maceration for 72 h, filtered with wattman filter paper (150 mm size), and the residue extracted further two times by maceration with the same duration (72 h each). Finally, the combined filtrate was kept in an oven (40 °C) for concentration. Further drying process was carried out in a desiccator for removal of water. Finally, the dried extract was maintained at −4 °C till the beginning of the actual experiment.
Phytochemical analysis of the crude extract
A preliminary phytochemical study of S. guineense leaf extract was performed using standard procedures [12, 13].
Parasite inoculation
Blood were collected from the tail veins of previously P. berghei infected donor mouse having a parasite load of 30–37% to infect the mice. Subsequently, the blood was diluted in normal saline (0.9%) so that the final suspension contained 107 infected red blood cells in each 0.2 ml of the preparation. Accordingly, mice were inoculated with 107 P. berghei parasitized RBCs via the intraperitoneal route [26–28].
Acute toxicity study
The safety of the extract when taken acutely was performed according to the OECD guideline 425. A fixed dose of 2000 mg/kg body weight of S. guineense crude leaf extract was administered to a single mouse via the oral route by gavage. Before the administration of the test substance, mice were prohibited from free access to food for 3 h. Similarly, food was with held for 1 h after extract administration. Following administration of the crude extract, mice were closely observed for an hour, occasionally for 4 h in a day (24 h) for a total of 14 days. Mice were closely monitored for the occurrence of any behavioral abnormalities indicated by decreased appetite, tremor, convulsion, increased saliva secretion, lacrimation, diarrhea, death as well as other manifestations of toxicity. In view of the fact that no death of the study mice at the test dose of 2000 mg/kg were observed, additionally 4 mice were sequentially dosed the same dose of the extract [29].
Test on early malaria infection
The suppressive activity of S. quineense crude leaf extract was evaluated according to the Peter’s suppressive assay (4- day suppressive test). The Peter’s test is widely used in screening of plant extracts for their in vivo antiplasmodial activity via the use of two important parameters (blood parasitemia and mean survival time of mice) [26, 27, 30]. Mice were infected with 1 × 107 P.berghei and kept in the same compartment before being assigned in 5 groups.
Following the infection, mice were arbitrarily distributed in to 3 extract treated & 2 control groups (each group containing 5 mice in a cage).
The crude leaf extract was administered at 200, 400 and 600 mg/kg and chloroquine 10 mg/kg body weight via the oral route once per day dose with gavage.
After three hours of parasite inoculation, mice were treated daily for 4 consecutive days. After treatment is completed (4th day), thin blood smears were made by drawing blood from the tail of each mouse. Accordingly, each smear was fixed in methanol, and giemsa (10%) stained for subsequent determination of parasitaemia with a microscope (via counting 4 fields of about 100 RBCs in each field).
The difference between the mean value of the negative control group and those of the extract treated groups were determined to evaluate the activity of S. quineense extract in mice [28, 29, 31, 32].
Monitoring of body weight changes
Body weight of each mouse was recorded before infection (day 0) and on (day 4) using sensitive digital balance.
Monitoring of mean survival time
Mortality of the study mice was closely observed daily and the number of days from the time of infection with P. berghei up to the incidence of death was recorded for every mouse in both the treatment and control groups during the follow up period. Mean Survival Time (MST) of all mice were determined using the formula [28]:
Evaluation of the extract on residual P. berghei infection
The residual infection protocol described by Peter [32] was employed to evaluate the prophylactic activity of the extract. Consequently, either sex of 25 mice were weighed and randomized into five groups of five mice each. Group I received 0.5 ml distilled water per kg body weight. Groups II, III and IV received 200, 400 & 600 mg/kg body weight of S. guineense extract orally respectively. The standard drug, (10 mg/kg/day chloroquine), was administered to Group V. Treatment continued for three successive days (from D0 - D2). On the 4th day (D3), mice were infected with 1 × 107 P. berghei infected red blood cells. Finally, after 72 h, parasitaemia was determined via blood smear.
Evaluation on established infection (Rane’s test)
The curative potential of S. guineense was evaluated by employing the method described by Ryley and Peters (1970). On the 1st day (day 0), mice were injected intraperitoneally with a standard inoculum of 1 × 107 P. berghei infected RBCs. Seventy-two hours later, following confirmation of parasitaemia, the mice were randomly assigned into two control and three test groups, each group containing five mice per cage. The test groups were sequentially treated with the prepared leaf extract of S. guineense (200, 400 and 600 mg/kg/day). The standard drug (10 mg/kg/day chloroquine) and vehicle (0.5 ml distilled water) was administered to the positive and negative control groups respectively. Treatment continued for 5 consecutive days at a single dose per day. Geimsa stained (10%) thin blood film (prepared by drawing blood from the tail vein of each mouse) was examined microscopically to determine the percentage of parasitaemia.
Statistical analysis
Results of the study were presented as mean ± SEM. Data was analyzed using SPSS version 20. Statistical significance was determined by One-way ANOVA coupled to Tukey’s HSD technique to compare result between doses and among treatment and control groups. For all the data obtained, the result was considered significant at 95% confidence level and P-value < 0.05.
Results
Phytochemical analysis
Preliminary phytochemical study of the extract of S. guineense (Wild) DC leaves revealed the presence/absence of plant secondary metabolites shown in Table 1.
Acute toxicity
S. guineense leaf extract didn’t cause death of the study mice at the limit dose of 2 g/kg. Similarly, both physical and behavioral observations of the study mice also did not point out any visible signs of toxicity. This indicates that the LD50 of the extract is above 2 g/kg.
In vivo antimalarial activity tests
Test on early malaria infection (the 4-day suppressive test)
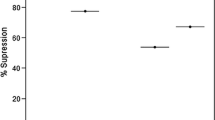
Leaf extract of S. guineense reduced parasitaemia level in the study mice dose-dependently at all tested doses. The crude extract, at the highest doses employed, (400 and 600 mg/kg per day) exhibited 49.09 and 59.39% chemosuppression respectively. Average parasite load at these doses were much lower (p < 0.05) than that observed in the untreated mice. The extract was also able to suppress parasitaemia (26.67%) at 200 mg/kg). The complete data is presented in Table 2.
The comparison analysis indicated that the extract prevented weight loss significantly (p < 0.05) at all tested doses compared to distilled water treated control group. The increase in body weight was found to be highest at the largest dose used in the study (9.82%) (Table 3).
The extract prolonged mean survival period of the study mice (from 8 ± 1.73 to 10.8 ± 2.59 days). The corresponding vehicle treated mice survived only for 7 ± 0.70 days. Though much lower than the chloroquine-treated group (which lived for 28 days), the extract at 600 mg/kg was capable of significantly increasing (P < 0.05) survival date of mice (Table 4).
Test on prophylactic activity (repository test)
S. guineense extract exhibited a dose-dependent reduction in parasitaemia level in mice. At the highest dose used in the study (600 mg/kg body weight), the crude extract demonstrated a considerable (p < 0.05) antiplasmodial activity compared to the vehicle treated control group. Average chemosuppression at this dose was 48.57% which is lower than that exhibited by the standard drug (72.85%).
Test on established malaria infection (curative test)
S.guineense leaf exerted a considerable (P < 0.05) curative effect at 600 and 400 mg/kg. Mean parasite counts at these doses were 6 ± 0.44 and 13 ± 0.72 respectively. The extract at 200 mg/kg was also capable of decreasing parasite load to 17 ± 0.66 while, the mean parasite count in the untreated control group was 43 ± 0.76 (Table 5). Parasite load in extract treated mice was lower than that of the untreated mice indicating its pharmacological effect against established malaria infection. Nevertheless, this noticeable antiplasmodial effect of S. guineense was not comparable to the standard drug that reduced mean parasite density to 2 ± 0.37.
S. guineense leaf extract treated mice lived for 15 ± 0.44, 13 ± 0.14, and 8 ± 0.72 days at 600, 400 and 200 mg/kg/day dose respectively. On the contrary, mice receiving vehicle lived for 7 ± 0.22 days only. Chloroquine treated mice displayed the longest mean survival time (28 ± 0.56 days) which is significantly (P < 0.05) high compared to mice in both extract and distilled water treated groups.
Discussion
In vivo screening of medicinal plants for their potential antimalarial activity is usually performed with a rodent malaria parasite, particularly P. berghei, which has been used extensively in the discovery and development of several conventional antimalarial drugs exemplified by halofantrine, chloroquine, mefloquine and more recently artemisinin derivatives [27].
Therefore, in the current study, antimalarial activity of S.guineense was evaluated using P. berghei, which produces disease similar to those of human plasmodium infections, for the prediction of treatment outcomes [31]. A standard antimalarial drug suppresses parasitemia significantly [33] which is in agreement with the effect of chloroquine in this study that achieved 97.57% suppression of the growth of P. berghei (the complete data is available in Table 2).
The 4-day suppressive assay is a standard test universally used for antimalarial screening, and the determination of percent inhibition of parasite growth is regarded as the most dependable parameter in antimalarial drug discovery [34]. In the 4-day suppressive test on P. berghei infected mice, S. guineense crude leaf extract exhibited dose-dependent activity at different doses employed in the study. The result is similar to other in vivo studies [33, 35–38]. A significant (P < 0.05) parasite suppression was observed at doses of 600 and 400 mg/kg compared to the negative control group. It is important to note that the crude extract at the lowest dose (200 mg/kg) also exhibited parasite suppression though not statistically different from the control group indicating that the extract is endowed with antiplasmodial activity and supports its traditional claim as antimalarial herbal remedy in Africa [23, 24].
The methanolic leaf extract of S.guineense also displayed antimalarial effect against residual infection of the parasite at all tested doses. The result of the study clearly indicated dose-dependent parasite suppression of S.guineense leaf extract even though not comparable with the chloroquine treated control group which suppressed 72.85% (Table 6). The low activity of the extract observed in the repository test when compared to the effect against early infection may be due to rapid clearance of the active agent by the liver.
The crude extract was also capable of increasing mean survival time (MST) of the study mice indicating that it suppressed the growth of P. berghei. Moreover; the extract was capable of reducing the overall pathological effects of this parasite in mice. It is also good to note that the survival time of the study mice receiving 600 mg/kg of the extract was significantly (p < 0.05) high as compared to those groups receiving 200 and 400 mg/kg as well as distilled water treated control mice. This may suggest a dose-dependent schizontocidal activity of the extract.
Body weight loss is one feature of rodent malaria infection. The extract not only prevented body weight loss in mice but also increased the weight of the study mice (Table 3). This indicates that other than direct parasiticidal effects, the plant may possess other pharmacologic benefits to the host: acting as analgesics, antipyretics, immune stimulators or the extract may contain appetite enhancing agent (s) [39].
Phytochemical screening of S. guineense leaf extract revealed the presence of alkaloids, terpenoids, anthraquinones, flavonoids, tannins, saponins, glycosides, triterpenes and phenols (Table 1). Alkaloids, also present in this plant, are generally known for their antiplasmodial activity of many plants including Cinchona bark from which quinine was isolated [21, 22]. Terpenoids have been implicated for their antiprotozoal and antimalarial activities in many pharmacological studies [21, 22]. S. guineense leaf also contain phenols known for their anti-oxidant and other diverse physiological properties: anti-carcinogenic, anti-inflammatory and anti-parasitic activities [10]. Anthraquinones, also found in this plant, is identified as active antimalarial compound [11, 14]. Flavonoids, also present in S. guineense leaf extract, are other potential antimalarial compounds believed to act by inhibiting the fatty acid biosynthesis (FAS II) of the malaria parasite [14]. S. guineense leaf possesses potential immunomodulatory [21], anti-oxidant [15, 40], anti-inflammatory and analgesic effects [22, 41]. S. guineense extract may also act via another unknown mechanism that may contribute for its antiplasmodial effect.
Therefore, these observed schizontocidal activities of S. guineense in mice could be attributed to the diverse classes of phytochemical compounds present in the leaf. On the other hand, the plant may be endowed with undiscovered (unknown) antimalarial compound (s) that could be used for the production of relatively safe, effective and affordable antimalarial agent.
Conclusion
The present work has confirmed the efficacy of S. guineense supporting its traditional use against malaria. The results also indicated that the test substances have wide safety of margin making it potential source for the development of safer and cost-effective alternative drug in the treatment and cure of malaria.
Abbreviations
- ANOVA:
-
Analysis of variance
- DW:
-
Distilled water
- EHNRI:
-
Ethiopian Health and Nutrition Research Institute
- FAS:
-
Fatty acid biosynthesis
- LD50 :
-
Lethal dose 50 (Median lethal dose)
- MST:
-
Mean survival time
- ns:
-
Not significant
- OECD:
-
Organisation for Economic Co-operation and Development
- RBC:
-
Red blood cell
- Rx :
-
Treatment
- SEM:
-
Standard error of the mean
References
Dharani N, Rukunga G, Yenesew A, Mbora A, Mwaura L, Jamnadass R. Common antimalarial trees and shrubs of East Africa, a practical guide to propagation, domestication, germplasm, management and conservation of species. Nairobi: World Agroforestry Centre; 2008.
Harani N, Rukunga G, Yenesew A, Mbora A, Mwaura L, Dawson I, Jamnadass R. Common antimalarial trees and shrubs of East Africa: a description of species and a guide to cultivation and conservation through use. Nairobi: the World Agro forestry Centre (ICRAF); 2010.
Adera T. Beliefs and traditional treatment of malaria in Kishe settlement area, Southwest Ethiopia. Ethiop Med J. 2003;41:25–34.
Mohammed T, Erko B, Giday M. Evaluation of antimalarial activity of leaves of Acokanthera schimperi and Croton macrostachyus against Plasmodium berghei in Swiss albino mice. BMC Complement Altern Med. 2014;14:314–24.
Federal Ministry of Health Policy Planning Directorate. Health and health related indicators 2011. Addis Ababa: Branna Press; 2013.
Wells N, Alonso L, Gutteridge E. New medicines to improve control and contribute to the eradication of malaria. Nat Rev. 2009;8:879–92.
Basco L, Kobo V, Ngane M, Ndounga T, Metoh P, Ringwald G, Soula A. Therapeutic efficacy of sulfadoxine-pyrimethamine, amodiaquine and the sulfadoxine-pyrimethamine-amodiaquine combination against uncomplicated Plasmodium falciparum Malaria in young children in Cameroon. Bull World Health Organ. 2002;80:538–45.
Peter B. Drug resistance in Malaria. United States of America: Malaria Epidemiology Branch Centers for Disease Control and Prevention, WHO; 2001.
Teketay D, Tesfaye G, Fetene M. Regeneration of fourteen tree species in Harenna forest, southeastern Ethiopia. Flora. 2002;197:461–74.
Saxena S, Pant N, Jain D, Bhakuni R. Antimalarial agents from plant sources. Curr Sci. 2003;85:1314–29.
Frederich M, Tits M, Angenot L. Potential antimalarial activity of indole alkaloids. Trans R Soc Trop Med Hyg. 2008;102:11–9.
Fisseha M, Talemos S, Abreham A. An ethnobotanical study of medicinal plants in amaro woreda, Ethiopia. Ethnobot Res Appl. 2014;12:341–54.
Kasali F, Mahano A, Kadima N, Mpiana P, Ngbolua K, Tshibangu T. Ethnopharmacological survey of medicinal plants used against malaria in Butembo City (D. R. Congo). J Adv Bot Zool. 2012;1:2348–7313.
Bero J, Frederich M, Quetin-Leclercq J. Antimalarial compounds isolated from plants used in traditional medicine. J Pharm Pharmacol. 2009;61:1401–33.
Batista R, Silva A, Oliveira A. Plant derived antimalarial agents: New leads and efficient phytomedicines. Part two Non alkaloidal natural products. Molecules. 2009;14:3037–2.
Kuiate JR, Mouokeu S, Wabo HK, Tane P. Antidermatophytic triterpenoids from Syzygium jambos (L.) Alston (Myrtaceae). Phytother Res. 2007;21(2):149–52.
Ma Q, Kinner K. Chemoprevention by phenolic antioxidants. J Biol Chem. 2002;277:2477–84.
Winter R, Cornell K, Johnson L, Riscoe M. Hydroxy-anthraquinones as antimalarial agents. Bio Org Med Chem Agents. 1995;5:1927–32.
Mahajan S, Kamath V, Ghatpande S. Synergistic antimalarial activity of ketones with rufigallol and vitamin C. Parasitology. 2005;131:459–66.
Kang F, Onguene P, Lifongo A, Ndom J, Sippl W, Mbaze L. The potential of antimalarial compounds derived from African medicinal plants, part two: A Pharmacological evaluation of non-alkaloids and non- terpenoids. Malar J. 2014;13:1–20.
Ghildyal P, Gronhuag T, Rusten A, Skogsurd M. Chemical composition and immunological activities of polysaccharides isolated from the Malian medicinal plant Syzygium guineense. J Pharmacogn Phytother. 2010;2:76–85.
Otimenyin O, Umar M. Anti-inflamatory and analgesic activities of the ethanolic extract of the leaf of Syzygium guineense in rats and mice. IOSR J Pharm. 2012;2:33–6.
Sha-Tshibey D. Phytochemical & anti-drepanocytosis studies of Cajanus cajan, Callistemon viminalis, Melaleuca bracteata var. revolution gold and Syzygium guineense. 2010. Available at: https://researchspace.ukzn.ac.za/bitstream/handle/10413/8113/Tshibangu_Damien%20S_2010.pdf?sequence=1&isAllowed=y. (Accessed 29 Jan 2015).
Titanji V, Zofou D, Ngemenya M. The anti-malarial potential of medicinal plants used for the treatment of malaria in Cameroon folk medicine. Afr J Tradit Complement Altern Med. 2008;5:302–21.
Simoes-pires C, Vargas S, Marston A, Loset JR, Paulo MQ, Matheeusen A, Maes L. Ellagic acid derivatives from Syzygium cumini stem bark: Investigation of their antiplasmodial activity. Nat Prod Commun. 2009;4:1371–6.
Fidock A, Rosenthal P, Brun S, Nwaka S. Antimalarial drug discovery: Efficacy models for compound screening. Nat Rev Drug Discov. 2004;3:509–20.
Kalra B, Chawla S, Gupta P, Valecha N. Screening of antimalarial drugs: an overview. Indian J Pharm. 2006;38:5–12.
Christensen SB, Kharazmi A. Antimalarial natural products. In: Tringali C, editor. Bioactive compounds from natural sources: isolation, characterisation and biological properties. New York: Taylor & Francis; 2001. p. 387–404.
OECD, Test No. 425: Acute Oral Toxicity: Up-and-Down Procedure. Paris: OECD Publishing; 2008. doi: http://dx.doi.org/10.1787/9789264071049-en.
National Research Council. Guide for the care and use of laboratory animals. Washington: The National Academic Press; 1996.
Mishra S, Sharma H, Mishra R, Gupta S. A review on antimalarial drug discovery and its screening method. World J Pharm and Pharm Sci. 2014;8:1288–304.
Peters W. Drug resistance in plasmodium berghei vincke and lips, 1948; I. Chloroquine resistance. Exp Parasitol. 1965;17:80–9.
Birhanu Z, Wuhab MA, Abula T. Antimalarial activity of calpurnia aurea hydroalcoholic leaf extract in mice infected with Plasmodium berghei. JPHOL. 2015;2:73–9.
Mojab F. Antimalarial natural products: a review. Avicenna J Phytomed. 2012;2:52–62.
Dikasso D, Makonnen E, Debella A, et al. In vivo antimalarial activity of hydroalcoholic extracts from asparagus africanus Lam. In mice infected with plasmodium berghei. Ethiop J Health Dev. 2006;20:112–8.
Kassa M, Mohana R, Hunde A. Antimalarial activity of bersama abyssinica against plasmodium falciparum. Ethiop Pharm J. 1996;14:16–21.
Deressa T, Mekonnen Y, Animut A. In vivo antimalarial activities of clerodendrum myricoides, dodoneaangustifolia and aloedebrana against plasmodium berghei. Ethiop J Health Dev. 2010;24:25–9.
Mengiste B, Makonnen E, Urga K. In vivo antimalarial activity of dodonaea angustifolia seed extracts against plasmodium berghei in mice model. Ethiopian J Sci. 2012;4:47–63.
Oluwakanyinsona A, Adeniyi Y, Babayi H, Angela C, Anagbogu RA, Agbakwuru VA. Anti-malarial activity of ethanolic stem bark extracts of faidherbia albida (Del.) in mice. Sch Res Libr. 2010;5:261–8.
Pieme C, Negoupayo J, Nkoulou H, Moukete M, Nono B, Moor V, Minkande J, Ngogang J. Syzygium guineense extracts show antioxidant activities and beneficial activities on oxidative stress induced by ferric chloride in the liver homogenate. Antioxid. 2014;3:618–35.
Kiseko K, Hiroyuki M, Syun-ichi F, Ryuiichi F, Tomotaka K, Seiji M. Anti-malarial activity of leaf - extract of Hydrangea macrophyla, a common Japanese plant. Acta Med Okayama. 2010;54:227–32.
Acknowledgement
We acknowledge University of Gondar for allowing material assistance for the study. Ethiopian Health and Nutrition Research Institute is also greatly acknowledged for providing the malaria parasite.
Availability of data and materials
The data sets during and/or analyzed during the current study available from the corresponding author on reasonable request.
Authors’ contribution
SA: Collected the plant material, prepared the extract, performed phytochemical screening test, antiplasmodial assays, data analysis and drafted the manuscript ZB: Coordinated the overall work, assisted the antimalarial assay, performed acute toxicity study, interpreted the data and prepared the manuscript. Finally, both authors read and approved the final manuscript.
Competing interest
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Ethical clearance to conduct the experiment on mice was obtained from institutional review board of University of Gondar.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Tadesse, S.A., Wubneh, Z.B. Antimalarial activity of Syzygium guineense during early and established Plasmodium infection in rodent models. BMC Complement Altern Med 17, 21 (2017). https://doi.org/10.1186/s12906-016-1538-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12906-016-1538-6