Abstract
Background
Breast cancer is the most frequently diagnosed cancer in women worldwide. The objective of this study was to identify factors associated with late diagnosis of breast cancer in Togolese women.
Methods
We conducted a prospective cross-sectional study with descriptive and analytical purposes on cases of breast cancer in women in 2021, in Togo. The patients included in this study were women followed in the gynecology department for stages III and IV breast cancer.
Results
We included 62 cases of breast cancer. The average age of the patients was 38.6 ± 12.5 years with extremes of 17 and 76 years. The breast nodule was the most common reason for consultation in 75.8% of cases. The histological types diagnosed were invasive carcinoma of non-specific type (58; 93.55%), mucinous carcinoma (3; 4.84%) and lobular carcinoma (1; 1.61%). For the stage of the cancer, 43 patients were stage III (69.4%) and 19 stage IV (30.6%).
In multivariate analysis, the factors associated with late diagnosis of breast cancer were: fear of diagnosis (aOR = 1.29; p = 0.0014), long delay in diagnosis (aOR = 2.62; p = 0.0001) and failure to perform breast self-examination (aOR = 1.68; p = 0.0022).
Conclusion
The fear of the diagnosis, the absence of self-examination of the breasts and the use of traditional treatment and self-medication in first intention constituted the essential factors of the late diagnosis of breast cancer. Strategies should be put in place at the national level to impact on these factors for an early diagnosis of breast cancer.
Similar content being viewed by others
Background
Breast cancer is the most common cancer worldwide, ahead of lung cancer with 2,261,419 new cases in 2020, or 11.7% of all cancer cases and 684,996 deaths, or 6.9% [1, 2]. During the same year, Africa recorded 1,109,209 cases including 49,339 cases in West Africa for 25,626 deaths [2]. Its incidence and mortality rates are expected to increase significantly over the next few years [3, 4]. Breast cancer incidence has increased significantly over the past two decades to 2.0% per year and is expected to reach over 19.3 million women by 2025, with the majority originating from sub-Saharan Africa [5]. In developing countries including Togo, breast cancer is a major public health issue, it is the leading cause of death among women with 324,000 deaths, which represents 14.3% of all deaths [6,7,8].
In Togo, a study carried out in 2016 reveals that breast cancer is the most frequently diagnosed in women with a prevalence of 21.2% of cancers in women and 10% of all cancers diagnosed in the country [9]. More recent data in 2020 show that this cancer is diagnosed at advanced stage III using the Nottingham classification (55.10%) [10]. In addition, more than half of the patients (52.1%) had T3-T4 tumors and the histoprognostic evaluation showed that grade 2 tumors were predominant (51.3%) followed by grade 3 (42.7%) [11,12,13]. Given the late diagnosis of breast cancer, the narrowness of the technical platform and the low standard of living of the population, we initiated this study, the aim of which was to identify factors associated with the late diagnosis of breast cancer in women in Togo.
Methods
We report the results of a prospective cross-sectional study with descriptive and analytical purposes on cases of breast cancer in women admited and followed up in the gynecology department and confirmed histologically at the Laboratory of Pathological Anatomy and Cytology of the CHU Sylvanus Olympia in 2021. Togo is a country of 56,600 Km2, with an estimated population of 7,200,000 inhabitants, located between Ghana in the west, Benin in the east and Burkina faso in th north. The data were collected during an interview during the consultation with a histopathological confirmation of breast cancer at the Laboratory of Pathological Anatomy and Cytology from the registers of this laboratory. The patients included in this study were women followed in the gynecology department for stages III and IV breast cancer.
The parameters studied were demographic data (age, profession, parity, religious denomination, level of education and marital status); clinical date (reason for consultation, clinical size and topography); anatomopathological data (histological type, histoprognostic grade, pTNM stage as well as data relating to the diagnostic delay (accessibility to appropriate care structures, consultation time, fear of diagnosis, caregiver profile, delay in carrying out histology, the practice of early detection methods) [14]. About the profession, the informal sector was all women who carry out an activity of income but not declared and a civil servant when the work is formally declared.
A univariate and multivariate logistic regression was carried out in order to find the factors associated with the long delay in consultation. The independent variable was the long consultation delay coded 1 if yes and 0 if not. The long consultation period is mentioned if the period between the first symptom and the first consultation is greater than 6 months [4]. When the independent variable was statistically associated with the dependent variable during the univariate analysis with a degree of significance p ˂0.20, it was introduced into the initial model. The top-down step-by-step procedure was used for final model selection. It consisted of including the variables chosen in the initial model. Univariate analysis was used to estimate the odds ratio (OR) and its 95% confidence interval. The multivariate analysis made it possible to estimate the adjusted odds ratio (RCa) and its 95% confidence interval for each variable retained.
Results
Socio-demographic characteristics of patients
Table 1 summarizes the socio-demographic characteristics of the patients. We collected 62 cases of breast cancer. The average age of the patients was 38.6 ± 12.5 years with extremes of 17 and 76 years. All social strata were represented but the informal sector was the majority with 52 cases (83.9%), followed by civil servants with a percentage of 11.3%. Only civil servants had health coverage. According to the level of education, the patients were mostly college level. Married women represented 54.8%, followed by single women (25.8%). Patients who had children represented 47 cases (75.8) and 34 of them had at least 3 children.
Clinical and mammographic characteristics of patients
The breast nodule was the most common reason for consultation with 75.8% followed by breast swelling with 30.6%. The other reasons for consultation were mastodynia (29%), nipple discharge (11.3%), breast ulceration (11.3%) and abscess (1.6%) (Fig. 1). The left breast was the most affected in most women in our study with a percentage of 51.6%. The mean tumor size on mamography was 36.6 ± 50.1 mm with extremes of 17 mm and 240 mm (Table 2).
Histopathological data
These were mastectomy pieces with axillary dissection. On section, the tumor presented a size varying between 3 and 11 cm long axis, with hemorrhagic and necrotic changes.The histological types diagnosed were invasive carcinoma of non-specific type (58; 93.55%), mucinous carcinoma (3; 4.84%) and lobular carcinoma (1; 1.61%). For the stage of the cancer, 43 patients were stage III (69.4%) and 19 stage IV (30.6%). The Nottingham histoprognostic grade was specified in 56 patients including 45 grade II, 7 grade I and 4 grade III.
Factors studied in the context of delayed diagnosis
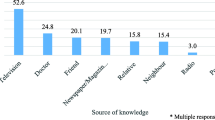
Thirty-seven patients (59.7%) claimed to have traveled less than 10 km to get to the care structure, 17 patients between 10 and 20 km and 8 patients more than 20 km. Breast self-examination was practiced by only 15 (24.2%) patients. The average consultation time was 23.6 ± 46.1 weeks with the extremes of one week and 288 weeks. The first consultation was with a doctor in 45 cases, a traditional healer in 9 cases. Eight patients had taken self-medication before the medical consultation. The average time taken to honor a histological examination was 5.7 ± 9.3 months with extremes of one day to 49.7 months. The average time taken from the first symptoms to the diagnosis of breast cancer was 6.3 ± 10.2 months with the extremes of 8 days and 50.07 months.
In univariate analysis, the factors associated with late diagnosis of breast cancer were: distance from health care structures with (p = 0.0037), fear of diagnosis (p = 0.00001), type of first consultation (p = 0.0026) andabsence of practice of self-examination of the breasts (p = 0.0012) (Table 3). In multivariate analysis, the factors associated with late diagnosis of breast cancer were: fear of diagnosis (aOR = 1.29; p = 0.0014), long delay in diagnosis (aOR = 2.62; p = 0.0001) and failure to perform breast self-examination (aOR = 1.68; p = 0.0022) (Table 4).
Discussion
Late diagnosis of breast cancer remains a topical problem in our practice environment. In our series, as in most African publications, the diagnostic delay was particularly long, in our series the average delay is 6.3 months [15,16,17]. The reasons for the late diagnosis were the remoteness of health facilities, the fear of the diagnosis, the type of first consultation, the lack of practice of self-examination of the breasts. Socio-cultural habits represented by first-line use of traditional medicine and the problem of staff qualification were also reasons for late diagnosis of breast cancer [11, 13]. The training of nursing staff, especially general practitioners, nurses and midwives, should be able to limit the risk of diagnostic errors insofar as breast cancer often poses a problem of differential diagnosis with benign mastopathies [18,19,20,21].
The first factor obtained was fear of the diagnosis (p-value = 0.0014; RCa = 1.29; 95% CI [1.36–2.58]). Half of these patients had consulted after a period of six months against 43.3% of patients who had no phobia related to this condition. Thus, for a woman, being afraid of being diagnosed with breast cancer would increase the risk of diagnosing it at the late stage by 1.29% [2, 6]. The patient's psychic experience is heavily affected, with the psychological disorders that usually accompany the announcement of any cancer, passing through the acceptance of the disease until mourning, such as: depression, anxiety and fear of death, will be grafted other disorders, which can be as reprimanding as the disease itself [22].
The second factor was the type of consultation opted for the detection of symptoms (with a p-value = 0.0001). Some patients opted for traditional therapy, 77.8% had a long delay in diagnosis (RCa = 2.62; 95% CI [2.01–4.7]). Similarly, half of those who had chosen the self-medication route had a long diagnostic delay (RCa = 1.29; 95% CI [1.07–2.78]). This means that moving towards traditional treatment would increase the chance of being diagnosed with breast cancer at an already advanced stage by 2.62%, while self-medication would increase it by 1.29%. The circuit of patients suffering from breast cancer is often complex in Africa. Most turn to traditional healers who waste patients' time both in diagnosis and in therapeutic management. This would partly explain the fact that cancer patients often arrive late in health structures and often with complications or even metastases [23]. Beliefs and especially ignorance would be the parameters that direct patients to these traditional healers who unfortunately do not know their limits in the management of serious and chronic pathologies such as cancer [24].
The three factor was failure to perform breast self-examination. Al-though self-examination is the most commonly used early detection technique,evidence of its effectiveness is discussed [11, 25]. This technique can lead toover detection of nodules leading to unnecessary visits to the doctor and ex-penses related to the diagnosis, which is not desirable in the context of development countries where health facilities and resources are limited [26]. However, al-though current evidence does not support self-examination as a breast cancerscreening approach, teaching breast self-examination at the individual level incountries where most women with breast cancer advanced disease may improveawareness of breast cancer and lead to an earlier stage of diagnosis [27, 28]. Clinicalbreast examination has the advantage of being a relatively simple and inexpen-sive technique for the early detection of breast tumors [10]. It should be doneadequately by trained health workers [28, 29]. The role of self-examination andclinical breast examination is important in areas where mammography may notbe available for financial and accessibility reasons [29]. In addition, statistics in-dicate that 90% of breast nodules are discovered by women themselves [29]. As for the students’ knowledge of mammography as a means of screening forbreast cancer, 75.3% were aware of it. Mammographic screening proves to be beneficial when it is car-ried out in an organized and regular manner in the form of a national publichealth policy or when the per capita income of the population allows it to absorbmost of the costs [30]. Mammography screening is financially and technically difficult to implement and maintain, requiring high-quality machines, well-trainedradiologists and technicians, and investment in pathology and treatment facili-ties [31]. Therefore, organized screening is difficult in developing countries. Socioeconomic dependence and late diagnosis reflect higher rates of breast can-cer morbidity and mortality in developing countries [17, 29,30,31]. The impact of mam-mography screening may be more beneficial in developing countries than whathas been observed in developed countries [17].
A percentage of 53.2% of this group had consulted after six months (RCa = 1.68; 95% CI [1.47–2.27]), which means that a woman not practicing breast self-examination would have a 1.68% chance of being diagnosed with late-stage breast cancer [22, 32]. The psychic experience of the patient is heavily affected. The psychological disorders that usually accompany any announcement of cancer, ranging from acceptance of the disease to mourning; such as depression, anxiety and fear of death [1, 18]. Other disorders will be added, in particular the devaluation or loss of self-esteem, isolation, disorders of body image and/or sexual identity, which can be as reprimanding as the disease itself [4, 19]. The social experience of the patient who will continually avoid the gaze of others is another severe test [22, 32]. Several of these incriminated factors, taken individually, have an impact on the long diagnostic delay [2,3,4,5, 33, 34]. This is the case of the time taken to carry out the anatomopathological examination. Indeed, to date, Togo only has one pathological anatomy and cytology laboratory; which considerably increases the delay in histological diagnosis [7,8,9]. On the clinical level, the questioning in our series showed that less than 24.2% of the patients practiced self-examination which represents an important act in the early diagnosis of breast cancer. In the West, on the other hand, it constitutes, along with systematic screening, a habitual reflex in women, so that 80% of patients are seen at early stages [35,36,37,38]. The circumstances of discovery in our series were related to a pejorative stage and dominated by breast nodule with 75.8% followed by breast swelling with 30.6%. In developed countries, early diagnosis predominated at the stage of nodules and subclinical lesions detected by screening mammography [39,40,41].
Conclusion
The fear of the diagnosis, the absence of self-examination of the breasts and the recourse to traditional treatment and self-medication in first intention constituted the essential factors of the late diagnosis of breast cancers. This fear is generated by the gloomy prognosis to which it is subject and the cost of its treatment. The fact that women do not systematically practice self-examination explains why this cancer is always diagnosed in its symptomatic phase. The use of parallel treatments lengthens the diagnostic delay and prolongs the evolution and development time of the disease. Screening goes through information, education and the fight against poverty. Early screening of breast cancer requires information to the population, education and the fight against poverty. This early screening should contribute to the fight against the problem of delayed diagnosis in our context.
Availability of data and materials
Extracted data are with the corresponding author and available under reasonable request.
Abbreviations
- AJCC:
-
American Joint Committee on Cancer
- TNM:
-
Tumor, Nodes, metastasis
- OR:
-
Odds ratio
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
Adeloye D, Sowunmi OY, Jacobs W, David RA, Adeosun AA, Amuta AO, et al. Estimating the incidence of breast cancer in Africa: a systematic review and meta-analysis. J Glob Health. 2018;8(1):010419.
Adeloye D, Sowunmi OY, Jacobs W, David RA, Adeosun AA, Amuta AO, et al. J Glob Health. 2018;8(1):010419. https://doi.org/10.7189/jogh.08.010419. PMID: 29740502.
Joko-Fru WY, Miranda-Filho A, Soerjomataram I, Egue M, Akele-Akpo MT, da N’ G, et al. Breast cancer survival in sub-Saharan Africa by age, stage at diagnosis and human development index: a population-based registry study. Int J Cancer. 2020;146(5):1208–18.
Lukong KE, Ogunbolude Y, Kamdem JP. Breast cancer in Africa: prevalence, treatment options, herbal medicines, and socioeconomic determinants. Breast Cancer Res Treat. 2017;166(2):351–65.
Pace LE, Shulman LN. Breast cancer in Sub-Saharan Africa: challenges and opportunities to reduce mortality. Oncologist. 2016;21(6):739–44. https://doi.org/10.1634/theoncologist.2015-0429. Epub 2016 Apr 18PMID: 27091419.
Djiwa T, Koui B, Simgban P, Mézéwè Sama B, Bombonne M, Doukouré B, Darré T. Histo-molecular profile of breast cancer in young women in Togo. Clin Pathol. 2022;15:2632010X221112452. https://doi.org/10.1177/2632010X221112452.
Jedy-Agba E, McCormack V, Adebamowo C, Dos-Santos-Silva I. Stage at diagnosis of breast cancer in sub-Saharan Africa: a systematic review and meta-analysis. Lancet Glob Health. 2016;4(12):e923–35. https://doi.org/10.1016/S2214-109X(16)30259-5.
Darre T, Kpatcha TM, Bagny A, Maneh N, Gnandi-Piou F, Tchangai B, et al. Descriptive Epidemiology of Cancers in Togo from 2009 to 2016. Asian Pac J Cancer Prev. 2017;18(12):3407–11. https://doi.org/10.22034/APJCP.2017.18.12.3407. PMID: 29286611.
Darré T, Tchaou M, Djiwa T, Douaguibe B, Bassowa A, Adani-Ifé S, et al. Breast cancer in togolese women: imaging and clinicopathological findings. Breast Cancer (Auckl). 2021;15:11782234211020242. https://doi.org/10.1177/11782234211020242.
Darre T, Tchaou M, Djiwa T, Simgban P, Amavi AK, N’Timon B, et al. Male breast cancer in Togo: imaging and clinicopathological findings. Int J Breast Cancer. 2020;2020:3056067. https://doi.org/10.1155/2020/3056067.
Darré T, Tchaou M, Folligan K, Amadou A, N’Timon B, Sonhaye L, et al. Breast cancer cases of female patients under 35 years of age in Togo: a series of 158 cases. Mol Clin Oncol. 2017;7(6):1125–9. https://doi.org/10.3892/mco.2017.1461.
Adani-Ifè A, Amégbor K, Doh K, Darré T. Breast cancer in togolese women: immunohistochemistry subtypes. BMC Womens Health. 2020;20(1):261. https://doi.org/10.1186/s12905-020-01130-2. PMID: 33228656.
Hortobagyi GN, Connolly JL, D’Orsi CJ, Edge SB, Mittendorf EA, et al. Breast. In: Amin MB, Edge S, Greene F, et al, editors; American Joint Committee on Cancer. AJCC cancer staging manual. 8th ed. New York, NY: Springer. 2017.
Balekouzou A, Yin P, Pamatika CM, Bishwajit G, Nambei SW, Djeintote M, et al. Epidemiology of breast cancer: retrospective study in the Central African Republic. Public Health. 2016;16(1):1230.
Ly M, Antoine M, André F, Callard P, Bernaudin JF, Diallo DA. Breast cancer in sub-Saharan African women: review. Bull Cancer. 2011;98:797–806.
Aman NA, Doukoure B, Koffi KD, Koui BS, Traore ZC, Kouyate M, Effi AB. HER2 overexpression and correlation with other significant clinicopathologic parameters in Ivorian breast cancer women. BMC Clin Pathol. 2019;19:1.
Akuoko CP, Armah E, Sarpong T, Quansah DY, Amankwaa I, Boateng D. Barriers to early presentation and diagnosis of breast cancer among African women living in sub-Saharan Africa. PLoS One. 2017;12(2):e0171024. https://doi.org/10.1371/journal.pone.0171024.
Azubuike SO, Muirhead C, Hayes L, McNally R. Rising global burden of breast cancer: the case of sub-Saharan Africa (with emphasis on Nigeria) and implications for regional development: a review. World J Surg Oncol. 2018;16(1):63.
Mutebi M, Anderson BO, Duggan C, Adebamowo C, Agarwal G, Ali Z, et al. Breast cancer treatment: a phased approach to implementation. Cancer. 2020;126(Suppl 10):2365–78. https://doi.org/10.1002/cncr.32910.
Aziato L, Clegg-Lamptey JN. Breast cancer diagnosis and factors influencing treatment decisions in Ghana. Health Care Women Int. 2015;36(5):543–57.
Agodirin O, Olatoke S, Rahman G, Kolawole O, Oguntola S, Olasehinde O, et al. Determinants of late detection and advanced-stage diagnosis of breast cancer in Nigeria. PLoS One. 2021;16(11):e0256847. https://doi.org/10.1371/journal.pone.0256847.
Darré T, Amegbor K, Sonhayé L, Kouyate M, Aboubarak A, N’Timo B, et al. Histo-epidemiological profile of breast cancer: about 450 cases seen at the university hospital of Lome. Méd Afr Noire. 2013;60:53–8.
Darre T, Djiwa T, N’Timon B, Simgban P, Tchaou M, Napo-Koura G. Breast primary angiosarcoma: a clinicopathologic and imaging study of a series cases. Breast Cancer (Auckl). 2022;16:11782234221086726. https://doi.org/10.1177/11782234221086726.
Tchaou M, Darre T, Amavi AK, Kanassoua KK, N’Timon B, Sonhaye L, et al. Breast abscessed cancer in nonlactating women in tropical environment: radiological, bacteriological, and anatomopathological features about 3 cases. Case Rep Radiol. 2017;2017:1639847. https://doi.org/10.1155/2017/1639847.
Luyeye Mvila G, Postema S, Marchal G, Van Limbergen E, Verdonck F, Matthijs G, et al. From the set-up of a screening program of breast cancer patients to the identification of the first BRCA mutation in the DR Congo. BMC Public Health. 2014;14:759. https://doi.org/10.1186/1471-2458-14.
Luyeye Mvila G, Batalansi D, Praet M, Marchal G, Laenen A, Christiaens MR, et al. Prognostic features of breast cancer differ between women in the Democratic Republic of Congo and Belgium. Breast. 2015;24(5):642–8.
Aman NA, Doukoure B, Koffi KD, Koui BS, Traore ZC, Kouyate M, et al. Immunohistochemical evaluation of Ki-67 and comparison with clinicopathologic factors in breast carcinomas. Asian Pac J Cancer Prev. 2019;20(1):73–9.
Effi AB, Aman NA, Koui BS, Koffi KD, Traore ZC, Kouyate M. Breast cancer molecular subtypes defined by ER/PR and HER2 status: association with clinicopathologic parameters in ivorian patients. Asian Pac J Cancer Prev. 2016;17(4):1973–8.
Effi AB, Aman NA, Koui BS, Koffi KD, Traoré ZC, Kouyate M. Immunohistochemical determination of estrogen and progesterone receptors in breast cancer: relationship with clinicopathologic factors in 302 patients in Ivory coast. BMC Cancer. 2017;17(1):115. https://doi.org/10.1186/s12885-017-3105-z. PMID: 28173783.
Darre T, Tchaou M, Djiwa T, Tcharié LE, Brun LV, Gbeasor-Komlanvi AF, et al. Breast cancer: knowledge, attitudes on risk factors and means of screening by medical students from Lomé Togo. Adv Breast Cancer Res. 2020;9:127–37.
Tesfaw A, Getachew S, Addissie A, Jemal A, Wienke A, Taylor L, Kantelhardt EJ. Late-stage diagnosis and associated factors among breast cancer patients in South and Southwest Ethiopia: a multicenter study. Clin Breast Cancer. 2021;21(1):e112–9. https://doi.org/10.1016/j.clbc.2020.08.011. Epub 2020 Oct 1PMID: 33536135.
Gebremariam A, Dereje N, Addissie A, Worku A, Assefa M, Abreha A, et al. Factors associated with late-stage diagnosis of breast cancer among women in Addis Ababa. Ethiopia Breast Cancer Res Treat. 2021;185(1):117–24. https://doi.org/10.1007/s10549-020-05919-5. Epub 2020 Sep 18PMID: 32948993.
Youngblood VM, Nyirenda R, Nyasosela R, Zuze T, Yang Y, Kudowa E, et al. Outcomes and prognostic factors for women with breast cancer in Malawi. Cancer Causes Control. 2020;31(4):393–402. https://doi.org/10.1007/s10552-020-01282-4. Epub 2020 Mar.
Moodley J, Walter FM, Scott SE, Mwaka AM. Towards timely diagnosis of symptomatic breast and cervical cancer in South Africa. S Afr Med J. 2018;108(10):803–4. https://doi.org/10.7196/SAMJ.2018.v108i10.13478. PMID: 30421705.
Tetteh DA, Faulkner SL. Sociocultural factors and breast cancer in sub-Saharan Africa: implications for diagnosis and management. Womens Health (Lond). 2016;12(1):147–56. https://doi.org/10.2217/whe.15.76. Epub 2016 Jan 12PMID: 26757491.
Ben Fatma L, Belaid I, Said N, Gahbiche S, Hochlef M, Chabchoub I, et al. What could be the reasons of late diagnosis of breast cancer in Tunisia? Tunis Med. 2018;96(10–11):665–71 PMID: 30746659.
Maghous A, Rais F, Ahid S, Benhmidou N, Bellahamou K, Loughlimi H, et al. Factors influencing diagnosis delay of advanced breast cancer in Moroccan women. BMC Cancer. 2016;16:356. https://doi.org/10.1186/s12885-016-2394-y.PMID:27268201FreePMC.
Agodirin O, Aremu I, Rahman G, Olatoke S, Olaogun J, Akande H, Romanoff A. Determinants of delayed presentation and advanced stage diagnosis of breast cancer in Africa: a systematic review and meta-analysis. Asian Pac J Cancer Prev. 2021;22(4):1007–17.
Toure M, Nguessan E, Bambara AT, Kouassi YK, Dia JM, Adoubi I. Factors linked to late diagnosis in breast cancer in Sub-Saharan Africa: case of Côte d’Ivoire. Gynecol Obstet Fertil. 2013;41(12):696–700. https://doi.org/10.1016/j.gyobfe.2013.08.019.
Aloulou S, El Mahfoudi A, El Omrani A, Khouchani M. Factors related to late diagnosis of breast cancer: experience of CHU Mohammed VI Marrakech. Pan Afr Med J. 2015;21:162. https://doi.org/10.11604/pamj.2015.21.162.4363.
Acknowledgements
Not applicable
Funding
None.
Author information
Authors and Affiliations
Contributions
T. Darré was responsible for the conception of the study; participated in the study design; undertook the field study; conducted the data collection, analysis, and interpretation; and wrote the manuscript. L.T., P.S, M.B., T.Dj., B.N., B.S., A.K., B.D., B.K.M., Y.S.; and M.T. were involved in the data collection, analysis, and interpretation. They wrote and finalized the manuscript. G.N.K. is responsible for the overall scientific management of the study, for analysis and interpretation, and for the preparation of the final manuscript. All authors have read and approved the final manuscript for submission for publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the “Comité de Bioéthique pour la Recherche en Santé (CBRS)” (Bioethics Committee for Health Research) from the Togo Ministry of Health, Ref N0: 0101/2016/MS/CAB/DGS/DPLET/CBRS). All patients and relatives of patients had received information on the purpose and procedures of this study and provided written and informed consent. The study has been carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Darré, T., Tchandikou, L., Simgban, P. et al. Factors associated with late diagnosis of breast cancer in women in Togo, Sub-Saharan Africa. BMC Women's Health 23, 106 (2023). https://doi.org/10.1186/s12905-023-02257-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12905-023-02257-8