Abstract
Objective
Myofascial pain syndrome with trigger points is the most common cause of nonodontogenic pain. Although injection of the trigger points is the most effective pain reduction treatment, many patients exhibit recurrence after a short period. Therefore, the aim of the current study was to evaluate the clinical efficacy of magnesium sulfate injections in the treatment of the masseter muscle trigger points when compared to saline injections.
Material and method
This study randomly (1:1) assigned 180 patients to one of two treatment groups based on whether their trigger points were injected with 2 ml of saline or magnesium sulfate. Pain scores, maximum mouth opening (MMO), and quality of life were measured at the pre-injection and 1, 3, and 6 months post-injection.
Results
The pain scores were significantly higher in the saline group during all follow-up assessments, whereas the MMO was significantly higher in the magnesium sulfate group up to 3 months of follow-up (p < 0.001). However, the difference in MMO ceased to be statistically significant after 6 months of follow-up (p = 0.121). Additionally, the patient’s quality of life score was significantly higher in the magnesium sulfate group compared to the saline group (p < 0.001).
Conclusion
Injection of magnesium sulfate is an effective treatment measure for myofascial trigger points. However, further studies with a proper design addressing the limitations of the current study are necessary.
ClinicalTrials: org (ID: NCT04742140) 5/2/2021.
Similar content being viewed by others
Introduction
Myofascial pain syndrome with trigger points (TrPs) is the most common cause of nonodontogenic pain in the orofacial region [1], affecting approximately 40–60% of the adult population [2, 3]. Trigger points are defined as localized areas affected by spasms of the skeletal muscle, inflammation, and low blood flow, typically resulting in localized and referred pain upon palpation, loss of function, sleep disturbances, and a decrease in the patient's quality of life [2, 3].
Muscle pain and fatigue change muscle structure and function. It affects the jaw functions and force by decreasing the firing rate, conduction velocity, and excitability of motor units. In addition to the condylar degeneration which is a bone remodeling response to mechanical pressure [4, 5].
Injection of materials such as local anesthetics, botulinum toxins, corticosteroids, and physiologic saline is an effective method of reducing local and referred pain associated with TrPs. The needling action of these injections and the substances used contribute to successful management of chronic and active trigger points by relaxing the muscle fibers and alleviating pain [6,7,8]. However, many patients suffer from a recurrence of myofascial pain after a short period of injections, highlighting an unmet clinical need for a new treatment measure that can provide a longer lasting effect [7].
Magnesium sulfate (MgSO4) is commonly used for the treatment of musculoskeletal problems as it has muscle relaxant and vasodilator properties that can have an analgesic effect [9]. These properties can likely be attributed to its ability to block presynaptic acetylcholine discharge from neuromuscular and sympathetic junctions [10]. Moreover, MgSO4 solution can also have an antinociceptive effect in central and visceral pain tests, indicating its potential for use as an adjuvant pain therapy with limited adverse reactions. Previous studies have administered MgSO4 orally or intravenously to reduce pain intensity, particularly in patients with myogenous pain [11]. Yousef et al. [12] found that the use of MgSO4 supplements during the postoperative period in patients with refractory chronic lower back pain reduced pain intensity and improved lumbar spine mobility. The low molecular weight of MgSo4 also makes it suitable for the treatment of deeper tissues due to better penetration, resulting in superior therapeutic effects when compared to injection of other materials used for the treatment of myofascial trigger points [13]. Although previous studies have examined the administration of MgSo4 through oral and intravenous routes, there is limited evidence on the therapeutic effects of injecting MgSO4 into myofascial trigger points. Therefore, the aim of the current study was to investigate the clinical efficacy of MgSO4 injections in the treatment of masseter muscle trigger points when compared to saline injection to evaluate the pain score, maximum mouth opening, and quality of life as clinical parameters.
Material and methods
This study was conducted between February 2021 and December 2021 at the Oral and Maxillofacial Department, Faculty of Dentistry, Fayoum University. The study was approved by the Beni Suef Research Ethics Committee (code: FDBSUREC/11022021/SA) and the protocol was registered on ClinicalTrials.org (ID: NCT04742140) on 5th February 2021.
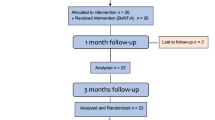
Informed consent for sharing clinical data and images for scientific purposes was collected from all patients prior to commencement of the study, which was performed in accordance with the Declaration of Helsinki [14] and reported as per the CONSORT guidelines 2012 [15] (Fig. 1).
Sample size estimation
The primary outcome measure was pain measured using a visual analog scale (VAS). A sample calculation (STATA V16.0) performed using data from a previous study showed that a total of 150 patients would need to be included for a study power of 80% at an alpha of 0.05. However, this study included a total of 180 patients (90 in each group) to account for any possible dropouts [16].
Study design and randomization
This prospective randomized (1:1) blinded clinical trial used an unstratified random block design (block sizes 2, 4, and 6) to ensure balance in the number of patients assigned to each group.
This study included 180 patients diagnosed with orofacial pain and trigger points in the masseter muscle unilaterally or bilaterally for a period of at least 6 months. The inclusion criteria were as follows: (1) definite diagnosis of myofascial pain based on the DC/TMD criteria with a referral [17]; (2) presence of one or more unilateral or bilateral trigger points in the masseter muscle; and (3) no history of any invasive procedures of the related masseter muscle. The exclusion criteria were (1) any painful conditions (other than myofascial trigger points) affecting the orofacial region; (2) any systemic diseases that could masticatory function (e.g., rheumatoid arthritis and epilepsy); and (3) pregnancy and lactation.
The patients were randomly assigned to one of two groups based on the treatment methods used, as follows: Group I (MgSo4 treatment) and group II (saline treatment).
The primary predictor variable was the treatment method used. The patients, surgeons, and assessors were blinded throughout the period of the study.
Intervention
After localization of the TrPs, the skin was disinfected with alcohol, the tight muscle band was grabbed between two fingers, and a 30-gage \({\raise0.5ex\hbox{$\scriptstyle 3$} \kern-0.1em/\kern-0.15em \lower0.25ex\hbox{$\scriptstyle 4$}}\)-inch needle was introduced 1–2 cm away from the TrP at a 30º angle to the skin. Negative aspiration was performed and each TrP was injected with 2 ml of either saline or MgSo4 (Magnesium sulfate sterile ampoule 10 ml, 100 mg/ml = 0.41 mMol/ml. Egyptian Int. Pharmaceutical Industries Co., Egypt) [18].
Outcome measurement
Outcomes, including the pain score, maximum mouth opening (MMO), and quality of life, were measured preinjection and 1, 3, and 6 months after injection.
Pain intensity was measured using a 10-point VAS, where a score of 0 indicated no pain and a score of 10 indicated maximum pain [19]. The MMO was assessed by measuring the interincisal distance between the upper and lower central incisors [19]. The quality of life was assessed using the Oral Health Impact Profile questionnaire (OHIP-14) containing 14 questions divided into seven domains of oral health. The participant was asked to score each question using a scale from 1 to 5 [never (score 0); hardly ever (score 1); occasionally (score 2); fairly often (score 3); and very often (score 4)], and the sum of all 14 items was calculated. The OHIP score could range from 0 to 56 units, with the former indicating no problems and higher scores representing greater impairment of quality of life [20].
Statistical analysis
Categorical data were presented as frequencies and percentages and were compared using Fisher’s exact test, whereas numerical data were reported as mean and standard deviation values. The Shapiro–Wilk test was used to assess normality, and parametric analyses included independent t-tests for intergroup comparisons and repeated measures analysis of variance and posthoc Bonferroni corrections for intragroup comparisons. Nonparametric analyses included Mann–Whitney U tests for intergroup comparisons and Friedman’s test followed by pairwise comparisons using multiple Wilcoxon signed rank tests with Bonferroni correction for intragroup comparisons. The significance level was set at p < 0.05, and all statistical analyses were performed using R, version 4.1.1 for Windows [21].
Results
This study included 180 cases divided equally into two groups [MgSo4 group n = 90, 15 males and 75 females; saline group n = 90, 13 males and 77 females]. The mean age of the MgSo4 group was 35.91 years, whereas that of the saline group was 30.53 years (Table 1).
No complications were observed except redness and mild discomfort at the injection site that was seen to resolve within 24 h in both groups.
The pain scores were significantly higher in the saline group compared to the MgSo4 group at all follow-up timepoints (p < 0.05; Table 2), whereas the MMO value was significantly higher in the MgSo4 group up to 3 months of follow-up (p < 0.001). However, the differences in MMO were no longer statistically significant after 6 months of follow-up (p = 0.121; Table 3). The OHIP-14 score was significantly higher in the MgSo4 group compared to the saline group throughout the study period (p < 0.001; Table 4).
Discussion
Myofascial pain syndrome is a neuromuscular problem characterized by muscle spasms, pain, and the presence of myofascial TrPs that present as muscle band contractions [17, 22,23,24]. TrPs most commonly affect the masseter muscles in the orofacial region, and are one of the major triggers of nonodontogenic pain [25, 26].
Because myofascial muscles are a part of the stomatognathic system, imbalance in any part of this system could have a detrimental impact on its function such as chewing, posture and non-physiological occlusion.that affect the patient's quality of life [27].
Injection of myofascial TrPs with different materials such as saline, local anesthesia, botulinum toxin, and platelet rich plasma injections can help reduce pain and has been seen to be widely tolerated [22, 28, 29]. However, many patients exhibit recurrence of myofascial pain after a short period of injections, highlighting the unmet clinical need for a new treatment measure with a longer lasting effect.
The aim of the current study was to evaluate the clinical efficacy of MgSo4 injections in the treatment of masseter muscles with TrPs when compared to saline injections. MgSo4 has been recommended for the treatment of myofascial TrPs due to its muscle relaxant and vasodilator properties that can have a pain-relieving effect. Few studies till date have examined the effects of MgSo4 on various musculoskeletal inflammatory disorders [9,10,11,12].
This study included 180 patients, and 84.4% of both study groups were female. This findings, in agreement with previous epidemiological evidence on tempero-mandibular disorders, can be attributed to hormonal and bio-behavioral factors, a higher demand for treatment among females, and their increased tendency toward psychological disorders [30, 31].
The mean age of patients in the MgSo4 group was 35.91 ± 12.61 years whereas that in the saline group was 30.53 ± 8.51 years, and this was in agreement with previous evidence that found that myofascial TrPs typically occurred in patients aged between 27 and 50 years [32].
The current study used the VAS scale to estimate pain intensity at each study interval, and significantly lower values were observed in patients receiving MgSo4 injections at all follow-up intervals when compared to patients receiving saline injections (P < 0.05). This could likely be attributed to the increased vasodilation provided by the former in several vascular beds, resulting in greater blood flow to the trigger point and removal of irritating substances that cause pain. Additionally, it also eliminates muscle tension and excessive tenderness by competing with calcium at the motor end plate and reducing acetyl choline discharge [33, 34]. This, in turn, leads to reduction of pain intensity at the site of injection, and these findings are in harmony with those of Ibrahim et al. [9], who also reported observing a palliative effect following iontophoresis with MgSO4 in healthy adult volunteers. Furthermore, Sane et al. [35], studied the effect of local injection of ropivacaine and bupivacaine injection with magnesium sulfate on postoperative pain in vertebral laminectomy surgery and concluded that local anesthesia combined with magnesium sulfate provided greater postoperative analgesia and considerably reduced postoperative opioid use.
On the other hand, Ahmed et al. [36], tested the efficacy of ultrasound-guided erector spinae plane block with and without the addition of magnesium sulphate on pain control in patients with postherpetic neuralgia and found that the addition of magnesium sulphate made no difference when compared to the use of bupivacaine alone.
The MMO was significantly higher in the MgSO4 group up to 3 months of follow-up (p < 0.001), although this statistical significance ceased to exist after 6 months (p = 0.121). Increased tension in the muscular band, inhibition of motor activity, muscle shortening, and occurrence of spasms often results in hypomobility, and the improvement in MMO observed in this study could be attributed to the muscle relaxation effect of MgSO4 which lowers acetylcholine release at the myoneural junction, blocking peripheral neuromuscular transmissions and inhibiting skeletal muscle contractions [34].
This is harmonized with the finding of Fathy et al. [37], who compared the efficacy of transforaminal MgSO4 injection against Ozone on pain intensity and functional disability in patients with lumbar disc prolapse and concluded that MgSO4 offered better analgesia, noticeably reduced analgesic ingestion and improved the functional disability.
Quality of life is an important parameter when evaluating the outcomes of various treatment measures for chronic pain. OHIP-14 is a specific tool used to assess oral function and measure oral health related quality of life. In the current study, all treatment groups exhibited improvement in the OHIP-14 score at the follow-up assessments, with the MgSo4 injection group exhibiting significantly better outcomes compared to the saline injection group (P < 0.001). This could be attributed to a reduction in pain intensity and improvement of function in the former [19, 38,39,40,41].
Compromised quality of life has been often reported for patients suffering from chronic pain which recovered with different treatment that improves the pain level [42]. This is in line with Azi et al. [43], who evaluate the analgesic effect of trigger point acupuncture combined with cyclobenzaprine chlorhydrate and sodium dipyrone. Azi et al. concluded that pain relief and improvement in quality of life at 4 weeks in both groups. Moreover, Brodsky et al. [44], evaluated change in health-related quality of life at the group and individual levels in a consecutive series of patients with chronic myofascial neck pain and concluded that considerable improvement over time was found for all scores post-treatment of myofascial neck pain.
The present study had several limitations. First, it did not compare the effects of MgSo4 injections to any other materials such as local anesthesia, botulinum toxin, or platelet rich plasma. Second, objective methods of assessment such as EMG could not be used due to limited resources.
Conclusion
The findings of this study suggest that MgSo4 injections are an effective treatment modality for myofascial TrPs of the masseter muscle. It reduces the pain and improves the maximum mouth opening, in addition to the quality of life. However, further studies with an improved design that addresses the limitations of the current study are necessary.
Availability of data and materials
The datasets used and/analyzed in the current study are available upon reasonable request from the corresponding author.
Abbreviations
- TrPs:
-
Trigger points
- MgSo4:
-
Magnesium sulfate
- VAS:
-
Visual analog scale
- MMO:
-
Maximum mouth opening
- OHIP-14:
-
Quality of life assessed using oral health impact profile questionnaire
References
De Leeuw R, Klasser GD. Orofacial pain: guidelines for assessment, diagnosis, and managemen. Hanover Park Quintessence: Publishing, Incorporated, The American Academy of Orofacial Pain IL; 2018.
Okeson JP. Orofacial pain: guidelines for assessment, diagnosis, and management. Chicago: Quintessence; 1996. p. 113–84.
Okeson JP, de Leeuw R. Differential diagnosis of temporomandibular disorders and other orofacial pain disorders. Dent Clin North Am. 2011;55(1):105–20. https://doi.org/10.1016/j.cden.2010.08.007 (Pubmed:21094721).
Bakke M, Möller E. Craniomandibular disorders and masticatory muscle function. Scand J Dent Res. 1992;100(1):32–8. https://doi.org/10.1111/j.1600-0722.1992.tb01806.x.
Frost HM. A 2003 update of bone physiology and Wolff’s Law for clinicians. Angle Orthod. 2004;74(1):3–15. https://doi.org/10.1043/0003-3219.
Hong C. Myofascial pain therapy. J Musculoskelet Pain. 2004;12(3):37–43. https://doi.org/10.1300/J094v12n03_06.
Yilmaz O, Sivrikaya EC, Taskesen F, Pirpir C, Ciftci S. Comparison of the efficacy of botulinum toxin, local anesthesia, and platelet-rich plasma injections in patients with myofascial trigger points in the masseter muscle. J Oral Maxillofac Surg. 2021;79(1):88.e1-9. https://doi.org/10.1016/j.joms.2020.09.013 (Pubmed:33045182).
Wong CSM, Wong SHS. A new look at trigger point injections. Anesthesiol Res Pract. 2012;2012:1–5. https://doi.org/10.1155/2012/492452.
Ibrahim NA, Raoof NA, Mosaad DM. Effect of magnesium sulfate iontophoresis on myofascial trigger points in the upper fibres of the trapezius. J Taibah Univ Medical Sci. 2021;16(3):369–78. https://doi.org/10.1016/j.jtumed.2020.12.015 (Pubmed:34140864).
Dahle LO, Berg G, Hammar M, Hurtig M, Larsson L. The effect of oral magnesium substitution on pregnancy-induced leg cramps. Am J Obstet Gynecol. 1995;73(1):175–80. https://doi.org/10.1016/0002-9378(95)90186-8 (Pubmed:7631676).
Albrecht E, Kirkham KR, Liu SS, Brull R. Peri-operative intravenous administration of magnesium sulphate and postoperative pain: a meta-analysis. Anaesthesia. 2013;68(1):79–90. https://doi.org/10.1111/j.1365-2044.2012.07335.x (Pubmed:23121612).
Yousef AA, Al-deeb AE. A double-blinded randomized controlled study of the value of sequential intravenous and oral magnesium therapy in patients with chronic low back pain with a neuropathic component. Anaesthesia. 2013;68(3):260–6. https://doi.org/10.1111/anae.12107 (Pubmed:23384256).
Ghimirey KB, Ita K. Microneedle-assisted percutaneous transport of magnesium sulfate. Curr Drug Deliv. 2020;17(2):140–7. https://doi.org/10.2174/1567201817666191217093936 (Pubmed:31845631).
General Assembly of the World Medical Association. World medical association declaration of Helsinki: ethical principles for medical research involving human subjects. J Am Coll Dent. 2014;81:14–8.
Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. Ann Intern Med. 2010;154(4):291–2.
Sakalys D, Rokicki JP, Januzis G, Kubilius R. Plasma rich in growth factors injection effectiveness for myofascial pain treatment in masticatory muscles. Randomized controlled trial. J Oral Rehabil. 2020;47:796–801. https://doi.org/10.1111/joor.12973 (Pubmed:32271467).
Reiter S, Goldsmith C, Emodi-Perlman A, Friedman-Rubin P, Winocur E. Masticatory muscle disorders diagnostic criteria: the American Academy of Orofacial Pain versus the research diagnostic criteria/temporomandibular disorders (RDC/TMD). J Oral Rehabil. 2012;39(12):941–7. https://doi.org/10.1111/j.1365-2842.2012.02337.x (Pubmed:22882635).
Nitecka-Buchta A, Walczynska-Dragon K, Batko-Kapustecka J, Wieckiewicz M. Comparison between collagen and lidocaine intramuscular injections in terms of their efficiency in decreasing myofascial pain within masseter muscles: a randomized, single-blind controlled trial. Pain Res Manag. 2018;2018:1–10.
Taşkesen F, Cezairli B. The effectiveness of the masseteric nerve block compared with trigger point injections and dry needling in myofascial pain. CRANIO®. 2020; 16:1–6.
Slade GD, Spencer AJ. Development and evaluation of the oral health impact profile. Commun Dent Health. 1994;11(1):3–11 (Pubmed:8193981).
Team RC: A Language and Environment for Statistical Computing (ed. Computing RFfS). Vienna, Austria. 2013.
Venancio Rde A, Alencar FG Jr, Zamperini C. Botulinum toxin, lidocaine, and dry-needling injections in patients with myofascial pain and headaches. Cranio. 2009;27(1):46–53. https://doi.org/10.1179/crn.2009.008 (Pubmed:19241799).
Okada-Ogawa A, Sekine N, Watanabe K, Kohashi R, Asano S, Iwata K, Imamura Y. Change in muscle hardness after trigger point injection and physiotherapy for myofascial pain syndrome. J Oral Sci. 2019;61(1):36–44. https://doi.org/10.2334/josnusd.17-0453 (Pubmed:30568046).
Kurtoglu C, Gur OH, Kurkcu M, Sertdemir Y, Guler-Uysal F, Uysal H. Effect of botulinum toxi- A in myofascial pain patients with or without functional disc displacement. J Oral Maxillofac Surg. 2008;66(8):1644–51. https://doi.org/10.1016/j.joms.2008.03.008 (Pubmed:18634953).
Romero-Reyes M. Uyanik JM Orofacial pain management: current perspectives. J Pain Res. 2014;7:99–115. https://doi.org/10.2147/JPR.S37593 (Pubmed:24591846).
Fernandez-Carnero J, La Touche R, Ortega-Santiago R, Galan-del-Rio F, Pesquera J, Ge HY, Fernandez-de-Las-Penas C. Short-term effects of dry needling of active myofascial trigger points in the masseter muscle in patients with temporomandibular disorders. J Orofac Pain. 2010;24(1):106–12 (Pubmed:20213036).
Fiorillo L. Spine and TMJ: a pathophysiology report. J Funct Morphol Kinesiol. 2020;5(2):24. https://doi.org/10.3390/jfmk5020024.
Kamanli A, Kaya A, Ardicoglu O, Ozgocmen S, Zengin FO, Bayik Y. Comparison of lidocaine injection, botulinum toxin injection, and dry needling to trigger points in myofascial pain syndrome. Rheumatol Int. 2005;25(8):604–11.
Nitecka-Buchta A, Walczynska-Dragon K, Kempa WM, Baron S. Platelet-rich plasma intramuscular injections - antinociceptive therapy in myofascial pain within masseter muscles in temporomandibular disorders patients: a pilot study. Front Neurol. 2019;10:250. https://doi.org/10.3389/fneur.2019.00250 (Pubmed:30941095).
Classification GRD. epidemiology, and natural history of myofascial pain syndrome. Curr Pain Headache Rep. 2001;5(5):412–20. https://doi.org/10.1007/s11916-001-0052-8 (Pubmed:11560806).
Alvarez DJ, Rockwell PG. Trigger points: diagnosis and management. Am Fam Phys. 2002;65(4):653–60 (Pubmed:11871683).
LeResche L. Epidemiology of temporomandibular disorders: implications for the investigation of etiologic factors. Crit Rev Oral Biol Med. 1997;8(3):291–305. https://doi.org/10.1177/10454411970080030401 (Pubmed:9260045).
Nishio A, Gebrewold A, Altura BT, Altura BM. Comparative vasodilator effects of magnesium salts on rat mesenteric arterioles and venules. Arch Int Pharmacodyn Ther. 1989;298:139–63 (Pubmed:2757462).
Wang H, Liang QS, Cheng LR, Li XH, Fu W, Dai WT, Li ST. Magnesium sulfate enhances non-depolarizing muscle relaxant vecuronium action at adult muscle-type nicotinic acetylcholine receptor in vitro. Acta Pharmacol Sin. 2011;32(12):1454–9. https://doi.org/10.1038/aps.2011.117 (Pubmed:21986576).
Sane S, Mahdkhah A, Golabi P, Hesami SA, Kazemi HB. Comparison the effect of bupivacaine plus magnesium sulfate with ropivacaine plus magnesium sulfate infiltration on postoperative pain in patients undergoing lumbar laminectomy with general anesthesia. Br J Neurosurg. 2020;17:1–4. https://doi.org/10.1080/02688697.2020.1861430.
Ahmed SA, Magdy AA, Abdullah MA, Albadry AA. The effect of erector spinae plane block with and without addition of magnesium on relief of pain from post-herpetic neuralgia. Pain Phys. 2022;25(5):365–72.
Fathy W, Hussein M, Ibrahim RE, Abdel-Aziz MM, Adel S, Soliman SH, Elmoutaz H, Abdelkader M. Comparative effect of transforaminal injection of Magnesium sulphate versus Ozone on oxidative stress biomarkers in lumbar disc related radicular pain. BMC Anesthesiol. 2022;22(1):1-10. https://doi.org/10.1186/s12871-022-01789-0.
Kirkland AE, Sarlo GL, Holton KF. The role of magnesium in neurological disorders. Nutrients. 2018;10(6):730. https://doi.org/10.3390/nu10060730 (Pubmed:29882776).
Pouteau E, Kabir-Ahmadi M, Noah L, Mazur A, Dye L, Hellhammer J, Pickering G, DuBray C. Superiority of magnesium and vitamin B6 over magnesium alone on severe stress in healthy adults with low magnesemia: a randomized, single-blind clinical trial. PLoS ONE. 2018;13(12):1–17. https://doi.org/10.1371/journal.pone.0208454 (Pubmed:30562392).
Schwalfenberg GK, Genuis SJ. The importance of magnesium in clinical healthcare. Scientifica. 2017;2017:4179326. https://doi.org/10.1155/2017/4179326 (Pubmed:29093983).
Ng KT, Yap JLL, Izham IN, Teoh WY, Kwok PE, Koh WJ. The effect of intravenous magnesium on postoperative morphine consumption in noncardiac surgery: a systematic review and meta-analysis with trial sequential analysis. Eur J Anaesthesiol. 2020;37(3):212–23. https://doi.org/10.1097/EJA.0000000000001164 (Pubmed:31977626).
Çeliker R, Atalay A, Guven Z. Health-related quality of life in patients with myofascial pain syndrome. Curr Pain Headache Rep. 2010;14(5):361-6. https://doi.org/10.1007/s11916-010-0141-7.
Gazi MC, Issy AM, Avila IP, Sakata RK. Comparison of acupuncture to injection for myofascial trigger point pain. Pain Pract. 2011;11(2):132–8. https://doi.org/10.1111/j.1533-2500.2010.00396.x.
Brodsky M, Spritzer K, Hays RD, Hui KK. Change in health-related quality-of-life at group and individual levels over time in patients treated for chronic myofascial neck pain. J Evid Based Complement Altern Med. 2017;22(3):365–8. https://doi.org/10.1177/2156587216662779.
Acknowledgements
Not applicable
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). This research received no specific grants from any public or commercial funding agencies or from the nonprofit sector.
Author information
Authors and Affiliations
Contributions
SR: study design, major contributor in writing the manuscript; AM: data analysis; AS: patient data interpretation, manuscript drafting. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Beni Suef Research Ethics Committee (approval code: FDBSUREC/11022021/SA). The study was performed in accordance with the Declaration of Helsinki. Informed consent to share clinical data and images for scientific purposes was collected from all patients prior to commencement.
Consent for publication
Not applicable.
Competing interests
The authors have no competing interests to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Refahee, S.M., Mahrous, A.I. & Shabaan, A.A. Clinical efficacy of magnesium sulfate injection in the treatment of masseter muscle trigger points: a randomized clinical study. BMC Oral Health 22, 408 (2022). https://doi.org/10.1186/s12903-022-02452-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-022-02452-3