Abstract
Background
Chronic periodontitis (CP), defines as destruction of the supporting tissues of the teeth and resorption of the alveolar bone. It is widespread in human populations and represent an important problem for public health. CP results from inflammatory mechanisms created by the interaction between environmental and host genetic factors that confer the individual susceptibility to the disease.
Aim
The aim of the current study was to explore and summarize some functional biomarkers that are associated with CP susceptibility.
Methods
CP is considered to be a multifactorial disease. The pathogenesis of multifactorial diseases is characterized by various biological pathways. The studies revealed that polymorphisms were associated with susceptibility to periodontal diseases. In other word, genetic variations can change the development of CP. However, there are some conflicting results, because there are different variations in frequency of some alleles in any populations. Therefore, we conducted the current review to completely understanding the special biomarkers for CP.
Results
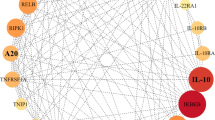
There is some evidence that SNPs in the IL-1α, IL-1β, IL1RN, IL-6, IL-10, TNF-α, TGF-β1, IFN-γ and VDR may be associated with CP susceptibility.
Conclusion
In conclusion, numerous studies have reported the host genetic factors associated with CP susceptibility and related traits. Therefore, it is prevail to study the multiple SNPs and their effects to find the useful diagnosis methods. The current study will investigate the relationship between polymorphisms in cytokine genes and the susceptibility to the chronic periodontitis.
Similar content being viewed by others
Introduction
Accumulation of microbial plaque in gingiva can induce inflammatory responses which lead to periodontal diseases. This inflammation progresses to the periodontitis as a chronic inflammatory condition. In periodontal disease, tooth-supporting tissues are destroyed. In untreated patients, ligamentous support of the teeth is lost. Subsequently, the resorption of the alveolar bone caused loss of the teeth [1,2,3].
Periodontal disease has two major forms: chronic and aggressive. Aggressive periodontitis is a rapidly progressive condition, but chronic periodontitis (CP) has a relatively slower rate. Chronic periodontitis is common in more than 30% of adults, while up to 13% of the adults will be affected by severe periodontitis [4].
It is believed that CP has multifactorial etiopathogenesis. Host genetic, environmental and microbiological factors are the three major parameters which can determine the natural history of disease [2]. It means that, either subgingival biofilm and host genetic variations together are necessary to cause disease [1]. On the other hand, some strong evidences have been emphasized that host genetic has an important effect in the pathogenesis of periodontitis. In addition, the studies have been conducted on twins reported that the human genome may alter the frequency of the disease in half of the population [4, 5]. In this regard, understanding the genetic basis of CP can be used as an early and a useful diagnostic method for detecting the susceptibility to the disease. Given that, the genes can change the etiology of disease, so we can provide the appropriate treatment methods. It is estimated that there are possibly 20 genes which may increase the relative risk for CP. However, it should be noted that the effects of these genes are not independent of environmental factors and ethnicity [6].
In CP gram-negative anaerobic bacteria induce the attachment loss of tooth from its supporting tissues. This mechanism has been mediated by some regulatory and inflammatory cytokines. In other words, cytokines contribute to periodontitis susceptibility. Therefore, it has been suggested that insufficient production of cytokines against inflammatory activities can cause the disease. Some studies have shown that there was a relationship between cytokine SNPs and CP. Such variations can change the levels of cytokines production, which in turn may result in changes in immune responses and can cause long lasting inflammations. Therefore, study on relationship between genotype and/or allele frequencies and disease susceptibility can introduce some genotypes and alleles that can increase the risk of inflammatory disease [7]. Recently, some scientists have reported the effects of single nucleotide polymorphisms (SNPs) in candidate genes in susceptibility to CP (Table 1.) [2, 8,9,10,11,12,13]. It seems that the use of the genetic risk score could be useful in detection of the CP susceptibility [14,15,16,17,18,19]. However, a number of conflicting results have been reported, because there are different variations in frequency of some alleles in any populations. The aim of the current study was to explore and summarize some functional biomarkers such as Interleukin-1 and Tumor necrosis factor alpha; as pro-inflammatory cytokines; IL-6, IL-10; as regulatory cytokines; VDR; as a connective tissue metabolism-associated-gene; that are associated with CP susceptibility.
Candidate SNPs involved in CP
IL-1 gene cluster
Interleukin-1 (IL-1) is a pro-inflammatory cytokine, which encoded by IL-1 gene cluster at position 2q13–21. This cytokine produced by monocytes, macrophages and dendritic cells which induce a complex network of proinflammatory cytokines and plays an important role in the regulation of immune and inflammatory responses to infections. IL-1 induces the migration of immune cells to the sites of infection through the expression of adhesion factors on endothelial cells [20, 21].
IL-1 is composed of two different molecules with similar function, IL-1α and IL-1β. IL-1α regulates the intracellular events, whereas IL-1β act as an extracellular protein. It has been reported that the levels of IL-1α, IL-1β and also IL-1/IL-receptor antagonist (RA, anti inflammatory cytokine) have been increased in patients with periodontal diseases [22, 23]. The data showed that the IL-1 cluster gene SNPs were associated with higher risk for periodontitis [24,25,26]. Karimbux et al. [27], Mao et al. [28], Yin et al. [29], Zeng et al. [30] in their meta-analysis studies have revealed that IL-1α and IL-1β genetic variations are significant contributors to CP in different geographical populations. On the other hand, these studies showed that the selected polymorphisms of the IL-1 genes were associated with susceptibility to aggressive periodontitis but not to chronic periodontitis in the some populations [31]. At the first time, Kornman et al. reported a relationship between IL-1α − 889 and IL-1β + 3953 SNPs and disease severity in patients with periodontitis [32]. This study continued by other scientists to examine the relationship between the SNPs in interleukin-1 gene and periodontitis. Some polymorphisms of the IL-1 gene have been studied in association with both aggressive and chronic periodontitis: IL-1α − 889, + 4845; IL-1β − 511, − 31, + 3954 and IL1RN VNTR (variable number of tandem repeats), + 2018.
IL-1α-889C/T polymorphism is located in the IL-1α promoter. IL-1α − 889 and IL-1β + 3954 were strongly associated with the periodontitis [32]. This report caused that Kinane et al. evaluated the epidemiological properties of IL-1 gene polymorphisms in people with periodontitis [33]. Furthermore, it has been shown that IL-1α − 889 and IL-1β + 3954 risk alleles could increase and the IL1RN VNTR risk allele decrease the IL-1α and IL-1β levels in the gingival crevicular fluid of periodontal patients [34,35,36,37]. It means that these SNPs can increase or decrease the gene transcription and protein production levels, which causes changes in the inflammatory responses.
The case-control studies in Caucasians and non-Caucasians have been shown that IL-1 rare variant (R allele), were different among various populations. In this regard, the carriage rate of the IL-1α − 889R-allele varies from 43 to 90% and 35 to 79% in patients and controls, respectively. In addition, Asian populations have a lower carriage rate of the IL-1α − 889R-allele (8–23%) than other populations [38, 39]. These findings demonstrate that the ethnicity may affect the carriage rate of SNPs among different population. Therefore, possible positive associations between an SNP and disease within one population may not necessarily be extrapolated to other populations. Only some studies have reported a relationship between the carriage rates of the IL-1α − 889R-allele and CP as a single genetic risk factor [40,41,42,43].
There are conflicting results about IL-1β + 3954 SNP. Recently, Wu et al. [44] identified significant associations between moderate to severe adult CP and IL-1β polymorphisms in four different ethnicities: Caucasians, African Americans populations, Hispanics and Asians. A meta-analysis by Ma et al. [45], showed that IL-1β + 3954 polymorphism probably increased the risk of CP in Asians, and might be in association with a strongly increased risk of CP in Indians, but not in Chinese populations. In Asian population the carriage rate of the IL-1β + 3954R-allele is lower (≤10%) than the Caucasian populations (13–74%) [38, 39, 46]. Lopez et al., Moreira et al. and Wagner et al. have shown an association between the IL-1β + 3954R-allele and CP [43, 47, 48]. Laine et al. reported an association in a sub-group of patients [42]. Galbraith et al. and Gore et al. found a relationship between IL-1β + 3954R-allele and periodontitis and disease severity [49, 50]. However, Rogers et al. reported an association between the normal variant (N-allele) of the IL-1β + 3954 and CP, but not for IL-1β + 3954R-allele [51]. In another study, Struch et al. have not found any significant differences for carriage rates of the IL-1β + 3954R-allele between CP patients and controls in a Caucasian population [52]. Although some results did not support that the IL-1β SNP could be identified as a risk factor for CP, but the synergistic interactions of the some genotypes of IL-1β SNPs with environmental factors might play an important role in the pathogenesis of periodontal disease [53, 54].
Amirisetty et al. [55] and Masamattiet al. [56] suggested a strong association of the IL-1β − 511 and + 3954 variants with chronic periodontitis in Indian population. Although, some studies reported carriage rates for IL-1β-511R-allele, but, nowadays, IL-1β-511 polymorphisms haven’t been reported to be associated with CP. The finding showed that the carriage rate of the IL-1β-511R-allele was higher among Asians (67%) compared to Caucasians (43–59%) [46, 50, 57, 58].
There were conflicting results about IL1RN gene encoding the IL-1Rα. There are few studies investigating IL1RN gene polymorphisms in periodontitis. The results of some meta-analysis suggested that IL-1RN VNTR polymorphism might contribute to an increased risk to CP [59]. In a Turkish population, the frequency of IL1RN + 2018R-allele in patients with CP was higher than controls [60]. Results have been shown that the presence of the IL1RN, IL-1α − 889 and IL-1β + 3954R-alleles simultaneously had an association with CP susceptibility [42] and severity [32] in nonsmoking Caucasian patients. In Asian populations, the prevalence of the composite genotype was very low (3%) but in Caucasian populations, it was significantly higher (10 to 46%) [38, 39, 61]. In some case-control studies in Caucasians [47, 62] and non-Caucasians [63], the IL-1 composite genotype have reported as a risk factor for CP susceptibility. Meisel et al. showed that the IL-1 composite genotype was associated with periodontal disease only in Caucasian smokers [64]. Moreover, subjects with the IL-1 composite genotype have increased counts of periodontal pathogens [65]. Nevertheless, the findings revealed a higher frequency of IL-1 composite genotype in non-smoking patients who had not periodontal pathogens [42]. It means that IL-1 gene SNPs can change the susceptibility to the disease in the absence of other risk factors.
Taken together, the IL-1 gene cluster SNPs cannot be considered as risk factors for CP for all populations. However, IL-1 composite genotype may be a genetic risk factor for Caucasian population.
Il-6
During an acute and/or chronic infection, immune cells, such as T cells produces IL-6 which causes inflammation in tissues [66, 67].
IL-6 can control the immune responses via the inhibition of type 1 cytokines and activation of type 2 cytokines. In addition, IL-6 involved in regulation of metabolic and neural processes. IL-6 can bind to its membrane glycoprotein GP130 receptor. Subsequently, IL-6-GP130 complex, leading to GP130 homodimer formation and signal induction [66].
The IL-6 is encoded by the IL-6 gene localized on chromosome 7p21. Some studies demonstrated that polymorphisms of this gene can affect the concentration of IL-6 in serum [68, 69]. Polymorphisms in the promoter region of the IL-6 gene affect transcription and expression of IL-6 in individuals. There are three SNPs in the IL-6 promoter region (− 597G/A, -572C/G and -174G/C), that have been reported in chronic inflammations. These SNPs control the up-regulation of IL-6 levels and affect the serum levels of circulating interleukin-6. The IL-6-174 could influence IL-6 expression levels. The subjects with IL-6-174C-allele have lower plasma levels of IL-6 compared to the individuals with G-allele [70]. Therefore, IL-6-174C-allele may prevent proper immune response against periodontal pathogens in the host.
The carriage rates of the IL-6-174C-allele were 37–67% and 44–54% in Brazilian [71,72,73] and Caucasian populations [58, 74, 75], respectively. In addition, IL-6 -174, − 190 and − 597 SNPs were not polymorphic in a Japanese population [76]. Heidari et al. [77] Brett et al. [58], Babel et al. [74], Tervonen et al. [75] and Trevilatto et al. [72] have revealed the association between IL-6-174G/C and susceptibility to CP. Nevertheless, Nibali et al. found an association for IL-6-174 in combination With IL-6 -1480 and − 1363 SNPs, but not for IL-6 -174 alone [78].
With regard to the other IL-6 gene SNPs, it has been revealed that the IL-6-572 SNP may be a protective factor for CP [79]. In addition, the results have been suggested that the IL-6-1363 G/T and IL-6R + 48,892 A/C polymorphisms may contribute to genetic susceptibility to CP in Chinese population [80]. However, in a meta-analysis, Nikolopoulos et al. [81] did not show any association between IL-6-174 and CP, but, it seems that IL6–174 SNP may be change the susceptibility to CP.
Il-10
Interleukin-10 (IL-10) is an anti-inflammatory cytokine which has vital role in pathogenesis of periodontal diseases [82, 83]. This cytokine is expressed by various cells specially leukocytes. In addition, T helper 1 (Th1), Th2, CD8 T cells and B cells, from the adaptive immune system can express IL-10. Macrophages, mast cells, natural killer cells in the innate immune system also produce IL-10 cytokine [84]. Interleukin-10 can control viral infections and related tissue damages via stimulating the secretion of immune factors, controlling the phagocytosis and antigen presentation. In addition, IL-10 can play a role in the regulation of proinflammatory cytokines such as IL-1 and TNF-α. On the other hand, IL-10 improves the innate and adaptive immunity [85, 86].
The gene encoded IL-10 is located on chromosome 1q31-q32. This gene is in a cluster with closely related to the IL-19, IL-20, and IL-24. Polymorphisms in the promoter region of the IL-10 gene can affect the expression of IL-10 cytokine which leads to changes in inflammatory processes [87,88,89]. There are some conflicting results regarding the association between IL-10 polymorphisms and CP [90,91,92]. Some studies to analyze the SNPs in the promoter region of the IL-10 gene and its relation with periodontal disease have revealed that these polymorphisms might be associated with susceptibility to CP [93,94,95,96,97]. However, in some studies, analysis of allelic and genotypic frequencies of IL-10 SNPs revealed no causal relationship between the presence of polymorphisms and development of CP [98, 99].
The IL-10 -1082, − 819, and − 592 polymorphisms are in linkage disequilibrium and produce two important haplotypes. The studies revealed that IL-10 -1082, − 819 and − 592 polymorphisms were related to the CP in Swedish, Turkish and Brazilian patients [90, 92]. Moreover, in vitro studies have reported that GCC/GCC genotype is associated with increased expression of IL-10 cytokine compare to the other genotypes [100, 101].
The in vitro and in vivo studies have been shown that, IL-10-592R-allele was related to the lower levels of IL-10 and may change the expression of IL-10 in response to inflammatory disease [100,101,102]. IL-10 can prevent the periodontal tissue destruction through inhibiting the receptor activator of nuclear factor-κB (RANK) and matrix metalloproteinases (MMPs) [103, 104]. Therefore, subjects with IL-10-592R-allele have a higher risk for susceptibility to inflammatory diseases.
With regard to the other IL-10 SNPs, the results have been shown that IL-10-1082 polymorphism were not associated with CP susceptibility, especially, in Caucasians, and the carriage rates of the IL-10-1082R-allele were 44–81% [91, 105]. However, there was an association between IL-10-1082 N-allele and CP in Swedish Caucasians [90].
The IL-10-819 SNP has been associated with CP in Brazilians but not in other populations [91, 92, 105].
Scarel et al., Sumer et al. and Claudino et al. have found a higher R-allele carriage rate for IL-10-592 SNP in CP patients [91, 92, 102]. The carriage rate of the IL-10-592R-allele were 68–75% and 41% - 51 in CP patient and controls, respectively.
Our recent study showed that (unpublished data), the prevalences of AG and GG genotypes of IL-10-1082 in comparison with the AA genotype were significantly higher in CP patients than control groups. In addition, subjects with at least one IL-10-1082-G allele significantly had an increased risk for CP. The distribution of the IL-10-819 and IL-10-592 genotypes was not different between CP and control subjects. The combination of different genotypes showed that GCC haplotype was significantly different between case and control groups. Our results demonstrated that IL-10-1082 polymorphism was a putative risk factor for CP and associated with increased susceptibility to the disease.
In a Japanese population haplotype frequencies of the IL-10 -1082, − 819, and − 592 SNPs have been analyzed and no significant differences were found between groups in regard to the carriage rates of the haplotypes [106]. The remarkable point was that the IL-10-1082 N-allele was absent among the Japanese, but not in Caucasians [90, 106].
Finally, it seems that, IL-10-592 SNP has been associated with CP susceptibility and might be a genetic marker for CP susceptibility. Given that IL-10 can inhibit the matrix metalloproteinases and reduce the periodontal tissue destruction [103, 104], recommended to reveal the possible relationship between IL-10 polymorphisms (− 1082, − 819, − 592) and chronic periodontitis. These studies need to be replicated to enable conclusions to be drawn.
TNF-α
Tumor necrosis factor alpha (TNF-α) is a proinflammatory cytokine involved in inflammations. TNF-α can control the production of chemokines or cyclooxygenase products, which consequently induce inflammation. It is produced by many cell types mainly macrophages. TNF-α controls the apoptotic cell death and inflammation and inhibit viral replication through the regulation of immune cells [9, 107, 108]. Insufficient TNF-α production causes various diseases such as cancer, psoriasis and inflammatory bowel diseases [107, 109, 110]. By destructing arachidonic acid, this cytokine causes an increment of prostaglandin E2 concentration, and then activation of osteoclasts. TNF-α stimulates osteoclasts differentiation and along with IL-1 may cause release of the matrix metalloproteinase (MMPs) and destruction of the extracellular matrix and bone resorption [81, 111, 112]. This mechanism probably is done on inflamed periodontal tissues during CP disease.
The human TNF-α gene is located on chromosome 6p21.3. This gene has an AU-rich element in the 3’ UTR region that is a polymorphic site [9, 108, 113].
It has been shown that the TNF-α gene SNPs were risk factors for periodontitis in both Caucasians and non-Caucasians populations. A number of important SNPs in the TNF-α gene have been studied: − 1031, − 863, − 857, − 376, − 308, and − 238 (in promoter region) and + 489 (in the first intron).
Yang et al. [114] reported that TNF-α-1031 SNP was a risk factor for CP. However, there was lack of association between TNF-α-857C/T and -238G/A gene polymorphisms and susceptibility to CP in Chinese population. Some findings from meta-analysis by Ding et al. [115], supported that TNF-α-308G/A and -863C/A polymorphisms may contribute to the susceptibility to periodontitis. The results of some studies revealed an association between TNF-α-308 SNP and periodontitis [116]. The carriage rate of the TNF-α-308R-allele in Japanese population [46] was 2–3% and significantly was lower than other populations (18–44%) [49, 58, 75, 111, 117,118,119,120,121]. Our study on an Iranian population did not show a significant difference in frequencies of TNF-α-308 genotypes and alleles between CP and control groups [108]. Stereological analysis of interdental gingiva in the same CP patients with different TNF-α-308 SNP also showed no significant differences in volume density of epithelium, connective tissue, collagenous and non-collagenous matrixes and blood vessels between CP patients [9].
With regard to the other SNPs in TNF-α gene, the results have been revealed that the frequencies of TNF-α-238R-allele were different between various ethnic populations [46, 117, 120]. Soga et al. [46] reported positive associations between TNF-α − 1031, − 863, and − 857 SNPs and CP. But, these findings have not been replicated and needed for further studies to evaluate the real function of the TNF-α polymorphisms in CP susceptibility.
TGF-β
Transforming growth factor beta (TGF-β) is a multifunctional cytokine that controls proliferation, cellular differentiation, apoptosis, angiogenesis, and immune reactions. TGF-β is secreted by various inflammatory cells such as macrophages during tissue injury and regulates synthesis of connective tissue components and matrix proteins by fibroblasts and other cell types via chemotactic mechanisms [11, 122].
This cytokine exists in three isoforms: TGF-β1, TGF-β2 and TGF-β3 that have been expressed in high levels in most tissues. Various cells that secret TGF-β also has autocrine signaling properties because these cells express the TGF-β receptor family. TGF-β can induce differentiation of fibroblasts at the sites of inflammation in order to repair the lesions. In addition, it seems that induction of TGF-β secretion leads to increased eradication of inflammation through apoptotic mechanisms [11, 123].
TGF-β1 is a pleiotrophic growth factor that is involved in the regulation of numerous immunomodulatory processes [124]. It was suggested that TGF-β1 could be considered as a disease predictive biomarker [125]. Studies indicated that the expression level of TGF-β1 mRNA in the regulatory T cells present in the gingival tissue is correlated with periodontitis [126, 127]. Khalaf et al. [128] reported that the expression level of TGF-β1could predict the progression of periodontitis. TGF-β1 can increase osteoprotegerin expression in bone marrow stromal cells. Therefore, it seems that TGF-β1 has a supportive role against the bone destruction process during CP [127].
TGF-β1–29C/T, -509C/T, and -788C/T, are the main TGF-β1 SNPs. In our previous study [10], we did not find a significant association between -509C/T and -788C/T variants of the TGF-β1 gene and risk of CP in an Iranian population. We proposed that TGF-β1–29 SNP, may contribute to the development of CP. Moreover, Holla et al. [129], could not find an association between TGF-β1–29 and − 509 SNPs and CP in a Czech population. In line with our results, Kobayashi et al. [130] did not find any association between TGF-β1 polymorphisms and periodontitis in the Japanese population. Also, Atilla et al. [131] have found that TGF-β-788 variant was not associated with CP in a Turkish population. Nevertheless, the results of our quantitative studies showed that TGF-β1–509 and − 29 SNPs were strongly associated with quantitative parameters of connective tissue constituents of interdental gingiva in CP patients [2, 11, 12]. On the other hand, de Souza et al. [132] found that frequency distribution of TGF-β1–509 genotypes and alleles in the severe CP was significantly different from the control and moderate CP groups. Cui et al. [133] in a meta-analysis suggested that the TGF-β1–509 SNP was associated with the periodontitis risk in Asians but not in Caucasians. Atanasovska-Stojanovska et al. [134] concluded that polymorphisms of TGF-β1 gene were associated with an increased risk of CP in a Macedonian population. They found an association between the -29C/T SNP and susceptibility to CP.
In regard to the other TGF-β1 polymorphisms, Babael et al. [135] revealed that the TGFβ1-codon 25 variant was more common in control subjects than in CP patients. However, Erciyas et al. [68] did not show an association between TGFβ1-codon 10 and 25 SNPs and periodontitis.
In conclusion, the data suggest that TGF-β1 gene polymorphisms may contribute to a genetic risk factor for CP. However, further studies analyzing gene-gene and gene-environment interactions are required. Such studies lead to have a better understanding of the association between the TGF-β1 SNPs and CP risk.
IFN-γ
Type II class of interferons such as interferon gamma (IFN-γ) play an important role in controlling the immune system. The IFN-γ gene is located on chromosome 12q24 and usually produced by natural killer (NK) cells, Th1 and cytotoxic T lymphocyte cells [8]. IFN-γ can activate the macrophages and increase the expression of Class II MHC molecules and then induce anti-viral and anti-tumor functions. It can inhibit the replication of viruses and inflammatory diseases will occur if the amount of protein change [136]. High levels of IFN-γ are expressed in diseased periodontal tissues and associated with severity of disease. It seems that IFN-γ is involved in the alveolar bone resorption in periodontitis [137, 138].
IFN-γ has a heterodimeric receptor that consists of Interferon gamma receptor 1 (IFNGR1) and Interferon gamma receptor 2 (IFNGR 2). When IFN-γ binds to its receptor, the JAK-STAT signaling pathway is activated. Also, if IFN-γ is attached to the glycosaminoglycan heparan sulfate, it will be deactivated [139].
Polymorphisms of IFN-γ and its receptor can cause chronic inflammatory diseases [8, 140,141,142]. Recently, Heidari et al. have studied the association between the IFN-γ and IFN-γR1 gene polymorphisms and risk of CP in an Iranian population. They revealed that IFN-γ (+ 874 A/T) was significantly in positive association with chronic periodontitis [8]. In addition, our another investigation (unpublished data), showed that there was a significant relationship between the IFN-γ (+ 874 T/A) gene polymorphism and the risk of hepatitis B virus infection as another chronic inflammatory disease in Iranian population. We did not find any significant differences in IFN-γR1 (− 611A/G), IFN-γR1 (+ 189 T/G), IFN-γR1 (+95C/T) SNPs between case and control groups.
The + 874 T allele is linked to the 12 CA repeats and the A allele is connected with the non-12 CA repeats. This specific sequence provides a binding site for the transcription factor NFkB which induces IFN-γ gene expression [143, 144]. Babel et al., Reichert et al. and Hooshmand et al. studied allele and genotype frequencies of IFN-γ polymorphisms in patients with periodontitis [135, 145, 146]. In addition, Reichert et al. [145] confirmed a significant relationship between IFN-γ + 874 variant and some periodontal pathogens such as aggregatibacter actinomycetemcomitans and prevotella intermedia. However, Holla et al. [147] did not find significant relationship between variants of the IFN-γ and susceptibility to CP or microbial composition. Loo et al. [148] study also did not find any significant differences in their selected genes (IL-1b, IL-6, IFN-γ and IL-10) between the CP patients and healthy subjects.
In regard to the IFN-γR1 SNPs, the effects of IFN-γR1–611 SNP are stronger than of IFN-γ R1–56 [149]. Rosenzweig et al. [150] found that G-611 carrier constructs are stronger in promoter activity than constructs carrying -611A. IFN-γ R1 + 95C/T SNP seems to control the intron-exon splicing process [151].
In conclusion, IFN-γ gene seems to be a good candidate for association with CP. However, larger studies are needed to confirm the relationships of IFN-γ genetic variations and pathogenesis of CP, because the studies have not yielded any strong indication that it might be an important factor in disease susceptibility.
Vitamin D
Vitamin D can control the survival and homeostasis of the cell. It is closely related to the immunomodulatory factors which leads to a reduction of the severity of the inflammation. The combination of vitamin D and its receptor (VDR) induces innate immunity systems through inhibiting the Th1 cell functions and activating the Th2 cell responses [152, 153].
Vitamin D and vitamin D receptor are important mediators of bone metabolism. Dysfunction of these compounds and their gene polymorphisms lead to bone resorption, which is one of the most common complications of the periodontal disease. Also, vitamin D and its receptor can regulate phagocytosis by monocytes [154].
The gene encoding VDR is located on chromosome 12q12–q14. Several studies showed that the VDR gene variations were associated with chronic infectious diseases, especially hepatitis and tuberculosis [155,156,157,158]. However, till now the actual role of the VDR SNPs in CP susceptibility have not been clarified completely. It has been reported that the Fok1 polymorphism may change the expression of the protein, but not the Taq1, Bsm1, and Apa1 polymorphisms [159]. In this regard, it has been identified that VDR SNPs, such as Taq1, Bsm1, Fok1, and Apa1 were associated with CP [58, 160,161,162,163,164,165,166,167]. The carriage rates of the VDR Taq1R-allele were 4–23% in Asian populations [163, 164] which were significantly lower than other ethnic populations (42–78%). In some studies, the Taq1N-allele has been related to CP susceptibility. There was not an association between VDR Bsm1 SNP and CP [160,161,162]. Given that the VDR gene can affect both immune functions and bone metabolism, therefore, VDR SNPs, specially the VDR Taq1 may be risk factors for CP susceptibility. Further studies should be undertaken to confirm the current preliminary data.
Summary and conclusions
Infections can be affected by host genetic factors. The aim of the current review is to provide prognostic genetic markers for detection of the susceptibility of an individual to the chronic periodontitis. Genetic varieties can affect the function of the immune system by changing the transcription of immune factors.
Complex diseases, such as inflammatory bowel disease, type 2 diabetes and many other immune-mediated diseases, share a number of genetic risk variants. In this regard, if a candidate gene has an effect on multiple phenotypes, the pleiotropy occurs. Recently, the effects of pleiotropy in the pathogenesis of complex diseases have been studied [168]. Pleiotropy is associated with many SNPs recorded in the National Human Genome Research Institute (https://www.genome.gov/) brochure. It is interesting to note that in the genes that mediate the immune diseases pleiotropy increases. This definition can improve identifying the risk factors for CP. Therefore, a gene that was recognized as a risk factor for an inflammatory infectious disease might have a similar effect in the process of developing periodontal diseases. For example, IL-10 and 28B, which are important risk factors for hepatitis B virus infection may also be associated with CP. Finally, the overlap of genetic risk factors among diseases may be a useful reason, to analysis such genetic variations in CP. These studies can identify precisely the heritability of CP. As mentioned above, there are a large number of host genetic factors that are believed to be associated with CP susceptibility. It seems that single allelic variants are responsible for disease susceptibility. The most successful example is the identification of SNPs in different cytokine genes in CP.
A genetic variation may be a risk factor for a disease in one population but not for other populations. As the genotype and allele frequencies are vary between different ethnic and geographical populations. With regard to this issue, the studies show that, the IL-1α − 889, IL-1β + 3954, IL1RN VNTR, IL-6-174, IL-10-1087, TNF-α-308, TGF-β1–29, IFN-γ + 874, VDR TaqI and BsmI SNPs were polymorphic in Caucasian in contrast to Asian populations. It means that, ethnic background can change the association between SNPs and disease susceptibility.
Another important point is the accurate disease phenotype definition. There are two forms of periodontitis, which have some similar clinical symptoms: chronic periodontitis and aggressive periodontitis. Therefore, correct disease classification should be used in patient selection.
The studies with regard to the identifying significant genetic factors for susceptibility to chronic periodontitis are not reproducible always. There are differences among the various studies for some SNPs. Nevertheless, there is some evidence that SNPs in the IL-1α, IL-1β, IL1RN, IL-6, IL-10, TNF-α, TGF-β1, IFN-γ and VDR may be associated with CP susceptibility. These SNPs can change the signaling pathways of Wnt/b-catenin, p53 and JAK/STAT and induce CP. Such signaling pathways are believed to modulate the host immune system and are considered as useful biomarkers for determining CP.
It should be noted that, genetic predisposing to CP is not the only risk factor for disease. The interaction between genetic, bacterial and lifestyle factors can also affect the disease susceptibility. In other words, individual habits, microorganisms and diet can affect the expression of the gene through the changing the individual’s epigenome.
In conclusion, the study has implied the relationship between genetic variations and CP susceptibility and related traits. However, the real mechanism of interaction between these factors and host immunity functions not specified yet. Moreover, genetic factors alone cannot explain pathogenesis of inflammation. Therefore, further investigation of other host genetic and environment factors, by novel technologies are needed. This process provided therapeutic and preventive strategies for CP.
Abbreviations
- CP:
-
Chronic periodontitis
- IFN-γ:
-
Interferon gamma
- IL-1:
-
Interleukin-1
- IL-10:
-
Interleukin-10
- IL-6:
-
Interleukin-6
- SNPs:
-
Single nucleotide polymorphisms
- TGF-β:
-
Transforming growth factor beta
- TNF-α:
-
Tumor necrosis factor alpha
- VDR:
-
Vitamin D receptor
References
Philstrom BL, Michalowicz BS, Johnson NW. Periodontal diseases. Lancet. 2005;366:1809–20.
Heidari Z. The association between Proinflammatory gene polymorphisms and level of gingival tissue degradation in chronic periodontitis. Gene Cell Tissue. 2014;1:2.
Heidari Z, Saberi EA, Mahmoudzadeh-Sagheb H, Farhad-Mollashahi N, Zadfatah F. Stereological analysis of the dental pulp in patients with advanced periodontitis. ZJRMS. 2013;15(7):44–9.
Michalowicz BS, Aeppli D, Virag JG, Klump DG, Hinrichs JE, Segal NL. Periodontal findings in adult t wins. J Periodontol. 1991;62:293–9.
Michalowicz BS, Aeppli DP, Kuba RK, Bereuter JE, Conry JP, Segal NL. A twin study of genetic variation in proportional radiographic alveolar bone height. J Dent Res. 1991;70:1431–5.
Hart TC, Marazita ML, Wright JT. The impact of molecular genetics on oral health paradigms. Crit Rev Oral Biol Med. 2000;1:26–56.
Risch N, Merikangas K. The future of genetic studies of complex human diseases. Science. 1996;273:1516–7.
Heidari Z, Mahmoudzadeh-Sagheb H, Hashemi M, Ansarimoghaddam S, Moudi B, Sheibak N. Association between IFN-γ +874 A/T and IFN-γR1 (−611A/G, +189T/G and +95C/T) gene polymorphisms and chronic periodontitis in a sample of Iranian population. Int J Dent. 2015;2015. https://doi.org/10.1155/2015/375359.
Heidari Z, Mahmoudzadeh-Sagheb H, Hashemi M, Rigi Ladez MA. Stereological analysis of interdental gingiva in chronic periodontitis patients with tumor necrosis factor alpha (−308G/a) gene polymorphisms. GCT. 2014;1(1):e18315.
Heidari Z, Mahmoudzadeh-Sagheb H, Rigi-Ladiz MA, Taheri M, Moazenni-Roodi A, Hashemi M. Association of TGF-β1− 509 C/T, 29 C/T and 788 C/T gene polymorphisms with chronic periodontitis: a case–control study. Gene. 2013;518(2):330–4.
Heidari Z, Mahmoudzadeh-Sagheb H, Sheibak N. Sssociation between TGF-BETA1 (−509) C/T gene polymorphism and tissue degradation level in chronic peridontitis: a stereological study. GCT. 2015;2(3):e31698.
Heidari Z, Mahmoudzadeh-Sagheb HR, Hashemi M, Rigi-Ladiz MA. Quantitative analysis of interdental gingiva in patients with chronic periodontitis and transforming growth factor-β1 29C/T gene polymorphisms. J Periodontol. 2014;85(2):281–9.
Archana PM, Salman AA, Kumar TS, Saraswathi PK, Panishankar KH, Kumarasamy P. Association between interleukin-1 gene polymorphism and severity of chronic periodontitis in a south Indian population group. J Indian Soc Periodontol. 2012;16(2):174–8.
Ricci M, Garoia F, Tabarroni C, Marchisio O, Barone A, Genovesi A, Covani U. Association between genetic risk score and periodontitis onset and progression: a pilot study. Arch Oral Biol. 2011;56(12):1499–505.
Deng JS, Qin P, Li XX, Du YH. Association between interleukin-1beta C (3953/4)T polymorphism and chronic periodontitis: evidence from a meta-analysis. Hum Immunol. 2013;74(3):371–8.
Song GG, Choi SJ, Ji JD, Lee YH. Association between tumor necrosis factor-alpha promoter −308 a/G, −238 a/G, interleukin-6 -174 G/C and −572 G/C polymorphisms and periodontal disease: a meta-analysis. Mol Biol Rep. 2013;40(8):5191–203.
Sharma N, Joseph R, Arun R, Chandni R, Srinivas KL, Banerjee M. Cytokine gene polymorphism (interleukin-1beta +3954, Interleukin-6 [−597/−174] and tumor necrosis factor-alpha −308) in chronic periodontitis with and without type 2 diabetes mellitus. Indian J Dent Res. 2014;25(3):375–80.
Scapoli L, Girardi A, Palmieri A, Carinci F, Testori T, Zuffetti F, Monguzzi R, Lauritano D. IL6 and IL10 are genetic susceptibility factors of periodontal disease. Dent Res J. 2012;9(Suppl 2):1735–3327.
Cantore S, Mirgaldi R, Ballini A, Coscia MF, Scacco S, Papa F, Inchingolo F, Dipalma G, De Vito D. Cytokine gene polymorphisms associate with microbiogical agents in periodontal disease: our experience. Int J Med Sci. 2014;11(7):674–9.
Simi A, Tsakiri N, Wang P, Rothwell NJ. Interleukin-1 and inflammatory neurodegeneration. Biochem Soc Trans. 2007;35(5):1122–6.
Dinarello CA. Interleukin-1 in the pathogenesis and treatment of inflammatory diseases. Blood. 2011;117(14):3720–32.
Stashenko P, Fujiyoshi P, Obernesser MS, Prostak L, Haffajee AD, Socransky SS. Levels of interleukin 1 beta in tissue from sites of active periodontal disease. J Clin Periodontol. 1991;18(7):548–54.
Ishihara Y, Nishihara T, Kuroyanagi T. Gingival crevicular interleukin-1 and interleukin-1 receptor antagonist levels in periodontally healthy and diseased sites. J Periodontal Res. 1997;32(6):524–9.
Atanasovska-Stojanovska A, Popovska M, Trajkov D, Spiroski M. IL1 cluster gene polymorphisms in Macedonian patients with chronic periodontitis. Bratisl Lek Listy. 2013;114(7):380–5.
Lavu V, Venkatesan V, Venkata Kameswara Subrahmanya Lakkakula B, Venugopal P, Paul SF, Rao SR. Polymorphic regions in the interleukin-1 gene and susceptibility to chronic periodontitis: a genetic association study. Genet Test Mol Biomarkers. 2015;19(4):175–81.
Hao L, Li JL, Yue Y, Tian Y, Wang M, Loo WT, Cheung MN, Chow LW, Liu Q, Yip AY, et al. Application of interleukin-1 genes and proteins to monitor the status of chronic periodontitis. Int J Biol Markers. 2013;28(1):92–9.
Karimbux NY, Saraiya VM, Elangovan S, Allareddy V, Kinnunen T, Kornman KS, Duff GW. Interleukin-1 gene polymorphisms and chronic periodontitis in adult whites: a systematic review and meta-analysis. J Periodontol. 2012;83(11):1407–19.
Mao M, Zeng XT, Ma T, He W, Zhang C, Zhou J. Interleukin-1alpha −899 (+4845) C-->T polymorphism increases the risk of chronic periodontitis: evidence from a meta-analysis of 23 case-control studies. Gene. 2013;532(1):114–9.
Yin WT, Pan YP, Lin L. Association between IL-1alpha rs17561 and IL-1beta rs1143634 polymorphisms and periodontitis: a meta-analysis. Genet Mol Res. 2016;15(1):15017325.
Zeng XT, Liu DY, Kwong JS, Leng WD, Xia LY, Mao M. Meta-analysis of association between interleukin-1beta C-511T polymorphism and chronic periodontitis susceptibility. J Periodontol. 2015;86(6):812–9.
Boukortt KN, Saidi-Ouahrani N, Boukerzaza B, Ouhaibi-Djellouli H, Hachmaoui K, Benaissa FZ, Taleb L, Drabla-Ouahrani H, Deba T, Ouledhamou SA, et al. Association analysis of the IL-1 gene cluster polymorphisms with aggressive and chronic periodontitis in the Algerian population. Arch Oral Biol. 2015;60(10):1463–70.
Kornman KS, Crane A, Wang HY, di Giovine FS, Newman MG, Pirk FW. The interleukin-1 genotype as a severity factor in adult periodontal disease. J Clin Periodontol. 1997;24:72–7.
Kinane DF, Hart TC. Gene and gene polymorphisms associated with periodontal disease. Critical Reviews in Oral Biology & Medicine. 2003;14:430–49.
Shiroddria S, Smith J, McKay IJ, Kennett CN, Hughes FJ. Polymorphisms in the IL-1A gene are correlated with levels of interleukin-1α protein in gingival crevicular fluid of teeth with severe periodontal disease. J Dent Res. 2000;79(11):1864–9.
Pociot F, Molvig J, Wogensen L, Worsaae H, Nerup J. A TaqI polymorphism in the human interleukin-1β (IL1β)genecorrelateswithIL-1β secretioninvitro. Eur J Clin Investig. 1992;22(6):396–402.
Andus T, Daig R, Vogl D. Imbalance of the interleukin 1 system in colonic mucosa—association with intestinal inflammation and interleukin 1 receptor agonist genotype 2. Gut. 1997;41(5):651–7.
Engebretson SP, Lamster IB, HerreraAbreu M, Celenti RS, Timms JM, Chaudhary AG, di Giovine FS, Kornman KS. The influence of interleukin gene polymorphism on expression of interleukin-1beta and tumor necrosis factor-alpha in periodontal tissue and gingival crevicular fluid. J Periodontol. 1999;70:567–73.
Kobayashi T, Ito S, Kuroda T. The interleukin-1 and Fcγ receptor gene polymorphisms in Japanese patients with rheumatoid arthritis and periodontitis. J Periodontol. 2007;78(12):2311–8.
Anusaksathien O, Sukboon A, Sitthiphong P, Teanpaisan R. Distribution of interleukin-1β+3954 and IL1α−889 genetic variations in a Thai population group. J Periodontol. 2003;74(12):1796–802.
Li QY, Zhao HS, Meng HX, Zhang L, Xu L, Chen ZB, Shi D, Feng XH, Zhu XL. Association analysis between interleukin-1 family polymorphisms and generalized aggressive periodontitis in a Chinese population. J Periodontol. 2004;12:1627–35.
Moreira PR, Costa JE, Gomez RS, Gollob KJ, Dutra WO. The IL1A (−889) gene polymorphism is associated with chronic periodontal disease in a sample of Brazilian individuals. J Periodontal Res. 2007;42(1):23–30.
Laine ML, Farre MA, Gonzalez G, van Dijk LJ, Ham AJ, Winkel EG, Crusius JB, Vandenbroucke JP, van Winkelhoff AJ, Pena AS. Polymorphisms of the interleukin-1 gene family, oral microbial pathogens, smoking in adult periodontitis. J Dent Res. 2001;8:1695–9.
Wagner J, Kaminski WE, Aslanidis C. Prevalence of OPG and IL-1 gene polymorphisms in chronic periodontitis. J Clin Periodontol. 2007;34(10):823–7.
Wu X, Offenbacher S, Lomicronpez NJ, Chen D, Wang HY, Rogus J, Zhou J, Beck J, Jiang S, Bao X, et al. Association of interleukin-1 gene variations with moderate to severe chronic periodontitis in multiple ethnicities. J Periodontal Res. 2015;50(1):52–61.
Ma L, Chu WM, Zhu J, Wu YN, Wang ZL. Interleukin-1β (3953/4) C→T polymorphism increases the risk of chronic periodontitis in Asians: evidence from a meta-analysis of 20 case-control studies. Arch Med Sci. 2015;11(2):267–73.
Soga Y, Nishimura F, Ohyama H, Maeda H, Takashiba S, Murayama Y. Tumor necrosis factor-alpha gene (TNFα)−1031/−863,−857 single-nucleotide polymorphisms (SNPs) are associated with severe adult periodontitis in Japanese. J Clin Periodontol. 2003;30(6):524–31.
Lopez NJ, Jara L, Valenzuela CY. Association of interleukin-1 polymorphisms with periodontal disease. J Periodontol. 2005;2:234–43.
Moreira PR, de Sa AR, Xavier GM. A functional interleukin-1 β gene polymorphism is associated with chronic periodontitis in a sample of Brazilian individuals. J Periodontal Res. 2005;40(4):306–11.
Galbraith GM, Hendley TM, Sanders JJ. Polymorphic cytokine genotypes as markers of disease severity in adult periodontitis. J Clin Periodontal. 1999;26(11):705–9.
Gore EA, Sanders JJ, Pandey JP, Palesh Y, Galbraith GMP. Interleukin1-beta allele2: association with disease status in adult periodontitis. J Clin Periodontol. 1998;25:781–5.
Rogers MA, Figliomeni L, Baluchova K. Do interleukin-1 polymorphisms predict the development of periodontitis or the success of dental implants? J Periodontal Res. 2002;37(1):37–41.
Struch F, Dau M, Schwahn C, Biffar R, Kocher T, Meisel P. Interleukin-1 gene polymorphism, diabetes, and periodontitis: results from the study of health in Pomerania (SHIP). J Periodontol. 2008;79(3):501–7.
Isaza-Guzmán DM, Hernández-Viana M, Bonilla-León DM, Hurtado-Cadavid MC, Tobón-Arroyave SI. Determination of NLRP3 (rs4612666) and IL-1B (rs1143634) genetic polymorphisms in periodontally diseased and healthy subjects. Arch Oral Biol. 2016;65:44–51.
Mendonca SA, Teixeira FG, Oliveira KM, Santos DB, Marques LM, Amorim MM, Gestinari Rde S. Study of the association between the interleukin-1 beta c.3954C>T polymorphism and periodontitis in a population sample from Bahia, Brazil. Contemp Clin Dent. 2015;6(2):176–82.
Amirisetty R, Patel RP, Das S, Saraf J, Jyothy A, Munshi A. Interleukin 1beta (+3954, −511 and −31) polymorphism in chronic periodontitis patients from North India. Acta Odontol Scand. 2015;73(5):343–7.
Masamatti SS, Kumar A, Baron TK, Mehta DS, Bhat K. Evaluation of interleukin -1B (+3954) gene polymorphism in patients with chronic and aggressive periodontitis: a genetic association study. Contemp Clin Dent. 2012;3(2):144–9.
Geismar K, Enevold C, Sorensen LK. Involvement of interleukin-1 genotypes in the association of coronary heart disease with periodontitis. J Periodontol. 2008;79(12):2322–30.
Brett PM, Zygogianni P, Griffths GS. Functional gene polymorphisms in aggressive and chronic periodontitis. JournalofDentalResearch. 2005;48(12):1149–53.
Ding C, Zhao L, Sun Y, Li L, Xu Y. Interleukin-1 receptor antagonist polymorphism (rs2234663) and periodontitis susceptibility: a meta-analysis. Arch Oral Biol. 2012;57(6):585–93.
Berdeli A, Emingil G, Gurkan A, Atilla G, Kose T. Association of the IL-1RN2 allele with periodontal diseases. Clin Biochem. 2006;39(4):357–62.
Armitage GC, Wu Y, Wang HY, Sorrell J, Di Giovine FS, Duff GW. Low prevalence of a periodontitis-associated interleukin-1 composite genotype in individuals of Chinese heritage. J Periodontol. 2000;71(2):164–71.
McDevitt MJ, Wang HY, Knobelman C. Interleukin-1 genetic association with periodontitis in clinical practice. J Periodontol. 2000;71(2):156–63.
Agrawal AA, Kapley A, Yeltiwar RK, Purohit HJ. Assessment of single nucleotide polymorphism at IL1A+4845 and IL-1B+3954 as genetic susceptibility test for chronic periodontitis in Maharashtrian ethnicity. J Periodontol. 2006;77(9):1515–21.
Meisel P, Siegemund A, Grimm R. The interleukin-1 polymorphism, smoking, and the risk of periodontal disease in the population-based SHIP study. J Dent Res. 2003;82(3):189–93.
Socransky SS, Haffajee AD, Smith C, Duff GW. Microbiological parameters associated with IL-1 gene polymorphisms in periodontitis patients. J Clin Periodontol. 2000;27(11):810–8.
Scheller J, Chalaris A, Schmidt-Arras D, Rose-John S. The pro- and anti-inflammatory properties of the cytokine interleukin-6. Biochim Biophys Acta. 2011;1813:878–88.
Sanchooli T, Heidari Z, Mahmoudzadeh-Sagheb H, Hashemi M, Rigi Ladez MA. The relationship between Interleukin-6 -174 G/C gene polymorphism and chronic periodontitis. Zahedan J Res Med Sci. 2012;14(3):13–7.
Erciyas K, Pehlivan S, Sever T, Igci M, Arslan A, Orbak R. Association between TNF-a, TGF-ß1, IL-10, IL-6 and IFN-g gene polymorphisms and generalized aggressive periodontitis. Clin Invest Med. 2010;33(2):85–91.
Mesa F, O’Valle F, Rizzo M, Cappello F, Donos N, Chaudhary N. Association between COX-2 rs 6681231 genotype and Interleukin-6 in periodontal connective tissue. A Pilot Study. PLOS ONE. 2014;9(2):1–6.
Fishman D, Faulds G, Jeffery R, Mohamed-Ali V, Yudkin JS, Humphries S, Woo P. The effect of novel polymorphisms in the interleukin-6 (IL-6) gene on IL-6 transcription and plasma IL-6 levels, and an association with systemic-onset juvenile chronic arthritis. J Clin Invest. 1998;102:1369–76.
Moreira PR, Lima PMA, Sathler KOB. Interleukin-6 expression and gene polymorphism are associated with severity of periodontal disease in a sample of Brazilian individuals. Clin Exp Immunol. 2007;148(1):119–26.
Trevilatto PC, Scarel-Caminaga RM, de Brito RB Jr, de Souza AP, SRP L. Polymorphism at position −174 of IL-6 gene is associated with susceptibility to chronic periodontitis in a Caucasian Brazilian population. J Clin Periodontol. 2003;30(5):438–42.
Gabriela Teixeira F, Mendonca SA, Menezes Oliveira K, Barbosa Dos Santos D, Miranda Marques L, Mendonca Amorim M, de Souza Gestinari R. Interleukin-6 c.-174G>C Polymorphism and Periodontitis in a Brazilian Population. Mol Biol Int. 2014;490308(10):4.
Babel N, Cherepnev G, Babel D. Analysis of tumor necrosis factor-β, transforming growth factor-β, interleukin10, IL-6, and interferon-γ gene polymorphisms in patients with chronic periodontitis. J Periodontol. 2006;77(12):1978–83.
Tervonen T, Raunio T, Knuuttila M, Karttunen R. Polymorphisms in the CD14 and IL-6 genes associated with periodontal disease. J Clin Periodontol. 2007;34(5):377–83.
Komatsu K, Tai H, Galicia JC. Interleukin-6 (IL6)—373 A9T11 allele is associated with reduced susceptibility to chronic periodontitis in Japanese subjects and decreased serum IL-6 level. Tissue Antigens. 2005;65(1):110–4.
Heidari Z, Mahmoudzadeh-Sagheb H, Hashemi M, Ansarimoghaddam S, Sheibak N. Estimation of volume density of interdental papilla components in patients with chronic periodontitis and interleukin-6 (−174G/C) gene polymorphisms. Dent Res J. 2016;13(2):139–44.
Nibali L, D’Aiuto F, Donos N, Griffiths GS, Parkar M, Tonetti MS. Association between periodontitis and common variants in the promoter of the interleukin-6 gene. Cytokine. 2009;45:50–4.
Holla LI, Fassmann A, Stejskalova A, Znojil V, Vanek J, Vacha J. Analysis of the interleukin-6 gene promoter polymorphisms in Czech patients with chronic periodontitis. J Periodontol. 2004;75(1):30–6.
Zhang HY, Feng L, Wu H, Xie XD. The association of IL-6 and IL-6R gene polymorphisms with chronic periodontitis in a Chinese population. Oral Dis. 2014;20(1):69–75.
Nikolopoulos GK, Dimou NL, Hamodrakas SJ, Bagos PG. Cytokine gene polymorphisms in periodontal disease: a meta-analysis of 53 studies including 4178 cases and 4590 controls. J Clin Periodontol. 2008;35(9):754–67.
Preshaw PM, Taylor JJ. How has research into cytokine interactions and their role in driving immune responses impacted our understanding of periodontitis? J Clin Periodontol. 2011;38:60–84.
Dentino A, Lee S, Mailhot J, Hefti AF. Principles of periodontology. Periodontol. 2000;2013(61):16–53.
Bazzoni F, Tamassia N, Rossato M, Cassatella MA. Understanding the molecular mechanisms of the multifac- eted IL-10-mediated antiinflammatory response: lessons from neutrophils. Eur J Immunol. 2010;40:2360–8.
Sabat R, Grutz G, Warszawska K. Biology of interleukin-10. Cytokine Growth Factor Rev. 2010;21:331–44.
Ouyang W, Rutz S, Crellin NK, Valdez PA, Hymowitz SG. Regulation and functions of the IL-10 family of cytokines in inflammation and disease. Annu Rev Immunol. 2011;29:71–109.
Jin X, Hu Z, Kang Y, Liu C, Zhou Y, Wu X. Association of IL-10-1082 G/G genot ype with lower mor talit y of acute respiratory distress syndrome in a Chinese population. Mol Biol Rep. 2012;39:1–4.
Zhang G, Manaca MN, McNamara-Smith M, Mayor A, Nhabomb AN, Berthoud TK. Interleukin-10 (IL-10) polymorphisms are associated with IL-10 production and clinical malaria in Young children. Infect Immun. 2012;80:2316–22.
Moudi B, Heidari Z, Mahmoudzadeh-Sagheb H, Hashemi M. Association between IL-10 gene promoter polymorphisms (−592 A/C, −819 T/C, −1082 A/G) and susceptibility to HBV infection in an Iranian population. Hepat Mon. 2016;16(2). https://doi.org/10.5812/hepatmon.32427.
Berglundh T, Donati M, Hahn-Zoric M, Hanson LA, Padyukov L. Association of the-1087 IL 10 gene polymorphism with severe chronic periodontitis in Swedish Caucasians. J Clin Periodontol. 2003;30:249–54.
Scarel-Caminaga RM, Trevilatto PC, Souza AP, Brito RB, Camargo LE, Line SR. Interleukin 10 gene promoter polymorphisms are associated with chronic periodontitis. J Clin Periodontol. 2004;31:443–8.
Sumer AP, Kara N, Keles GC, Gunes S, Koprulu H, Bagci H. Association of interleukin-10 gene polymorphisms with severe generalized chronic periodontitis. J Periodontol. 2007;78:493–7.
Atanasovska-Stojanovska A, Trajkov D, Popovska M, Spiroski M. IL10–1082, IL10–819 and IL10–592 polymorphisms are associated with chronic periodontitis in a Macedonian population. Hum Immunol. 2012;73(7):753–8.
Zhong Q, Ding C, Wang M, Sun Y, Xu Y. Interleukin-10 gene polymorphisms and chronic/aggressive periodontitis susceptibility: a meta-analysis based on 14 case-control studies. Cytokine. 2012;60(1):47–54.
Albuquerque CM, Cortinhas AJ, Morinha FJ, Leitao JC, Viegas CA, Bastos EM. Association of the IL-10 polymorphisms and periodontitis: a meta-analysis. Mol Biol Rep. 2012;39(10):9319–29.
Crena J, Subramanian S, Victor DJ, Gnana PP, Ramanathan A. Single nucleotide polymorphism at −1087 locus of interleukin-10 gene promoter is associated with severe chronic periodontitis in nonsmoking patients. Eur J Dent. 2015;9(3):387–93.
Jaradat SM, Ababneh KT, Jaradat SA, Abbadi MS, Taha AH, Karasneh JA, Haddad HI. Association of interleukin-10 gene promoter polymorphisms with chronic and aggressive periodontitis. Oral Dis. 2012;18(3):271–9.
Hannum R, Godoy FR, da Cruz AS, Vieira TC, Minasi LB, de M E Silva D, da Silva CC, da Cruz AD. Lack of association between IL-10 -1082G/a polymorphism and chronic periodontal disease in adults. Genet Mol Res. 2015;14(4):17828–33.
Chambrone L, Ascarza A, Guerrero ME, Pannuti C, de la Rosa M, Salinas-Prieto E, Mendoza G. Association of −1082 interleukin-10 gene polymorphism in Peruvian adults with chronic periodontitis. Med Oral Patol Oral Cir Bucal. 2014;19(6):e569–73.
Crawley E, Kay R, Sillibourne J, Patel P, Hutchinson I, Woo P. Polymorphic haplotypes of the interleukin-10 5′ flanking region determine variable interleukin-10 transcription and are associated with particular phenotypes of juvenile rheumatoid arthritis. Arthritis Rheum. 1999;42(6):1101–8.
Koss K, Satsangi J, Fanning GC, Welsh KI, Jewell DP. Cytokine (TNF alpha, LT alpha and IL-10) polymorphisms in inflammatory bowel diseases and normal controls: differential effects on production and allele frequencies. Genes Immun. 2000;1(3):185–90.
Claudino M, Trombone AFP, Cardoso CR. The broad effects of the functional IL-10 promoter-592 polymorphism: modulation of IL-10, TIMP-3, and OPG expression and their association with periodontal disease outcome. J Leukoc Biol. 2008;48(6):1565–73.
Garlet GP, Martins JRW, Fonseca BA, Ferreira BR, Silva JS. Matrix metalloproteinases, their physiological inhibitors and osteoclast factors are differentially regulated by the cytokine profile in human periodontal disease. JClin Periodontol. 2004;31(8):671–9.
Zhang X, Teng YT. Interleukin-10 inhibits gram-negative-microbe-specific human receptor activator of NF-kappaB ligand-positive CD4+-Th1-cellassociated alveolar bone loss in vivo. Infect Immun. 2006;74(8):4927–31.
Reichert S, Machulla HK, Klapproth J, Zimmermann U, Reichert Y, Glaser CH. He interleukin-10 promoter haplotype ATA is a putative risk factor for aggressive periodontitis. J Periodontal Res. 2008;43:40–7.
Yamazaki K, Tabeta K, Nakajima T. Interleukin10 gene promoter polymorphism in Japanese patients with adult and early-onset periodontitis. J Clin Periodontol. 2001;28(9):828–32.
Locksley RM, Killeen N, Lenardo MJ. The TNF and TNF receptor superfamilies: integrating mammalian biology. Cell. 2001;104(4):487–501.
Solhjoo S, Mahmoudzadeh-Sagheb H, Heidari Z, Hashemi M, Rigi Ladez MA. Association between TNF-α (− 308 G → a) gene polymorphism and chronic periodontitis. Zahedan J Res Med Sci. 2014;16(2):10–4.
Victor FC, Gottlieb AB. TNF-alpha and apoptosis: implications for the pathogenesis and treatment of psoriasis. J Drugs Dermatol. 2002;1(3):264–75.
Brynskov J, Foegh P, Pedersen G, Ellervik C, Kirkegaard T, Bingham A, Saermark T. Tumour necrosis factor alpha converting enzyme (TACE) activity in the colonic mucosa of patients with inflammatory bowel disease. Gut. 2002;51(1):37–43.
Fassmann A, Holla LI, Buckova D, Vasku A, Znojil V, Vanek J. Polymorphisms in the +252(a/G) lymphotoxinalpha and the −308(a/G) tumor necrosis factor-alpha genes and susceptibility to chronic periodontitis in a Czech population. J Periodontal Res. 2003;38(4):394–9.
Menezes NG, Colombo AP. Lack of association between the TNF-α-308(G/a)genetic polymorphism and periodontal disease in Brazilians. Braz Oral Res. 2008;22(4):322–7.
Nedwin GE, Naylor SL, Sakaguchi AY, Smith D, Jarrett-Nedwin J, Pennica D, Goeddel DV, Gray PW. Human lymphotoxin and tumor necrosis factor genes: structure, homology and chromosomal localization. Nucleic Acids Res. 1985;13(17):6361–73.
Yang W, Jia Y, Wu H. Four tumor necrosis factor alpha genes polymorphisms and periodontitis risk in a Chinese population. Hum Immunol. 2013;74(12):1684–7.
Ding C, Ji X, Chen X, Xu Y, Zhong L. TNF-a gene promoter polymorphisms contribute to periodontitis susceptibility: evidence from 46 studies. J Clin Periodontol. 2014;41:748–59.
Ozer Yucel O, Berker E, Mesci L, Eratalay K, Tepe E, Tezcan I. Analysis of TNF-alpha (−308) polymorphism and gingival crevicular fluid TNF-alpha levels in aggressive and chronic periodontitis: a preliminary report. Cytokine. 2015;72(2):173–7.
Schulz S, Machulla HKG, Altermann W. Genetic markersoftumournecrosisfactorα in aggressive and chronic periodontitis. J Clin Periodontol. 2008;35(6):493–500.
Donati M, Berglundh T, Hytonen AM, Hahn-Zoric M, Hanson LA, Padyukov L. Association of the−159 CD14 gene polymorphism and lack of association of the −308 TNFA and Q551R IL-4RA polymorphisms with severe chronic periodontitis in Swedish Caucasians. J Clin Periodontol. 2005;32(5):474–9.
Folwaczny M, Glas J, Torok HP, Mende M, Folwaczny C. Lack of association between the TNF α G−308A promoter polymorphism and periodontal disease. J Clin Periodontol. 2004;31(6):449–53.
Galbraith GMP, Steed RB, Sanders JJ, Pandey JP. Tumor necrosis factor alpha production by oral leukocytes: influence of tumor necrosis factor genotype. J Periodontol. 1998;69(4):428–33.
Sakellari D, Katsares V, Georgiadou M, Kouvatsi A, Arsenakis M, Konstantinidis A. No correlation of five gene polymorphisms with periodontal conditions in a Greek population. J Clin Periodontol. 2006;33(11):765–70.
Hanafy SM, Ado A. Impact of single nucleotide polymorphism of TGF-β1 gene (SNP-Codon10) on hepatocellular carcinoma risk in Egyptian patients following HCV infection. Aust J Basic Appl Sci. 2011;5:1814–21.
Xiao YQ, Freire-de-Lima CG, Schiemann WP, Bratton DL, Vandivier RW, Henson PM. Transcriptional and translational regulation of TGF-beta production in response to apoptotic cells. J Immunol. 2008;181:3575–85.
Verrecchia F, Mauviel A. Transforming growth factor-beta signaling through the Smad pathway: role in extracellular matrix gene expression and regulation. J Invest Dermatol. 2002;118(2):211–5.
Vikram V, Ramakrishnan T, Anilkumar K, Ambalavanan N. Changes in transforming growth factor-beta1 in gingival Crevicular fluid of patients with chronic periodontitis following periodontal flap surgery. J Clin Diagn Res. 2015;9(2):1.
Mize TW, Sundararaj KP, Leite RS, Huang Y. Increased and correlated expression of connective tissue growth factor and transforming growth factor beta 1 in surgically removed periodontal tissues with chronic periodontitis. J Periodontal Res. 2015;50(3):315–9.
Ernst CW, Lee JE, Nakanishi T, Karimbux NY, Rezende TM, Stashenko P, Seki M, Taubman MA, Kawai T. Diminished forkhead box P3/CD25 double-positive T regulatory cells are associated with the increased nuclear factor-kappaB ligand (RANKL+) T cells in bone resorption lesion of periodontal disease. Clin Exp Immunol. 2007;148(2):271–80.
Khalaf H, Lonn J, Bengtsson T. Cytokines and chemokines are differentially expressed in patients with periodontitis: possible role for TGF-beta1 as a marker for disease progression. Cytokine. 2014;67(1):29–35.
Holla LI, Fassmann A, Benes P, Halabala T, Znojil V. 5 polymorphisms in the transforming growth factor-beta 1 gene (TGF-beta 1) in adult periodontitis. J Clin Periodontol. 2002;29(4):336–41.
Kobayashi T, Murasawa A, Ito S, Yamamoto K, Komatsu Y, Abe A. Cytokine gene polymorphisms associated with rheumatoid arthritis and periodontitis in Japanese adults. J Periodontol. 2009;80:792–9.
Atilla G, Emingil G, Kose T, Berdeli A. TGF-beta1 gene polymorphisms in periodontal diseases. Clin Biochem. 2006;39(9):929–34.
de Souza AP, Trevilatto PC, Scarel-Caminaga RM, de Brito RB, Line SR. Analysis of the TGF-beta1 promoter polymorphism (C-509T) in patients with chronic periodontitis. J Clin Periodontol. 2003;30(6):519–23.
Cui L, Sun YP, Li DG, Wang SH, Shao D. Transforming growth factor-beta1 rs1800469 polymorphism and periodontitis risk: a meta-analysis. Int J Clin Exp Med. 2015;8(9):15569–74.
Atanasovska-Stojanovska A, Trajkov D, Popovska M, Spiroski M. Analysis ofTransforming growth factor-Beta1 GenePolymorphisms in Macedonian patients with ChronicPeriodontitis. Macedonian Journal of Medical Sciences. 2009;2(1):30–5.
Babel N, Cherepnev G, Babel D, Tropmann A, Hammer M, Volk HD, Reinke P. Analysis of tumor necrosis factor-alpha, transforming growth factor-beta, interleukin-10, IL-6, and interferon-gamma gene polymorphisms in patients with chronic periodontitis. J Periodontol. 2006;77(12):1978–83.
Schoenborn JR, Wilson CB. Regulation of interferon-gamma during innate and adaptive immune responses. Adv Immunol. 2007;96:41–101.
Honda T, Domon H, Okui T, Kajita K, Amanuma R, Yamazaki K. Balance of inflammatory response in stable gingivitis and progressive periodontitis lesions. Clin Exp Immunol. 2006;144:35–40.
Dutzan N, Vernal R, Hernandez M, Dezerega A, Rivera O, Silva N, Aguillon JC, Puente J, Pozo P, Gamonal J. Levels of interferon-gamma and transcription factor T-bet in progressive periodontal lesions in patients with chronic periodontitis. J Periodontol. 2009;80(2):290–6.
Sadir R, Forest E, Lortat-Jacob H. The heparan sulfate binding sequence of interferon-gamma increased the on rate of the interferon-gamma-interferon-gamma receptor complex formation. J Biol Chem. 1998;273(18):10919–25.
Bream JH, Carrington M, O’Toole S. Polymorphisms of the human IFNG gene noncoding regions. Immunogenetics. 2000;51:50–8.
Pravica V, Asderakis A, Perrey C. In vitro production of IFN-gamma correlates with CA repeat polymorphism in the human IFN-gamma gene. Eur J Immunogenet. 1999;26:1–3.
Huang Y, Yang H, Borg BB. A functional SNP of interferon-gamma gene is important for interferon-alpha-induced and spontaneous recovery from hepatitis C virus infection. Proc Natl Acad Sci U S A. 2007;104:985–90.
Pravica V, Perrey C, Stevens A, Lee JH, Hutchinson IV. A single nucleotide polymorphism in the first intron of the human IFN-gamma gene: absolute correlation with a polymorphic CA microsatellite marker of high IFN-gamma production. Hum Immunol. 2000;61:863–6.
Bream JH, Ping A, Zhang X, Winkler C, Young HA. A single nucleotide polymorphism in the proximal IFN-gamma promoter alters control of gene transcription. Genes Immun. 2002;3(3):165–9.
Reichert S, Machulla HK, Klapproth J, Zimmermann U, Reichert Y, Glaser C, Schaller HG, Schulz S. Interferon-gamma and interleukin-12 gene polymorphisms and their relation to aggressive and chronic periodontitis and key periodontal pathogens. J Periodontol. 2008;79(8):1434–43.
Hooshmand B, Hajilooi M, Rafiei A, Mani-Kashani KH, Ghasemi R. Interleukin-4 (C-590T) and interferon-gamma (G5644A) gene polymorphisms in patients with periodontitis. J Periodontal Res. 2008;43(1):111–5.
Holla LI, Hrdlickova B, Linhartova P, Fassmann A. Interferon-gamma +874A/T polymorphism in relation to generalized chronic periodontitis and the presence of periodontopathic bacteria. Arch Oral Biol. 2011;56(2):153–8.
Loo WTY, Fan CB, Bai LJ, Yue Y, Dou YD, Wang M. Gene polymorphism and protein of human pro-and anti-inflammator y cytokines in Chinese healthy subjects and chronic periodontitis patients. J Transl Med. 2012;10:S8.
Xiang L, Elci OU, Rehm KE, Marshall GD Jr. Associations between cytokine receptor polymorphisms and variability in laboratory immune parameters in normal humans. Hum Immunol. 2014;75(1):91–7.
Rosenzweig SD, Schaffer AA, Ding L, Sullivan R, Enyedi B, Yim JJ, Cook JL, Musser JM, Holland SM. Interferon-gamma receptor 1 promoter polymorphisms: population distribution and functional implications. Clin Immunol. 2004;112(1):113–9.
Lu J, Pan H, Chen Y, Tang S, Feng Y, Qiu S, Zhang S, Wu L, Xu R, Peng X, et al. Genetic polymorphisms of IFNG and IFNGR1 in association with the risk of pulmonary tuberculosis. Gene. 2014;543(1):140–4.
Hewison M. Vitamin D and innate and adaptive immunity. Vitam Horm Vitamins & Hormones. 2011;86:23–62.
Beard JA, Bearden A, Striker R. Vitamin D and the anti-viral state. J Clin Virol. 2011;50(3):194–200.
Selvaraj P, Chandra G, Jawahar MS, Rani MV, Rajeshwari DN, Narayanan PR. Regulatory role of vitamin D receptor gene variants of BsmI, ApaI, TaqI, and FokI polymorphisms on macrophage phagocytosis and lymphoproliferative response to mycobacterium tuberculosis antigen in pulmonary tuberculosis. J Clin Immunol. 2004;24(5):523–32.
Bellamy R, Hill AV. Genetic susceptibility to mycobacteria and other infectious pathogens in humans. Curr Opin Lmmunol. 1998;10:483–7.
Bellamy R, Ruwende C, Corrah T, McAdam KP, Thursz MR, Whittle HC, Hill AV. Tuberculosis and chronic hepatitis B virus infection in Africans and variation in the vitamin D receptor gene. J Infect Dis. 1999;179:721–4.
Roth DE, Soto G, Arenas F. Association between vitamin D receptor gene polymorphisms and response to treatment of pulmonary tuberculosis. J Infect Dis. 2004;190(5):920–7.
Gelder CM, Hart KW, Williams OM. Vitamin D receptor gene polymorphisms and susceptibility to Mycobacterium malmoense pulmonary disease. J Infect Dis. 2000;181(6):2099–102.
Gross C, Eccleshall RT, Malloy PJ, Villa ML, Marcus R, Feldman D. The presence of a polymorphism at the translation initiation site of the vitamin D receptor gene is associated with low bone mineral density in postmenopausal Mexican-American women. J Bone Miner Res. 1996;11(12):1850–5.
Naito M, Miyaki K, Naito T. Association between vitamin D receptor gene haplotypes and chronic periodontitis among Japanese men. Int J Med Sci. 2007;4(4):216–22.
Gunes S, Sumer AP, Keles GC. Analysis of vitamin D receptor gene polymorphisms in patients with chronic periodontitis. Indian J Med Res. 2008;127(1):58–64.
de Brito RB Jr, Scarel-Caminaga RM, Trevilatto PC, de Souza AP, Barros SP. Polymorphisms in the vitamin D receptor gene are associated with periodontal disease. J Periodontol. 2004;75(8):1090–5.
Tachi Y, Shimpuku H, Nosaka Y. Vitamin D receptor gene polymorphism is associated with chronic periodontitis. Life Sci. 2003;73(26):3313–21.
Sun JL, Meng HX, Cao CF. Relationship between vitamin D receptor gene polymorphism and periodontitis. J Periodontal Res. 2002;73(4):263-7.
Kaarthikeyan G, Jayakumar ND, Padmalatha O, Varghese S, Anand B. Analysis of association of TaqI VDR gene polymorphism with the chronic periodontitis in Dravidian ethnicity. Indian J Hum Genet. 2013;19(4):465–8.
Karasneh JA, Ababneh KT, Taha AH, Al-Abbadi MS, Marzouka N, Jaradat SM, Thornhill MH. Association of vitamin D receptor gene polymorphisms with chronic and aggressive periodontitis in Jordanian patients. Eur J Oral Sci. 2013;121(6):551–8.
El Jilani MM, Mohamed AA, Zeglam HB, Alhudiri IM, Ramadan AM, Saleh SS, Elkabir M, Amer IB, Ashammakhi N, Enattah NS. Association between vitamin D receptor gene polymorphisms and chronic periodontitis among Libyans. Libyan J Med. 2015;10:26771.
Sivakumaran S, Agakov F, Theodoratou E, Prendergast JG, Zgaga L, Manolio T, Rudan I, McKeigue P, Wilson JF, Campbell H. Abundant pleiotropy in human complex diseases and traits. Am J Hum Genet. 2011;89(5):607–18.
Shirodaria S, Smith J, McKay IJ, Kennett CN, Hughes FJ. Polymorphisms in the IL-1A gene are correlated with levels of interleukin-1alpha protein in gingival crevicular fluid of teeth with severe periodontal disease. J Dent Res. 2000;79:1864–9.
Bashour L, Khattab R, Harfoush E. The Role of Interleukin-1 Genotype in the Association between Coronary Heart Disease and Periodontitis in a Syrian Population. Hindawi Publishing Corporation ISRN Dentistry Volume 2013. Article ID 195678. https://doi.org/10.1155/2013/195678.
Li Y, Feng G, Deng Y, Song J. Contribution of Interleukin-10-592 (-590, -597) C>A Polymorphisms to Periodontitis Susceptibility: An Updated Meta-Analysis Based on 18 Case-Control Studies. Hindawi Disease Markers 2018. Article ID 2645963. https://doi.org/10.1155/2018/2645963.
Acknowledgements
The authors would like to thank all participants who willingly participated in this study.
Funding
None.
Availability of data and materials
Not applicable.
Author information
Authors and Affiliations
Contributions
BM and ZH and HM-S participated in the sequence alignment and drafted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Heidari, Z., Moudi, B. & Mahmoudzadeh-Sagheb, H. Immunomodulatory factors gene polymorphisms in chronic periodontitis: an overview. BMC Oral Health 19, 29 (2019). https://doi.org/10.1186/s12903-019-0715-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-019-0715-7