Abstract
Background
The impact of the T1 slope minus cervical lordosis (T1S-CL) on surgical outcomes in patients with degenerative cervical myelopathy undergoing laminoplasty (LP) remain uncertain.
Methods
One hundred patients who underwent cervical LP were retrospectively reviewed. Radiographic measurements included C2–C7 lordosis (CL), T1 slope (T1S), and C2–C7 sagittal vertical axis (SVA). Additionally, pain numeric rating scale, neck disability index (NDI), 12-Item Short-Form Health Survey, Euro QOL 5 dimensions (EQ5D), and Japanese Orthopedic Association score were investigated. According to past reports, T1S–CL > 20° was defined as mismatched. Then, based on T1S-CL mismatching, patients were divided into 2 groups.
Results
This research understudied 67 males and 33 females with a mean age of 67 y. Preoperatively, only eight patients showed a T1S-CL mismatch. While the C2–7 Cobb angles did not change significantly after surgery, the T1 slope (T1S) angle increased, increasing the T1S-CL as a result. As we compared the clinical outcomes based on the preoperative T1S-CL mismatching, there were no significant differences between the two groups. On the other hand, the number of patients in the mismatched group increased to 21 patients postoperatively. As we compared clinical outcomes based on the postoperative T1S-CL mismatching, the postoperative NDI score and preop/postop EQ5D score were significantly worse in the mismatch group.
Conclusions
Although cervical LP showed inferior outcomes in patients with postoperative T1S-CL mismatch even in the absence of severe preoperative kyphosis (> 10°), preoperative T1S-CL mismatch was not adversely prognostic.
Similar content being viewed by others
Background
Multiple surgical options for degenerative cervical myelopathy (DCM) have been observed, including posterior decompression and fusion, anterior decompression and fusion, then laminoplasty. As for posterior decompression, preoperative cervical kyphosis was related to poorer neurological improvements because of an insufficient posterior shift of the spinal cord after decompression surgery [1]. Additionally, although postoperative kyphotic changes occur after laminoplasty, the importance of preserving posterior supporting structures has been emphasized [2]. As the number of past papers on thoracolumbar deformity surgeries has increased, the influence of the T1 slope (T1S) on cervical spine surgery has also been attracting growing interest [3, 4]. Remarkably, the association between T1S and cervical lordosis (CL) has been advocated. Several past reports have also investigated the influence of T1S minus CL (T1S-CL) on the surgical outcomes of cervical spine surgery, because the ideal degree of CL is considered to be different, depending on the magnitude of T1S, including two reports on cervical laminoplasty [5, 6]. Besides, past reports included patients who experienced preoperative kyphosis of the cervical spine, which are considered to have affected the surgical results. Therefore, in this study, we solely focused on patients who lacked severe preoperative kyphosis (> 10°) and were considered indicative of laminoplasty. The purpose of this study was to investigate an influence of T1S-CL mismatch on surgical outcomes of cervical laminoplasty in the absence of preoperative kyphosis of > 10°.
Methods
Patient selection
The institutional review board of the authors institution approved the study protocols. We retrospectively reviewed 100 patients with degenerative cervical myelopathy who underwent double-door laminoplasty between 2004 and 2019 and replied to the questionnaires of patient-reported outcomes both pre- and postoperatively. Patients with preoperative kyphosis of > 10° or those without preoperative or postoperative radiographic examinations of the whole spine were excluded. Additionally, patients with rheumatoid arthritis, disc herniation, tumor, trauma, severe lumbar spinal canal stenosis, or previous surgery were also excluded.
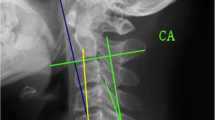
Data collection
Demographic data, including sex, age, and follow-up period, were collected from electronic medical records. Then, clinical data were evaluated using the recovery rating score of the Japanese Orthopedic Association (JOA), which was calculated using the method by Hirabayashi et al. [7]. Subsequently, neck pain was measured using the numerical rating scale (NRS). Patient-reported outcomes included the neck disability index (NDI), 12-Item Short-Form Health Survey (SF-12), and Euro QOL 5 dimensions (EQ5D). Next, pre-and postoperative standing lateral radiographs of the spine were obtained using the upper arms in a neutral hanging position. As for the radiographic parameters, the C2–C7 (CL) lateral Cobb angle, the T1 slope (T1S) angle, the C2–C7 SVA (C2-7SVA), and the T1S-CL were measured. The C2–C7 angle was measured, which was defined by the angle between the inferior end plate of C2 vertebra and the inferior endplate of C7 vertebra. T1-CL > 20° was defined as mismatching [5], and patients were divided into two based on their T1S-CL mismatching scores. Afterward, laminoplasty was conducted using an expansive double-door spinous process-splitting (Kurokawa) method [8]. The LP level depended on the degree of compression. Finally, patients were allowed to walk on the second day after surgery, isometric cervical muscle exercises allowed just after the operation, and collars were not routinely applied except when the patients complained of severe neck pain after surgery.
Statistical analysis
Statistical analyses were conducted using JMP for Windows v.15.0 (JMP® 15 SAS Institute Inc., Cary, NC, USA). Univariate statistical analyses were performed using the Student’s paired and unpaired t-tests. The P-value < 0.05 was considered statistically significant. Finally, Pearson’s correlation coefficient was used to assess correlations between the preoperative and postoperative cervical parameters.
Results
Patients
One hundred (67 males; 33 females) patients were included in this study, including sixty patients with cervical spondylotic myelopathy (CSM) and 40 patients with ossification of the posterior longitudinal ligament (OPLL). The mean age at surgery was 66.9 ± 10.1 years. The mean follow-up period was 31.4 ± 20.9 months (Table 1).
Radiographic and clinical outcomes
The preoperative and postoperative radiographic parameters were moderately to highly correlated, as shown in Table 2 (r = 0.59–0.78). While the C2–7 Cobb angle did not change significantly after surgery, the T1 slope (T1S) angle increased, increasing the T1S-CL as a result (Table 2). As for the clinical outcomes, all values improved postoperatively.
Next, we divided the patients into two groups based on their T1S-CL values. Preoperatively, only eight patients showed mismatches, namely, T1S-CL larger than 20°. Therefore, we compared the clinical outcomes based on the preoperative T1S-CL. Although no significant difference between the two groups was observed, postoperative NDI demonstrated worse scores in the mismatched group (Table 3). Alternatively, results showed a patient increase in the mismatched group to 21 patients postoperatively (Table 4). As we compared clinical outcomes based on the postoperative T1S-CL, the postoperative NDI and preop/postop EQ5D scores were significantly worse in the mismatched group (Table 4).
Discussion
Preoperative cervical kyphosis has been reported to result in poorer surgical outcomes after LP because of an insufficient posterior shifting of the spinal cord based. Therefore, anterior or posterior fixation surgery is considered in patients with preoperative kyphosis. However, even in patients with preoperative CL, previous studies have shown kyphotic alignment changes after LP, and poor prognostic parameters leading to postoperative kyphotic deformities after cervical LP have been reported [9, 10]. For example, Kim et al. [4] considered a high T1 slope a significant predictor of kyphotic alignment changes in patients after laminoplasty. They insisted that surgical trauma to the posterior musculature led to kyphotic deformity, because a high T1 slope represents the possibility of thoracolumbar deformity and a more prominent CL is required in such patients. The relationship between high T1 slope and increased CL is further supported by the fact that patients with a higher T1 slope demonstrated a higher incidence of postoperative interlaminar bony fusion in patients undergoing laminoplasty, possibly because such patients should have increased CL to maintain their head position [11]. Oshima et al. [12] reported that patients with larger C7-SVA showed poor patient-reported outcomes before and after surgery after adjusting for age using propensity scores. They also observed that although patients with a global imbalance also demonstrated cervical imbalance, which was considered the reason for the poor outcomes in such patients, the improvement of PROs was not different. As a result, they insisted on preserving the posterior supporting musculature particularly in patients with sagittal imbalance. Nonetheless, patients should have an adequate degree of CL dependent on the magnitude of thoracolumbar sagittal imbalance.
Additionally, it is reasonable to investigate the influence of T1S-CL on surgical outcomes after cervical surgery. According to past reports, an excellent T1S-CL value was proposed to be 16° in patients with spinal deformity [13]. Iyer et al. [14] have also shown that T1S-CL was correlated with decreasing preoperative NDI in patients undergoing cervical spine surgery. In patients undergoing LP, several past reports have investigated the influence of T1S-CL on surgical outcomes. For example, Chen et al. [6] investigated the impact of T1S-CL on postoperative neck pain (> 4 in VAS score) in 85 patients undergoing double-door laminoplasty. They reported that 20° of T1S-CL and 2.89 cm cervical SVA were considered cut-off values of postoperative neck pain. Rao et al. [5] similarly set the cut-off value of preoperative T1S-CL as 20° and investigated the influence on surgical outcomes after open-door laminoplasty. Consequently, they reported that patients with preoperative T1S-CL > 20° demonstrated a postoperative kyphotic deformity. Hence, these reports concluded that patients with preoperative T1S-CL > 20° should not undergo cervical laminoplasty to avoid postoperative cervical kyphotic changes. The current study divided the patients into two groups based on their T1S-CL mismatching (> 20°). Although patients in the postoperative T1S-CL mismatching group had lower EQ5D or NDI values, preoperative T1S-CL did not affect the surgical outcomes. One possible reason for the discrepancy between our study and past reports was that our study excluded cases of patients with severe preoperative kyphosis. Most of the patients had preoperatively cervical lordosis, and only 8% showed preoperative T1S-CL mismatch, which could have affected the statistical results. Nevertheless, a significant correlation between pre- and postoperative T1S-CL values was observed (r = 0.59). Interestingly, the results differed when we divided the patients based on their postoperative T1S-CL value. We observed that patients with T1S-CL mismatches demonstrated poorer surgical outcomes, which we consider reasonable because postoperative radiographic parameters more accurately represented the postoperative state of patients’ HRQOL. From the results of our study, we did not consider LP as contraindicative in patients with preoperative T1S-CL mismatch in case they did not have severe kyphosis of the cervical spine. Yet, considering that the correlation between pre-and postoperative T1S-CL values was relatively strong, patients with preoperative T1S-CL mismatch are proposed to develop postoperative T1-CL mismatch. Thus, surgeons should carefully preserve posterior supporting structures, such as semispinalis muscles attaching to C2 and nuchal ligaments connecting to C7.
This study focused on the degree of T1S-CL because we considered that the preoperative degree of cervical lordosis, not cervical sagittal balance, would influence the effectiveness of posterior decompression surgery. However, a T1S-CL mismatch > 20° was reported to be related to C2-C7 SVA > 40 mm, which is considered the threshold of cervical deformity [15, 16]. Indeed, several reports have also demonstrated the possible involvement of regional cervical balances in surgical LP outcomes. For example, cervical SVA was initially reported to be related to surgical results after a posterior fixation surgery of the cervical spine, showing that patients with postoperative cervical SVA of 40 mm or more had worse NDI scores. Similarly, Kato et al. reported that patients with preoperative cervical SVA of 35 mm or more expressed worse neck pain and SF-36 scores after cervical LP [17]. In their study, although cervical balance did not aggravate after surgery, cervical posture was considered to affect postoperative neck pain and HRQOL. Moreover, Sakai et al. [18] showed that sagittal cervical imbalance (center of gravity of the head > 42 mm) was the preoperative risk factor for kyphotic deformity after LP for CSM. These reports indicated surgical results based on postoperative neck pain or HRQOL, which can differ from the symptoms directly related to cervical myelopathy. Nevertheless, it should be noted that postoperative cervical kyphosis can occur after cervical laminoplasty in patients with a large cervical SVA or T1S-CL mismatch.
There are several limitations in this study. First, it is important to recognize that this study used a retrospective design. Second, the sample size was relatively small. Third, our sample lacked patients with severe cervical kyphosis (> 10°). Therefore, further prospective studies should provide sufficient evidence for treating patients with DCM.
Conclusions
Although cervical LP showed inferior outcomes in patients with postoperative T1S-CL mismatch even in the absence of severe preoperative kyphosis (> 10°), preoperative T1S-CL mismatch was not adversely prognostic.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to their containing information that could compromise the privacy of research participants but are available from the corresponding author on reasonable request.
Abbreviations
- CL:
-
Cervical lordosis
- CSM:
-
Cervical spondylotic myelopathy
- DCM:
-
Degenerative cervical myelopathy
- JOA:
-
Japanese Orthopedic Association
- NDI:
-
Neck disability index
- NRS:
-
Numeric rating scale
- OPLL:
-
Ossification of the posterior longitudinal ligament
- SVA:
-
Sagittal vertical axis
References
Suda K, Abumi K, Ito M, Shono Y, Kaneda K, Fujiya M. Local kyphosis reduces surgical outcomes of expansive open-door laminoplasty for cervical spondylotic myelopathy. Spine (Phila Pa 1976). 2003;28(12):1258–62.
Zhang JT, Li JQ, Niu RJ, Liu Z, Tong T, Shen Y. Predictors of cervical lordosis loss after laminoplasty in patients with cervical spondylotic myelopathy. Eur Spine J. 2017;26(4):1205–10.
Cho JH, Ha JK, Kim DG, et al. Does preoperative T1 slope affect radiological and functional outcomes after cervical laminoplasty? Spine (Phila Pa 1976). 2014;39(26):E1575–81.
Kim TH, Lee SY, Kim YC, Park MS, Kim SW. T1 slope as a predictor of kyphotic alignment change after laminoplasty in patients with cervical myelopathy. Spine (Phila Pa 1976). 2013;38(16):992–7.
Rao H, Huang Y, Lan Z, Xu Z, Li G, Xu W. Does preoperative T1 slope and cervical lordosis mismatching affect surgical outcomes after laminoplasty in patients with cervical spondylotic myelopathy? World Neurosurg. 2019;130:e687–93.
Chen HY, Yang MH, Lin YP, et al. Impact of cervical sagittal parameters and spinal cord morphology in cervical spondylotic myelopathy status post spinous process-splitting laminoplasty. Eur Spine J. 2020;29(5):1052–60.
Hirabayashi K, Miyakawa J, Satomi K, et al. Operative results and postoperative progression of ossification among patients with ossification of cervical posterior longitudinal ligament. Spine (Phila Pa 1976). 1981;6:354–64.
Hoshi K, Kurokawa T, Nakamura K, Hoshino Y, Saita K, Miyoshi K. Expansive cervical laminoplasties - Observations on comparative changes in spinous process lengths following longitudinal laminal divisions using autogenous bone or hydroxyapatite spacers. Spinal Cord. 1996;34(12):725–8.
Matsunaga S, Sakou T, Nakanisi K. Analysis of the cervical spine alignment following laminoplasty and laminectomy. Spinal Cord. 1999;37(1):20–4.
Suk KS, Kim KT, Lee JH, Lee SH, Lim YJ, Kim JS. Sagittal alignment of the cervical spine after the laminoplasty. Spine (Phila Pa 1976). 2007;32(23):656–60.
Oichi T, Oshima Y, Oka H, et al. Is high T-1 slope a significant risk factor for developing interlaminar bony fusion after cervical laminoplasty? A retrospective cohort study. J Neurosurg Spine. 2017;27(6):627–32.
Oshima Y, Takeshita K, Taniguchi Y, et al. Effect of preoperative sagittal balance on cervical laminoplasty outcomes. Spine (Phila Pa 1976). 2016;41(21):E1265–70.
Staub BN, Lafage R, Kim HJ, et al. Cervical mismatch: The normative value of T1 slope minus cervical lordosis and its ability to predict ideal cervical lordosis. J Neurosurg Spine. 2019;30(1):31–7.
Iyer S, Nemani VM, Nguyen J, et al. Impact of cervical sagittal alignment parameters on neck disability. Spine (Phila Pa 1976). 2016;41(5):371–7.
Protopsaltis TS, Ramchandran S, Hamilton DK, et al. Analysis of successful versus failed radiographic outcomes after cervical deformity surgery. Spine (Phila Pa 1976). 2018;43(13):E733–81.
Hyun SJ, Han S, Kim KJ, Jahng TA, Kim HJ. Assessment of T1 slope minus cervical lordosis and C2–7 sagittal vertical axis criteria of a cervical spine deformity classification system using long-term follow-up data after multilevel posterior cervical fusion surgery. Oper Neurosurg. 2019;16(1):20–6.
Kato M, Namikawa T. Effect of cervical sagittal balance on laminoplasty in patients with cervical. Global Spine J. 2017;7(2):154–61.
Sakai K, Yoshii T, Hirai T, et al. Cervical sagittal imbalance is a predictor of kyphotic deformity after laminoplasty in cervical spondylotic myelopathy patients without preoperative kyphotic alignment. Spine (Phila Pa 1976). 2016;41(4):299–305.
Acknowledgements
The authors thank all the following spine surgeons who participated in data collection.
Funding
No funds were received in support of this work.
Author information
Authors and Affiliations
Contributions
RS (1st author) designed the research, analyzed data, and wrote the manuscript. YO (corresponding author) analyzed data and supervised the study. HN, YY, NO, KN, SK, TD, YM, YT, ST, and YO designed the research and supervised the study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study procedure was conducted in accordance with guidelines approved by the institutional review board of the University of Tokyo Hospital (approval no. 10335) and the Declaration of Helsinki. Written informed consent was obtained from all participants and their parents before participating in this study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sakamoto, R., Nakamoto, H., Yoshida, Y. et al. Does T1 slope minus cervical lordosis mismatch affect surgical outcomes of cervical laminoplasty in the absence of preoperative severe kyphosis?. BMC Musculoskelet Disord 23, 810 (2022). https://doi.org/10.1186/s12891-022-05755-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-022-05755-2