Abstract
Background
The main objective of this study was to investigate the risk factors for recollapse of new vertebral compression fractures (NVCFs) after percutaneous kyphoplasty (PKP) treatment for osteoporotic vertebral compression fracture (OVCF) and to construct a new nomogram model.
Methods
We retrospectively analysed single-level OVCFs from January 2017 to June 2020, randomizing patients to a training set and a testing set. In the training set, independent risk factors for NVCFs in OVCF patients treated with PKP were obtained by univariate and multivariate regression analyses. These risk factors were then used as the basis for constructing a nomogram model. Finally, internal validation of the built model was performed in the testing set using the consistency index (C-index), receiver operating characteristic (ROC) curves, calibration curves and decision curve analysis (DCA).
Results
In total, 371 patients were included in this study. NVCFs occurred in 21.7% of the training set patients, and multivariate regression analysis showed that a low Hounsfield unit (HU) value, cement leakage, and thoracolumbar (TL) junction fracture were independent risk factors for NVCF after PKP. The C-index was 0.81 (95% CI: 0.74–0.81), and the validation showed that the predicted values of the established model were in good agreement with the actual values.
Conclusions
In this study, three independent risk factors were obtained by regression analysis. A nomogram model was constructed to guide clinical work and to make clinical decisions relatively accurately to prevent the occurrence of vertebral recollapse fractures.
Similar content being viewed by others
Background
The increasing ageing of the population has resulted in severe bone loss in elderly people, and osteoporotic vertebral compression fracture (OVCF) is one of the most common complications of osteoporosis, with an incidence of vertebral fracture exceeding 1/3 [1]. Vertebral fractures can occur with low-energy trauma (e.g., falls and violent coughing), resulting in acute or chronic low back pain, kyphosis, and prolonged bed rest and reducing patient survival [2, 3]. Approximately 40% of women who are over 50 years of age will experience an osteoporotic fracture in their lifetime [4].
Currently, percutaneous kyphoplasty (PKP) is widely used in clinical practice because of its minimally invasive and safe features, which can effectively relieve patients' back pain [5, 6]. However, complications associated with PKP include unsatisfactory reduction, cement leakage [7, 8], and adjacent vertebral fractures [9]. Seo et al. [10] suggested that after a fractured vertebral body is injected with bone cement, the increased stiffness of the strengthened vertebral body will lead to adjacent vertebral compression fractures (VCFs). However, Yi et al. [11] argued that there was no significant difference in the occurrence of postoperative new adjacent vertebral fractures in patients with cement-injected vertebral compared to patients treated conservatively. In addition, there are many studies on vertebral refractures and multiple risk factors that predispose patients to new vertebral compression fractures (NVCFs) [12, 13]. However, the sample sizes of these studies were small, and their clinical utility was not effective enough to translate into a convenient tool.
The risk of refracture of the vertebral body in patients treated with PKP/percutaneous vertebroplasty (PVP) has been widely considered, and relevant independent risk factors have been derived in previous studies [14, 15]. Unfortunately, few studies have visualized the obtained risk factors with data, so we constructed a nomogram model. Nomogram models are currently widely used, and a large number of them are applied in the diagnosis and prognosis of disease. A scientific and systematic approach was used to evaluate the probability of patients developing NVCFs postoperatively. By applying this model, surgeons can better prevent the recurrence of vertebral fractures after PKP and the unnecessary use of medical resources.
Materials and methods
Study subjects
This study reviewed patients who underwent PKP surgery for OVCFs from January 2017 to June 2020 and was approved by the ethics committee of Chengde Medical University Affiliated Hospital. The inclusion criteria were as follows: 1. a first single-level VCF in an elderly individual that was caused by a low-energy injury (e.g., fall, bending over) and was treated with PKP; 2. radiological examinations (MRI: T2-weighted imaging showing marked bone oedema of the fractured vertebral bodies) that confirmed the VCF; 3. back pain locally related to the VCF; 4. long-term local residence with no history of residency in other areas during the follow-up period; and 5. bilateral pedicles and posterior vertebral walls that were intact without fracture.
The exclusion criteria were as follows: 1. spinal cord or nerve root compression due to vertebral burst fractures; 2. infections, tumours, and systemic diseases; 3. steroid and long-term hormone use; and 4. presence of psychiatric abnormalities or language disorders.
All the patients included in this study were followed up for more than 1 year. Finally, the patients were divided into a training set (70%) and a testing set (30%) by using a randomized grouping method. The patients in the training set were used to construct the nomogram model, and their data were used to evaluate the value of this model in the testing set. All the patients were continuously given 0.25 µg/d calcitriol and D3 600 mg/d calcium after surgery. Additionally, after surgery, the patients received zoledronic acid once a year at a dose of 5 mg dissolved in 100 ml saline and were infused intravenously for at least 15 min. None of the patients received calcitonin or parathyroid drugs.
Data collection
We reviewed previous literature and included risk factors that were likely to cause VCF after PKP. In addition, general patient characteristics and radiological parameters, including age, sex, BMI, kyphotic angle (preoperative and postoperative), volume of bone cement, leakage of cement (extending beyond the superior or inferior endplates), fracture level, HU value of CT, and bisphosphonate therapy, were collected.
Surgical procedures
All the patients were treated with local anesthesia in the prone position. Two puncture needles were placed one-third anterior to the fractured vertebral body through bilateral pedicles under fluoroscopic guidance. Bilateral balloons were individually inflated to try to restore vertebral height, and then a "toothpaste-like" bone cement was injected. After the patients rested in bed for 6 h, a brace was worn for proper ambulation.
Assessment
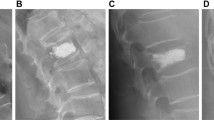
A patient presented with acute low back pain, and the fractured vertebral showed a high signal on T2-weighted fat suppression imaging. The thoracolumbar (TL) junction was defined as T11 to L2. BMI was defined as the weight (kg) divided by the square of the height (m2). The angle between the inferior endplate of the superior vertebral of the fractured vertebral and the superior endplate of the inferior vertebral on the lateral radiograph was defined as the kyphotic angle. In this study, we used the HU value of the CT measurement [16]. The measurement was performed by using the picture archiving and communication system (PACS, version 3.6; YLZ Information Technology Co., Ltd; CHINA) of our hospital. First, three tangents (25%, 50% and 75%) were created for the measured vertebral in the sagittal position, and the largest elliptical region of interest (ROI) containing only bone trabeculae was drawn in the axial position to obtain the average CT value (Fig. 1). The mean CT value of the TL junction not including fractured vertebral was defined as the HU value of the patient [17]. An HU value of less than 100 was defined as osteoporosis, and an HU value of more than 100 and less than 150 was defined as osteopenia [18, 19].
CT values were measured by PACS. A is a sagittal image of the lumbar spine with three tangents made on the measured vertebrae, corresponding to the three levels of (B), (C) and (D) in the axial position. The largest elliptical region of interest (ROI) containing only bone trabeculae was drawn in the axial position to obtain the average Hu value
Statistical analysis
This study used SPSS 26 (IBM Corp., Armonk, NY, USA) for statistical analysis of the data. First, the training and testing sets were compared. Then, continuous variables were statistically analysed using Student's t test or the Mann–Whitney U test; the chi-square or Fisher's exact test was used for categorical variables. Second, the risk factors were obtained from univariate analysis, and multivariate regression analysis was used to obtain independent risk factors for the occurrence of NVCFs after PKP surgery. Finally, the independent risk factors were plotted into a predictive nomogram model using the "rms" package of R software (version 3.6.1).
Evaluation of the model can better show its practical value. The consistency index (C-index) evaluates the model's predictive ability, which ranges from 0 to 1, with moderate accuracy defined as 0.5–0.7, high accuracy defined as 0.7–0.9 and extreme accuracy defined as greater than 0.9. The calibration curve may reveal an excellent response in patients with NVCFs vs. predicted NVCFs. Decision curve analysis (DCA) was used to assess the utility of the nomogram model based on the probability of net benefits and thresholds.
Results
A total of 393 patients were collected. According to the inclusion and exclusion criteria, 22 patients were excluded: 2 patients had language disorders, 8 patients lost to follow-up, and 12 patients had tumour diseases.
Clinical characteristics
In all, 371 patients were included in this study. A total of 263 patients were used as the training set to construct the nomogram model, and 108 patients were used as the testing set to validate the model. The general characteristics of the patients in both groups are shown in Table 1. The average age of the patients in the training set was 72.48 ± 7.29 years and the average age of the patients in the testing set was 72.10 ± 7.54 years. There was no significant difference between the two groups (P > 0.05).
Acquisition of independent risk factors and construction of nomogram models
Among the patients in the training set, those in the NVCF and N-NVCF groups had statistically significant differences in Hu values, cement leakage, and TL segments (P < 0.05) (Table 2). These three factors were found to be risk factors for new fractures of the vertebral body by univariate regression analysis. Finally, a low Hu value (OR: 0.96, 95% CI: 0.94–0.97), cement leakage (OR: 2.96, 95% CI: 1.49–5.88) and TL segment (OR: 3.11, 95% CI: 1.41–6.89) were found to be independent risk factors for vertebral body refracture after PKP by multifactorial regression analysis (Table 3). A novel nomogram model was constructed based on these three independent risk factors (Fig. 2).
Validation of the nomogram model
The constructed nomogram model was validated internally by the training set and testing sets. The C-index of this model was 0.81 (95% CI: 0.74–0.81), which shows that this model has high accuracy. In this study, receiver operating characteristic (ROC) curve were plotted, and areas under the ROC curve (AUC) of 0.81 and 0.80 were calculated for the training and testing sets, respectively (Fig. 3). The calibration curve results showed excellent agreement between the predicted probability and the actual probability of NVCFs (Fig. 4). DCA showed that this nomogram model could be an excellent prediction tool for NVCFs after PKP operation (Fig. 5).
Use of the nomogram model
The constructed nomogram model has the characteristics of simplicity and convenience in clinical use. The scores corresponding to each independent risk factor were summed to obtain a total score, and the total score was then used to calculate the probability of NVCFs. For example, the HU value was 60 in a 75-year-old patient, the fracture segment was the TL junction, and there was cement leakage; therefore, the calculation is as follows, the HU score for this patient was 69, the TL junction score was 20, the cement leakage score was 19, and the total score was 69 + 20 + 19 = 118, which was equivalent to a 70% risk of NVCFs after PKP.
Discussion
OVCFs are more likely to occur in elderly patients with osteoporosis, and patients undergoing minimally invasive surgical treatment can receive satisfactory results and an improved prognosis. However, fractured vertebral strengthened by bone cement are prone to postoperative NVCFs (Fig. 6). Some studies have shown that the probability of postoperative NVCFs in patients treated with PKP ranges from 6.5% to 34.8% [12, 20,21,22]. In this study, we found that a low HU value, bone cement leakage and TL junction fracture were independent risk factors by multivariate regression analysis for NVCFs after surgery. By obtaining clinically available risk factors, this study is the first to construct a nomogram model of postoperative refracture in PKP. Indeed, this study is different from previous investigations [13,14,15]. First, we developed a nomogram model, which was drawn from independent risk factors obtained by regression analysis, with the advantages of improved readability of the results and convenience of use. Second, a testing set was used in this study to verify the value of the established model. This nomogram model can help surgeons estimate the probability of postoperative refracture and develop individualized treatment or prevention plans for patients.
Bone mineral density (BMD) is usually measured by dual-energy X-ray absorptiometry (DXA) to obtain a T value. In clinical practice, DXA is not suitable for patients with spinal deformities, degenerative conditions or calcifications that would overestimate the T value [19]. Therefore, to improve the accuracy, some authors have started to search for new measurement methods. CT measurements are one of the standard tools used to diagnose fractures. Some scholars believe that CT (HU value) is an essential complementary means to indicate BMD, and it has been widely used in clinical work [17, 18, 23]. According to relevant studies, the HU value measured by CT can be obtained with high sensitivity and specificity [18, 24]. Several studies have shown that low BMD is not an independent risk factor for refracture, [21, 25] and the reason for this may be that the patients who develop OVCFs are elderly individuals whose lumbar degeneration is often severe, resulting in compensatory osteophytes, which reduce the accuracy of the T value. Therefore, instead of using the T value, the HU value was applied in this study. The results of this study show that the HU value (OR: 0.96) is an independent risk factor for NVCFs after surgery, which is consistent with previous studies [23].
Bone cement leakage is one of the common complications after PKP/PVP. In a follow-up study of 102 patients, Chen et al. [26] found that 14.7% of cement leakage cases occurred after PKP, and the integrity of the vertebral wall and the amount of cement injected were risk factors for cement leakage. A study reported that cement leakage was an independent risk factor for the occurrence of vertebral refracture after cement strengthening [17], which is similar to the results of this study. Li et al. [27] performed a multifactorial regression analysis of 403 patients in the training set and found that cement leakage, cement dispersion, and amount of cement were independent risk factors for vertebral refracture. Bone cement-related risk factors accounted for 3/6 this study, so bone cement has been a hot topic of related research. The intervertebral disc is the main cushioning device of the spine, and cement leakage into the disc can weaken the cushioning capacity, [28] making the vertebral more susceptible to NVCFs. By observing patients who underwent cement enhancement for OVCFs, Ahn et al. [29] attributed the refracture of adjacent vertebral to the direct pillar effect, which may be caused by the difference in strength after cement enhancement, and second, they attributed the refracture of nonadjacent segments to the dynamic hammer effect, which results in the difference in segmental mobility.
This study showed that TL junction fractures accounted for 56.0% of all fractures in the training set. TL junction (OR = 3.11) fractures were an independent risk factor for NVCFs. The TL junction is widely considered to be an excess region of biomechanical anatomy [30]. The TL junction is susceptible to NVCFs because it has a greater range of motion than other relatively inactive segments. A study demonstrated that older age is an independent risk factor for vertebral refracture [31]. However, Ji et al. [23] found that age and sex were not independent risk factors for the development of NVCFs after a multivariate regression analysis, which is consistent with the findings of this study. Li et al. [15] assessed 230 patients to analyse the risk factors for vertebral recollapse after undergoing PKP/PVP surgery. Regression analysis revealed no significant difference in the restoration of the Cobb angle(%) in the refracture group (40.38 ± 8.55) versus the non-refracture group (30.19 ± 10.24). This is consistent with our study.
Our nomogram model has strong practicability in the clinic. By applying it to patients with a first fracture, the risk of a second fracture can be estimated more accurately, and treatment can be personalized.
This study has some shortcomings. First, it was a retrospective analysis, all patients were from a single centre, and there was a lack of external data to verify the effectiveness of the model. Second, the follow-up time was short and should be extended. Finally, HU values measured by different CT devices may vary, and similarly, the same problem exists for DXA measurements, and standards for measurement need to be established.
Conclusions
In this study, we retrospectively analysed patients who developed NVCFs after undergoing PKP treatment and found that a low HU value, cement leakage and TL junction fracture were independent risk factors for NVCFs. Therefore, a new nomogram model has been constructed by which surgeons can effectively assess the probability of new vertebral fractures after a patient's original OVCF and can intervene immediately after surgery to prevent refractures.
Availability of data and materials
The data that support the findings of this study are not openly available due to reasons of sensitivity of human data and are available from the corresponding author upon reasonable request.
Abbreviations
- NVCFs:
-
New vertebral compression fractures
- PKP:
-
Percutaneous kyphoplasty
- OVCF:
-
Osteoporotic vertebral crush fracture
- C index:
-
Consistency index
- ROC:
-
Receiver operating characteristic
- DCA:
-
Decision curve analysis
- HU:
-
Hounsfield Units
- TL:
-
Thoracolumbar
- N- NVCF:
-
Non new vertebral compression fracture
- BMD:
-
Bone mineral density
- DXA:
-
Dual-energy x-ray absorptiometry
References
Buchbinder R, Golmohammadi K, Johnston RV, Owen RJ, Homik J, Jones A, Dhillon SS, Kallmes DF, Lambert RG. Percutaneous vertebroplasty for osteoporotic vertebral compression fracture. Cochrane Database Syst Rev. 2015;4:CD006349.
Bliuc D, Nguyen ND, Milch VE, Nguyen TV, Eisman JA, Center JR. Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA. 2009;301(5):513–21.
Korovessis P, Vardakastanis K, Repantis T, Vitsas V. Balloon kyphoplasty versus KIVA vertebral augmentation--comparison of 2 techniques for osteoporotic vertebral body fractures: a prospective randomized study. Spine (Phila Pa 1976). 2013;38(4):292–9.
Si L, Winzenberg TM, Chen M, Jiang Q, Palmer AJ. Residual lifetime and 10 year absolute risks of osteoporotic fractures in Chinese men and women. Curr Med Res Opin. 2015;31(6):1149–56.
Buchbinder R, Osborne RH, Ebeling PR, Wark JD, Mitchell P, Wriedt C, Graves S, Staples MP, Murphy B. A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med. 2009;361(6):557–68.
Clark W, Bird P, Gonski P, Diamond TH, Smerdely P, McNeil HP, Schlaphoff G, Bryant C, Barnes E, Gebski V. Safety and efficacy of vertebroplasty for acute painful osteoporotic fractures (VAPOUR): a multicentre, randomised, double-blind, placebo-controlled trial. Lancet. 2016;388(10052):1408–16.
Baumann C, Fuchs H, Kiwit J, Westphalen K, Hierholzer J. Complications in percutaneous vertebroplasty associated with puncture or cement leakage. Cardiovasc Intervent Radiol. 2007;30(2):161–8.
Patel AA, Vaccaro AR, Martyak GG, Harrop JS, Albert TJ, Ludwig SC, Youssef JA, Gelb DE, Mathews HH, Chapman JR, et al. Neurologic deficit following percutaneous vertebral stabilization. Spine (Phila Pa 1976). 2007;32(16):1728–34.
Rho YJ, Choe WJ, Chun YI. Risk factors predicting the new symptomatic vertebral compression fractures after percutaneous vertebroplasty or kyphoplasty. Eur Spine J. 2012;21(5):905–11.
Seo DH, Oh SH, Yoon KW, Ko JH, Kim YJ, Lee JY. Risk Factors of New Adjacent Compression Fracture after Percutaneous Vertebroplasty: Effectiveness of Bisphosphonate in Osteoporotic or Osteopenic Elderly Patients. Korean J Neurotrauma. 2014;10(2):86–91.
Yi X, Lu H, Tian F, Wang Y, Li C, Liu H, Liu X, Li H. Recompression in new levels after percutaneous vertebroplasty and kyphoplasty compared with conservative treatment. Arch Orthop Trauma Surg. 2014;134(1):21–30.
Lee BG, Choi JH, Kim DY, Choi WR, Lee SG, Kang CN. Risk factors for newly developed osteoporotic vertebral compression fractures following treatment for osteoporotic vertebral compression fractures. Spine J. 2019;19(2):301–5.
Park JS, Park YS. Survival analysis and risk factors of new vertebral fracture after vertebroplasty for osteoporotic vertebral compression fracture. Spine J. 2021;21(8):1355–61.
An Z, Chen C, Wang J, Zhu Y, Dong L, Wei H, Wu L. Logistic regression analysis on risk factors of augmented vertebra recompression after percutaneous vertebral augmentation. J Orthop Surg Res. 2021;16(1):374.
Li YX, Guo DQ, Zhang SC. Liang, Yuan K, Mo GY, Li DX, Guo HZ, Tang Y, Luo PJ: Risk factor analysis for re-collapse of cemented vertebrae after percutaneous vertebroplasty (PVP) or percutaneous kyphoplasty (PKP). Int Orthop. 2018;42(9):2131–9.
Schreiber JJ, Anderson PA, Rosas HG, Buchholz AL, Au AG. Hounsfield units for assessing bone mineral density and strength: a tool for osteoporosis management. J Bone Joint Surg Am. 2011;93(11):1057–63.
Zhong BY, He SC, Zhu HD, Wu CG, Fang W, Chen L, Guo JH, Deng G, Zhu GY, Teng GJ. Risk Prediction of New Adjacent Vertebral Fractures After PVP for Patients with Vertebral Compression Fractures: Development of a Prediction Model. Cardiovasc Intervent Radiol. 2017;40(2):277–84.
Pickhardt PJ, Pooler BD, Lauder T, del Rio AM, Bruce RJ, Binkley N. Opportunistic screening for osteoporosis using abdominal computed tomography scans obtained for other indications. Ann Intern Med. 2013;158(8):588–95.
Gausden EB, Nwachukwu BU, Schreiber JJ, Lorich DG, Lane JM. Opportunistic Use of CT Imaging for Osteoporosis Screening and Bone Density Assessment: A Qualitative Systematic Review. J Bone Joint Surg Am. 2017;99(18):1580–90.
Movrin I, Vengust R, Komadina R. Adjacent vertebral fractures after percutaneous vertebral augmentation of osteoporotic vertebral compression fracture: a comparison of balloon kyphoplasty and vertebroplasty. Arch Orthop Trauma Surg. 2010;130(9):1157–66.
Ko BS, Cho KJ, Park JW. Early Adjacent Vertebral Fractures after Balloon Kyphoplasty for Osteoporotic Vertebral Compression Fractures. Asian Spine J. 2019;13(2):210–5.
Harrop JS, Prpa B, Reinhardt MK, Lieberman I. Primary and secondary osteoporosis’ incidence of subsequent vertebral compression fractures after kyphoplasty. Spine (Phila Pa 1976). 2004;29(19):2120–5.
Ji C, Rong Y, Wang J, Yu S, Yin G, Fan J, Tang P, Jiang D, Liu W, Gong F, et al. Risk Factors for Refracture following Primary Osteoporotic Vertebral Compression Fractures. Pain Physician. 2021;24(3):E335–40.
Hendrickson NR, Pickhardt PJ, Del Rio AM, Rosas HG, Anderson PA. Bone Mineral Density T-Scores Derived from CT Attenuation Numbers (Hounsfield Units): Clinical Utility and Correlation with Dual-energy X-ray Absorptiometry. Iowa Orthop J. 2018;38:25–31.
Yang CC, Chien JT, Tsai TY, Yeh KT, Lee RP, Wu WT. Earlier Vertebroplasty for Osteoporotic Thoracolumbar Compression Fracture May Minimize the Subsequent Development of Adjacent Fractures: A Retrospective Study. Pain Physician. 2018;21(5):E483–91.
Chen C, Fan P, Xie X, Wang Y. Risk Factors for Cement Leakage and Adjacent Vertebral Fractures in Kyphoplasty for Osteoporotic Vertebral Fractures. Clin Spine Surg. 2020;33(6):E251–5.
Li Q, Long X, Wang Y, Fang X, Guo D, Lv J, Hu X, Cai L. Development and validation of a nomogram for predicting the probability of new vertebral compression fractures after vertebral augmentation of osteoporotic vertebral compression fractures. BMC Musculoskelet Disord. 2021;22(1):957.
Sun YC, Teng MM, Yuan WS, Luo CB, Chang FC, Lirng JF, Guo WY, Chang CY. Risk of post-vertebroplasty fracture in adjacent vertebral bodies appears correlated with the morphologic extent of bone cement. J Chin Med Assoc. 2011;74(8):357–62.
Ahn Y, Lee JH, Lee HY, Lee SH, Keem SH. Predictive factors for subsequent vertebral fracture after percutaneous vertebroplasty. J Neurosurg Spine. 2008;9(2):129–36.
Holmes JF, Miller PQ, Panacek EA, Lin S, Horne NS, Mower WR. Epidemiology of thoracolumbar spine injury in blunt trauma. Acad Emerg Med. 2001;8(9):866–72.
Chen Z, Chen Z, Wu Y, Wu Y, Ning S, Ning S, Ma T, Ma T, Wu Z, Wu Z. Risk Factors of Secondary Vertebral Compression Fracture After Percutaneous Vertebroplasty or Kyphoplasty: A Retrospective Study of 650 Patients. Med Sci Monit. 2019;25:9255–61.
Acknowledgements
Not applicable.
Funding
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Contributions
Author FC B and YS A designed the study. Author S H, FC B, L Z, and GY B collected the clinical data and conducted the statistical analysis. Author FC B and S H wrote the manuscript. Author FC B, S H, GY B, YS A and L Z revised the manuscript. All authors critically read the manuscript to improve intellectual content. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This research was approved by the ethics committee of Chengde Medical University Affiliated Hospital and Daqing oilfield General Hospital. Informed consent to participate was obtained from all individual participants included in the study prior to initiating data collection. All methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Bian, F., Bian, G., Zhao, L. et al. Risk factors for recollapse of new vertebral compression fractures after percutaneous kyphoplasty in geriatric patients: establishment of a nomogram. BMC Musculoskelet Disord 23, 458 (2022). https://doi.org/10.1186/s12891-022-05409-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-022-05409-3