Abstract
Background
Asthma is a diverse disease with various etiologic bases. Severe asthma can be associated with increased mortality, hospitalization, and decreased quality of life for asthma patients. High blood eosinophil counts were associated with severe asthma, but recent studies have failed to confirm this as a marker of severe asthma among adult asthma patients. As a result, the purpose of this study was to determine the association between the severity of asthma and high blood eosinophil count.
Methodology
A simple random sampling technique was used to select 291 asthmatic patients for an institution-based cross-sectional study. Socio-demographic, behavioral, and clinical characteristics were collected by using a pre-tested structured questionnaire. Four milliliters of venous blood were collected from asthmatic patients for complete blood count and peripheral morphology assessment. The eosinophil count was analyzed by the Unicel DxH 800 (Beckman Coulter, Ireland) analyzer. A statistical package for social science version 20 (SPSS) software was used to analyze the data. The non-parametric (Mann-Whitney U) test was used to compare the eosinophil count with different background variables. A binary logistic regression analysis was used to assess the factors associated with eosinophilia. A p-value less than 0.05 in multivariable logistic regression analysis was considered statistically significant.
Result
In this study, the overall magnitude of eosinophilia was 19.6% (95% CI = 14.8–24.1). Being admitted to the emergency department (AOR = 0.25; 95% CI: 0.09–0.69, p = 0.007) and being female (AOR = 0.49; 95% CI: 0.26–0.9, p = 0.025) were shown to have a statistically significant association with eosinophilia. Moreover, the absolute eosinophil count was significantly higher among asthmatic patients infected with intestinal parasitic infection (p < 0.045).
Conclusion
Being female and admission to the emergency department were negatively associated with eosinophilia. Lack of eosinophilia can be related to the low-T2 asthma phenotype. The absolute eosinophil counts were higher among intestinal parasite-infected patients. Therefore, different biomarkers will be considered for the proper diagnosis and management of adult asthma patients.
Similar content being viewed by others
Introduction
Asthma is a diverse disease characterized by chronic airway inflammation [1]. It is defined by a history of respiratory symptoms such as wheezing, chest tightness, shortness of breath, and cough that can fluctuate over time and in intensity along with variable expiratory airflow limitation [1, 2]. Asthma is a common disease of the airways that affects 339 million people worldwide [3]. Asthma prevalence is still growing in various countries [4]. In adults, the frequency of asthma ranges from 4 to 10% [4,5,6].
Asthma is a heterogenous disease with various etiologic bases [1, 7]. Asthma endotypes can be largely classified as type 2 (T2) high or T2-low [7]. T2-high asthma is distinguished by fractional exhaled nitric oxide (FeNO) > 25 ppb, blood and airway eosinophilia (peripheral blood eosinophil levels > 300 or > 150 cells/µL, and sputum eosinophils > 2%), increased severity, and therapeutic responsiveness to Glucocorticoids and T2 inflammatory inhibitors [8, 9]. During exposure to allergens, T2 inflammation coexists with eosinophilic inflammation mediated by cytokines such as interleukin (IL) -4, IL-5, and IL-13 [10, 11]. T2-low asthma is identified by increased neutrophils and a lack of airway and systemic eosinophilia [8, 10].
The European Respiratory Society (ERS)/American Thoracic Society (ATS) task force defines severe asthma as “asthma that needs treatment with high-dose inhaled corticosteroids (ICS) plus additional controller and/or systemic corticosteroids to keep it from being “uncontrolled” or it remains “uncontrolled” despite maximally optimized Global Initiative for Asthma (GINA) step 4 or 5 therapy and treatment of contributing factors, or it worsens when optimized therapy is reduced”. It is estimated that about 3 to 10% of asthma patients have severe asthma [1, 11].
Severe asthma is associated with higher mortality, hospitalization, and a decreased quality of life. Also, it results in physical, mental, emotional, social, and occupational costs for individuals as well as a financial impact on health care systems [12, 13].
Eosinophils are responsible for inflammatory effects when triggered by allergens. Persistent eosinophilic airway inflammation and airway remodeling lead to persistent airflow obstruction [14]. A high blood eosinophil count causes immune-modulatory responses such as airway inflammation, airway hyperresponsiveness, damage to the epithelial lining, and increased mucus secretion [15]. Nearly half of asthmatic patients have eosinophilic inflammation. Studies have shown that eosinophilia can be linked with increased disease severity, exacerbation frequency, and symptom burden, as well as impaired lung function [16,17,18].
Eosinophils are important predictors of disease severity and progression [19]. As a result, eosinophils play a critical role in asthma diagnosis. Moreover, eosinophil counts have emerged as a promising and easily measurable marker in eosinophilic airway inflammation [20, 21]. Although allergic sensitization has been identified as a risk factor for asthma [22], non-allergic asthma is more common in adults. The prevalence of allergic asthma is higher during early childhood and gradually declines with advanced age. Especially after the age of 40 years, the new cases are non-allergic asthma [23, 24].
The ERS/ATS task force considered sputum and blood eosinophilia as markers for severe asthma [11]. However, GINA stated that the blood eosinophil count is not employed as a diagnostic biomarker for asthma. Instead, it can be utilized as a prognostic biomarker, predicting therapeutic responsiveness and a diagnostic biomarker for defining asthma phenotypes in patients with type 2 inflammation [25]. Several cross-sectional and longitudinal studies have identified blood eosinophil counts as a risk factor for asthma exacerbation [26,27,28]. Conversely, recent follow-up studies found that eosinophil counts are not linked to asthma exacerbations [29, 30].
Many studies have revealed that eosinophil levels rise in cases of severe asthma. However, asthma is a diverse disease with different etiologies and phenotypes. Therefore, the main aim of this study was to determine the magnitude of the elevated peripheral eosinophil count and its association with the severity of asthma among adult asthmatic patients.
Methods and materials
Study design, area, and period
An institutional cross-sectional study was conducted from June to August 2021 in Northwest Ethiopia, at the University of Gondar Comprehensive Specialized Hospital (UGCSH) and Tibebe-Ghion Specialized Hospital (TGSH). UGCSH is located in Northwest Ethiopia, Amhara Regional State, in Gondar Town. The hospital can provide service for over 7 million people in the catchment area. There are over 400 regular follow-ups of asthmatic patients in the chronic outpatient department of the hospital. On the other hand, TGSH is located in Northwest Ethiopia, in Bahirdar City. The hospital provides health services for eight nearby zones in the Amhara regional state.
Study participants
This study included all adult asthmatic patients (≥ 18 years old) attending UGCSH and TGSH during the study period. On the other hand, patients with known chronic diseases such as HIV/AIDS, hematological malignancies, chronic kidney disease, and tuberculosis were excluded from this study by reviewing their medical records.
Sample size determination and sampling technique
Sample size determination
The sample size was determined by using the single population proportion formula by considering a proportion of 50%, 5% margin error, powe of 80%, and a 95% confidence interval. By using a formula, \(n=\frac{{\left({Z}_{\frac{\alpha }{2}}\right)}^{2}p\text{q}}{{\text{d}}^{2}}\) = (1.96)2 (0.5 × 0.5)/(0.05)2 = 384.
Since the total number of asthmatic patients in two hospitals per year was less than 10,000 (N < 10,000). Thus, a reduction formula was used. So, \(\text{n}=\frac{\text{n}\text{o}}{1+\frac{\text{n}0}{\text{N}} }\) = \(\frac{384}{1+\frac{384}{1200} }\)= 290.9 = Approx, n = 291
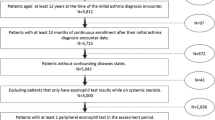
The study participants were proportionally allocated from each hospital (Fig. 1). The lottery-based simple random sampling technique was used to select the study participants.
Operational definitions
-
Asthma: any person who has been diagnosed with asthma by a physician working as a pulmonary medicine specialist under GINA guidelines. The diagnosis was made based on the following criteria: asthma medication use, history of various respiratory symptoms, and confirmed variable expiratory airflow limitation [1].
-
Admission to the emergency department: asthmatic patients who were admitted to the emergency department for health care utilization due to asthma [31].
-
The severity of asthma was classified based on the GINA 2019 guideline [32].
-
Stages of asthma were classified as intermittent, mild persistent, moderate persistent, and severe persistent based on the GINA 2019 guideline [32].
-
A physical exercise habit: a study subject who has experience doing the physical exercise once per day for at least 20–30 min as a continuous activity [33].
-
Elevated blood eosinophil count: is defined as an absolute eosinophil count greater than 0.04 × 103/µl [34].
Data collection and sample processing
The socio-demographic and behavioral characteristics of study participants were collected by using a structured pre-tested questionnaire via face-to-face interview. The clinical data of study participants, such as asthma duration, family history of asthma, history of asthma medication, asthma drug type, chronic disease, severity and stages of asthma, symptoms of asthma, and history of drug intake other than asthma before 3 months, were collected from the patient’s medical record (chart review) by using a checklist. Study participants were sent to the laboratory room, where the blood specimen was drawn and analyzed after trained clinical nurses completed data via face-to-face interview and chart review.
A venous blood specimen (4 milliliters) was collected from asthmatic patients with a syringe method by the trained laboratory technician. Then it is dispensed into the tube containing ethylene-diamine tetra-acetic acid anticoagulant for complete blood count (CBC) and peripheral morphology assessment. Complete blood counts of the study participants were analyzed by using five differential Unicel DxH 800 Coulter cellular analysis systems (Beckman Coulter, Ireland) automated hematological analyzers through Coulter counting, spectrophotometry, and VCS technology.
A peripheral blood morphology examination was performed to confirm flags generated by the automated hematology analyzer and to check whether the automated hematology analyzer provides a consistent result. A thin blood smear was prepared from leftover blood from CBC. Wright stain was used to stain the dried smear. The smear was carefully examined with a 100X oil immersion objective by laboratory technologists. All laboratory tests, such as CBC and peripheral morphology, were performed in the UGCSH and TGSH laboratories. The results of every study participant were recorded in a format designed for laboratory result registration.
Data quality assurance and management
The questionnaire was prepared in the English version, translated into the local language (Amharic), and retranslated back to the English version to check the accuracy and consistency. It has been pretested on 5% of asthmatic patients at Felege Hiwot Comprehensive Specialized Hospital. Then a questionnaire was modified based on the result of the pretest. Before the data collection began, training was given for data collectors to reduce technical and observer bias.
Pre-analytical, analytical, and post-analytical phases of quality assurance were maintained in the overall laboratory process to assure the quality of data. Quality control for working equipment and reagents was ensured by using standard controls. Standard operating procedures and manufacturers’ instructions were strictly followed during sample collection and laboratory procedures. The questionnaire was checked for consistency, clarity, and completeness by the principal investigator. The results of every test were properly recorded, reviewed, and transcribed.
Data processing and statistical analysis
The data was entered into Epi-data software (Version: 3.0.4), cleaned, and exported into Statistical Package for Social Science version 20 software (IBM Corp., Armonk, NY, USA) for analysis. To summarize the data, descriptive statistics such as frequencies and percentages were used. The Shapiro-Wilk test and histogram were used to check the normal distribution of continuous variables. The data was presented using tables.
Non-parametric (Mann-Whitney test) was used to compare median values of absolute eosinophil count with different background variables. Binary logistic regression, such as bivariable and multivariable logistic regression analysis, was performed. The strength of association between predictors and outcome was determined using the crude odds ratio (COR) and adjusted odds ratio (AOR) with a 95% confidence interval (CI). In the bivariable logistic regression analysis, variables having a p-value of less than 0.25 were fitted into the multivariable logistic regression analysis. Hosmer and Lemeshow’s goodness of fit statistics were used to test the model’s fitness. In all cases, a p-value of less than 0.05 was considered statistically significant.
Ethical consideration
Ethical clearance was obtained from the ethical review committee of the School of Biomedical and Laboratory Science, College of Medicine and Health Sciences, University of Gondar, on March 3, 2021, with letter reference number SBMLS-2748. The Department of Hematology and Immunohematology provided a support letter, which was forwarded to the directors of UGCSH and TGSH. In addition, a permission letter to conduct research was obtained from the UGCSH and TGSH directors.
Informed written consent was obtained from each study participant after the objective of the study was explained. For illiterate patients, informed consent was obtained after objective of study and detailed information was read by data collectors. Then fingerprint signature was taken from each study illiterate participant. Study participants were identified by using codes rather than individual identifiers. The results and information of the study participants were kept confidential. Study participants who had elevated eosinophil counts were linked to the UGCSH and TGSH chronic outpatient departments for proper management. All methods were performed per the relevant guidelines and regulations (Declaration of Helsinki).
Result
Sociodemographic characteristics of the study participants
In this study, we included a total of 291 study participants. Of those, about 164 (56.4%) were females. The age ranges from 18 to 65 years, with the median and interquartile range (IQR) of 50 (38 to 60) years. About 188 (64.6%) of the study participants were over 40 years old. Regarding the residence of study participants, 186 (63.9%) participants were urban residents. The majority of study participants were unable to read and write in their educational status, 126 (43.3%) (Table 1).
Behavioral characteristics of study participants and BMI
Of the study participants, 5 (1.7%) were current cigarette smokers; 52 (17.9%) had a habit of doing physical exercise; and 75 (23.4%) had a habit of drinking alcohol. About 64 (22%) had an alcohol-drinking habit. The mean ± standard deviation value of BMI is 2.26 ± 2.97 kg/m2. According to their BMI, about 51 (17.5%) of the study participants were overweight.
Clinical characteristics of study participants
The majority of the study participants had been living with asthma for less than five years, 121 (41.6%). Regarding severity and stages of asthma, about 176 (60.5%) and 186 (63.9%) had moderate severity and moderately persistent stages of asthma, respectively. Among study participants, about 241 (82.8%) had taken asthmatic drugs in the previous three months. In addition, about 86 (29.6%) were admitted to the emergency department (Table 2).
Magnitudes of the elevated peripheral eosinophil count and its comparison with background variables
In this study, the magnitude of eosinophilia was 19.6% (95% CI = 14.8–24.1) with a median and IQR of 0.2 (0.07–0.4). The non-parametric Mann-Whitney U test was used to compare median differences in absolute eosinophil counts between groups because the data were not normally distributed. Based on this analysis, only asthma medication, asthma-related ED admission, and intestinal parasitic infection showed a statistically significant median difference (Table 3).
Factors associated with elevated peripheral eosinophil count
A binary logistic regression analysis was performed to check for factors associated with eosinophilia. In bivariable logistic regression analysis, variables like gender, alcohol drinking habit, and asthma-related emergency department admission were shown to have an association with eosinophilia. In addition, the factors with a p-value less than 0.25 were fitted into multivariable logistic regression analysis. Being admitted to the emergency department (AOR = 0.25; 95% CI: 0.09–0.69, p = 0.007) and being female (AOR = 0.49; 95% CI: 0.26–0.9, p = 0.025) were showed a statistically significant association with eosinophilia in a multivariable logistic regression model (Table 4).
Discussion
In the present study, eosinophilia was observed in 19.6% (95% CI = 14.8–24.1) of asthmatic patients. This finding was consistent with the study conducted in the USA (18.5%) [35], the United Kingdom (16%) [36], Spain (20.7%) [37], and a cross-sectional survey of the United States general population (18%) [38]. However, the finding was lower than a study done in Japan (34%) [39], a pilot study in the USA (40%) [40], Canada (41%) [41], Brazil (40%) [42], Mexico (37.7%) [43], and the United Kingdom (43%) [44]. The possible reasons for the difference might be due to variation in study participants, socio-demographic characteristics, and sample size. In addition, the recruitment of circulating eosinophils is elevated during allergic conditions, particularly in asthma [45, 46]. It is also known that blood eosinophilia can be a marker of asthma [37].
The comparison of absolute eosinophil count with different background variables was done in the present study. Based on the findings of this study, the absolute eosinophil count was higher among patients who were infected with intestinal parasitic infections than among patients who were not infected with intestinal parasitic infections. This finding was supported by different studies [47, 48]. The possible explanation might be due to the production and activation of eosinophils induced by IL-5, which is secreted by Th2 cells. Thus, eosinophils are involved in host defense, inflammation, and immunomodulation [49]. Eosinophil levels are increased during allergic reactions and helminth infections [50].
In this study, we used binary logistic regression analysis to observe the association between the severity of asthma and eosinophilia. However, severe asthma did not show a statistically significant association with eosinophilia in the present study. This might be due to the fact that the majority of study participants were older (> 40 years old) and females, which are characteristics of adult-onset asthma. This finding was supported by the West Sweden Asthma study (WSAS) and Obstructive Lung Disease in Northern Sweden (OLIN) studies. A 15-year follow-up WSAS study showed that the severity of asthma was associated with blood neutrophilia rather than blood eosinophilia [51, 52]. Amelink et al. also showed that blood eosinophils are not a marker of severity in all asthmatic patients because asthma is a diverse disease with different phenotypes [53].
On the contrary, various studies have found that an elevated eosinophil count is associated with severe asthma [9, 35,36,37, 54, 55]. This is due to the fact that inflammation is firmly related to the existence of elevated eosinophils in the airway as well as the expression of the Th2 cytokine during allergic asthma. In particular, IL-5 plays a major role in the recruitment, survival, and maturation of eosinophils [11, 56]. Also, it should be known that asthma is a heterogeneous disease with different phenotypes.
Females were less likely to develop eosinophilia than males (AOR = 0.48; 95% CI: 0.26–0.9). This might be because women had a higher incidence of adult-onset asthma when compared to males [57,58,59]. It is known that in adults, asthma is more often non-allergic than allergic [23, 60]. Thus, T2-low asthma is characterized by neutrophilic airway inflammation through the involvement of non-type 2 cytokines such as IL-8 and IL7 rather than eosinophilic inflammation [29, 61].
Study participants who were admitted to the ED (AOR = 0.25; 95% CI: 0.09–0.69, p = 0.007) were less likely to develop eosinophilia than patients who were not admitted to the ED. The possible explanation might be that the patients attending the ED might be treated with a high dose of inhaled corticosteroids to reduce exacerbation according to GINA guidelines [1, 11, 62]. Eosinophil counts are known to be reduced by ICS’s anti-inflammatory effect [63,64,65]. ICS inhibits the transcription of protein-coding genes (such as IL-4, IL-5, IL-13, and TNF-α), as well as chemokines and adhesion molecules, reducing inflammatory cell recruitment and survival (like eosinophils, T-lymphocytes, and mast cells) [65]. Moreover, low cytokine production, particularly IL5, reduces the recruitment of eosinophils [66].
This study was limited to showing cause and effect relationships due to the cross-sectional nature of the study. We did not assess the association between the time of oral corticosteroid use and the drug dose with eosinophil level. Another limitation was that the asthma control status of patients was not studied.
In conclusion, the elevated blood eosinophil count was not associated with the severity of asthma among adult asthmatic patients. Lack of eosinophilia can be related to the low-T2 asthma phenotype. Elevated blood eosinophil counts were negatively associated with female sex and ED visits. However, the eosinophil values were higher in asthmatic patients infected with intestinal parasitic infection when compared to their counterparts. Therefore, different biomarkers will be considered in addition to eosinophil count for appropriate diagnosis and therapeutics among adult asthma patients.
Data Availability
All the data on which the conclusions of this manuscript were drawn are available from the corresponding author. So that anyone who needs the data can get it upon reasonable request.
Abbreviations
- ATS:
-
American Thoracic Society
- AOR:
-
Adjusted Odds Ratio
- BMI:
-
Body Mass Index
- CBC:
-
Complete Blood Count
- CI:
-
Confidence Interval
- COR:
-
Crude Odds Ratio
- ED:
-
Emergency Department
- ERS:
-
European Respiratory Society
- ICS:
-
Inhaled Corticosteroids
- IL:
-
Interleukin
- IP:
-
Intestinal Parasitic Infection
- GINA:
-
Global Initiative for Asthma
- OLIN:
-
Obstructive Lung Disease In Northern Sweden
- RBC:
-
Red Blood Cell
- SABA:
-
Short-acting beta 2 antagonists
- SC:
-
Systemic Corticosteroids
- SOP:
-
Standard Operating Procedure
- SPSS:
-
Statistical Package for Social Science
- TGSH:
-
Tibebe-Ghion Specialized Hospital
- Th2:
-
T Helper 2
- UGCSH:
-
University of Gondar Comprehensive Specialized hospital
- WSAS:
-
West Sweden Asthma Study
References
Global Initiative for Asthma (GINA). Global strategy for asthma management and prevention. 2021, available from: http://www.ginasthma.org/
World health organization (WHO) asthma fact sheet. 2021. https://www.who.int/news-room/fact-sheets/detail/asthma. Accessed date, December 2021.
Global Asthma Network (GAN). Auckland, New Zealand: The Global Asthma Report; 2018 [Accesed in May 2021]. Available from: http://www.globalasthmareport.org/Global%20Asthma%20Report%202018.pdf
Backman H, Räisänen P, Hedman L, Stridsman C, Andersson M, Lindberg A, et al. Increased prevalence of allergic asthma from 1996 to 2006 and further to 2016—results from three population surveys. Clin Experimental Allergy. 2017;47(11):1426–35.
Lötvall J, Ekerljung L, Rönmark EP, Wennergren G, Lindén A, Rönmark E, et al. West Sweden Asthma Study: prevalence trends over the last 18 years argues no recent increase in asthma. Respir Res. 2009;10(1):1–11.
To T, Stanojevic S, Moores G, Gershon AS, Bateman ED, Cruz AA, et al. Global asthma prevalence in adults: findings from the cross-sectional world health survey. BMC Public Health. 2012;12(1):1–8.
Kuruvilla ME, Lee F, Lee GB. Understanding asthma phenotypes, endotypes, and mechanisms of disease. Clin Rev Allergy Immunol. 2019;56(2):219–33.
Fahy JV. Type 2 inflammation in asthma—present in most, absent in many. Nat Rev Immunol. 2015;15(1):57–65.
Tran TN, Kerkhof M, Carter V, Price DB. Persistence of eosinophilic asthma endotype and clinical outcomes: a real-world observational study. J Asthma Allergy. 2021;14:727.
Israel E, Reddel HK. Severe and difficult-to-treat asthma in adults. N Engl J Med. 2017;377(10):965–76.
Khurana S, Bush A, Holguin F. Management of severe asthma: summary of the European Respiratory Society/American Thoracic Society task force report. Breathe. 2020;16(2).
Chen S, Golam S, Myers J, Bly C, Smolen H, Xu X. Systematic literature review of the clinical, humanistic, and economic burden associated with asthma uncontrolled by GINA steps 4 or 5 treatment. Curr Med Res Opin. 2018;34(12):2075–88.
Mukherjee M, Stoddart A, Gupta RP, Nwaru BI, Farr A, Heaven M, et al. The epidemiology, healthcare and societal burden and costs of asthma in the UK and its member nations: analyses of standalone and linked national databases. BMC Med. 2016;14(1):1–15.
Saglani S, Lloyd CM. Novel concepts in airway inflammation and remodeling in asthma. Eur Respir J. 2015;46(6):1796–804.
Possa SS, Leick EA, Prado CM, Martins MA, Tibério IFLC. Eosinophilic inflammation in allergic asthma. Front Pharmacol. 2013;4:46.
Price D, Wilson AM, Chisholm A, Rigazio A, Burden A, Thomas M, et al. Predicting frequent asthma exacerbations using blood eosinophil count and other patient data routinely available in clinical practice. J asthma allergy. 2016;9:1.
Talini D, Novelli F, Bacci E, Bartoli M, Cianchetti S, Costa F, et al. Sputum eosinophilia is a determinant of FEV1 decline in occupational asthma: results of an observational study. BMJ Open. 2015;5(1):e005748.
Zeiger RS, Schatz M, Dalal AA, Chen W, Sadikova E, Suruki RY, et al. Blood eosinophil count and outcomes in severe uncontrolled asthma: a prospective study. J Allergy Clin Immunology: Pract. 2017;5(1):144–53. e8.
Lalrinpuia B. Study on absolute eosinophil count correlation with severity of bronchial asthma. 2019.
Katz LE, Gleich GJ, Hartley BF, Yancey SW, Ortega HG. Blood eosinophil count is a useful biomarker to identify patients with severe eosinophilic asthma. Annals of the American Thoracic Society. 2014;11(4):531–6.
Zhang XY, Simpson JL, Powell H, Yang IA, Upham JW, Reynolds PN, et al. Full blood count parameters for the detection of asthma inflammatory phenotypes. Clin experimental allergy. 2014;44(9):1137–45.
Rönmark EP, Ekerljung L, Mincheva R, Sjölander S, Hagstad S, Wennergren G, et al. Different risk factor patterns for adult asthma, rhinitis, and eczema: results from West Sweden Asthma Study. Clin translational allergy. 2016;6:28.
Pakkasela J, Ilmarinen P, Honkamäki J, Tuomisto LE, Andersén H, Piirilä P, et al. Age-specific incidence of allergic and non-allergic asthma. BMC Pulm Med. 2020;20(1):9.
Warm K, Hedman L, Lindberg A, Lötvall J, Lundbäck B, Rönmark E. Allergic sensitization is age-dependently associated with rhinitis, but less so with asthma. J Allergy Clin Immunol. 2015;136(6):1559–65e2.
Eguiluz-Gracia I, Tay TR, Hew M, Escribese MM, Barber D, O’Hehir RE, et al. Recent developments and highlights in biomarkers in allergic diseases and asthma. Allergy. 2018;73(12):2290–305.
Sterk PJ, Sinha A. Emerging complexity in the biomarkers of exacerbation-prone asthma. American Thoracic Society; 2020. pp. 915–7.
Pavord ID, Holliday M, Reddel HK, Braithwaite I, Ebmeier S, Hancox RJ, et al. Predictive value of blood eosinophils and exhaled nitric oxide in adults with mild asthma: a prespecified subgroup analysis of an open-label, parallel-group, randomized controlled trial. The Lancet Respiratory Medicine. 2020;8(7):671–80.
Denlinger LC, Phillips BR, Ramratnam S, Ross K, Bhakta NR, Cardet JC, et al. Inflammatory and comorbid features of patients with severe asthma and frequent exacerbations. Am J Respir Crit Care Med. 2017;195(3):302–13.
Peters MC, Mauger D, Ross KR, Phillips B, Gaston B, Cardet JC, et al. Evidence for exacerbation-prone asthma and predictive biomarkers of exacerbation frequency. Am J Respir Crit Care Med. 2020;202(7):973–82.
Kimura H, Konno S, Makita H, Taniguchi N, Shimizu K, Suzuki M, et al. Prospective predictors of exacerbation status in severe asthma over a 3-year follow‐up. Clin Experimental Allergy. 2018;48(9):1137–46.
Stridsman C, Axelsson M, Warm K, Backman H. Uncontrolled asthma occurs in all GINA treatment steps and is associated with worse physical health–a report from the OLIN adult asthma cohort. J Asthma. 2021;58(5):586–95.
Global Initiative for Asthma (GINA). Global Strategy for Asthma Management and Prevention., 2019. Available at http://www.ginasthma.org. 2019; Accessed: December 20, 2019.
Corbridge SJ, Nyenhuis SM. Promoting physical activity and exercise in patients with asthma and chronic obstructive pulmonary disease. J Nurse Practitioners. 2017;13(1):41–6.
Keohane E, Otto CN, Walenga J. Rodak’s Hematology-E-Book: clinical principles and applications. Elsevier Health Sciences; 2019. Sixth edition.
Zeiger RS, Schatz M, Li Q, Chen W, Khatry DB, Gossage D, et al. High blood eosinophil count is a risk factor for future asthma exacerbations in adult persistent asthma. J Allergy Clin Immunology: Pract. 2014;2(6):741–50. e4.
Price DB, Rigazio A, Campbell JD, Bleecker ER, Corrigan CJ, Thomas M, et al. Blood eosinophil count, and prospective annual asthma disease burden: a UK cohort study. The Lancet Respiratory Medicine. 2015;3(11):849–58.
Pola-Bibian B, Dominguez-Ortega J, Vila-Nadal G, Entrala A, Gonzalez-Cavero L, Barranco P et al. Asthma exacerbations in a tertiary hospital: clinical features, triggers, and risk factors for hospitalization.Journal of investigational allergology & clinical immunology. 2016:0-
Tran TN, Khatry DB, Ke X, Ward CK, Gossage D. High blood eosinophil count is associated with more frequent asthma attacks in asthma patients. Ann Allergy Asthma Immunol. 2014;113(1):19–24.
Nagasaki T, Sato K, Kume N, Oguma T, Sunadome H, Ito I, et al. The prevalence and disease burden of severe eosinophilic asthma in Japan. J Asthma. 2019;56(11):1147–58.
Hasegawa K, Stoll SJ, Ahn J, Bittner JC, Camargo CA Jr. Prevalence of eosinophilia in hospitalized patients with asthma exacerbation. Respir Med. 2015;109(9):1230–2.
Husereau D, Goodfield J, Leigh R, Borrelli R, Cloutier M, Gendron A. Severe, eosinophilic asthma in primary care in Canada: a longitudinal study of the clinical burden and economic impact based on linked electronic medical record data. Allergy Asthma & Clinical Immunology. 2018;14(1):1–9.
Athanazio R, Stelmach R, Antila M, Machado A, Arruda LK, Neto A, et al. Cross-sectional, observational study to estimate the prevalence of the eosinophilic phenotype for brazilian patients with severe asthma: the BRAEOS study. Eur Respiratory Soc; 2020.
Bedolla-Barajas M, Morales-Romero J, Hernández-Colín DD, Larenas-Linnemann D, Mariscal-Castro J, Flores-Razo MM et al. Beyond eosinophilia: inflammatory patterns in patients with asthma. Journal of Asthma. 2020:1–16.
Kerkhof M, Tran T, Soriano J, Golam S, Gibson D, Hillyer EV, et al. Health Care Resource Use and costs of severe, uncontrolled asthma with high blood Eosinophil Counts in the UK General Population. B23 novel epidemiology, management, and outcomes in asthma. American Thoracic Society; 2017. pp. A2984–A.
Pease JE. Asthma, allergy, and chemokines. Curr Drug Targets. 2006;7(1):3–12.
Conroy DM, Williams TJ. Eotaxin and the attraction of eosinophils to the asthmatic lung. Respir Res. 2001;2(3):150.
Kaminsky RG, Soto RJ, Campa A, Baum MK. Intestinal parasitic infections and eosinophilia in a human immunodeficiency virus-positive population in Honduras. Memórias do Instituto Oswaldo Cruz. 2004;99(7):773–8.
Rahimi M, Mohammadzadeh T, Khanaliha K. Eosinophils and parasitic infections. Int J Enteric Pathogens. 2018;6(4):108–12.
Yasuda K, Kuroda E. Role of eosinophils in protective immunity against secondary nematode infections. Immunological Med. 2019;42(4):148–55.
Fulkerson PC, Fischetti CA, McBride ML, Hassman LM, Hogan SP, Rothenberg ME. A central regulatory role for eosinophils and the eotaxin/CCR3 axis in chronic experimental allergic airway inflammation. Proceedings of the National Academy of Sciences. 2006;103(44):16418-23.
Rönnebjerg L, Axelsson M. Severe Asthma in a General Population Study: Prevalence and Clinical Characteristics. 2021;14:1105–15.
Almqvist L, Rönmark E, Stridsman C, Backman H, Lindberg A, Lundbäck B et al. Remission of adult-onset asthma is rare: a 15-year follow-up study. ERJ Open Research. 2020;6(4).
Amelink M, de Groot JC, de Nijs SB, Lutter R, Zwinderman AH, Sterk PJ, et al. Severe adult-onset asthma: a distinct phenotype. J Allergy Clin Immunol. 2013;132(2):336–41.
Lima-Matos A, Ponte EV, de Jesus JPV, Almeida PCA, Lima VB, Kwon N, et al. Eosinophilic asthma, according to a blood eosinophil criterion, is associated with disease severity and lack of control among underprivileged urban brazilians. Respir Med. 2018;145:95–100.
Casciano J, Krishnan JA, Small MB, Buck PO, Gopalan G, Li C, et al. Value of peripheral blood eosinophil markers to predict severity of asthma. BMC Pulm Med. 2016;16(1):1–7.
Mathur SK, Viswanathan RK. Relevance of allergy in adult asthma. Curr Allergy Asthma Rep. 2014;14(5):437.
Sood A, Qualls C, Schuyler M, Arynchyn A, Alvarado JH, Smith LJ, et al. Adult-onset asthma becomes the dominant phenotype among women by age 40 years. The longitudinal CARDIA study. Annals of the American Thoracic Society. 2013;10(3):188–97.
De Marco R, Locatelli F, Sunyer J, Burney P. Differences in the incidence of reported asthma related to age in men and women: a retrospective analysis of the data of the european Respiratory Health Survey. Am J Respir Crit Care Med. 2000;162(1):68–74.
Räisänen P, Backman H, Hedman L, Andersson M, Stridsman C, Kankaanranta H et al. High but stable incidence of adult-onset asthma in northern Sweden over the last decades. ERJ Open Research. 2021;7(3).
Amelink M, de Nijs SB, de Groot JC, van Tilburg PM, van Spiegel PI, Krouwels FH, et al. Three phenotypes of adult-onset asthma. Allergy. 2013;68(5):674–80.
Breiteneder H, Peng YQ, Agache I, Diamant Z, Eiwegger T, Fokkens WJ, et al. Biomarkers for diagnosis and prediction of therapy responses in allergic diseases and asthma. Allergy. 2020;75(12):3039–68.
Chung KF, Wenzel SE, Brozek JL, Bush A, Castro M, Sterk PJ, et al. International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur Respir J. 2014;43(2):343–73.
Franco P, Pereira G, Giavina-Bianchi P, Agondi R. Inhaled corticosteroid use and its implication in peripheral eosinophil level. J Allergy Clin Immunol. 2020;145(2):AB28.
Lommatzsch M, Klein M, Stoll P, Virchow JC. Impact of an increase in the inhaled corticosteroid dose on blood eosinophils in asthma. Thorax. 2019;74(4):417–8.
Barnes PJ. Inhaled corticosteroids. Pharmaceuticals. 2010;3(3):514–40.
Fong EW, Levin RH. Inhaled corticosteroids for asthma. Pediatr Rev. 2007;28(6):e30–5.
Acknowledgements
The authors would like to thank the study participants and data collectors. Our acknowledgement also extends to the University of Gondar, College of Medicine and Health Science, School of Biomedical and Laboratory Science, Department of Hematology and Immunohematology.
Funding
The author(s) received no specific funding for this work.
Author information
Authors and Affiliations
Contributions
All authors have made substantial contribution on this research.
Conceptualization: YS
Analysis: YS, AB, AA, BM, TE
Investigation: YS, BL, AB, BW
Methodology: YS, AA, BM, TE, BW
Project administration: YS, BW, BM, AA
Supervision: YS
Validation: YS, AB, BM, TE, BL, BW
Writing original draft: YS
Writing, reviewing, and editing: YS, AA, BM, TE, BL, BW
Corresponding author
Ethics declarations
Ethical consideration
Ethical clearance was obtained from the ethical review committee of the School of Biomedical and Laboratory Science, College of Medicine and Health Sciences, University of Gondar, on March 3, 2021, with letter reference number SBMLS-2748. The Department of Hematology and Immunohematology provided a support letter, which was forwarded to the directors of UGCSH and TGSH. In addition, a permission letter to conduct research was obtained from the UGCSH and TGSH directors.
Informed written consent was obtained from each study participant after the objective of the study was explained. For illiterate patients, informed consent was obtained after objective of study and detailed information was read by data collectors. Then fingerprint signature was taken from each illiterate study participant and this prcedure was approved by ethical review committee of the School of Biomedical and Laboratory Science, College of Medicine and Health Sciences, University of Gondar. Study participants were identified by using codes rather than individual identifiers. The results and information of the study participants were kept confidential. Study participants who had elevated eosinophil counts were linked to the UGCSH and TGSH chronic outpatient departments for proper management. All methods were performed per the relevant guidelines and regulations (Declaration of Helsinki).
Consent for publication
Not applicable.
Conflict of Interest
The authors have no conflict of interest to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Solomon, Y., Malkamu, B., Berhan, A. et al. Peripheral blood eosinophilia in adult asthmatic patients and its association with the severity of asthma. BMC Pulm Med 23, 96 (2023). https://doi.org/10.1186/s12890-023-02383-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-023-02383-x