Abstract
Background
To monitor dypsnea and mortality at 5 and 10 years, respectively, after surgical treatment of tuberculosis-destroyed lung (TDL) patients.
Methods
TDL patients treated surgically at Beijing Chest Hospital from November 2007 to June 2019 were monitored in this observational study. Follow-up assessments of respiratory function indicators and survival conducted 5 and 10 years post-surgery led to patient grouping based on mMRC score into a dyspnea group (mMRC ≥ 1) and a non-dyspnea group (mMRC = 0). Cox regression analysis detected effects of patient demographics, clinical characteristics, surgical factors and respiratory function on 5 year post-surgical survival.
Results
By study completion (June 30, 2020), 32 of 104 patients were lost and 72 completed follow-up for a study total of 258.9 person-years. 45 patients (62.5%, 45/72) had mMRC scores of 0, while 12 (16.7%, 12/72), 21 (36.2%, 21/58) and 27 (60.0%, 27/45) patients exhibited dyspnea by 1, 3 and 5 years post-surgery, respectively. Low lung carbon monoxide diffusion score (DLCO% pred) and scoliosis contributed to dyspnea occurrence.
Conclusions
Most TDL patients lacked subjective dyspnea signs post-surgery, while dyspnea rates increased with time. Preoperative low lung diffusion function and Scoliosis were associated with factors for postoperative dyspnea. Surgical treatment increased TDL patient survival overall.
Similar content being viewed by others
Introduction
Tuberculous lung destruction (TDL) is characterized by diffuse structural damage to the lungs and a basic loss of respiratory function, which is very common in populations in developing countries [1, 2]. Hemoptysis, low fever, yellow sputum, chest tightness, and shortness of breath are the common symptoms in the patients. When developed the life-threatening hemoptysis symptom, surgical treatment is required [2,3,4]. Some patients with TDL have multidrug-resistant tuberculosis (MDR-TB) or extensively drug-resistant tuberculosis (XDR-TB), which could be treated surgically [4,5,6]. By the removal of ineffectively ventilated lung tissue, the ventilation/perfusion ratio could be improved, which relieves the patient’s dyspnea [7, 8]. Studies have shown that surgical treatment of TDL is effective, with complication rates is 9.6–45.7% [8,9,10]. Most previous TDL studies have focused on postoperative complications and mortality [11,12,13,14,15]. However, few studies focused on long-term TDL patient post-surgical prognosis based on long-term survival rates or clinical cure rates [16, 17]. In this study, we used Modified British Medical Research Council (mMRC) scores to evaluate TDL patient dyspnea and mortality for at least 12 months. The objective was to describe long-term outcomes of pulmonary resection surgical treatment of TDL patients by focusing on dyspnea incidence, survival of patients with severe dyspnea and factors contributing to long-term patient outcomes.
Materials and methods
Study subjects
Patients with TDL who underwent surgical treatment in the Department of Thoracic Surgery, Beijing Chest Hospital, Capital Medical University from November 2007 to June 2019 received follow-up for at least one year through June 30, 2020. The total follow-up time was 258.9 person-years and the median follow-up time was 3.85 years. The patient cohort included 44 males and 28 females of ages within the range of 37.9 ± 12.5 years. Postoperative dyspnea was defined as dyspnea with an mMRC score of ≥ 1 that first occurred in TDL patients between the time of postoperative discharge to the time of follow-up completion. Inclusion criteria included: (i) preoperative arterial blood gas analysis without respiratory failure; (ii) postoperative pathomorphology consistent with tuberculosis; (iii) surgical treatment performed according to the surgical indication of TDL. Exclusion criteria included: (i) bronchial asthma; (ii) chronic obstructive pulmonary disease; (iii) Interstitial lung disease; (iv) complicated disease due to malignant tumor; (v) chronic cardiac and rena insufficiency; (vi) chronic diseases identified during follow-up that directly affected mMRC scores.
The study design complied with the Helsinki Research Ethics Statement and was approved by the Ethics Committee of Beijing Chest Hospital (2018) Clinical Review No (43).
Data and methods
Demographic and general clinical data included age at onset, sex, body mass index (BMI) category (BMI < 18.5 underweight, BMI 18.5–24.9 normal, BMI ≥ 25 obese), smoking status, major complications (hypertension, coronary heart disease, diabetes), location of TDL disease (left, right) and presence or absence of chronic pulmonary aspergillosis and/or non-tuberculous mycobacterial infection.
The presence versus absence of lesion(s) in the contralateral lung (non-TDL lung) and of spinal scoliosis were determined using chest CT scans. The degree of scoliosis was assessed by measuring contralateral curvature angles (Cobb angles), with Cobb angles of ≤ 5 scored as normal and scores of > 5 scored as curved. A Jaeger Master Screen PFT device was used to measure lung function. Diffusing capacity of the lungs for carbon monoxide was measured using the single-breath method. Lung function data included forced vital capacity of predicted value (FVC% pred) and lung diffusion capacity for carbon monoxide of predicted value (DLCO% pred).
Surgical information collected for each patient reflected the extent of removal of lung lesions based on type of surgical intervention that included left or right lobectomy, lobectomy with pleural clearance and the left or right pneumonectomy with pleural clearance. Thoracoscopic surgery was performed in one case, while thoracotomy was performed in all other cases.
Follow-up
Face-to-face and telephone follow-up surveys were administered to TLD patients by trained health care practitioners from November 2008 to June 2020, for a median follow-up duration of 4.8 years. During the post-operative follow-up period, monitoring was conducted of both readmitted patients and those who were never readmitted in order to collect patient information with regard to postoperative antituberculous chemotherapy, mMRC score and survival status. Definitions of mMRC scores were as follows: 0, I have difficulty breathing only during strenuous exercise; 1, I get shortness of breath from walking briskly or climbing hills on flat ground; 2, Because of my shortness of breath, I walk more slowly on flat ground than my peers or need to stop to rest; 3, I need to stop and catch my breath after about 100 m or a few minutes on flat ground; 4, I had severe breathing difficulties that prevented me from leaving the house or from putting on or taking off my clothes. Based on mMRC scores, patients were divided into two groups: a non-dyspnea group (mMRC = 0) and a dyspnea group (mMRC ≥ 1). In this study, censored data were defined as an absence of dyspnea (n = 45) or loss of the patient to follow-up (n = 0) by June 2020. Re-hospitalization status and TLD surgery-associated factors responsible for readmittance included secondary bronchopleural fistula, repeated hemoptysis, infection, empyema, etc. as confirmed by two senior chief physicians. Regarding post-surgical use of anti-tuberculosis chemotherapy drugs, most patients complied with doctors’ recommendations and took their anti-tuberculosis chemotherapy drugs on time and completed the chemotherapy treatment course by 6–12 months post-surgery. However, a few patients did not take anti-tuberculosis drugs for economic or personal reasons.
Quality control
The follow-up plan and questionnaire were reviewed and verified by respiratory and thoracic surgery experts, while health doctors supervised the follow-up program. Face-to-face or telephone follow-up interviews to collect patient data were conducted by trained health care doctors who followed a standard procedure outlined in the study manual and used questionnaires that had been reviewed by the quality control team.
Statistical analysis
Categorical variables were expressed as numbers of cases and case proportions. The median and interquartilerange (IQR) were used to depict mMRC scores. The Wilcoxon-Sign rank sum test was used to compare differences of mMRC scores before and after surgical treatment of TDL patients, with compositions of mMRC groups before and after surgery compared using the McNemar Test. Results obtained using Cox models were interpreted based on dyspnea outcome as defined as the first occurrence of mMRC ≥ 1 detected during follow-up to June 2020; censored data was defined as no occurrence of dyspnea (mMRC ≥ 1, n = 45) or loss of patient to follow-up (n = 0) by June 2020. We incorporated risk factors (old age/low preoperative FEV1) based on risks reported previously [8, 13] and incorporated statistically significant variables revealed by the univariate Cox model into the multivariate Cox regression model. The stepwise variables selection method was used to screen for factors associated with dyspnea and Kaplan–meier method was used to plot the survival curve of patients with dyspnea according to mMRC ≥ 1 score. statistical analyses were performed using SPSS21.0 (SPSS, INC., Chicago, IL, USA).
Results
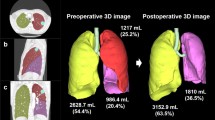
Follow-up monitoring of a total of 104 TDL patients who had undergone pulmonary resection surgery was conducted until June 30, 2020. Of the 104 cases, 32 cases were excluded from analysis, for a loss rate of 30.8% (32/104). For the 72 patients who completed follow-up, total follow-up times ranged from 1 to 5 years and the median follow-up time was 3.85 years (Fig. 1A).
Among 72 patients, 62.5% (45/72) of patients had no dyspnea (mMRC scores of 0) and received follow-up monitoring for 158.3 person-years. 37.5% (27/72) patients had varying degrees of dypsnea (with mMRC scores ≥ 1) and received follow-up monitoring for 100.6 person-years (Table 1). Proportions of patients with mMRC scores ≥ 1 in the first, third and fifth years after surgery were 12 (16.7%, 12/72), 21 (36.2%, 21/58) and 27 (60.0%, 27/45), respectively, of whom 2 patients received long-term home oxygen therapy (LTOT) for dyspnea due to secondary bronchopleural fistula (Fig. 1B).
Preoperative mMRC scores of 72 TDL patients were higher than their respective postoperative mMRC scores (P = 0.006). The difference in preoperative and postoperative numbers of patients in mMRC groups (mMRC = 0 vs. mMRC ≥ 1) was not statistically significant (P = 0.25). However, the preoperative proportion of patients within the mMRC ≥ 3 group (12.5%) was much greater than the corresponding postoperative proportion of patients in this group (0%) (Table 2).
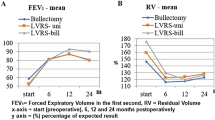
The results of univariate Cox regression showed that the incidence rate of cases with both TDL and scoliosis was higher than that of TDL cases without scoliosis (P = 0.001). In addition, the number of cases in the patient group with DLCO% pred < 80% was higher than the corresponding number in the patient group with DLCO% pred ≥ 80% (P = 0.044) (Table 3). Multivariate Cox regression analysis revealed that a value of DLCO% pred < 80% (HR: 2.735, 1.135–6.588) and scoliosis (HR: 4.467, 1.900–10.500) were risk factors for postoperative dyspnea (Table 4). The statistically significant difference between Kaplan–Meier curves stratified by DLCO% pred and scoliosis was also showed in Fig. 2.
During the follow-up period after TDL surgery, 5.5% (4/72) of patients were hospitalized for a second time, including 2 patients with bronchopleural fistula, 1 patient with relapse due to Mycobacterium tuberculosis infection and 1 patient with recurrent hemoptysis. Meanwhile, 94.4% (68/72) of patients were treated with antituberculotic drugs for treatment durations ranging from 0.1 to 72 months and a median treatment duration of 8 months (Table 4).
By the end of the follow-up period, 9 patients had died, with 3 patients dying on the 5th, 21st and 65th day after surgery due to multiple organ failure caused by excessive blood loss after thoracotomy for hemostasis. Another 3 patients died at home at 1, 3 and 5 years after surgery due to unknown causes, 2 patients died of lung cancer by 3 and 5 years after surgery and 1 patient died of pneumonia 9 years after surgery. Among the 9 patients who died, 5 patients were afflicted with both TDL and pulmonary Aspergillus infection, 1 with rheumatoid arthritis, and 1 with compulsory spondylitis (Table 5).
Binary logistic regression analysis revealed that male sex (OR: 12.6, 1.491–106.016), age > 60 years old (OR: 10.7, 2.168–53.002), preoperative acute massive hemoptysis (OR: 8.5, 1.531–47.182) and postoperative respiratory infections (OR: 3.927, 1.301–11.856) were statistically significant risk factors for postoperative death in TDL patients (Table 6).
Discussion
TDL was a secondary diagnosis in 1.3% of patients with tuberculosis [18]. Damaged lungs are prone to serious complications, including haemorrhage, empyema, secondary fungal infections and sepsis that can be treated by installation of a pulmonary systemic-shunt [19]. Severe hemoptysis can be treated effectively with surgery [2,3,4], which has also been shown to increase TDL patient long-term survival rates [11,12,13,14,15]. Results of one study demonstrated survival rates of 95% and 88% at 1 and 5 years after TDL surgery, respectively [17], while another study reported 5 year and 10 year survival rates of 94% and 87%, respectively [16]. Our results showed that survival rates at 1, 3, 5 and 10 years after TDL surgery were 98.6%, 95.1%, 90.0% and 66.7%, respectively, with improvement of dyspnea observed after surgery. Thus, these results suggest that TDL surgery can improve long-term survival rates, while also alleviating dyspnea.
In this study, TDL patients who received surgical treatment exhibited reduced rates of dyspnea (as compared to the preoperative rate) prior to discharge and at the end of long-term follow-up. Analysis of the possible mechanism underlying beneficial effects associated with surgical removal of diseased nonfunctional lung tissue revealed that nonfunctional lung tissue may have interfered with effective ventilation such that removal of these tissues led to intra-pulmonary arteriovenous shunting of blood that improved oxygenation and alleviated dyspnea. Meanwhile, persistence or emergence of postoperative dyspnea in some patients may have been associated with numerous diverse factors that caused further reduction of healthy lung tissue volume and degenerative changes that decreased lung function, warranting further investigation.
Our results suggest that scoliosis and preoperative DLCO% pred values < 80% are independent risk factors for postoperative dyspnea. The role played by scoliosis in perpetuating dyspnea after surgery may be due to the fact that TDL pneumonectomy cannot completely reverse scoliosis-induced impaired pulmonary ventilation and severely impaired restrictive ventilation. Meanwhile, low preoperative DLCO% values indicated the presence of TDL-induced severe and/or extremely severe pulmonary ventilation/perfusion dysregulation that could not be completely alleviated by surgical resection of lesions. Thus, in these patients surgery could not completely correct dysregulation of the pulmonary ventilation/perfusion ratio to adequately restore alveolar gas exchange, leading to persistence of postoperative dyspnea of variable severity. Nevertheless, very few patients with scoliosis required a long course of home oxygen therapy.
Our findings suggest that benefits and risks of surgery should be carefully assessed in patients with TDL with scoliosis and preoperative DLCO% pred values of < 80%. Moreover, enhanced pulmonary rehabilitation should be provided to this group of TDL patients after surgery.
In our follow-up observation cohort, a larger proportion of postoperative deaths occurred in males than females, accounting for 88.9% (8/9) and 55.6% (5/9) of pulmonary TB cases with coinfections with Aspergillus or non-mycobacteria, respectively. This result may reflect the fact that male TB patients are more likely to contract Aspergillus and non-mycobacterial infections than are females, due to greater exposures of males to the surrounding environment [20]. In Asia and Africa, 15.4% of TB cases are coinfected with Aspergillus or non-tuberculous mycobacteria, with Aspergillus coinfection significantly increasing risk of death [1]. In addition, our recent study demonstrated that TDL accompanied by chronic pulmonary aspergillosis was associated with an increase in number of serious postoperative complications in men [15]. Therefore, short- and long-term risks and benefits of surgery for men, especially those with pulmonary aspergillosis and/or non-pulmonary mycobacterial infection, need to be carefully evaluated.
This study had several limitations. First, it was a single-center observational follow-up study that utilized a patient cohort comprised of a limited number of cases, which may have led to biased results. Second, cases were monitored throughout a long-term follow-up period to collect data related to survival, respiratory function, rehospitalization and postoperative anti-TB treatment status. However, postoperative complications, postoperative psychological effects, such as anxiety and depression, as well as nutrition, exercise and other lifestyle factors and effects of confounding factors on respiratory function were not included in the analysis, which may have led to biased study results.
Conclusions
Most patients without signs of subjective dyspnea after TDL surgery enjoy good quality of life. However, as post-operative survival time increases, the number of patients with dyspnea increases, although very few patients require home oxygen therapy. Notably, preoperative low pulmonary diffusion function and scoliosis were associated with factors for postoperative dyspnea. Thus, for TDL patients with preoperative scoliosis, DLCO% pred < 80%, and male sex, benefits and risks of TDL surgery should be fully evaluated preoperatively, while enhanced pulmonary rehabilitation training should be provided postoperatively to this group of patients.
Availability of data and materials
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
- TDL:
-
Tuberculosis-destroyed lung
- mMRC:
-
Modified British medical research council
- MDR-TB:
-
Multidrug-resistant tuberculosis
- XDR-TB:
-
Extensively drug-resistant tuberculosis
- BMI:
-
Body mass index
- FVC% pred:
-
Forced vital capacity of predicted
- DLCO% pred:
-
Lung diffusion capacity for carbon monoxide of predicted
- CRP:
-
C-reaction protein
- OR:
-
Odds ratio
- CI:
-
Confidence interval
References
Bongomin F. Post-tuberculosis chronic pulmonary aspergillosis: an emerging public health concern. PLoS Pathog. 2020;16(8): e1008742.
Kosif Mısırlıoğlu A, Bayram S, Kıral H, Çoban Ağca M, Tokgöz Akyıl F, Alpay L, Baysungur V, Yalçınkaya İ. Factors affecting complication rates of pneumonectomy in destroyed lung. Turk gogus kalp damar cerrahisi dergisi. 2018;26(2):272–8.
Issoufou I, Sani R, Belliraj L, Ammor FZ, Moussa Ounteini A, Ghalimi J, Lakranbi M, Ouadnouni Y, Smahi M. Pneumonectomy for tuberculosis destroyed lung: a series of 26 operated cases. Rev Pneumol Clin. 2016;72(5):288–92.
Yuncu G, Ceylan KC, Sevinc S, Ucvet A, Kaya SO, Kiter G, Unsal S, Ozsinan F. Functional results of surgical treatment of bronchiectasis in a developing country. Arch Bronconeumol. 2006;42(4):183–8.
Treasure RL, Seaworth BJ. Current role of surgery in Mycobacterium tuberculosis. Ann Thorac Surg. 1995;59(6):1405–7 (Discussion 1408–1409).
Kir A, Tahaoğlu K, Okur E, Hatipoğlu T. Role of surgery in multi-drug-resistant tuberculosis: results of 27 cases. Eur J Cardio Thorac Surg Off J Eur Assoc Cardio Thorac Surg. 1997;12(4):531–4.
Kabiri EH, Hammoumi ME, Bhairis M, Oueriachi FE, Slaoui O, Amraoui M. Clinical and surgical analysis of lobectomy for destroyed lobe of the lung: a series of 47 patients. Asian Cardiovasc Thorac Ann. 2021;29(8):772–8.
Ruan H, Liu F, Han M, Gong C. Incidence and risk factors of postoperative complications in patients with tuberculosis-destroyed lung. BMC Pulm Med. 2021;21(1):273.
Blyth DF. Pneumonectomy for inflammatory lung disease. Eur J Cardio Thorac Surg Off J Eur Assoc Cardio Thorac Surg. 2000;18(4):429–34.
Shiraishi Y, Nakajima Y, Koyama A, Takasuna K, Katsuragi N, Yoshida S. Morbidity and mortality after 94 extrapleural pneumonectomies for empyema. Ann Thorac Surg. 2000;70(4):1202–6 (Discussion 1206–1207).
Bai L, Hong Z, Gong C, Yan D, Liang Z. Surgical treatment efficacy in 172 cases of tuberculosis-destroyed lungs. Eur J Cardio Thorac Surg Off J Eur Assoc Cardio Thorac Surg. 2012;41(2):335–40.
Halezeroglu S, Keles M, Uysal A, Celik M, Senol C, Haciibrahimoglu G, Arman B. Factors affecting postoperative morbidity and mortality in destroyed lung. Ann Thorac Surg. 1997;64(6):1635–8.
Huang CL, Zhang W, Ni ZY, Zuo T, Zhou M, Xu J, Yang ZF, Li L, Xiao J, Zhang DY. Efficacy of video-assisted thoracoscopic surgery for 29 patients with tuberculosis-destroyed lung. Int J Clin Exp Med. 2015;8(10):18391–8.
Sayir F, Ocakcioglu I, Şehitoğulları A, Çobanoğlu U. Clinical analysis of pneumonectomy for destroyed lung: a retrospective study of 32 patients. Gen Thorac Cardiovasc Surg. 2019;67(6):530–6.
Ruan H, Gong C, Wang J. The efficacy and safety of surgical treatment for patients with tuberculosis destroyed lung with or without chronic pulmonary aspergillosis. World J Surg. 2021;45(5):1595–601.
Kim YT, Kim HK, Sung SW, Kim JH. Long-term outcomes and risk factor analysis after pneumonectomy for active and sequela forms of pulmonary tuberculosis. Eur J Cardio Thorac Surg Off J Eur Assoc Cardio Thorac Surg. 2003;23(5):833–9.
Li Y, Hu X, Jiang G, Chen C. Pneumonectomy for treatment of destroyed lung: a retrospective study of 137 patients. Thorac Cardiovasc Surg. 2017;65(7):528–34.
Fawibe AE, Salami AK, Oluboyo PO, Desalu OO, Odeigha LO. Profile and outcome of unilateral tuberculous lung destruction in Ilorin Nigeria. West Afr J Med. 2011;30(2):130–5.
Kosar A, Orki A, Kiral H, Demirhan R, Arman B. Pneumonectomy in children for destroyed lung: evaluation of 18 cases. Ann Thorac Surg. 2010;89(1):226–31.
Stephen T, Thankachen R, Madhu AP, Neelakantan N, Shukla V, Korula RJ. Surgical results in bronchiectasis: analysis of 149 patients. Asian Cardiovasc Thorac Ann. 2007;15(4):290–6.
Acknowledgements
Not applicable.
Funding
Not applicable.
Ethics declarations
Ethics approval and consent to participate
The study design complies with the Helsinki Research Ethics Statement and was approved by the Ethics Committee of Beijing Chest Hospital (2018) Clinical Review No. (43). Informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ruan, H., Liu, F., Li, Y. et al. Long-term follow-up of tuberculosis-destroyed lung patients after surgical treatment. BMC Pulm Med 22, 346 (2022). https://doi.org/10.1186/s12890-022-02139-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-022-02139-z