Abstract
Background
Clinical efficacy of immune checkpoint inhibitors (ICIs) for non-small cell lung cancer (NSCLC) with uncommon histology (uNSCLC) is unknown.
Methods
Patients with NSCLC treated with ICI monotherapy between January 2014 and December 2018 in 10 Japanese hospitals were retrospectively evaluated. The patients were divided into: (1) NSCLC with common histology (cNSCLC), defined as adenocarcinoma and squamous cell carcinoma; and (2) uNSCLC, defined as incompatibility with morphological and immunohistochemical criteria for adenocarcinoma or squamous cell carcinoma. Propensity score matching was performed to balance the two groups.
Results
Among a total of 175 patients included, 44 with uNSCLC (10 pleomorphic carcinomas, 9 large cell neuroendocrine carcinomas, 2 large cell carcinomas, and 23 not otherwise specified) and 44 with matched cNSCLC (32 adenocarcinomas and 12 squamous cell carcinomas) were selected for analyses. Median progression-free survival (PFS) (4.4 months, 95% confidence interval [CI] 1.8–7.7 months) and overall survival (OS) (11.4 months, 95% CI 7.4–27.4 months) in the uNSCLC patients were not significantly different from those in matched cNSCLC patients (5.4 months, 95% CI 3.1–7.6 months, p = 0.761; and 14.1 months, 95% CI 10.6–29.6 months, p = 0.381). In multivariate analysis, Eastern Cooperative Oncology Group performance status (ECOG-PS) of 0–1 and programmed death ligand-1 (PD-L1) expression were predictive for PFS and OS in uNSCLC.
Conclusions
ICIs had similar clinical efficacy for treatment of uNSCLC and cNSCLC. Good ECOG-PS and PD-L1 expression were predictive for efficacy of ICIs in uNSCLC.
Similar content being viewed by others
Introduction
The emergence of immune checkpoint inhibitors (ICIs) has led to major changes in treatment paradigms for non-small cell lung cancer (NSCLC). Pembrolizumab, an anti-programmed death-1 (PD-1) antibody, or atezolizumab, an anti-programmed death ligand-1 (PD-L1) antibody, have demonstrated survival benefits over platinum-based chemotherapy in chemo-naïve patients with NSCLC [1, 2]. In previously treated patients with NSCLC, pembrolizumab, atezolizumab and nivolumab (anti-PD-1 antibody) have demonstrated long-term survival benefits over docetaxel [3,4,5,6]. Clinical guidelines recommend ICIs as first- second- or later-line treatments for unresectable NSCLC [7,8,9].
Although adenocarcinoma and squamous cell carcinoma are the dominant tumor pathologies in NSCLC, 8–18% of patients have uncommon histology, such as pleomorphic carcinoma, large cell neuroendocrine carcinoma (LCNEC), large cell carcinoma and not otherwise specified (NOS) [10,11,12,13]. As well as distinct histological features, NSCLC with uncommon histology (uNSCLC) has different clinical courses and poor therapeutic responses and prognosis compared with NSCLC with common histology (cNSCLC), such as adenocarcinoma or squamous cell carcinoma. For example, pleomorphic carcinoma of the lung is reported to progress aggressively and to be refractory to chemotherapy, with an objective response rate (ORR) of 17% and progression-free survival (PFS) of 2 months [14]. Patients with NSCLC-NOS are reported to have a median PFS of 5.9 months after first-line platinum-based chemotherapy, which is shorter than 7.3 months in patients with adenocarcinoma [15]. Patients with LCNEC have better clinical benefit from small cell lung cancer (SCLC)-based chemotherapy, such as etoposide/platinum, compared with NSCLC-based chemotherapy, such as gemcitabine/platinum, pemetrexed/platinum and paclitaxel/platinum [16].
However, little is known about the therapeutic benefits of ICIs for uNSCLCs. Some clinical trials for ICIs in NSCLC have included uNSCLCs; however, the proportion of uNSCLCs in the total study populations was only 2–7% [4, 5, 17, 18]. Given the distinct features and poor therapeutic responses to cytotoxic chemotherapy, it is unknown whether patients with uNSCLC have similar clinical benefits from ICIs as those with cNSCLC. In this multicenter retrospective study, we compared the efficacy of ICIs in patients with uNSCLC or cNSCLC using propensity-score-matched analysis. Additionally, we identified predictive factors for ICIs in patients with uNSCLC.
Materials and methods
Study design
This was a multicenter, retrospective cohort study that was approved by the Institutional Review Board of each participating institution. Patient consent was waved because it was a retrospective study. This study was registered with the University Hospital Medical Information Network (ID: UMIN000037777).
Patients
We retrospectively reviewed medical records of patients who were diagnosed with advanced or recurrent NSCLC between January 2014 and December 2018 in 10 hospitals in Japan. Patients with pathologically diagnosed NSCLC who received ICI monotherapy were included. Any lines of treatment were allowed if ICI monotherapy was administered. The recurrent stage was defined as recurrence after radical surgery and applicable for systemic therapy, but not for local therapy. Patients who received combination therapy with platinum-based chemotherapy and ICIs or had histories of previous ICI therapy were excluded. The patients were divided into 2 groups on the basis of pathological diagnosis: (1) cNSCLC, patients with adenocarcinoma or squamous cell carcinoma; and (2) uNSCLC, those without morphological and immunohistochemical criteria for adenocarcinoma or squamous cell carcinoma, such as pleomorphic carcinoma, large cell carcinoma, LCNEC or NOS. Pathological diagnosis was performed morphologically and immunologically at each institution.
Data collection
Clinical data, including age, sex, smoking history, pathology, PD-L1 tumor proportion score (TPS), cancer staging, Eastern Cooperative Oncology Group performance status (ECOG-PS), line of treatment, and type of ICI were obtained from the patients’ medical records. The responses to ICI were evaluated in accordance with the Response Evaluation Criteria in Solid Tumors (RESIST) version 1.1 [19]. Disease control rate (DCR) was defined as complete response (CR) plus partial response (PR) plus stable disease, and ORR as CR plus PR. PFS and OS were calculated from the date of first administration of ICI.
Propensity score matching
To balance the baseline of the two groups, 1:1 propensity score matching was performed. Propensity scores were calculated using a logistic regression model and included the following variables: age, sex, smoking status, cancer stage, PD-L1 TPS, line of ICI, and ECOG-PS.
Statistical analysis
Fisher’s exact test and Mann–Whitney U test were used for categorical and continuous variables, respectively. Kaplan–Meier method and the log-rank tests were used for PFS and OS. Cox proportional hazards regression analysis was used to identify predictive variables for PFS and OS. Logistic regression analysis was used to identify predictive variables for ORR and DCR. Variables of p < 0.100 in univariate analyses, pathology (uNSCLC vs. cNSCLC), and PD-L1 expression were included for multivariate analyses. All values are expressed as median (range) or number (%). A p value < 0.05 was considered significant. All statistical analyses were performed with EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan), which is a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria, version 2.13.0) [20].
Results
Patient characteristics
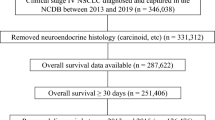
A total of 175 patients (44 uNSCLCs and 131 cNSCLCs) were included in the study. Patient characteristics are shown in Table 1. The uNSCLC group had a median age of 66 years, and most patients were men (95%), and most had a smoking history (95%) and good ECOG-PS of 0–1 (82%). Eight (18%), 10 (23%), and 16 (36%) patients in the uNSCLC group had brain, liver and bone metastases, respectively. The histological types were 10 (23%) pleomorphic carcinomas, 9 (20%) LCNECs, 2 (5%) large cell carcinomas, and 23 (52%) NOSs. No patient had epidermal growth factor receptor (EGFR) mutation or anaplastic lymphoma kinase (ALK) fusion. The expression of tumor PD-L1 was TPS ≥ 50% in 17 (39%) patients, 1–49% in 10 (23%), < 1% in 6 (14%), and not available in 11 (25%). The ICIs were administered as first-, second- or later-line in 7 (16%), 22 (50%) and 15 (34%) patients, respectively. Of these, 22 (50%), 16 (36%) and 6 (14%) patients received nivolumab, pembrolizumab and atezolizumab, respectively. The unmatched cNSCLC group had a significantly lower proportion of men (p = 0.010), higher proportion of stage IV disease (p = 0.004), better ECOG-PS (p = 0.001), and less liver metastasis (p = 0.039) compared with the uNSCLC group. A significantly higher proportion of patients in the unmatched cNSCLC group was not evaluated the tumor PD-L1 status (p < 0.001). Seven (5%) patients and one (1%) patient in the unmatched cNSCLC group had EGFR gene mutation and ALK fusion gene, respectively. After 1:1 propensity score matching, 44 patients with cNSCLC were selected (matched cNSCLC) (Fig. 1). The matched cNSCLC group had comparable patients’ demographics to the uNSCLC group. Only one patient had an active driver mutation (in EGFR) in the matched cNSCLC group.
In the uNSCLC group, 7 (16%) patients were still receiving ICIs at the time of data cutoff and the remaining 37 (84%) were not receiving ICIs because of progressive diseases (n = 27), adverse events (n = 8) or physician’s decision (n = 2) (Fig. 1). In the matched cNSCLC group, only 4 (9%) patients were still receiving ICIs while the other 40 (91%) were not receiving ICIs because of progressive diseases (n = 31), adverse events (n = 7) or physician’s decision (n = 2). The median follow-up time was 11.9 months (range 0.1–43.8 months).
Efficacy of ICIs
The ORR of 30% (95% confidence interval [CI], 17–45%) in the uNSCLC group was comparable with 34% (95% CI, 20–50%) in the matched cNSCLC group (p = 0.819) (Fig. 2A) (Table 2). The DCR of 61% (95% CI, 45–76%) in the uNSCLC group was comparable with 61% (95% CI, 45–76%) in the matched cNSCLC group (p = 1.000) (Fig. 2B) (Table 2). The median PFS of 4.4 months (95% CI 1.8–7.7 months) in the uNSCLC group was not significantly different from 5.4 months (95% CI 3.1–7.6 months) in the matched cNSCLC group (p = 0.761) (Fig. 3A). The median OS of 11.4 months (95% CI 7.4–27.4 months) in the uNSCLC group was comparable with 14.1 months (95% CI 10.6–29.6 months) in the matched cNSCLC group (p = 0.381) (Fig. 3B).
Univariate and multivariate analyses for efficacy of ICIs
In univariate analysis, PD-L1 expression and first-line treatment were predictive for ORR, and ECOG-PS and PD-L1 expression were predictive for DCR (Additional file 1: Tables S1 and S2). In multivariate analysis, PD-L1 expression was predictive for ORR and DCR, and ECOG-PS was predictive for ORR (Additional file 1: Tables S1 and S2). In univariate Cox proportional hazard analysis, ever-smokers, ECOG-PS of 0–1, and PD-L1 expression (both TPS ≥ 50% and ≥ 1%) were significant predictive factors for PFS. In multivariate analysis, ECOG-PS of 0–1 and PD-L1 expression were independent predictive factors for PFS (Table 3). Ever-smokers and ECOG-PS of 0–1 were independent predictive factors for OS in multivariate analysis, while PD-L1 TPS ≥ 50% demonstrated a borderline predictive significance and TPS ≥ 1% did not (Table 4). Meanwhile, uNSCLC was not predictive for ORR, DCR, PFS or OS. Additionally, the presence of brain, liver, and bone metastases or line of ICI treatment was not predictive for ORR, DCR, PFS or OS. When limited to the patients with uNSCLC, ECOG-PS of 0–1 and PD-L1 expression were independent predictive factors for PFS and OS (Additional file 1: Tables S3 and S4).
Subgroup analyses of histological subtypes
Patients with uNSCLC were evaluated on the basis of histological subtype (Additional file 1: Table S5). In pleomorphic carcinoma, tumor PD-L1 showed TPS ≥ 50% in 5 (50%) patients, 1–49% in 3 (30%) patients, and < 1% in 0 (0%) patients; PD-L1 was not evaluated in 2 patients (20%). In LCNEC, TPS was ≥ 50% in 1 (11%) patient, 1–49% in 1 (11%) patient, < 1% in 4 (44%) patients, and not evaluated in 3 (33%) patients. In NOS, TPS was ≥ 50% in 9 (39%) patients, 1–49% in 6 (26%) patients, < 1% in 2 (9%) patients, and not evaluated in 6 (26%). The median PFS and OS were 7.7 months (95% CI: 0.4 months–not estimated [NE]) and 9.5 months (95% CI: 1.2 months–NE) in pleomorphic carcinoma, respectively; 1.3 months (95% CI: 0.1 months–NE) and 3.8 months (95% CI: 0.1 months–NE) in LCNEC; and 4.1 months (95% CI: 1.8–6.4 months) and 13.8 months (95% CI: 6.5–24.2 months) in NOS (Additional file 1: Fig. S1 A–B). No significant difference in PFS and OS was observed in subtypes in the uNSCLC group compared with the matched cNSCLC group.
Patients in the matched cNSCLC were also evaluated separately on the basis of their histological subtypes (Additional file 1: Table S6). The expression of tumor PD-L1 was TPS ≥ 50% in 13 (41%) patients, 1–49% in 8 (25%), < 1% in 3 (9%), and not evaluated in 8 (25%) in adenocarcinoma; and ≥ 50% in 2 (17%), 1–49% in 4 (33%), < 1% in 2 (17%), and not evaluated in 4 (33%) in squamous cell carcinoma. The median PFS and OS were 4.2 months (95% CI: 1.8–7.8 months) and 16.8 months (95% CI: 13.7–29.6 months) in adenocarcinoma; and 3.2 months (95% CI: 1.8–5.3 months) and 12.5 months (95% CI: 9.2–19.4 months) in squamous cell carcinoma (Additional file 1: Fig. S2 A-B). There was no significant difference in PFS (p = 0.132) and OS (p = 0.070) between adenocarcinoma and squamous cell carcinoma.
Discussion
In the current study, we found that ICIs were efficacious for patients with uNSCLC and those with cNSCLC with comparable demographic characteristics after propensity score matching. Good ECOG-PS and high PD-L1 expression were significant predictive factors for efficacy of ICIs, regardless of tumor histology. Patients with uNSCLC are known to demonstrate insufficient response to chemotherapy. However, our data indicate that ICIs may provide therapeutic benefits even for patients with uNSCLC, especially those who have good ECOG-PS and high PD-L1 expression.
The median PFS of 4.4 months and median OS of 11.4 months after ICI monotherapy in the current study were comparable with those in previous studies of ICI monotherapy in patients who mostly had cNSCLC (PFS, 2.3–4.0 months and OS, 9.2–13.8 months) [3,4,5,6]. In a retrospective study of 21 patients with LCNEC who received ICI monotherapy, median PFS and OS were 4.2 and 11.8 months, respectively [21]. In 49 patients with pulmonary pleomorphic carcinoma who received ICI monotherapy, median PFS and OS were 7.2 and 22.2 months, respectively [22]. Given that conventional chemotherapies for NSCLC often provide limited survival benefits for lung cancer with uncommon histology, ICI monotherapy can be considered as a treatment option [14,15,16].
Tumor PD-L1 expression is a gold standard biomarker for the efficacy of ICIs in NSCLC; however, the level of tumor PD-L1 expression and its predictive ability varies among different tumor types. For example, only 13.5% of patients with gastric cancer had PD-L1 TPS ≥ 1% and the efficacy of nivolumab was not associated with PD-L1 expression [23]. Furthermore, in renal cell carcinoma, 11% and 24% of patients had PD-L1 TPS ≥ 5% and ≥ 1%, respectively, and the efficacy of nivolumab was not associated with PD-L1 expression [24]. Although uNSCLC has different pathological features from cNCSLC, tumor PD-L1 expression (TPS ≥ 1%) was observed in ~ 60% of the patients with uNSCLC and was also predictive for efficacy of ICIs.
Good ECOG-PS, a well-known predictive factor for the efficacy of ICIs in NSCLC, was also predictive in uNSCLC [11, 12, 25, 26]. Although precise mechanisms underlying ECOG-PS and the efficacy of ICIs are unknown, poor general condition may reflect deteriorated host immune status and lead to weakened effector T cells. When compared with cNSCLC, uNSCLC tends to progress rapidly and be resistant to standard chemotherapy [14, 15]. Therefore, it is suggested that patients with uNSCLC are predisposed toward poor general condition without adequate treatments. Approximately 20% of the patients with uNSCLC had poor ECOG-PS ≥ 2, compared with only 3% of those with unmatched cNSCLC. Our data suggest that early initiation of ICIs may be considered for patients with uNSCLC, especially if they have high PD-L1 expression and good ECOG-PS.
There were two main limitations to this study. First, differences in PD-L1 expression and the efficacy of ICIs among different histological subtypes of uNSCLC were unknown, because of the limited number of patients and 25% of the patients did not undergo PD-L1 testing. It is reported that 80% of patients with pleomorphic carcinoma had high PD-L1 expression and favorable clinical response to ICIs (median PFS 7.2 months and median OS 22.2 months) [22]. Only 10–22% of patients with LCNEC had PD-L1 expression and had median PFS of 4.2 months and median OS of 11.8 months [21, 27, 28]. In the current study, the patients with pleomorphic carcinoma had the highest proportion of PD-L1 expression and the longest PFS, whereas those with LCNEC had the lowest PD-L1 and the worst PFS. It is possible that the clinical impact of PD-L1 expression and efficacy of ICIs differed owing to the histological subtypes of uNSCLC. Second, we only evaluated ICI monotherapy. Several single or combination therapeutic strategies for ICIs have emerged, such as cytotoxic T-lymphocyte antigen-4 antibody therapy, combination therapy with ICI and chemotherapy, and combinations of different ICI agents [17, 18, 29]. The clinical benefits of the novel ICIs for uNSCLC are unknown and should be investigated further.
Conclusions
ICIs had similar clinical efficacy for treatment of uNSCLC and cNSCLC. Additionally, good ECOG-PS and high PD-L1 expression were predictive for the efficacy of ICIs in uNSCLC.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Reck M, Rodriguez-Abreu D, Robinson AG, et al. Pembrolizumab versus chemotherapy for PD-L1-positive non-small-cell lung cancer. N Engl J Med. 2016;375:1823–33.
Herbst RS, Giaccone G, de Marinis F, et al. Atezolizumab for first-line treatment of PD-L1-selected patients with NSCLC. N Engl J Med. 2020;383:1328–39.
Brahmer J, Reckamp KL, Baas P, et al. Nivolumab versus docetaxel in advanced squamous-cell non-small-cell lung cancer. N Engl J Med. 2015;373:123–35.
Borghaei H, Paz-Ares L, Horn L, et al. Nivolumab versus docetaxel in advanced nonsquamous non-small-cell lung cancer. N Engl J Med. 2015;373:1627–39.
Herbst RS, Baas P, Kim DW, et al. Pembrolizumab versus docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): a randomised controlled trial. Lancet. 2016;387:1540–50.
Rittmeyer A, Barlesi F, Waterkamp D, et al. Atezolizumab versus docetaxel in patients with previously treated non-small-cell lung cancer (OAK): a phase 3, open-label, multicentre randomised controlled trial. Lancet. 2017;389:255–65.
National Comprehensive Cancer Network, NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines), non-small cell lung cancer. version 4. 2021. https://www.nccn.org/professionals/physician_gls/pdf/nscl.pdf. Accessed 16 May 2021.
Planchard D, Popat S, Kerr K, et al. Metastatic non-small cell lung cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2018;29:iv192–237.
Hanna NH, Schneider BJ, Temin S, et al. Therapy for stage IV non-small-cell lung cancer without driver alterations: ASCO and OH (CCO) joint guideline update. J Clin Oncol. 2020;38:1608–32.
Yang P, Allen MS, Aubry MC, et al. Clinical features of 5,628 primary lung cancer patients: experience at Mayo Clinic from 1997 to 2003. Chest. 2005;128:452–62.
Lin SY, Yang CY, Liao BC, et al. Tumor PD-L1 expression and clinical outcomes in advanced-stage non-small cell lung cancer patients treated with nivolumab or pembrolizumab: real-world data in Taiwan. J Cancer. 2018;9:1813–20.
Morita R, Okishio K, Shimizu J, et al. Real-world effectiveness and safety of nivolumab in patients with non-small cell lung cancer: a multicenter retrospective observational study in Japan. Lung Cancer. 2020;140:8–18.
Travis WD, Brambilla E, Nicholson AG, et al. The 2015 World Health Organization classification of lung tumors: impact of genetic, clinical and radiologic advances since the 2004 classification. J Thorac Oncol. 2015;10:1243–1260.
Vieira T, Girard N, Ung M, et al. Efficacy of first-line chemotherapy in patients with advanced lung sarcomatoid carcinoma. J Thorac Oncol. 2013;8:1574–7.
Righi L, Vavala T, Rapa I, et al. Impact of non-small-cell lung cancer-not otherwise specified immunophenotyping on treatment outcome. J Thorac Oncol. 2014;9:1540–6.
Sun JM, Ahn MJ, Ahn JS, et al. Chemotherapy for pulmonary large cell neuroendocrine carcinoma: similar to that for small cell lung cancer or non-small cell lung cancer? Lung Cancer. 2012;77:365–70.
Socinski MA, Jotte RM, Cappuzzo F, et al. Atezolizumab for first-line treatment of metastatic nonsquamous NSCLC. N Engl J Med. 2018;378:2288–301.
Gandhi L, Rodriguez-Abreu D, Gadgeel S, et al. Pembrolizumab plus chemotherapy in metastatic non-small-cell lung cancer. N Engl J Med. 2018;378:2078–92.
Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45:228–47.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48:452–8.
Sherman S, Rotem O, Shochat T, Zer A, Moore A, Dudnik E. Efficacy of immune check-point inhibitors (ICPi) in large cell neuroendocrine tumors of lung (LCNEC). Lung Cancer. 2020;143:40–6.
Lee J, Choi Y, Jung HA, et al. Outstanding clinical efficacy of PD-1/PD-L1 inhibitors for pulmonary pleomorphic carcinoma. Eur J Cancer. 2020;132:150–8.
Kang YK, Boku N, Satoh T, et al. Nivolumab in patients with advanced gastric or gastro-oesophageal junction cancer refractory to, or intolerant of, at least two previous chemotherapy regimens (ONO-4538-12, ATTRACTION-2): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2017;390:2461–71.
Motzer RJ, Escudier B, McDermott DF, et al. Nivolumab versus everolimus in advanced renal-cell carcinoma. N Engl J Med. 2015;373:1803–13.
Juergens RA, Mariano C, Jolivet J, et al. Real-world benefit of nivolumab in a Canadian non-small-cell lung cancer cohort. Curr Oncol. 2018;25:384–92.
Crinò L, Bidoli P, Delmonte A, et al. Italian cohort of nivolumab expanded access program in squamous non-small cell lung cancer: Results from a real-world population. Oncologist. 2019;24:e1165–71.
Eichhorn F, Harms A, Warth A, Muley T, Winter H, Eichhorn ME. PD-L1 expression in large cell neuroendocrine carcinoma of the lung. Lung Cancer. 2018;118:76–82.
Tsuruoka K, Horinouchi H, Goto Y, et al. PD-L1 expression in neuroendocrine tumors of the lung. Lung Cancer. 2017;108:115–20.
Hellmann MD, Paz-Ares L, Bernabe Caro R, et al. Nivolumab plus Ipilimumab in advanced non-small-cell lung cancer. N Engl J Med. 2019;381:2020–31.
Acknowledgements
We would like to acknowledge patients and their families. We thank Cathel Kerr, BSc, PhD, from Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
KM has full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. MK participated in study concept and design; acquisition, analysis and interpretation of data; statistical analyses; and drafting of the manuscript. NI participated in study concept and design, interpretation of data, drafting of the manuscript, and supervision. YI, HH, YS, KF, TF, NE and YN participated in study concept and design, interpretation of data, and drafting of the manuscript. MK, TM, MN, KK, MT, SM, SM, KA, MF, HK and HM participated in study concept and design, data acquisition, and drafting of the manuscript. TS participated in study concept and design, drafting of the manuscript, and supervision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Institutional Review Board of Hamamatsu University School of Medicine (No. 19–122).
Consent to participate
Not applicable.
Competing interests
All authors have no conflict of interest in relation to this manuscript.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. Table S1. Logistic regression analysis for objective response. Table S2. Logistic regression analysis for disease control rate. Table S3. Cox proportional hazard analysis for progression-free survival in uncommon non-small cell lung cancer. Table S4. Cox proportional hazard analysis for overall survival in uncommon non-small cell lung cancer. Table S5. Patient characteristics according to histological subtypes in uncommon non-small cell lung cancer. Table S6. Patient characteristics according to histological subtypes in matched common non-small cell lung cancer. Fig. S1. Kaplan-Meier curves for progression-free survival and overall survival by histology in uncommon non-small cell lung cancer group. Fig. S2. Kaplan-Meier curves for progression-free survival and overall survival by histology in matched common non-small cell lung cancer group.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Miyashita, K., Karayama, M., Inoue, Y. et al. Efficacy of immune checkpoint inhibitors in non-small cell lung cancer with uncommon histology: a propensity-score-matched analysis. BMC Pulm Med 21, 309 (2021). https://doi.org/10.1186/s12890-021-01681-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-021-01681-6