Abstract
Background
Chronic obstructive pulmonary disease (COPD) is a major public health problem. The present study aims to provide a global and regional estimate of the prevalence of COPD based on spirometry according to the two most widely used diagnostic criteria of COPD: fixed ratio (FR) and lower limit of normal (LLN).
Methods
We conducted a systematic review of the literature according to PRISMA guidelines. MEDLINE, Web of Sciences, and Scopus databases were searched to identify studies on the spirometry-based prevalence of COPD in individuals aged 40 years and older. The meta-analysis was performed using MedCalc 19 software.
Results
In total, 42 of the 3393 studies reviewed were eligible for inclusion. The overall prevalence of COPD in people aged 40 years and older was 12.64% (95% CI 10.75%-14.65%) and 7.38% (95% CI 5.47% − 9.55%) based on FR and LLN criteria, respectively. By gender, men had a higher prevalence of COPD compared to women (15.47%; 95% CI 12.22%-19.02% for men versus 8.79%; 95% CI 6.94%-10.82% for women). Using the LLN criteria, the prevalence of COPD in both sexes was almost identical (8.67%; 95% CI 8.44%- 8.90% for men and 8.00%; 95% CI 6.42% − 9.73% for women). We reported a high prevalence of COPD among smokers and the elderly by both definitions of airway obstruction. Regional prevalence estimates using the FR definition indicate that the highest COPD prevalence was recorded in the Americas and the lowest was recorded in the Eastern Mediterranean region. Using the LLN definition, the highest prevalence was recorded in the Southeast Asian region and the lowest prevalence was recorded in the American region. The most common COPD stage was stage II, with a prevalence of 50.46%. The results indicate a huge lack of prevalence data in the African and Eastern Mediterranean region. The results were given using a random-effect model due to the high heterogeneity between studies.
Conclusion
Results show that the prevalence of COPD differs according to the diagnostic criteria used. In addition, management and prevention strategies targeting risk factors for COPD are certainly needed to reduce the global burden of this chronic respiratory disease.
Similar content being viewed by others
Background
Chronic obstructive pulmonary disease (COPD) is defined as a heterogeneous lung condition characterized by chronic respiratory symptoms (dyspnea, cough, and expectoration) due to persistent abnormalities of the airways and/or alveoli that often result in progressive airflow limitation [1]. It represents a real challenge for global health systems, with significant socioeconomic and health consequences [2]. According to the World Health Organization (WHO), COPD is considered among the top ten causes of death worldwide [3]. In 2016, 251 million cases of COPD were recorded worldwide, according to estimates from the Global Burden of Disease (GBD) study [4]. It imposes a massive burden, mainly due to the high cost and its negative impact on the quality of life of affected patients [5]. COPD is an important cause of mortality. Between 2009 and 2019, the mortality rate of COPD increased by 35.4% [6]. Furthermore, WHO mortality and disease burden projections state that COPD will be the third leading cause of death worldwide by 2030 [7].
COPD is a multifactorial disease, with tobacco smoke being the best-known and most important risk factor for irreversible airflow obstruction [8, 9]. However, non-smokers can also develop COPD. Estimates suggest that 25–45% of COPD cases are non-smokers [10]. Outdoor and indoor air pollution from biomass smoke, occupational exposures to dust and chemical gases in the workplace, male gender, advanced age, low body mass index, history of respiratory diseases, and family history of respiratory diseases are all factors listed as having a role in the development of COPD in non-smokers [11, 12].
Worldwide, COPD remains an underestimated and underdiagnosed disease. The main causes of underdiagnosis identified in the literature are lack of knowledge of the disease on the part of patients and physicians, underestimation of symptoms, and underuse of the spirometer to establish the diagnosis [13]. Indeed, the spirometer is the gold standard for the diagnosis of COPD [14, 15]. The most frequently used diagnostic criteria are the fixed ratio (FR), which states that the presence of a ratio of forced expiratory volume in one second (FEV1) to forced vital capacity (FVC) post-bronchodilator less than 0.70 confirms the diagnosis, and the lower limit of normal (LLN) criteria, in which the diagnosis is based on the comparison of values measured by spirometry with reference values identified from healthy and non-smoking subjects [1, 16]. Non-use of pulmonary function testing and over-reliance on clinical diagnosis can lead to misdiagnosis of airflow obstruction, as evidenced by data from the published literature, which showed that spirometry assessment revealed that 43.8% of cases diagnosed by a physician were misdiagnosed [17].
Estimating the global prevalence of COPD is crucial to understanding its magnitude and reducing the burden of disease associated with this chronic condition. Systematic reviews and meta-analyses of global COPD prevalence estimates exist in the literature. For example, Adeloye et al. reported the summary global prevalence of COPD without considering the case definitions used [18]. In addition, Vermaghani and colleagues estimated the prevalence of COPD based only on studies using the fixed ratio as the diagnostic criteria [19]. One study estimated the worldwide prevalence of COPD using the FR and LLN criteria [20]. The main objective of this review is to provide a recent estimate of the global and regional prevalence of COPD according to the FR and LLN criteria over the past 6 years. Our study also aims to estimate the prevalence of COPD according to several parameters, such as gender, severity stage, age groups, and smoking status, using both diagnostic criteria. These estimates will serve as a basis for understanding the burden of COPD worldwide and for developing effective prevention and management strategies to address it.
Materials and methods
This review was developed according to the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) [21] (Additional File 1).
Inclusion criteria
The inclusion criteria in this systematic literature review included (i) studies reporting the prevalence of COPD based on spirometry testing; (ii) studies reporting the prevalence of COPD in people aged 40 years and older based on spirometry testing; (iii) studies published between 2016 and 2022; (iv) publications published in English and French; and (v) studies in open access.
Information source
We conducted a literature search of the MEDLINE, Web of Sciences, and Scopus databases to identify relevant studies related to the research objective and published between January 2016 and July 2022, using the following keywords: COPD, prevalence, and epidemiology. A combination of keywords using search operators was performed to refine the search results and identify relevant publications.
Studies selection
The studies identified by the literature search were first selected on the basis of their titles and abstracts. If there was uncertainty about the eligibility of a study, a second selection was made by consulting the full text. Studies that did not meet the eligibility criteria were excluded from the analysis. Reference lists of the selected studies and related reviews of literature were manually checked for potential inclusions. The study selection process was performed by two postgraduate students and two professors.
Data extraction
To extract data from the included studies, a data extraction form was created on Microsoft Excel. The form included; (a) title; (b) first author’s name; (c) journal name; (d) publication year; (e) publication language; (f) study design; (g) study location; (h) study objective; (i) data collection tools; (j) COPD diagnostic criteria; k) results found; and l) the author’s observations and conclusions.
Quality assessment of included studies
To assess the quality of the studies included in this review, we used the STROBE quality assessment checklist (Strengthen The Reporting of Observational Studies in Epidemiology) [22,23,24]. The assessment was based on five criteria: study objective, sampling technique, sample size, measurement of lung function, and diagnostic criteria used.
When the study objective was well defined, we assigned a score of 1, otherwise,a score of 0 was assigned. If the study used a random sampling technique, we gave it a score of 1. If the study used a non-random sampling technique or did not mention the technique used, we gave it a score of 0. If the sample size was greater than 384 participants and/or the calculation was well defined, we gave a score of 1, otherwise, a score of 0 was given. Regarding the assessment of lung function, we assigned a score of 1 for all studies since we only included studies reporting the prevalence of COPD based on a spirometry test. We assigned a score of 2 if the diagnosis of COPD was made on the basis of the FR criteria. When the LLN criteria were used, a score of 1 was assigned. A total score of 6 points indicates that the study is of high quality. When a score of 4 or 5 points has been obtained, the study is considered to be of moderate quality. Lower scores of 3, 2, 1 and 0 indicate that the study is of low quality.
Data synthesis and analysis
Given the high level of heterogeneity, a rondom effect meta-analysis was performed. The choice of meta-analysis model (random effect, fixed effect, or mixed effect) was determined by the existence or presence of heterogeneity between the included studies. Inter-study heterogeneity was measured by the I2 test to estimate the percentage of variability between the included studies [25, 26]. An I2 value > 70% indicates high heterogeneity. Heterogeneity is said to be moderate if the I2 value is between 70 and 50%. An I2 < 50% indicates low heterogeneity between the results of the studies [27, 28]. Forest plots were based on the prevalence of COPD according to the two diagnostic criteria FR and LLN. A meta-regression was performed to provide COPD estimates of COPD by several parameters and to detect sources of heterogeniety. A sensitivity analysis was performed to see the effect of studies with a high weight on the overall results of the meta-analysis. The meta-analysis was performed using MedCalc version 19.4 statistical software (MedCalc Software bv; https://www.medcalc.org; 2019). Egger’s test is used to assess the risk of bias between studies while visualizing the symmetry or asymmetry of the funnel plots.
Results
Studies selection
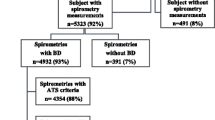
A total of 3993 potentially relevant records were identified through a database search (1372 studies identified from Scopus, 1692 identified from the Web of Sciences, and 929 identified from MEDLINE). After deleting 1333 duplicates, 2276 were excluded on the basis of their titles and abstracts. Full-text reading of 384 articles excluded 342 that did not meet the eligibility criteria. Overall, 42 studies meeting the inclusion criteria were included in this systematic review of the literature and meta-analysis (Fig. 1).
Characteristics of the included studies
All of the studies included in the review were published in the English language. Seven studies were published in 2022, seven in 2021, seven in 2020, four in 2019, four in 2018, four in 2017, and nine studies were published in 2016. Thirty-seven studies used a cross-sectional design while a longitudinal design was used by only five studies. Eligible studies were conducted in twenty-three countries. Twenty-three studies were conducted in the Western Pacific region, eight in the European region, four in the Americas region, three in the Southeast Asian region, three in the Eastern Mediterranean region, and only one study was conducted in the African region. Regarding the study area, thirty-one studies were conducted in a mixed area, nine in urban areas, and two in rural areas. The total sample size was 339475 participants aged 40 years and older and ranged from 141 to 94551 participants. The mean age of the participants was 57.30 years and ranged from 44 to 68 years. To make the diagnosis of COPD, twenty-four studies used the FR, criteria and six studies used the LLN criteria. Twelve studies made the diagnosis of persistent obstruction using both criteria at the same time (Table 1).
Quality of included studies
Of the forty-two eligible studies, twenty-one were of high quality, and twenty-one were of moderate quality. No study was of low quality. Table 2 shows the scores awarded according to each evaluation criteria and the total score for each study.
Estimated overall prevalence of COPD
The overall prevalence of COPD in people aged 40 years and above was 12.64% (95% CI 10.75%-14.65%) and 7.38% (95% CI 5.47% − 9.55%) based on FR and LLN criteria, respectively (Table 3; Figs. 2 and 3). According to the FR criteria, men had a higher prevalence compared to women (15.47%, 95% CI 12.22% − 19.02% and 8.79%, 95% CI 6.94% − 10.82% among men and women, respectively). According to the LLN criteria, there was no difference in the prevalence of COPD between the two sexes (the prevalence in men and women was 8.67% (95% CI 8.44% − 8.90%) and 8.00% (95% CI 6.42% − 9.73%), respectively) (Table 2). The most common stage of irreversible airflow obstruction was stage II, with a prevalence of 50.46% (95% CI 44.59% − 56.33%) (p < 0.0001), followed by stage I, with a prevalence of 35.21% (95% CI 26.70%- 44.23%) (p < 0.0001). Stages III and IV were the least frequent, with a prevalence of 6.77% (95% CI 4.78% − 9.07%) (p < 0.0001) and 1.047% (95% CI 0.60%-1.60%) respectively (p < 0.0003). Sensitivity analysis showed no change in the overall prevalence of COPD according to the two diagnostic criteria.
Estimated overall prevalence of COPD among individuals over 40 years of age by age category and smoking status
The random-effects meta-analysis indicated a significant increase in the prevalence of COPD as the population aged, independent of the diagnostic criteria employed. By the fixed ratio criteria, the prevalence of COPD increased from 4.37% (95% CI 2.76% − 6.33%) in those aged 40–49 years to 24.03% (95% CI 20.04%-28.26%) in those aged 70 years and older. By LLN criteria, the prevalence was 5.22% (95% CI 2.34%-9.17%) and 14.23% (95% CI 11.96%-16.75%) in those aged 40–49 and 70 years and older, respectively (Table 4).
Smokers had a higher prevalence of COPD than non-smokers. Using the FR criteria, the prevalence of COPD among never smokers, former smokers, and current smokers was 8.15%, 18.38%, and 21.51%, respectively. Using the LLN criteria, the respective prevalence of irreversible airflow obstruction among never smokers, former smokers, and current smokers were 3.77%, 7.55%, and 11.13% (Table 4).
Estimated regional prevalence of COPD among people aged 40 years and above
According to the FR criteria, the highest prevalence was recorded in the American region with a proportion of 22.93%, followed by the South East Asian region with an estimate of 19.48%. This was followed by the Europe, Western Pacific, and Eastern Mediterranean regions with a proportion of 13.09%, 11.17%, and 7.95%, respectively. No studies were found on the prevalence of COPD using the FR criteria in the African region. Using the LLN criteria, the South East Asian region recorded the highest prevalence of 10.17%, followed by the African region with an estimate of 7.7%, the Western Pacific region with a proportion of 7.56%, the European region with a proportion of 7.34%, and the Eastern Mediterranean region with a prevalence of 6.9%. The American region recorded the lowest prevalence (4.82%) (Table 5).
Estimated overall prevalence of COPD among individuals aged 40 years and older during the period 2016–2019 and 2020–2022
The prevalence of COPD increased significantly between the 2016–2019 and 2020–2022 periods. According to the FR criteria, it was 10.43% (95% CI 8.11%-12.99%) in the 2016–2019 period and reached 15.17% (95% CI 11.67%-19.02%) in the 2020–2022 period (P < 0.001). Using the LLN as the diagnostic criteria, there was a significant but small decrease in the prevalence of COPD between the periods 2016–2019 and 2020–2022; it was 7.88% (95% CI 6.60% -9.27%) in the period 2016–2019 and 6.46% (95% CI 2.62%-11.84%) in the period 2020–2022 (P < 0.0001). (Figure 4, and Figure 1 of supplementary material)
Estimated prevalence of COPD among individuals aged 40 years and older during 2016–2019 and 2020–2022. (a) Estimated prevalence of COPD among individuals aged 40 years and older during 2016–2019 and 2020–2022 by FR criteria. (b) Estimated prevalence of COPD between 2016–2019 and 2020–2022 by LLN criteria
Bias of publication
The limited number of studies did not allow to assess the bias of publication in some determinants. Whereas, these biases of publication were studies in some other determinants related to FR criteria (FR overall, age groups, residence, severity stage, sex, smoking status, 2016–2019 period, 2020–2022 period) and related to LIN criteria (LIN overall, sex, WHO region, 2016–2019 period). An asymmetric funnel plot was observed in all determinants, suggesting the existence of bias of publication between the included studies. The results of Egger’s test was confirmed the existence of these biases of publication (Fig. 5).
Discussion
This review presents an estimate of the worldwide prevalence of COPD in people aged 40 years and older during the last 6 years, according to the most frequently used spirometric interpretation criteria, namely FR and LLN. Our study also aims at estimating the prevalence of COPD according to several parameters, such as age categories, smoking status, and severity stage, which will serve as a basis for understanding the burden of COPD and instituting effective prevention strategies.
The estimated overall prevalence of COPD in people aged 40 years and older was 12.64% (95% CI, 10.75-14.65%) and 7.38% (95% CI, 5.47-9.55%) according to the FR and LLN definitions, respectively. This estimate is similar to that reported by Vermaghani et al., who estimated an overall COPD prevalence of 12.16% (95% CI 10.91%-13.4%) according to the FR definition [19]. A previous meta-analysis that had as its main objective to estimate the overall prevalence of COPD in people aged 30 years and older during the period 1990–2010, according to the same diagnostic criteria, reported a prevalence of 11.7% [18], a lower estimate than that reported by our study. Furthermore, in a recently published meta-analysis, the worldwide prevalence of COPD according to the FR definition was 10.3%, which is lower than our results [20]. Even more, we found a prevalence of 15.17% (95% CI, 11.67-19.02%) during the period 2020–2022 according to the FR definition, which is much higher than that estimated by Adeloye et al. [20]. Consequently, the prevalence of COPD, according to FR criteria, is rising steadily, and targeted efforts to control this chronic respiratory condition are deemed necessary. The overall prevalence of COPD according to the LLN criteria is similar to that reported by Adeloye et al., who reported a total COPD prevalence of 7.6% [20]. Furthermore, comparison of COPD prevalence between the 2016–2019 period and the 2020–2022 period showed a slight decrease in COPD prevalence from 7.88 to 6.46% over the two periods, respectively. These data lead to the main conclusion that COPD prevalence estimates differ considerably depending on the diagnostic criteria used.
Estimates of the overall prevalence of COPD by sex indicate a high prevalence of irreversible airflow limitation in men compared to women according to the FR definition (prevalence of COPD was 15.47% in men versus a prevalence of 8.79% in women). This finding is supported by previous evidence showing a high prevalence of COPD among male participants, according to the same diagnostic criteria. For example, Vermaghani et al. estimated a prevalence of 15.70% and 9.93%, respectively, for men and women [19]. Furthermore, Adeloye et al. revealed that 14.3% of men aged 30 years and older suffer from COPD, compared to a prevalence of 7.6% in women [18]. A recent meta-analysis with the main objective of estimating the prevalence of COPD by sex revealed a synthetic prevalence of 8.16% in men and 6.16% in women [71]. The difference in prevalence between the two sexes according to the FR criteria could be explained by the fact that men consume more tobacco than women [72], and have a high risk of occupational exposure [73]. However, tobacco consumption by women in developed countries and the use of biofuels for cooking and heating by women in developing countries could decrease the gap observed in this study [74]. Using LLN as a diagnostic criteria, no difference in terms of COPD prevalence between the two sexes was observed (8.67% in men vs. 8.00% in women). A similar result was found by a previous study, which indicated that the prevalence of COPD according to LLN criteria did not differ between men and women [75].
Our meta-analysis found a high prevalence of COPD in the American region, with a prevalence of 22.93% according to the FR definition. This is similar to the results of many previous meta-analyses of regional COPD prevalence estimates. For example, Adeloye et al. and Vermaghani et al. reported that the American region had the highest prevalence compared to other regions, with prevalences of 15.2% and 14.53% respectively [18, 19]. Furthermore, comparison of regional estimates with those found in our study, indicates that the prevalence of COPD is increasing both globally and regionally. Our results also indicate that the lowest prevalence was recorded in the Eastern Mediterranean region (prevalence of 7.95% according to the FR definition). This differs from previous evidence, which found that the lowest prevalence was recorded in the South East Asian region [18, 19]. Using the LLN definition as the diagnostic criteria, the highest prevalence was recorded in the South East Asian region and the lowest in the Americas. This finding confirms that the spirometric definition used impacts the reported prevalence of COPD. Similarly, the heterogeneity of COPD prevalence between regions could be explained by the difference in associated risk factors, survey methodology, case definition used, as well as the characteristics of the included sample [76,77,78].
The contradictory results obtained in this systematic review and meta-analysis lead to a main conclusion, which stipulates that the spirometric criteria used to make the diagnosis affects the estimated prevalence of COPD and therefore makes comparisons difficult. Consulting the scientific literature, several studies have been carried out to propose which of the two definitions is the best for making an adequate diagnosis of COPD and have drawn sometimes a contradictory conclusions. Van Dijik and colleagues conducted a systematic review of the literature to compare the clinical relevance of the two diagnostic criteria and concluded that the severity criteria of airflow limitation can help in choosing which spirometric criteria to apply. The authors suggested using the FR criteria for the most severe cases and the LLN for the least severe [79]. In another meta-analysis, the authors compared the risk of comorbidities and mortality in patients with different diagnostic criteria and revealed a high risk of mortality in patients meeting both criteria and a risk of exacerbations in patients diagnosed by the FR [80]. In another study, Manino et al. showed that patients meeting LLN criteria were four times more likely to die [81]. Each criteria has its limitations. The FR overestimates COPD in the elderly and underestimates it in the young [76, 82, 83], leading to unnecessary treatment and healthcare expenditure [84]. On the other hand, the use of LLN as a diagnostic criteria can lead to different estimates of COPD depending on the LLN used [85]. Some researchers have also criticized the reference equations used, which do not incorporate all covariates [86]. In addition, Burney and colleagues revealed that defining disease according to reference values measured in a representative sample of the normal population biases the fraction attributable to the population [87]. Determining the best diagnostic criteria is therefore not possible, and the debate surrounding this topic is still open. An international consensus on the appropriate diagnostic criteria is needed to establish an accurate diagnosis and reduce the burden of this chronic disease worldwide.
We found that the most frequent COPD stage was the moderate COPD stage with a prevalence of 50.46%, followed by the mild COPD stage with a prevalence of 35.21%. The severe and very severe COPD stages were the least frequent, with a prevalence of 6.77% and 0.9%, respectively. This result is consistent with the findings of many previous studies. For example, Vermaghani and colleagues reported that the majority of COPD patients are in the moderate stage of the disease [19]. This highlights the need to promote early diagnosis and management of COPD patients in the less severe stages of the disease.
The existing literature indicates that COPD increases significantly with aging, this was confirmed by our meta-analysis. The prevalence of COPD according to the FR definition increased from 4.37 to 24.03% in people in the age group 40–49 years and those aged 70 years and over, respectively, and increased from 5.22 to 14.23% according to the LLN definition among the same age group, respectively. Indeed, age is an important risk factor that increases COPD morbidity and the risk of exacerbations in affected individuals [88, 89]. The model of Fletcher and Peto suggests that the rate of mean expiratory volume in one second (FEV1) decreases with age [90]. This model has subsequently been validated by other studies. For example, a prospective cohort study found that the annual rate of FEV1 decreased in people over 67 years of age than in people of younger age [91]. This could be explained by the fact that with aging, alveolar spaces widen and the lungs lose their elasticity, the risk of oxidative stress increases, and the number of anti-aging molecules decreases [92]. In light of these data, the government and public health policy makers should pay more attention to the elderly in order to detect COPD early and avoid any complications that may endanger the health and/or well-being of the elderly. We found that smoking was associated with a high prevalence of COPD. Indeed, smoking is a well-recognized risk factor for COPD [93, 94]. Tobacco smoke induces the proliferation of immune cells and the appearance of inflammatory mediators responsible for the lesions characteristic of COPD [95, 96]. Data have indicated that a reduction in tobacco consumption leads to a significant reduction in the number of COPD-related deaths. Therefore, tobacco control should be a global health priority for governments.
The present study has a number of limitations. Firstly, heterogeneity between studies was high, which could influence the interpretation of the results. In addition, we did not estimate the overall prevalence of pre- and post-bronchodilator COPD. A high number of the included studies estimated the pre-bronchodilator prevalence. Yet, guidelines recommend bronchodilator administration to establish the diagnosis of permanent flow obstruction and differentiate it from asthma. Therefore, the estimates revealed by the present study may not present the true prevalence of COPD. The distribution of studies across regions was disproportionate. Therefore, the regional prevalence reported in the present study may overestimate the burden of COPD in some regions and underestimate it in others. Furthermore, given the lack of published studies on COPD by FR criteria in Africa, we were unable to estimate the prevalence of COPD in this region. These data illustrate the enormous need for prevalence data in developing countries regions. We limited our search to articles published in English and French, which may miss the inclusion of other publications reporting prevalence data for this chronic respiratory condition in other languages. Similarly, the non-inclusion of COPD-related terms in the search strategy, such as chronic bronchitis or pulmonary emphysema, could miss capturing relevant studies. However, the estimation of the prevalence of COPD globally, regionally, and by several other parameters according to the two most widely used spirometry criteria was among the strengths of this meta-analysis.
Conclusions
COPD is a significant public health problem. In this study, we found that the prevalence of COPD differs considerably depending on the diagnostic criteria used. Alarming data on the prevalence of COPD by several parameters were identified and were consistent with existing evidence. Therefore, the control of COPD must be a major health concern of public authorities in order to reduce the global burden of this chronic respiratory condition. This cannot be achieved in the absence of effective management and prevention strategies targeting the risk factors involved in the development of permanent airway obstruction.
Data availability
All data generated or analysed during this review are included in this published article and its supplementary information files.
Abbreviations
- COPD:
-
Chronic obstructive pulmonary disease
- FR:
-
Fixed ratio
- LLN:
-
Lower limit of normal
- FVC:
-
Forced vital capacity
- FEV 1:
-
Forced expiratory volume in one second
- WHO:
-
World health organazation
- GBD:
-
Global burden of disease
- PRISMA:
-
Preferred reporting items for systematic reviews and meta-Analyses
- STROBE:
-
Strengthening the reporting of observational studies in epidemiology
- EMR:
-
Eastern Mediterranean Region
- EUR:
-
European Region
- AMR:
-
Americas Region
- SEAR:
-
South East Asia Region
- WPR:
-
Western Pacific Region
- AFR:
-
African Region
References
Celli B, Fabbri L, Criner G, Martinez FJ, Mannino D, Vogelmeier C, Montes de Oca M, Papi A, Sin DD, Han MK, Agusti A. Definition and nomenclature of Chronic Obstructive Pulmonary Disease: time for its revision. Am J Respir Crit Care Med. 2022;206(11):1317–25. https://doi.org/10.1164/rccm.202204-0671PP.
Iheanacho I, Zhang S, King D, Rizzo M, Ismaila AS. Economic burden of Chronic Obstructive Pulmonary Disease (COPD): a systematic literature review. Int J Chron Obstruct Pulmon Dis. 2020;15:439–60. https://doi.org/10.2147/COPD.S234942.
The top 10 causes of death– World Health Organization (WHO). Available https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death. Consulted on 09/11/2022.
López-Campos JL, Tan W, Soriano JB. Global burden of COPD. Respirology. 2016;21(1):14–23. https://doi.org/10.1111/resp.12660.
Ferrer M, Alonso J, Morera J, Marrades RM, Khalaf A, Aguar MC, Plaza V, Prieto L, Antó JM. Chronic obstructive pulmonary disease stage and health-related quality of life. The Quality of Life of Chronic Obstructive Pulmonary Disease Study Group. Ann Intern Med. 1997;127(12):1072–9. https://doi.org/10.7326/0003-4819-127-12-199712150-00003.
Indian Institute of Metrology and Health Assessment. 2020. Available: http://www.healthdata.org/india. Consulted on 09/11/2022.
Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3(11):e442. https://doi.org/10.1371/journal.pmed.0030442.
Yau CK, Rahim FF, Sheng CJ, Ling CX, Weng LK, Chia TC, Chye TK, Ting OS, Jin TH, Ali IAH. Assessing airflow limitation among smokers in a primary care setting. Malays J Med Sci. 2018;25(3):78–87. https://doi.org/10.21315/mjms2018.25.3.8.
Gogou E, Kotsiou OS, Siachpazidou DS, Pinaka M, Varsamas C, Bardaka F, Gerogianni I, Hatzoglou C, Gourgoulianis KI. Underestimation of respiratory symptoms by smokers: a thorn in chronic obstructive pulmonary disease diagnosis. NPJ Prim Care Respir Med. 2021;31(1):14. https://doi.org/10.1038/s41533-021-00226-y.
Salvi SS, Barnes PJ. Chronic obstructive pulmonary disease in non-smokers. Lancet. 2009;374(9691):733–43. https://doi.org/10.1016/S0140-6736(09)61303-9.
Oh H, Lee YE. Prevalence and risk factors of Chronic Obstructive Pulmonary Disease among nonsmokers: Fifth Korea National Health and Nutrition Examination Survey (2010–2012). Osong Public Health Res Perspect. 2016;7(6):385–93. https://doi.org/10.1016/j.phrp.2016.11.006.
Vanfleteren LE, Lamprecht B, Studnicka M, Kaiser B, Gnatiuc L, Burney P, Wouters EF, Franssen FM. Body mass index and chronic airflow limitation in a worldwide population-based study. Chron Respir Dis. 2016;13(2):90–101. https://doi.org/10.1177/1479972315626012.
Yu WC, Fu SN, Tai EL, Yeung YC, Kwong KC, Chang Y, Tam CM, Yiu YK. Spirometry is underused in the diagnosis and monitoring of patients with chronic obstructive pulmonary disease (COPD). Int J Chron Obstruct Pulmon Dis. 2013;8:389–95. https://doi.org/10.2147/COPD.S48659.
Wheatley JR. Spirometry: key to the diagnosis of respiratory disorders. Med J Aust. 2017;207(10):422–3. https://doi.org/10.5694/mja17.00684.
Celli BR. The importance of spirometry in COPD and asthma: effect on approach to management. Chest. 2000;117(2 Suppl):15S–9S. https://doi.org/10.1378/chest.117.2_suppl.15s.
Swanney MP, Ruppel G, Enright PL, Pedersen OF, Crapo RO, Miller MR, Jensen RL, Falaschetti E, Schouten JP, Hankinson JL, Stocks J, Quanjer PH. Using the lower limit of normal for the FEV1/FVC ratio reduces the misclassification of airway obstruction. Thorax. 2008;63(12):1046–51. https://doi.org/10.1136/thx.2008.098483.
Heffler E, Crimi C, Mancuso S, Campisi R, Puggioni F, Brussino L, Crimi N. Misdiagnosis of asthma and COPD and underuse of spirometry in primary care unselected patients. Respir Med. 2018;142:48–52. https://doi.org/10.1016/j.rmed.2018.07.015.
Adeloye D, Chua S, Lee C, Basquill C, Papana A, Theodoratou E, Nair H, Gasevic D, Sridhar D, Campbell H, Chan KY, Sheikh A, Rudan I, Global Health Epidemiology Reference Group (GHERG). Global and regional estimates of COPD prevalence: systematic review and meta-analysis. J Glob Health. 2015;5(2):020415. https://doi.org/10.7189/jogh.05.020415.
Varmaghani M, Dehghani M, Heidari E, Sharifi F, Moghaddam SS, Farzadfar F. Global prevalence of chronic obstructive pulmonary disease: systematic review and meta-analysis. East Mediterr Health J. 2019;25(1):47–57. https://doi.org/10.26719/emhj.18.014.
Adeloye D, Song P, Zhu Y, Campbell H, Sheikh A, Rudan I, NIHR RESPIRE Global Respiratory Health Unit. Global, regional, and national prevalence of, and risk factors for, chronic obstructive pulmonary disease (COPD) in 2019: a systematic review and modelling analysis. Lancet Respir Med. 2022;10(5):447–58. https://doi.org/10.1016/S2213-2600(21)00511-7.
Moher D, Liberati A, Tetzlaff J, Altman DG. The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. https://doi.org/10.1371/journal.pmed.1000097.
Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, Poole C, Schlesselman JJ, Egger M, STROBE Initiative. Strengthening the reporting of Observational studies in Epidemiology (STROBE): explanation and elaboration. PLoS Med. 2007;4(10):e297. https://doi.org/10.1371/journal.pmed.0040297.
Sanderson S, Tatt ID, Higgins JP. Tools for assessing quality and susceptibility to bias in observational studies in epidemiology: a systematic review and annotated bibliography. Int J Epidemiol. 2007;36(3):666–76. https://doi.org/10.1093/ije/dym018.
Sutradhar I, Das Gupta R, Hasan M, Wazib A, Sarker M. Prevalence and risk factors of Chronic Obstructive Pulmonary Disease in Bangladesh: a systematic review. Cureus. 2019;11(1):e3970. https://doi.org/10.7759/cureus.3970.
Borenstein M, Higgins JP, Hedges LV, Rothstein HR. Basics of meta-analysis: I2 is not an absolute measure of heterogeneity. Res Synth Methods. 2017;8(1):5–18. https://doi.org/10.1002/jrsm.1230.
Von Hippel PT. The heterogeneity statistic I(2) can be biased in small meta-analyses. BMC Med Res Methodol. 2015;15:35. https://doi.org/10.1186/s12874-015-0024-z.
Borenstein M, Hedges LV, Higgins JPT, et al. Introduction to Meta-Analysis. Hoboken, NJ: John Wiley & Sons; 2009. https://doi.org/10.1002/9780470743386.
Analysing data and. undertaking meta-analyses. https://training.cochrane.org/handbook/current/chapter-10.
Bourbeau J, Doiron D, Biswas S, Smith BM, Benedetti A, Brook JR, Aaron SD, Chapman KR, Hernandez P, Maltais F, Marciniuk DD, O’Donnell D, Sin DD, Walker B, Dsilva L, Nadeau G, Coats V, Compton C, Miller BE, Tan WC, CanCOLD Collaborative Research Group and the Canadian Respiratory Research Network. Ambient air Pollution and Dysanapsis: associations with lung function and chronic obstructive Pulmonary Disease in the Canadian cohort obstructive lung Disease Study. Am J Respir Crit Care Med. 2022;206(1):44–55. https://doi.org/10.1164/rccm.202106-1439OC.
Farooqi MAM, Ma J, Ali MU, et al. Prevalence and burden of COPD misclassification in the Canadian longitudinal study on aging (CLSA). BMJ Open Respir Res. 2022;9(1):e001156. https://doi.org/10.1136/bmjresp-2021-001156.
Grafino M, Todo-Bom F, Lutas AC, Cabral J, Pereira M, Valença J, Furtado ST. Spirometry for the diagnosis of airway obstruction in patients with risk factors for COPD: the GOLD and lower limit of normal criteria. J Bras Pneumol. 2022;47(6):e20210124. https://doi.org/10.36416/1806-3756/e20210124.
Machiguchi H, Arizono S, Tawara Y, Oomagari M, Yanagita Y, Tanaka T, Senjyu H, Kozu R. Sex differences in the International Primary Care Airways Group Questionnaire for Screening of Chronic Obstructive Pulmonary Disease: a Retrospective, cross-sectional study. Int J Chron Obstruct Pulmon Dis. 2022;17:1467–76. https://doi.org/10.2147/COPD.S364088.
Pagano L, McKeough Z, Wootton S, Zwar N, Dennis S. Accuracy of the COPD diagnostic questionnaire as a screening tool in primary care. BMC Prim Care. 2022;23(1):78. https://doi.org/10.1186/s12875-022-01685-z. PMID: 35421929.
Wang D, Fan G, Wu S, Yang T, Xu J, Yang L, Zhao J, Zhang X, Bai C, Kang J, Ran P, Shen H, Wen F, Huang K, Chen Y, Sun T, Shan G, Lin Y, Xu G, Wang R, Shi Z, Xu Y, Ye X, Song Y, Wang Q, Zhou Y, Li W, Ding L, Wan C, Yao W, Guo Y, Xiao F, Lu Y, Peng X, Zhang B, Xiao D, Wang Z, Bu X, Zhang H, Zhang X, An L, Zhang S, Zhu J, Cao Z, Zhan Q, Yang Y, Liang L, Dai H, Cao B, He J, Wang C. China Pulmonary Health (CPH) Study Group. Development and validation of a Screening Questionnaire of COPD from a large epidemiological study in China. COPD. 2022;19(1):118–24. https://doi.org/10.1080/15412555.2022.2042504.
Xiao S, Wu F, Wang Z, Chen J, Yang H, Zheng Y, Deng Z, Peng J, Wen X, Huang P, Dai C, Lu L, Zhao N, Ran P, Zhou Y. Validity of a portable spirometer in the communities of China. BMC Pulm Med. 2022;22(1):80. https://doi.org/10.1186/s12890-022-01872-9.
Kim T, Kang J. Association between dual use of e-cigarette and cigarette and chronic obstructive pulmonary disease: an analysis of a nationwide representative sample from 2013 to 2018. BMC Pulm Med. 2021;21(1):231. https://doi.org/10.1186/s12890-021-01590-8.
Leung C, Bourbeau J, Sin DD, Aaron SD, FitzGerald JM, Maltais F, Marciniuk DD, O’Donnell D, Hernandez P, Chapman KR, Walker B, Road JD, Zheng L, Zou C, Hogg JC, Tan WC, CanCOLD Collaborative Research Group. The prevalence of Chronic Obstructive Pulmonary Disease (COPD) and the heterogeneity of risk factors in the Canadian Population: results from the Canadian obstructive lung disease (COLD) study. Int J Chron Obstruct Pulmon Dis. 2021;16:305–20. https://doi.org/10.2147/COPD.S285338.
Li L, Zhong X, Zheng A, JianKun C, Budukadeer AA, Aini P, Tuerxun M, Yasen M, Ma T, Ren J, Semaiti R, Xie C, Li F, Rexiati M, Tang L, Abudurexiti G, Zheng D, Li JQ. Prevalence and risk factors of Chronic Obstructive Pulmonary Disease in Kashi Region, Northwestern China. Int J Chron Obstruct Pulmon Dis. 2021;16:655–63. https://doi.org/10.2147/COPD.S289620.
Shangguan C, Yu L, Liu G, Song Y, Chen J. Risk assessment of chronic obstructive pulmonary disease using a bayesian network based on a provincial survey. Pol Arch Intern Med. 2021;131(4):345–55. https://doi.org/10.20452/pamw.15867.
Su J, Ye Q, Zhang D, Zhou J, Tao R, Ding Z, Lu G, Liu J, Xu F. Joint association of cigarette smoking and PM2.5 with COPD among urban and rural adults in regional China. BMC Pulm Med. 2021;21(1):87. https://doi.org/10.1186/s12890-021-01465-y.
Tamaki K, Sakihara E, Miyata H, Hirahara N, Kirichek O, Tawara R, Akiyama S, Katsumata M, Haruya M, Ishii T, Simard EP, Miller BE, Tal-Singer R, Kaise T. Utility of self-administered questionnaires for identifying individuals at risk of COPD in Japan: the OCEAN (Okinawa COPD casE finding AssessmeNt) study. Int J Chron Obstruct Pulmon Dis. 2021;16:1771–82. https://doi.org/10.2147/COPD.S302259.
Zhang DD, Liu JN, Ye Q, Chen Z, Wu L, Peng XQ, Lu G, Zhou JY, Tao R, Ding Z, Xu F, Zhou L. Association between socioeconomic status and chronic obstructive pulmonary disease in Jiangsu Province, China: a population-based study. Chin Med J (Engl). 2021;134(13):1552–60. https://doi.org/10.1097/CM9.0000000000001609.
Adhikari TB, Acharya P, Högman M, Neupane D, Karki A, Drews A, Cooper BG, Sigsgaard T, Kallestrup P. Prevalence of Chronic Obstructive Pulmonary Disease and its Associated factors in Nepal: findings from a community-based Household Survey. Int J Chron Obstruct Pulmon Dis. 2020;15:2319–31. https://doi.org/10.2147/COPD.S268110.
Kim CY, Kim BK, Kim YJ, Lee SH, Kim YS, Kim JH. Longitudinal evaluation of the Relationship between Low Socioeconomic Status and Incidence of Chronic Obstructive Pulmonary Disease: Korean Genome and Epidemiology Study (KoGES). Int J Chron Obstruct Pulmon Dis. 2021;15:3447–54. https://doi.org/10.2147/COPD.S276639.
Melbye H, Stylidis M, Solis JCA, Averina M, Schirmer H. Prediction of chronic heart failure and chronic obstructive pulmonary disease in a general population: the Tromsø study. ESC Heart Fail. 2020;7(6):4139–50. https://doi.org/10.1002/ehf2.13035.
Sharifi H, Ghanei M, Jamaati H, Masjedi MR, Aarabi M, Sharifpour A, Radmand G, Najafimehr H, Buist AS. Burden of obstructive lung disease in Iran: prevalence and risk factors for COPD in North of Iran. Int J Prev Med. 2020;11:78. https://doi.org/10.4103/ijpvm.IJPVM_478_18.
Sumit AF, Das A, Miraj IH, Bhowmick D. Association between chronic obstructive pulmonary disease (COPD) and occupational exposures: a hospital based quantitative cross-sectional study among the Bangladeshi population. PLoS ONE. 2020;15(9):e0239602. https://doi.org/10.1371/journal.pone.0239602.
Timur A, Balci E, Durmus H. Prevalence of Chronic Obstructive Pulmonary Disease in individuals over 40 in Central Kayseri. Erciyes Med J. 2020;42(3):322–8.
Yan X, Xu L, Shi B, Wang H, Xu X, Xu G. Epidemiology and risk factors of chronic obstructive pulmonary disease in Suzhou: a population-based cross-sectional study. J Thorac Dis. 2020;12(10):5347–56. https://doi.org/10.21037/jtd-20-1616.
Bikbov MM, Kazakbaeva GM, Zainullin RM, Salavatova VF, Arslangareeva II, Panda-Jonas S, Gilmanshin TR, Nikitin NA, Mukhamadieva SR, Yakupova DF, Khikmatullin RI, Aminev SK, Nuriev IF, Zaynetdinov AF, Uzianbaeva YV, Jonas JB. Prevalence, awareness, and Associated factors of airflow obstruction in Russia: the Ural Eye and Medical Study. Front Public Health. 2019;7:350. https://doi.org/10.3389/fpubh.2019.00350.
De Matteis S, Jarvis D, Darnton A, Hutchings S, Sadhra S, Fishwick D, Rushton L, Cullinan P. The occupations at increased risk of COPD: analysis of lifetime job-histories in the population-based UK Biobank Cohort. Eur Respir J. 2019;54(1):1900186. https://doi.org/10.1183/13993003.00186-2019.
Sheng W, Huang Y, Deng Z, Ma H. Investigation of the prevalence and diagnosis of Chronic Obstructive Pulmonary Disease in a Group of Elderly individuals residing in an Island Area of Ningbo. Can Respir J. 2019;2019:6918340. https://doi.org/10.1155/2019/6918340.
Zha Z, Leng R, Xu W, Bao H, Chen Y, Fang L, Liu Z, Ye D. Prevalence and risk factors of chronic obstructive pulmonary disease in Anhui Province, China: a population-based survey. BMC Pulm Med. 2019;19(1):102. https://doi.org/10.1186/s12890-019-0864-0.
Broström E, Jõgi R, Gislason T, Benediktsdottir B, Burney PGJ, Janson C. The prevalence of chronic airflow obstruction in three cities in the nordic-baltic region. Respir Med. 2018;143:8–13. https://doi.org/10.1016/j.rmed.2018.08.007.
Ding Y, Yang D, He P, Yao J, Sun P, Li Q, Xie P, Lin D, Sun D, Niu H, Tian Z. Prevalence and risk factors of chronic obstructive pulmonary diseases in a Hlai community in Hainan Island of China. Clin Respir J. 2018;12(1):126–33. https://doi.org/10.1111/crj.12497.
Fang L, Gao P, Bao H, Tang X, Wang B, Feng Y, Cong S, Juan J, Fan J, Lu K, Wang N, Hu Y, Wang L. Chronic obstructive pulmonary disease in China: a nationwide prevalence study. Lancet Respir Med. 2018;6(6):421–30. https://doi.org/10.1016/S2213-2600(18)30103-6.
Leem AY, Park B, Kim YS, Jung JY, Won S. Incidence and risk of chronic obstructive pulmonary disease in a Korean community-based cohort. Int J Chron Obstruct Pulmon Dis. 2018;13:509–17. https://doi.org/10.2147/COPD.S148618.
Kotaki K, Ikeda H, Fukuda T, Yuki F, Hasuo K, Kawano Y, Kawasaki M. Effectiveness of diagnostic screening tests in mass screening for COPD using a cooperative regional system in a region with heavy air pollution: a cross-sectional study. BMJ Open. 2017;7(1):e012923. https://doi.org/10.1136/bmjopen-2016-012923.
Nakao M, Yamauchi K, Ishihara Y, Omori H, Solongo B, Ichinnorov D. Prevalence and risk factors of airflow limitation in a Mongolian population in Ulaanbaatar: cross-sectional studies. PLoS ONE. 2017;12(4):e0175557. https://doi.org/10.1371/journal.pone.0175557.
Sobrino E, Irazola VE, Gutierrez L, Chen CS, Lanas F, Calandrelli M, Ponzo J, Mores N, Serón P, Lee A, He J, Rubinstein AL. Estimating prevalence of chronic obstructive pulmonary disease in the Southern Cone of Latin America: how different spirometric criteria may affect disease burden and health policies. BMC Pulm Med. 2017;17(1):187. https://doi.org/10.1186/s12890-017-0537-9.
Torén K, Murgia N, Olin AC, Hedner J, Brandberg J, Rosengren A, Bergström G. Validity of physician-diagnosed COPD in relation to spirometric definitions of COPD in a general population aged 50–64 years - the SCAPIS pilot study. Int J Chron Obstruct Pulmon Dis. 2017;12:2269–75. https://doi.org/10.2147/COPD.S136308.
Denguezli M, Daldoul H, Harrabi I, Gnatiuc L, Coton S, Burney P, Tabka Z. COPD in nonsmokers: reports from the Tunisian Population-based Burden of Obstructive Lung Disease Study. PLoS ONE. 2016;11(3):e0151981. https://doi.org/10.1371/journal.pone.0151981.
El Rhazi K, Nejjari C, Ben Jelloun MC, El Biaze M, Attassi M, Garcia-Larsen V. Prevalence of chronic obstructive pulmonary disease in Fez, Morocco: results from the BOLD study. Int J Tuberculosis Lung Disease. 2016;20(1):136–41.
Fukuyama S, Matsumoto K, Kaneko Y, Kan-o K, Noda N, Tajiri-Asai Y, Nakano T, Ishii Y, Kiyohara Y, Nakanishi Y, Inoue H, Hisayama Pulmonary Physiology Study Group. Prevalence of Airflow Limitation defined by pre- and Post-bronchodilator Spirometry in a community-based Health Checkup: the Hisayama Study. Tohoku J Exp Med. 2016;238(2):179–84. https://doi.org/10.1620/tjem.238.179.
Karrasch S, Brüske I, Smith MP, Thorand B, Huth C, Ladwig KH, Kronenberg F, Heinrich J, Holle R, Peters A, Schulz H. What is the impact of different spirometric criteria on the prevalence of spirometrically defined COPD and its comorbidities? Results from the population-based KORA study. Int J Chron Obstruct Pulmon Dis. 2016;11:1881–94. https://doi.org/10.2147/COPD.S104529.
Koul PA, Hakim NA, Malik SA, Khan UH, Patel J, Gnatiuc L, Burney PG. Prevalence of chronic airflow limitation in Kashmir, North India: results from the BOLD study. Int J Tuberc Lung Dis. 2016;20(10):1399–404. https://doi.org/10.5588/ijtld.15.0968.
Loh LC, Rashid A, Sholehah S, Gnatiuc L, Patel JH, Burney P. Low prevalence of obstructive lung disease in a suburban population of Malaysia: a BOLD collaborative study. Respirology. 2016;21(6):1055–61. https://doi.org/10.1111/resp.12793.
Obaseki DO, Erhabor GE, Gnatiuc L, Adewole OO, Buist SA, Burney PG. Chronic airflow obstruction in a black African Population: results of BOLD Study, Ile-Ife, Nigeria. COPD. 2016;13(1):42–9. https://doi.org/10.3109/15412555.2015.1041102.
Omori H, Kaise T, Suzuki T, Hagan G. Prevalence of airflow limitation in subjects undergoing comprehensive health examination in Japan: survey of chronic obstructive pulmonary disease patients epidemiology in Japan. Int J Chron Obstruct Pulmon Dis. 2016;11:873–80. https://doi.org/10.2147/COPD.S99935.
Park HJ, Byun MK, Kim HJ, Kim JY, Kim YI, Yoo KH, Chun EM, Jung JY, Lee SH, Ahn CM. Dietary vitamin C intake protects against COPD: the Korea National Health and Nutrition Examination Survey in 2012. Int J Chron Obstruct Pulmon Dis. 2016;11:2721–8. https://doi.org/10.2147/COPD.S119448.
Burney P, Jarvis D, Perez-Padilla R. The global burden of chronic respiratory disease in adults. Int J Tuberc Lung Dis. 2015;19(1):10–20. https://doi.org/10.5588/ijtld.14.0446.
GBD 2015 Chronic Respiratory Disease Collaborators. Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990–2015: a systematic analysis for the global burden of Disease Study 2015. Lancet Respir Med. 2017;5(9):691–706. https://doi.org/10.1016/S2213-2600(17)30293-X.
Ntritsos G, Franek J, Belbasis L, Christou MA, Markozannes G, Altman P, Fogel R, Sayre T, Ntzani EE, Evangelou E. Gender-specific estimates of COPD prevalence: a systematic review and meta-analysis. Int J Chron Obstruct Pulmon Dis. 2018;13:1507–14. https://doi.org/10.2147/COPD.S146390.
Ng M, Freeman MK, Fleming TD, Robinson M, Dwyer-Lindgren L, Thomson B, Wollum A, Sanman E, Wulf S, Lopez AD, Murray CJ, Gakidou E. Smoking prevalence and cigarette consumption in 187 countries, 1980–2012. JAMA. 2014;311(2):183–92. https://doi.org/10.1001/jama.2013.284692.
Lamprecht B, Soriano JB, Studnicka M, Kaiser B, Vanfleteren LE, Gnatiuc L, Burney P, Miravitlles M, García-Rio F, Akbari K, Ancochea J, Menezes AM, Perez-Padilla R, de Montes M, Torres-Duque CA, Caballero A, González-García M, Buist S, BOLD Collaborative Research. Group, the EPI-SCAN Team, the PLATINO Team, and the PREPOCOL Study Group. Determinants of underdiagnosis of COPD in national and international surveys. Chest. 2015;148(4):971–85. https://doi.org/10.1378/chest.14-2535.
Celli BR, Halbert RJ, Isonaka S, Schau B. Population impact of different definitions of airway obstruction. Eur Respir J. 2003;22(2):268–73. https://doi.org/10.1183/09031936.03.00075102
Meteran H, Miller MR, Thomsen SF, Christensen K, Sigsgaard T, Backer V. The impact of different spirometric definitions on the prevalence of airway obstruction and their association with respiratory symptoms. ERJ Open Res. 2017;3(4):00110–2017. https://doi.org/10.1183/23120541.00110-2017.
Buist AS, McBurnie MA, Vollmer WM, Gillespie S, Burney P, Mannino DM. International variation in the prevalence of COPD (the BOLD Study) a population-based prevalence study [published correction appears in. Lancet. 2012;380(9844):806–6. https://doi.org/10.1016/S0140-6736(07)61377
van Dijk WD, Gupta N, Tan WC, Bourbeau J. Clinical relevance of diagnosing COPD by fixed ratio or lower limit of normal: a systematic review. COPD. 2014;11(1):113-20. https://doi.org/10.3109/15412555.2013.781996
Xiong H, Huang Q, Shuai T, Zhu L, Zhang C, Zhang M, Wang Y, Liu J. Assessment of comorbidities and prognosis in patients with COPD diagnosed with the fixed ratio and the lower limit of normal: a systematic review and meta-analysis. Respir Res. 2020;21(1):189 https://doi.org/10.1186/s12931-020-01450-9
Mannino DM, Sonia Buist A, Vollmer WM. Chronic obstructive pulmonary disease in the older adult: what defines abnormal lung function? Thorax. 2007;62(3):237-41 https://doi.org/10.1136/thx.2006.068379
Bárbara C, Rodrigues F, Dias H, Cardoso J, Almeida J, Matos MJ, Simão P, Santos M, Ferreira JR, Gaspar M, Gnatiuc L, Burney P. Chronic obstructive pulmonary disease prevalence in Lisbon, Portugal: the burden of obstructive lung disease study. Rev Port Pneumol. 2013;19(3):96–105. https://doi.org/10.1016/j.rppneu.2012.11.004.
Vollmer WM, Gíslason T, Burney P, Enright PL, Gulsvik A, Kocabas A. Comparison of spirometry criteria for the diagnosis of COPD results from the BOLD study. Eur Respir J. 2009;34(3):588–97. https://doi.org/10.1183/09031936.00164608.
Swanney MP, Ruppel G, Enright PL, Pedersen OF, Crapo RO, Miller MR, Jensen RL, Falaschetti E, Schouten JP, Hankinson JL, Stocks J, Quanjer PH. Using the lower limit of normal for the FEV1/FVC ratio reduces the misclassification of airway obstruction. Thorax. 2008;63(12):1046-51 https://doi.org/10.1136/thx.2008.098483
Çolak Y, Nordestgaard BG, Vestbo J, Lange P, Afzal S. Comparison of five major airflow limitation criteria to identify high-risk individuals with COPD: a contemporary population-based cohort. Thorax. 2020;75(11):944-54. https://doi.org/10.1136/thoraxjnl
Marks GB. Are reference equations for spirometry an appropriate criterion for diagnosing disease and predicting prognosis? https://doi.org/10.1136/thoraxjnl-2011-200584
Burney P, Minelli C. Using reference values to define disease based on the lower limit of normal biased the population attributable fraction, but not the population excess risk: the example of chronic airflow obstruction. J Clin Epidemiol. 2018;93:76–78. https://doi.org/10.1016/j.jclinepi.2017.10.020
Li CL, Lin MH, Tsai YC, Tseng CW, Chang CL, Shen LS, Kuo HC, Liu SF. The Impact of the Age, Dyspnoea, and Airflow Obstruction (ADO) Index on the Medical Burden of Chronic Obstructive Pulmonary Disease (COPD). J Clin Med. 2022;11(7):1893. https://doi.org/10.3390/jcm11071893
Galani M, Kyriakoudi A, Filiou E, et al. Older age, disease severity and co-morbidities independently predict mortality in critically ill patients with COPD exacerbation. Pneumon. 2021;34(2):9 https://doi.org/10.18332/pne/139637
Fletcher C, Peto R. The natural history of chronic airflow obstruction. Br Med J. 1977 Jun 25;1(6077):1645–8. https://doi.org/10.1136/bmj.1.6077.1645
Kim SJ, Lee J, Park YS, Lee CH, Yoon HI, Lee SM, Yim JJ, Kim YW, Han SK, Yoo CG. Age-related annual decline of lung function in patients with COPD. Int J Chron Obstruct Pulmon Dis. 2015;11:51–60. https://doi.org/10.2147/COPD.S95028.
Orrelles JB, Restrepo BI, Bai Y, Ross C, Schlesinger LS, Turner J. The Impact of Aging on the Lung Alveolar Environment, Predetermining Susceptibility to Respiratory Infections. Front Aging. 2022;3:818700. https://doi.org/10.3389/fragi.2022.818700
Wheaton AG, Liu Y, Croft JB, VanFrank B, Croxton TL, Punturieri A, Postow L, Greenlund KJ. Chronic Obstructive Pulmonary Disease and Smoking Status - United States, 2017. MMWR Morb Mortal Wkly Rep. 2019;68(24):533–538. https://doi.org/10.15585/mmwr.mm6824a1
Llordés M, Jaén A, Almagro P, Heredia JL, Morera J, Soriano JB, Miravitlles M. Prevalence, Risk Factors and Diagnostic Accuracy of COPD Among Smokers in Primary Care. COPD. 2015;12(4):404–12. https://doi.org/10.3109/15412555.2014.974736
Leap J, Arshad O, Cheema T, Balaan M. Pathophysiology of COPD. Crit Care Nurs Q. 2021;44(1):2–8. https://doi.org/10.1097/CNQ.0000000000000334.
Godtfredsen NS, Lam TH, Hansel TT, Leon ME, Gray N, Dresler C, Burns DM, Prescott E, Vestbo J. COPD-related morbidity and mortality after smoking cessation: status of the evidence. Eur Respir J. 2008;32(4):844–53. https://doi.org/10.1183/09031936.00160007.
Acknowledgements
Not applicable.
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
Al wachami Nadia: conceptualization,methodology, investigation, supervision, writing of the original draft, and revision; Guennouni Morad: Statistical analysis and writing of the original draft; Iderdar Younes: conceptualisation, investigation; Boumendil Karima: Conceptualization; Mourajid Yassmine: Conceptualization, Arraji Maryem: Conceptualization; Bouchachi Fatima-zahra: Investigation; Barkaoui Mohamed: revision; Mohamed Elhabib Louerdi: conceptualization and revision; Hilali Abderraouf: revision; Chahboune Mohamed: conceptualization, methodology and revision. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
AL Wachami, N., Guennouni, M., Iderdar, Y. et al. Estimating the global prevalence of chronic obstructive pulmonary disease (COPD): a systematic review and meta-analysis. BMC Public Health 24, 297 (2024). https://doi.org/10.1186/s12889-024-17686-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-17686-9