Abstract
Background
Chronic Obstructive Pulmonary Disease (COPD) remains one of the leading causes of morbidity and mortality worldwide, and its epidemiology in Latin America and the Caribbean is not well described. The aim of this study was to evaluate the prevalence and incidence of COPD in Latin America and the Caribbean.
Methods
We searched systematically in Web of Science (WoS)/Core Collection, WoS/MEDLINE, WoS/Scielo, Scopus, PubMed, and Embase from 2010 to 2021. Studies assessing the prevalence and incidence of COPD according to the GOLD classification were included. The overall prevalence of COPD was calculated as a function of the general population using a random-effects model.
Results
20 studies (19 cross-sectional and 1 cohort) met the inclusion criteria. The prevalence of COPD in the general population older than 35 years was 8.9%. The prevalence in men was 13.7% and in women 6.7%. The prevalence in smokers and ex-smokers was 24.3%. The incidence in the general population of COPD according to one study was 3.4% at 9 years of follow-up.
Conclusions
COPD is prevalent in Latin America, especially in men and in smokers and ex-smokers. Further prevalence and incidence studies in the general population are needed, as well as health policies and strategies to address the disease.
Similar content being viewed by others
Background
Chronic obstructive pulmonary disease (COPD) is a pathology with high morbidity and mortality. [1]. Approximately 300 million people have COPD globally [2], with a prevalence of approximately 12.2% [3]. This disease represents the fifth leading cause of death worldwide and it is estimated that by 2030 it will be the fourth [1]. 80% of COPD deaths occur in low- and middle-income countries [4]. Tobacco is the main cause, contributing to other co-morbidities and fatal outcomes [1]. In addition, the disease represents a high economic burden, with costs of approximately $ 5600 per patient per year [5], which increase according to the severity of the disease [6].
The diagnosis of COPD can be made based on various criteria such as symptomatology, biomarkers, ancillary questionnaires, and spirometry [7, 8]. However, the current benchmark is spirometry with an FEV1/FVC value of less than 0.7 post-bronchodilation, a criterion proposed in 2001 by the Global Initiative for Chronic Obstructive Lung Disease (GOLD) [9]. Risk factors for developing COPD include mainly passive and/or active smoking, as well as residence in highly polluted areas, exposure to biomasses, and handling of inhalation chemicals [10]. COPD has also been associated with complications such as cardiovascular disease, lung cancer, pneumonia, and even increased mortality due to SARS-CoV-2 [11, 12]. COPD patients are subjected to increased physical and psychological burden due to decreased life expectancy and performance, and associated comorbidities and respiratory symptoms (dyspnoea and exacerbations) [13, 14].
In many places or latitudes, the prevalence and/or incidence of COPD is changing. This is due to multiple factors such as increased cigarette smoking, exposure to tobacco smoke, variations in indoor and outdoor air pollution. On the other hand, screening and health service delivery programs have been established in different regions [4, 15]. In Latin America and the Caribbean, not much is known about the epidemiology of this disease. Systematic reviews have been conducted on the prevalence and incidence of COPD worldwide and in different populations; however, their results cannot be extrapolated to Latin America and the Caribbean because the included studies from this region are few or non-existent [3], or are not uniform in the diagnostic criteria for COPD [16]. A previous systematic review has also been conducted in Latin America and the Caribbean [17]. However, we believe that an update is needed, given the fact that 10 years have passed. Therefore, this systematic review aimed to identify the prevalence and incidence of COPD in the Latin American and Caribbean populations.
Methods
We performed a systematic review following the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines 2020 [18]. The study protocol has been registered at PROSPERO, number CRD42021233807.
Eligibility criteria
We included cross-sectional observational and cohort studies reporting prevalence or incidence of COPD in different settings (general population, primary care centers, or hospitals) conducted in Latin America and the Caribbean since 2010. Following the protocol, we considered studies that assessed COPD with the classification of airflow limitation severity (GOLD: post-bronchodilator FEV1/FVC ratio < 0.70) [9]. Studies with fewer than 30 patients, manuscripts not available in full text, and duplicate populations were excluded. In the case of duplicate populations, the most complete study was included.
Literature search and study selection
A systematic search was conducted in six databases: Web of Science (WoS)/Core Collection, WoS/MEDLINE, WoS/Scielo, Scopus, PubMed, and Embase between January 1, 2010, and 23 March 2021. No language restrictions were applied. The full search for each database is available in Additional file 1: Material S1. We also reviewed the reference list of all included studies and previous systematic reviews for additional eligible studies.
The identified references were exported to Rayyan software where duplicates were manually removed. Subsequently, the authors (ABB, JJOR, PPL) screened the articles by titles and abstracts to identify potentially relevant articles for inclusion. Selected studies were then reviewed at the full text (ABB, JJOR). These processes were conducted independently and discrepancies were resolved in meetings with all authors to decide whether the study was included.
Data extraction
Two authors (ABB, JJOR) independently extracted the following data of interest using a Microsoft Excel sheet: author, year of publication, study design, country, setting, smoking status, sample size, age, sex, disease prevalence/incidence. Discrepancies were resolved in a meeting.
Risk of bias
Three authors (ABB, JJOR, PPL) independently assessed the methodological quality of prevalence and incidence studies using the Joanna Briggs Institute Critical Appraisal Tool [19]. Another author (DRSM) resolved discrepancies at this stage. This scale has 9 items with possible responses of "Yes", "No" and "Unclear". The quality score presented in Table 1 was found by considering "Yes" as one point and "No" and "Unclear" as zero points, i.e. the higher the score the lower the risk of bias.
Statistical analyses
We performed the analyses with STATA V16.0 software. We calculated pooled COPD prevalence in the general population, using a random-effects model, with their 95% confidence intervals using the exact method. We used the Freeman-Tukey Double Arcsine transformation to stabilize variances. The criteria for including studies in the main meta-analysis were: studies conducted in patients in the community and including smokers, ex-smokers, and non-smokers. To assess heterogeneity and its sources, we used the I2 test and performed subgroup analyses according to sex, country, and risk of bias. We also performed a sensitivity analysis to assess the variation in prevalence when excluding each article from the meta-analysis. Publication bias was assessed with Egger's statistic considering a p < 0.05 as statistically significant. On the other hand, we assessed prevalences according to smoking status (non-smokers, ex-smokers, and smokers) and according to study setting (community, primary care center, and hospital).
Results
Selection of studies
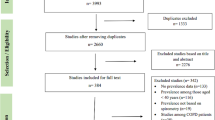
The systematic search identified 5874 studies, with 2839 studies remaining after the removal of duplicates. Studies were screened by title and abstract, and 172 were selected for full-text review. In the full-text review, 151 studies were excluded because they did not meet the eligibility criteria, leaving 20 studies, which were included in the full-text review [20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39] were included in the review (Fig. 1). The excluded full-text studies and reasons for exclusion are shown in Additional file 1: Material S2.
Characteristics of the studies included
Of the 20 studies that met the eligibility criteria, 19 were cross-sectional studies (Table 1) and only one was longitudinal (cohort study). Of the cross-sectional studies, the number of participants was 33 637 and ranged from 66 to 5314. All studies included participants older than 35 years. The mean age ranged from 49.8 to 65.3. The countries in which the studies were conducted were Brazil [20, 23, 27, 29, 33, 37,38,39], Mexico [24, 28,29,30, 34], Argentina [25, 26, 31, 32] Uruguay [25, 26, 29, 32], Chile [26, 29, 32], Colombia [21, 25, 35], Peru [22], and Trinidad and Tobago [36]. Thirteen studies were conducted in the general population [21, 22, 24, 26, 28,29,30,31,32,33, 36, 37, 39] four in hospitals [20, 34, 35, 38] and three in primary care centers [23, 25, 27]. Concerning the type of population, both Moreira et al. and Ramirez-Venegas et al. were studies conducted only in the female population [20, 30]; Romero-Lopez et al. conducted the study in people with HIV [34]. Three studies were conducted in an older adult population [20, 27, 35]. Bastidas et al. evaluated patients scheduled for spirometry [35]. Regarding smoking status, most studies included smokers, ex-smokers, and non-smokers. Seven studies had a high population prevalence of smokers or ex-smokers [23, 24, 27,28,29, 33, 38]. Moreira et al. included non-smoking women exposed to wood smoke [20]. The study by Orduz et al. was conducted on non-smokers. [21].
Regarding the cohort study, it was conducted in the general population in Brazil with a follow-up of 9 years [39]. The number of participants was 594, all of whom were aged 40 years or older. The study included non-smokers, former smokers, and current smokers (Additional file 1: Material S3).
Prevalence of COPD in Latin America and the Caribbean
Of the 19 cross-sectional studies, 8 (n = 23,449) met the criteria to be included in the main meta-analysis [22, 26, 29,30,31,32, 36, 37]. The prevalence of COPD in the general population was 8.9% (95% CI: 66–116; I22: 97.9%) with a range of 2.5 to 14.5% (Fig. 2). In the included studies, all participants were older than 35 years with a mean age between 39.6 and 58.8. Most of the included studies were in both sexes, with some predominance of the male population (approximately 60% male and 40% female).
Sub-group analysis
In addition, COPD prevalence was assessed according to sex, country, and risk of bias. With respect to sex, COPD prevalence was higher in men (13.7%; 95% CI: 9.7–18.3; IQ2: 96.4%) than in women (6.7%; 95% CI: 4.0–10.0; IQ2: 97.4%) (Additional file 1: Material S4). Regarding country, the highest prevalence was in Argentina (11.7%; 95% CI: 8.9–14.7), while the lowest was in Mexico (2.5%; 95% CI: 1.6–3.7) (Fig. 3 and Additional file 1: Material S5). In terms of risk of bias, the studies with the highest methodological quality gave a prevalence of 8.3% (95% CI: 6.4–10.3; I2: 90.5%) (Additional file 1: Material S6).
In addition, studies were found that evaluated patients who were smokers and ex-smokers and in other settings. Concerning smoking status, the prevalence of COPD was higher in smokers and ex-smokers (24.3%; 95% CI: 16. 5–33.1; I2: 98.4%), ranging from 11.1 to 59.2% (Additional file 1: Material S7). Additionally, we found that prevalences in studies conducted in primary care centers (21.9%; 95% CI: 15.6–29.0) and in hospitals (27.3%; 95% CI: 10.2–48.8; I2: 98.3%) were higher than in the general population (Additional file 1: Material S8).
Publication bias
Using Egger's test, no publication bias (p = 0.196) was found in the meta-analysis.
Incidence of COPD in Latin America and the Caribbean
On the other hand, a cohort study found a cumulative incidence of COPD of 3.4% at 9 years follow-up. Of these cases, 40% were non-smokers, 35% smokers, and 25% ex-smokers [39] (Additional file 1: Material S3).
Risk of bias
When assessing the risk of bias, more than 90% of the studies met the items of adequate sample size, subjects, and setting described in detail, use of validated methods for the identification of COPD, and reliably measured condition in all participants. On the other hand, a large proportion did not meet the items of the appropriate sampling frame, sampling, and statistical analysis. The overall assessment score is given in Table 1 and detailed in the Additional file 1: Material S9.
Discussion
In this systematic review we found that the prevalence of COPD in Latin American patients was 8.9% (95% CI: 6.5–11.6; I2: 97.9%), while the cumulative incidence, obtained from 1 study, was 3.4% at 9 years.
In this systematic review, we aimed to estimate the prevalence of COPD in Latin America and the Caribbean [9]. We found that the prevalence of COPD according to GOLD criteria in the general population of the eight meta-analyzed studies (8.9%; 95% CI: 6.5–11.6; I2: 97.9%), was similar to that reported in a global systematic review (12.2%; 95% CI: 10.9–13.4; I2: 29.8%) [3] and to a Latin American and Caribbean systematic review whose search date was 2012 (13.4%; 95% CI: 10.1–17.1; I2: 94.9%) [17]. This similarity may be because the previous reviews were conducted in the general population and used the GOLD criteria. These figures show that the prevalence of COPD is maintained even though smoking has decreased in recent years [40], possibly due to other risk factors such as exposure to environmental pollution, biomasses, etc. [41].
On the other hand, when we evaluated prevalence by country, we found considerable variability. This can be explained by differences in biomass exposure, smoking levels, industrialization, genetic factors (e.g. alpha-1 antitrypsin deficiency) and the burden of other predisposing factors such as tuberculosis or asthma [22, 42, 43]. Compared to the present study, the systematic review by Ciapponi et al. (search date: 2012) reported higher prevalences in the countries of Mexico (7.8%), Brazil (15.2 to 15.8%), Chile (16.9%), and Uruguay (19.7%). Considering that the populations are from the same region, these differences may be attributed to the decline in tobacco use in these countries in recent years [44]. Public health strategies could have helped to reduce tobacco use [45].
Regarding sex, we found that the prevalence in men was twice that of women (7% more), although there is overlap in the confidence intervals. Similarly, the global systematic review of Varmaghani et al. [3] and the Latin American and Caribbean review by Ciapponi et al. [17] found a difference of 5% and 7.8% in favor of men, respectively. This indicates that, despite geographical and cultural differences, both in LATAM and globally, the prevalence of COPD is higher in men than in women. This finding is in agreement with previous literature [46] and could be explained by higher smoking habits in men than in women. [47].
In addition, we observed that the prevalence of COPD among non-smokers was lower among current or former smokers, which is explained by the fact that smoking is the main risk factor for COPD [48]. COPD in non-smoking patients could be due to indoor and outdoor pollution, occupational exposures (agriculture, dust…), treated pulmonary tuberculosis, chronic asthma, low socioeconomic status, and poor nutrition [49].
We also found that the prevalences of studies conducted in primary care centers and hospitals were higher compared to those studies conducted in the community. This is possibly because primary care centers and hospitals care for symptomatic individuals and individuals with risk factors for the disease [50].
In order to reduce the prevalence of COPD in this region, we suggest the following: to create or improve policies and legislation regarding tobacco and its derivates; to create or improve screening programs across the health systems; and to implement or strengthen the general knowledge of non-transmittable diseases, like COPD, at schools with educational programs [51].
Limitations of the studies
The statistical heterogeneity between studies was high and did not decrease in the subgroup analyses, possibly because the confidence intervals of the included studies are narrow and do not overlap with each other. Regarding the risk of bias, studies included in the general population meta-analysis were at low risk. We recommend that future studies be more detailed in describing the population, and present COPD prevalence by smoking status, age and sex. We also recommend that they use the GOLD criteria and report that they are using them [9], as more than 70 studies were excluded for that reason in the selection process. In addition, further well-designed studies that include people over 40 years of age and that assess the incidence and prevalence in other countries are needed to understand the epidemiological behavior of COPD in the region.
Limitations and strengths
Our systematic review has some limitations. First, we did not search the grey literature, so we believe that there may be studies in non-indexed journals or repositories that were not included in this review. In that sense, we did not find the information available for more than half of the countries in the region, so the external validity of our results should be interpreted with caution. The statistical heterogeneity of the studies included in the quantitative synthesis was high.
On the other hand, our review has several strengths. We conducted a comprehensive systematic search of global as well as regional databases and reviewed citations of included studies. We covered a period for which COPD prevalence had not been reported in previous reviews. The same diagnostic criteria for COPD were taken into consideration to reduce clinical heterogeneity among the included studies. Finally, the overall and subgroup analysis was performed taking into consideration the corresponding clinical context as well as the methodological quality of the included studies.
Conclusion
The prevalence of COPD in the general population in Latin America and the Caribbean was 8.9%. Prevalence was higher in men, in patients who were smokers and/or ex-smokers, and in studies conducted in hospitals and primary care centers. Only one study reported that the cumulative incidence of COPD at 9 years of follow-up was 3.4%. More incidence and prevalence studies in the general population of other countries are needed. We also suggest that health strategies and policies for early detection and prevention of COPD should be considered, especially in populations with the highest prevalence.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its Additional file 1.
Abbreviations
- COPD:
-
Chronic obstructive pulmonary disease
- GOLD:
-
Global initiative for chronic obstructive lung disease
- PRISMA:
-
Preferred reporting items for systematic reviews and meta-analysis
References
Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLOS Med. 2006;3:e442.
Ruvuna L, Sood A. Epidemiology of chronic obstructive pulmonary disease. Clin Chest Med. 2020;41:315–27.
Varmaghani M, Dehghani M, Heidari E, Sharifi F, Moghaddam SS, Farzadfar F. Global prevalence of chronic obstructive pulmonary disease: systematic review and meta-analysis. East Mediterr Health J. 2019;25:47–57.
World Health Organization. Chronic obstructive pulmonary disease (COPD) [Internet]. 2021 [cited 2021 Aug 10]. Available from: https://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(copd).
Halpern MT, Stanford RH, Borker R. The burden of COPD in the U.S.A.: results from the confronting COPD survey. Respir Med. 2003;97(Suppl C):81–9.
Iheanacho I, Zhang S, King D, Rizzo M, Ismaila AS. Economic burden of chronic obstructive pulmonary disease (COPD): a systematic literature review. Int J Chron Obstruct Pulmon Dis. 2020;15:439–60.
Rosenberg SR, Kalhan R. Biomarkers in chronic obstructive pulmonary disease. Transl Res J Lab Clin Med. 2012;159:228–37.
Tamaki K, Sakihara E, Miyata H, Hirahara N, Kirichek O, Tawara R, Akiyama S, Katsumata M, Haruya M, Ishii T, Simard EP, Miller BE, Tal-Singer R, Kaise T. Utility of self-administered questionnaires for identifying individuals at risk of COPD in Japan: The OCEAN (Okinawa COPD casE finding AssessmeNt) study. Int J Chron Obstruct Pulmon Dis. 2021;16:1771–82.
Global Initiative for Chronic Obstructive Lung Disease - GOLD. 2020 Global strategy for prevention, diagnosis and management of COPD. Glob. Initiat. Chronic Obstr. Lung Dis. - GOLD 2020 [cited 2021 Aug 10]. Available from: https://goldcopd.org/gold-reports/.
Salvi S. Tobacco smoking and environmental risk factors for chronic obstructive pulmonary disease. Clin Chest Med. 2014;35:17–27.
Gerayeli FV, Milne S, Cheung C, Li X, Yang CWT, Tam A, Choi LH, Bae A, Sin DD. COPD and the risk of poor outcomes in COVID-19: a systematic review and meta-analysis. EClinicalMedicine. 2021;33:100789.
Barnes PJ, Celli BR. Systemic manifestations and comorbidities of COPD. Eur Respir J. 2009;33:1165–85.
Shavelle RM, Paculdo DR, Kush SJ, Mannino DM, Strauss DJ. Life expectancy and years of life lost in chronic obstructive pulmonary disease: findings from the NHANES III follow-up study. Int J Chron Obstruct Pulmon Dis. 2009;4:137–48.
Horner A, Burghuber OC, Hartl S, Studnicka M, Merkle M, Olschewski H, Kaiser B, Wallner EM, Lamprecht B. Quality of life and limitations in daily life of stable COPD outpatients in a real-world setting in Austria - results from the CLARA project. Int J Chron Obstruct Pulmon Dis. 2020;15:1655–63.
Raherison C, Girodet P-O. Epidemiology of COPD. Eur Respir Rev. 2009;18:213–21.
Adeloye D, Chua S, Lee C, Basquill C, Papana A, Theodoratou E, Nair H, Gasevic D, Sridhar D, Campbell H, Chan KY, Sheikh A, Rudan I. Global and regional estimates of COPD prevalence: systematic review and meta–analysis. J Glob Health. 2015;5:020415.
Ciapponi A, Alison L, Agustina M, Demián G, Silvana C, Edgardo S. The epidemiology and burden of COPD in Latin America and the Caribbean: systematic review and meta-analysis. COPD. 2014;11:339–50.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ Br Med J Publ Group. 2021;372:n71.
Munn Z, Moola S, Lisy K, Riitano D, Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. JBI Evid Implement. 2015;13:147–53.
Moreira MAC, Barbosa MA, Jardim JR, Queiroz MCCAM, Inácio LU. Chronic obstructive pulmonary disease in women exposed to wood stove smoke. Rev Assoc Med Bras. 2013;6:607–13.
Orduz García CE, Toro MV, Gómez JC. EPOC, bronquitis crónica y síntomas respiratorios, asociados a la contaminación por PM10 en la ciudad de Medellín (Colombia). Rev Med. 2013;21:21.
Jaganath D, Miranda JJ, Gilman RH, Wise RA, Diette GB, Miele CH, Bernabe-Ortiz A, Checkley W, CRONICAS Cohort Study Group. Prevalence of chronic obstructive pulmonary disease and variation in risk factors across four geographically diverse resource-limited settings in Peru. Respir Res. 2015;16:40.
Rabahi MF, Pereira SA, Silva Júnior JLR, de Rezende AP, Castro da Costa A, de Sousa CK, Conde MB. Prevalence of chronic obstructive pulmonary disease among patients with systemic arterial hypertension without respiratory symptoms. Int J Chron Obstruct Pulmon Dis. 2015;10:1525–9.
Sansores R, Ramírez-Venegas A, Pérez-Bautista O, Falfán-Valencia R, Villalba J, Velázquez-Uncal M. Prevalence of chronic obstructive pulmonary disease in asymptomatic smokers. Int J Chron Obstruct Pulmon Dis. 2015;10:2357.
López Varela MV, Montes de Oca M, Rey A, Casas A, Stirbulov R, Di Boscio V, PUMA Team. Development of a simple screening tool for opportunistic COPD case finding in primary care in Latin America: the PUMA study. Respirology. 2016;21:1227–34.
Sobrino E, Irazola VE, Gutierrez L, Chen C-S, Lanas F, Calandrelli M, Ponzo J, Mores N, Serón P, Lee A, He J, Rubinstein AL. Estimating prevalence of chronic obstructive pulmonary disease in the Southern Cone of Latin America: how different spirometric criteria may affect disease burden and health policies. BMC Pulm Med. 2017;17:187.
de Queiroz MC, Moreira MAC, Rabahi MF. Underdiagnosis of COPD at primary health care clinics in the city of Aparecida de Goiânia, Brazil. J Bras Pneumol. 2012;38:692–9.
Laniado-Laborin R, Rendón A, Bauerle O. Chronic obstructive pulmonary disease case finding in Mexico in an at-risk population. Int J Tuberc Lung Dis. 2011;15:818–23.
López Varela MV, Montes de Oca M, Halbert R, Muiño A, Tálamo C, Pérez-Padilla R, Jardim JRB, Valdivia G, Pertuzé J, Menezes AMB. Comorbilidades y estado de salud en individuos con y sin EPOC en 5 ciudades de América Latina: Estudio PLATINO. Arch Bronconeumol. 2013;11:468–74.
Ramírez-Venegas A, Velázquez-Uncal M, Pérez-Hernández R, Guzmán-Bouilloud NE, Falfán-Valencia R, Mayar-Maya ME, Aranda-Chávez A, Sansores RH. Prevalence of COPD and respiratory symptoms associated with biomass smoke exposure in a suburban area. Int J Chron Obstruct Pulmon Dis. 2018;13:1727–34.
Echazarreta AL, Arias SJ, del Olmo R, Giugno ER, Colodenco FD, Arce SC, Bossio JC, Armando G, Soriano JB. Prevalencia de enfermedad pulmonar obstructiva crónica en 6 aglomerados urbanos de Argentina: el estudio EPOC.AR. Arch Bronconeumol. 2018;54:260–9.
Siddharthan T, Grigsby MR, Goodman D, Chowdhury M, Rubinstein A, Irazola V, Gutierrez L, Miranda JJ, Bernabe-Ortiz A, Alam D, Kirenga B, Jones R, van Gemert F, Wise RA, Checkley W. Association between household air pollution exposure and chronic obstructive pulmonary disease outcomes in 13 low- and middle-income country settings. Am J Respir Crit Care Med. 2018;197:611–20.
Vieira Rocha SA, de Carvalho Hoepers AT, Fröde TS, Marques Steidle LJ, Pizzichini E, Menezes Pizzichini MM. Prevalence of smoking and reasons for continuing to smoke: a population-based study. J Bras Pneumol. 2019;45:e20170080.
Romero-López Z, Rojas-Cisneros FA, Ochoa-Vázquez MD, Rico-Méndez FG, Mata-Marín JA. Prevalence of chronic obstructive pulmonary disease in patients diagnosed with HIV without prior antiretroviral treatment. Gac Méd Mex. 2020;156(4):283–9.
Bastidas Goyes AR, Barragán Amado AF, Martinez MM, Pinzón Villamil N, Daniel AM. Validation and reproducibility of the lung function questionnaire (LFQ) for the diagnosis of COPD in Colombia. Pneumologia. 2020;69:37–46.
Conyette L, Lutchmansingh F, Sakhamuri S, Simeon D, Ivey MA, Burney P, Seemungal T. Prevalence and risk factors of airflow obstruction in a Caribbean population. Int J Tuberc Lung Dis. 2020;24:512–9.
Karloh M, Vieira Rocha SA, Menezes Pizzichini MM, Cavalli F, Matte DL, Pizzichini E. Is the COPD assessment test sensitive for differentiating COPD patients from active smokers and nonsmokers without lung function impairment. A population-based study. J Bras Pneumol. 2018;44:213–9.
Chatkin G, Chatkin JM, Aued G, Oliveira Petersen G, Thais Jeremias E, Valladão TF. Avaliação da concentração de monóxido de carbono no ar exalado em tabagistas com DPOC. J Bras Pneumol. 2010;36:332–8.
Moreira GL, Gazzotti MR, Manzano BM, Nascimento O, Perez-Padilla R, Menezes AMB, Jardim JR. Incidence of chronic obstructive pulmonary disease based on three spirometric diagnostic criteria in Sao Paulo, Brazil: a nine-year follow-up since the PLATINO prevalence study. Sao Paulo Med J. 2015;3:245–51.
WHO global report on trends in prevalence of tobacco use 2000–2025, third edition. [cited 2021 Aug 25].Available from: https://www.who.int/publications-detail-redirect/who-global-report-on-trends-in-prevalence-of-tobacco-use-2000-2025-third-edition.
Perez-Padilla R, Menezes AMB. Chronic obstructive pulmonary disease in Latin America. Ann Glob Health. 2019;85:7.
Sandford AJ, Weir TD, Paré PD. Genetic risk factors for chronic obstructive pulmonary disease. Eur Respir J. 1997;10:1380–91.
Menezes AMB, Hallal PC, Perez-Padilla R, Jardim JRB, Muiño A, Lopez MV, Valdivia G, de Oca MM, Talamo C, Pertuze J, Victora CG. Tuberculosis and airflow obstruction: evidence from the PLATINO study in Latin America. Eur Respir J. 2007;30:1180–5.
Malta DC, Flor LS, Machado ÍE, Felisbino-Mendes MS, Brant LCC, Ribeiro ALP, Teixeira RA, Macário EM, Reitsma MB, Glenn S, Naghavi M, Gakidou E. Trends in prevalence and mortality burden attributable to smoking, Brazil and federated units, 1990 and 2017. Popul Health Metr. 2020;18:24.
Malta DC, Morais Neto OL de, Silva Junior JB da. Apresentação do plano de ações estratégicas para o enfrentamento das doenças crônicas não transmissíveis no Brasil, 2011 a 2022. Epidemiol. E Serviços Saúde Coordenação-Geral de Desenvolvimento da Epidemiologia em Serviços / Secretaria de Vigilância em Saúde / Ministério da Saúde. 2011;20:425–438.
Ntritsos G, Franek J, Belbasis L, Christou MA, Markozannes G, Altman P, Fogel R, Sayre T, Ntzani EE, Evangelou E. Gender-specific estimates of COPD prevalence: a systematic review and meta-analysis. Int J Chron Obstruct Pulmon Dis. 2018;13:1507–14.
Zhang M, Liu S, Yang L, Jiang Y, Huang Z, Zhao Z, Deng Q, Li Y, Zhou M, Wang L, Chen Z, Wang L. Prevalence of smoking and knowledge about the hazards of smoking among 170 000 Chinese adults, 2013–2014. Nicotine Tob Res. 2019;21:1644–51.
Martínez-Aguilar NE, Vargas-Camaño ME, Hernández-Pliego RR, Chaia-Semerena GM, del Pérez-Chavira MR, Martínez-Aguilar NE, Vargas-Camaño ME, Hernández-Pliego RR, Chaia-Semerena GM, del Pérez-Chavira MR. Inmunopatología de la enfermedad pulmonar obstructiva crónica. Rev Alerg Méx. 2017;64:327–46.
Salvi SS, Barnes PJ. Chronic obstructive pulmonary disease in non-smokers. Lancet Lond Engl. 2009;374:733–43.
Vega-Sánchez ÁE, Téllez-Navarrete NA, Pérez-Padilla R. chronic obstructive pulmonary disease: perspectives for primary health care. Rev Investig Clín. 2019;71:55–63.
National Center for Chronic Disease Prevention and Health Promotion (U.S.). Public health strategic framework for COPD prevention. 2011 [cited 2022 Jun 16]. Available from: https://stacks.cdc.gov/view/cdc/12104.
Acknowledgements
Special thanks to Moises Huarhua, from Universidad Peruana Unión, who provided support by reviewing the draft of this article and to Josmel Pacheco-Mendoza, from Universidad San Ignacio de Loyola, who reviewed the systematic search strategy.
Funding
This article was self-funded by the authors.
Author information
Authors and Affiliations
Contributions
Conception of study and development of protocol: JJOR, DRSM, ABB, PPL; Study coordination: DRSM; Searches: DRSM and ABB; Data Extraction, Data Verification, Arbitration: JJOR, DRSM, ABB, PPL; Data Synthesis/Analysis: DRSM and JHM. Data discussions and drafting paper: All authors; All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. Supplementary materials S1–9.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Olortegui-Rodriguez, J.J., Soriano-Moreno, D.R., Benites-Bullón, A. et al. Prevalence and incidence of chronic obstructive pulmonary disease in Latin America and the Caribbean: a systematic review and meta-analysis. BMC Pulm Med 22, 273 (2022). https://doi.org/10.1186/s12890-022-02067-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-022-02067-y