Abstract
Background
People living with HIV(PLWH) are deemed more vulnerable to the SARS-CoV-2 infection than the uninfected population. Vaccination is an effective measure for COVID-19 control, yet, little knowledge exists about the willingness of men who have sex with men (MSM) living with HIV in China to be vaccinated.
Methods
This cross-sectional study evaluated the willingness of MSM living with HIV to receive COVID-19 vaccination in six cities of Guangdong, China, from July to September 2020. Factors associated with willingness to receive COVID-19 vaccination using multivariable logistic regression.
Results
In total, we recruited 944 HIV-positive MSM with a mean age of 29.2 ± 7.7 years. Of all participants, 92.4% of them were willing to receive the COVID-19 vaccine. Participants who were separated, divorced, or widowed (adjusted OR: 5.29, 95%CI: 1.02–27.48), had an annual income higher than 9,000 USD (adjusted OR: 1.70, 95%CI: 1.01–2.86), had ever taken an HIV self-test (adjusted OR: 1.78, 95%CI: 1.07–2.95), had ever disclosed sexual orientation to a doctor/nurse (adjusted OR: 3.16, 95%CI: 1.33–7.50), had ever disclosed sexual orientation to others besides their male partners (adjusted OR: 2.18, 95%CI: 1.29–3.69) were more willing to receive the vaccine. Sex with a female partner in the past six months decreased the likelihood of willingness to receive the vaccine (adjusted OR: 0.40, 95%CI: 0.17–0.95). Economic burden, worry that my health condition could not bear the risk of receiving COVID-19 vaccines, and concern that the vaccination would affect the immune status and antiretroviral therapy were the main reasons for unwillingness to receive vaccination.
Conclusion
Our study showed that HIV-positive MSM had a high willingness to receive the COVID-19 vaccination. Targeted interventions such as health education should be conducted among MSM with HIV infection to enhance COVID-19 vaccine uptake.
Similar content being viewed by others
Introduction
The coronavirus disease 2019 (COVID-19) is a severe respiratory infection caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The pandemic reportedly caused more than 500 million infections and 6 million deaths globally by May 2022 [1]. Studies have shown that people living with HIV(PLWH) have an increased risk of SARS-CoV-2 infection and mortality [2]. The COVID-19 pandemic also brought other impacts to PLWH, including affecting their physical, emotional, and social well-being, interfering with the delivery of effective healthcare and access to HIV treatment [3]. Surveillance data had shown that over one-third of men who have sex with men (MSM) living with HIV in the United States were not on adequate treatment and may be immunocompromised, potentially increasing risks associated with susceptibility of COVID-19 [4]. And the stigma and discrimination for MSM also may result in health inequities, which bring the higher risk for COVID-19 [5, 6].
Vaccination is considered one of the most effective strategies for infectious diseases prevention and control [7]. Existing surveys suggest that the COVID-19 vaccination should reach a minimum coverage of 70% to achieve the herd immunity required for epidemic control [8]. Several COVID-19 vaccines have been approved for use in many countries [9]. However, the vaccination uptake was still low [10], especially among the vulnerable population [11, 12]. Improved understanding of the willingness to receive COVID-19 vaccines and associated factors can inform more comprehensive and equitable vaccine implementation strategies [13]. Several studies have explored the willingness to receive COVID-19 vaccination and its associated factors among different populations. In the general population, the rates of COVID-19 vaccination willingness reportedly range from 23.6 to 97% globally [14,15,16] and higher than 80% in China [17, 18]. Furthermore, a previous study among French PLWH showed that approximately 70% were willing to receive the COVID-19 vaccine and others hesitated for various reasons [19]. Another study conducted in the USA reported a moderately high acceptance of the COVID-19 vaccine among sexual and gender minority men and transgender women [20]. However, studies assessing willingness to accept COVID-19 vaccination among HIV-positive MSM in low- and middle-income countries, including China, are rare.
In China, seven COVID-19 candidate vaccines are in clinical trials, three of which are in Phase 3 trials as of August 2020 [21]. The results showed that the candidate COVID-19 vaccines had good immunogenicity and safety [21]. Even though the COVID-19 epidemic has slowed [22], multiple local outbreaks in China along with the ongoing import of cases from overseas. This put the vast majority of the Chinese population without immunity against SARS-CoV-2, especially vulnerable groups like PLWH, at continued risk of infection. In response to the potential re-emergence of COVID-19 epidemics in China, it is necessary to understand the willingness of MSM living with HIV to be vaccinated and take measures to improve vaccination coverage.
Till now, little is known about the willingness to receive COVID-19 vaccination among HIV-positive MSM and associated factors in China, which bring difficulty for controlling the pandemic of COVID-19 among people living with HIV. This study aimed to investigate the willingness to receive the COVID-19 vaccine and to assess the factors associated with COVID-19 vaccination among HIV-positive MSM to provide a reference for COVID-19 vaccine promotion strategies. We hypothesized that factors associated with the COVID-19 vaccination willingness among HIV-positive MSM were various and perceptions of COVID-19 vaccination would affect their willingness.
Methods
Study design and participants
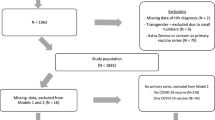
This cross-sectional study was performed between July and September 2020. Study participants complied with the following inclusion criteria: born as male; ≥ 18 years old; identified as living with HIV in the past two years; transmitted through homosexual route; and currently live in the six southern cities (Guangzhou, Shenzhen, Zhongshan, Dongguan, Foshan, and Zhuhai) of Guangdong Province, China. Participants who were not able to understand the questionnaire items or refused to be surveyed were excluded. All the participants were recruited by a convenience sampling technique through sending an invitation to the registered MSM HIV cases identified after 2018 by the local Center for Disease Control and Prevention (CDC) or the HIV healthcare centers. After the screening, all the eligible participants electrically signed on the informed consent and completed an online self-administered questionnaire. The Chinese online survey tool, Wenjuanxing (www.wjx.cn), was used to administer the survey. The sample size was computed via the formula N = Zα2 p (1—p)/d2, where α = 0.05 and Zα = 1.96. The estimated acceptable margin of error for proportion d was 0.05, and the proportion of MSM living with HIV who were willing to receive the COVID-19 vaccination was estimated at 50%. Finally, the minimum sample size was estimated at about 385. This proposed study aimed to recruit 1000 newly identified HIV-positive MSM for an HIV partner notification survey across the six study cities in Guangdong province of China [23], which is more than the minimum sample size required.
Measures
Sociodemographic information, including age, employment status (employed or unemployed), marital status (unmarried, engaged or married, separated or divorced, widowed), education level (high school or lower, higher than high school), annual income (≤ 9000USD, > 9000USD), gender identity (male, female, transgender, unsure/other), and sexual orientation (homosexual, bisexual, heterosexual, unsure/other), was collected from each eligible participant. Solicited data on sexual behavior in the preceding six months included ever had sex with a female partner, ever had multiple male sexual partners, ever had stable male sex partners, ever had casual male sex partners, and so on. Clinical characteristics assessed included whether participants had comorbidities, had ever self-tested for HIV, the first CD4 + T lymphocyte count (CD4 count). Sexual orientation disclosure, defined as having discussed their sexual orientation with a doctor/nurse or others, was also assessed. The participants’ perception of susceptibility was also collected, which was measured by a single yes or no item: "Do you think HIV-positive members are more likely to get infected with COVID-19?". Willingness to receive the COVID-19 vaccination was measured by the single yes or no item "Would you be willing to receive COVID-19 vaccine if provided?". The reasons for willingness or unwillingness to receive the COVID-19 vaccination was also asked by some yes or no questions (multiple answers).
Statistical analysis
Categorical variables were presented as numbers (n)/percentage (%) and compared with the Chi-square test or Fisher's exact test. Continuous variables were presented as mean and standard deviation (normally distributed) or the median and interquartile range (non-normally distributed) and compared with the t-test or Wilcoxon rank-sum test. Univariable and multivariable logistic regression analysis was used to determine whether any factors (age groups, educational level, annual income, employment status, and other factors) were associated with the willingness of COVID-19 vaccination. A stepwise forward method of selecting variables was applied and variables with p values < 0.10 in the likelihood ratio test entered the multivariable logistic regression model. The goodness of fit to the logistic regression model was tested using the Hosmer–Lemeshow goodness-of-fit test. The associations between the potential influencing factors and outcomes were presented as odds ratios (ORs) and 95% confidence intervals (CIs). A two-tailed p-value < 0.05 was statistically significant. Data were analyzed using SPSS version 26 (IBM Corp., Armonk, NY).
Ethics statement
This study was approved by Ethics Committee of Guangzhou Center for Disease Control and Prevention (GZCDC-ER-P2019001). Signed electronic informed consent forms were obtained from all participants involved in the study.
Results
Characteristics of study participants
Total 944 participants were recruited in this study. The mean age of the participants was 29.2 ± 7.7 years. The majority of participants were unmarried (81.9%), employed (96.9%), had higher than high school education (54.5%), and 53.2% (502/944) earned 9000 USD or less annually. 95.1% (898/944) had self-identified their gender as male, and 70.8% (668/944) were homosexuals (Table 1).
Among them, 26.1% (246/944) had comorbidities (hypertension, diabetes, or others), 44.3% (418/944) had the first CD4 count lower than 500/μL, and 59.1% (558/944) had ever taken an HIV self-test; 73.0% (689/944) did not have multiple male sexual partners in the last six months, 94.7%(894/944) did not have sex with a female partner in the past six months, 34.6% (327/944) had stable male sex partners in the past six months, and 25.5% had casual male sex partners in the past six months. Besides, 23.0% (217/944) had ever disclosed their sexual orientation to a doctor/nurse, and 82.8% (782/944) had ever disclosed their sexual orientation to others besides their male partners.
Willingness to receive the COVID-19 vaccine
The willingness to receive COVID-19 vaccination in different cities were shown in Fig. 1. Overall, 92.4% (872/994) of participants were willing to receive the COVID-19 vaccine, and 60.3% (569/944) were willing to pay for the COVID-19 vaccine.
A significantly higher willingness was observed in MSM living with HIV who had high school level or higher education, had ever self-tested for HIV, disclosed their sexual orientation to a doctor/nurse, disclosed their sexual orientation to others besides their male partners and had not have sex with a female partner in the past six months (all p < 0.05) (Table 1).
Factors associated with willingness to receive the COVID-19 vaccine
Univariate logistic regression showed that marital status, educational level, ever had taken an HIV self-test, sexual orientation disclosure to a doctor/nurse, sexual orientation disclosure to others besides male partners and ever had sex with a female partner in the past six months were associated with willingness to receive COVID-19 vaccination among MSM living with HIV (p < 0.05, unadjusted ORs were shown in Table 2).
We further adjusted confounding factors using a forward stepwise multivariable logistic regression model, the Nagelkerke R2 showed that the model is explaining 14.4% of the variation in willingness to receive COVID-19 vaccination, the outcome of Hosmer and Lemeshow Test (χ2 = 9.87, df = 7, p = 0.196) showed the model had a good fit. According to the results of Table 2, participants who were separated, divorced, or widowed (adjusted OR: 5.29, 95%CI: 1.02–27.48), had an annual income higher than 9000 USD (adjusted OR: 1.70, 95%CI: 1.01–2.86), had ever taken an HIV self-test (adjusted OR: 1.78, 95%CI: 1.07–2.95), sexual orientation disclosure to a doctor/nurse (adjusted OR: 3.16, 95%CI: 1.33–7.50), and sexual orientation disclosure to others besides male partners (adjusted OR: 2.18, 95%CI: 1.29–3.69) were associated with increased likelihood of willingness to receive COVID-19 vaccination among MSM living with HIV. However, participants who had ever had sex with a female partner in the past six months were associated with decreased the likelihood of willingness to receive the vaccine (adjusted OR: 0.40, 95%CI: 0.17–0.95).
Reasons for vaccination decisions
As shown in Fig. 2, 32.1% (280/872) participants cited a willingness to be vaccinated when provided for free. We observed a J-shaped distribution of the willingness to accept vaccination among willing participants, and 30.0% (270/872) of participants expressed their willingness to pay below 15 USD, which declined to 5.6% (49/872) when the price was higher than 150 USD.
The main reasons for unwillingness to receive the COVID-19 vaccine were “economic burden (43.1%)”, “Worry that my health condition could not bear the risk of receiving COVID-19 vaccines (30.6%)”, “Worry that the vaccination will affect my immune status and antiretroviral therapy” and “Worry about the quality of the vaccine” (22.2%). Moreover, the main reasons for willingness to be vaccinated were “I don’t want to get infection with SARS-CoV-2 (78.4%)”, "I worry that my risk of COVID-19 infection is higher than normal people (47.5%)”, and “I worry that my condition will be worse than normal people if infected (37.6%)” (Table 3).
Discussion
Understanding the willingness to receive the COVID-19 vaccine among HIV-positive MSM is essential in improving the COVID-19 vaccination rate. We found that the majority of the MSM living with HIV were willing to receive the COVID-19 vaccine. Factors including having ever taken an HIV self-test, sexual orientation disclosure to a doctor/nurse or others, annual income, and marital status were associated with COVID-19 vaccination willingness.
Our study showed that around 92% of the HIV-positive MSM are willing to receive the COVID-19 vaccine. This proportion was higher than that of PLWH in France [19] and the United States [20] as well as the general population in most parts of the world [24,25,26] and China [17]. Findings from several studies suggested that the willingness to get vaccinated against COVID-19 has evolved [27]. Even though willingness was relatively high in this study, we should continually be concerned about the willingness to get vaccination against COVID-19 among HIV-positive MSM at different times.
In our study, the participant who had ever disclosed their sexual orientation to a doctor/nurse or others besides their male partners and those who ever self-tested for HIV had a higher willingness to receive the COVID-19 vaccine. Studies have shown that HIV-positive MSM who had ever disclosed their sexual orientation to health providers or ever self-tested for HIV had less HIV stigma [28], while HIV stigma was a barrier for accessing health services, including vaccinations [29]. Previous studies have also shown the introduction of quality comprehensive HIV care to reduce stigma and increase uptake of HIV services, including vaccinations [30, 31]. MSM living with HIV who had ever disclosed their sexual orientation to a nurse/doctor were more likely to receive the COVID-19 vaccine, which suggests that the health providers could play an essential role in promoting the uptake of COVID-19 vaccines. Also, reports show that MSM with full disclosure to a primary clinician may have increased optimal uptake of vaccinations [32]. Thus, potential interventions to promote sexual orientation disclosure without prejudice may help to improve COVID-19 vaccination uptake [32]. In addition, participants who had ever self-tested for HIV may have better knowledge and awareness about HIV [33], and that may cause them to have a higher willingness for the vaccine.
Our study findings also suggest that separated, divorced, or widowed MSM living with HIV had a higher likelihood of willingness to receive COVID-19 vaccination than married ones. This finding was inconsistent with other studies [17, 34]. Separated, divorced, or widowed living alone with limited assistance often could have accounted for this finding. They may have limited access to healthcare, irregular health facility visits, and less support from family members [35]. And this may cause them to seek preventive measures that protect them from further infections. Our study also showed that MSM living with HIV who earned more than 9000 USD annually had a higher willingness to receive the COVID-19 vaccine. This observation is similar to the results of some other studies [36, 37] and could be because people with higher income may pay more attention to their health and adopt healthier COVID-19 prevention behaviors. Besides, the rate of willingness to receive COVID-19 vaccination declined from 92.4 to 62.1% if the vaccine would not be free, and only a few participants (2.5%) would afford more than 150 USD for it. Our study results showed that participants perceive ‘Economic burden’ as a significant barrier to receive COVID-19 vaccination. The results also suggest that offering the COVID-19 vaccines for a lower cost or free might improve the willingness to receive vaccination among MSM living with HIV. While this may not be a barrier in China as COVID-19 vaccinations are currently offered for free [38] but may hinder uptake in countries with paid COVID-19 vaccination programs.
Our study showed different reasons for willingness or unwillingness to receive the COVID-19 vaccine. The main reasons for unwillingness to receive the COVID-19 vaccination indicate that participants may have concerns about the side effects and the impact on the immune status and antiviral therapy after the COVID-19 vaccination. However, the United Nations AIDS program (UNAIDS) recommends that COVID-19 vaccines are safe for PLWH and could bring them the same benefits as uninfected individuals. Hence, the COVID-19 vaccination should be recommended for PLWH regardless of their CD4 count and HIV viral load levels and possibly prioritized in vaccination rollouts [39]. The national technical guideline for COVID-19 vaccination in China encourages PLWH to take up inactivated vaccines or recombinant subunit vaccines [40]. A recent pilot study conducted by the Chinese National Center for Clinical Laboratories found that 60 and 63% of PLWHA who had received two doses of COVID-19 vaccine stimulate neutralizing antibody or T-cell responses, respectively, without any severe side effect after vaccination [41]. Therefore, perceptions on COVID-19 vaccination should be improved among HIV-positive MSM.
This study provided crucial information on the willingness to receive COVID-19 vaccination among HIV-positive MSM and associated factors, which could provided reference for developing tailored vaccination strategies for HIV-positive MSM. More attention should be paid to HIV-positive MSM who had lower income as these group reported lower willingness. Additionally, health education programs should be designed and developed to improve perceptions related to COVID-19 vaccination among HIV-positive MSM and their confidence in COVID-19 vaccines to improve the vaccination rate.
Some of the advantages of our research are worth noticing. This study was investigated 4 months before the initiation of national free vaccination policy, which offered the initial insights about willingness to receive COVID-19 vaccination among HIV-positive MSM with relatively large sample. The study also had some limitations. First, information on sexual behaviors was collected using a questionnaire. Therefore, sexual risks may have been over-reported or under-reported due to reporting and social desirability bias. However, administering the questionnaire online provided anonymity that reduced the risk of this bias. Second, our study participants might not represent the general population of MSM living with HIV in China due to the potential limitations of our purposive enrollment methods. Third, the cross-sectional study method limited association analysis. Fourth, our study was conducted before September 2020, when the COVID-19 vaccine had not been approved in China yet. Hence, it was unknown whether the COVID-19 vaccines would be offered freely in China. Moreover, the limited information about vaccination eligibility and locations influenced people’s thoughts, decisions, and perceptions about getting vaccinated. Therefore, an individual’s willingness to get vaccinated may evolve with new information [42, 43]. However, our findings showed strong demand for the vaccine and the high recognition of vaccination importance among MSM with HIV. And this could still provide a reference for the implementation of vaccination programs among MSM living with HIV. Despite the above limitations, our study has important strengths. We examined the willingness to receive COVID-19 vaccination using a large-scale sample of participants. We would subsequently conduct a more comprehensive research at a different time to compare with the results of this study next.
Conclusions
In conclusion, our study showed that a large majority of MSM living with HIV are willing to receive the COVID-19 vaccine. MSM living with HIV in China who had ever taken an HIV self-test and disclosed their sexual orientation to a doctor/nurse or others were more willing to receive the COVID-19 vaccination. Targeted interventions such as health education should be conducted among MSM with HIV infection to enhance COVID-19 vaccine uptake.
Availability of data and materials
The datasets used and/or analyzed during the current study are not publicly available due to protect the privacy and confidentiality of participants in this study but are available upon reasonable request to the corresponding author.
Abbreviations
- PLWH:
-
People living with HIV
- MSM:
-
Men who have sex with men
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus 2
- COVID-19:
-
Coronavirus disease 2019
- CDC:
-
Center for Disease Control and Prevention
- Cis:
-
Confidence intervals
References
Kim SY, Yeniova AÖ. Global, regional, and national incidence and mortality of COVID-19 in 237 countries and territories, January 2022: a systematic analysis for World Health Organization COVID-19 Dashboard. Life Cycle. 2022;2:e10.
Lee KW, Yap SF, Ngeow YF, Lye MS. COVID-19 in people living with HIV: a systematic review and meta-analysis. Int J Environ Res Public Health. 2021;18(7):3554.
Shiau S, Krause KD, Valera P, Swaminathan S, Halkitis PN. The Burden of COVID-19 in People Living with HIV: a syndemic perspective. AIDS Behav. 2020;24(8):2244–9.
Centers for Disease Control and Prevention. Selected National HIV Prevention and Care Outcomes. 2019. https://www.cdc.gov/hiv/ppt/library/slidesets/cdc-hiv-prevention-and-care-outcomes-2016.pptx. Accessed 04 Dec 2020.
Heslin KC, Hall JE. Sexual orientation disparities in risk factors for adverse COVID-19-related outcomes, by race/ethnicity - behavioral risk factor surveillance system, United States, 2017–2019. MMWR Morb Mortal Wkly Rep. 2021;70(5):149–54.
Gibb JK, DuBois LZ, Williams S, McKerracher L, Juster RP, Fields J. Sexual and gender minority health vulnerabilities during the COVID-19 health crisis. Am J Hum Biol. 2020;32(5): e23499.
Delany I, Rappuoli R, De Gregorio E. Vaccines for the 21st century. EMBO Mol Med. 2014;6(6):708–20.
D’souza G, DOWDY D. What is Herd Immunity and How Can We Achieve It With COVID-19? Johns Hopkins Bloomerg SchooL of Public Health. 2021 [4/6/2021]. Available at: https://www.jhsph.edu/covid-19/articles/achieving-herd-immunity-with-covid19.html. Accessed on 26th May, 2021.
Wouters OJ, Shadlen KC, Salcher-Konrad M, et al. Challenges in ensuring global access to COVID-19 vaccines: production, affordability, allocation, and deployment. Lancet. 2021;397(10278):1023–34.
Kim SY, Ahmad S. Global, regional, and national disruptions to COVID-19 vaccine coverage in 237 countries and territories, March 2022: a systematic analysis for World Health Organization COVID-19 Dashboard, Release 1. Life Cycle. 2022;2:e14.
Hughes MM, Wang A, Grossman MK, et al. County-Level COVID-19 vaccination coverage and social vulnerability - United States, December 14, 2020-March 1, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(12):431–6.
Chou WS, Budenz A. Considering emotion in COVID-19 vaccine communication: addressing vaccine hesitancy and fostering vaccine confidence. Health Commun. 2020;35(14):1718–22.
Soares P, Rocha JV, Moniz M, et al. Factors associated with COVID-19 vaccine hesitancy. Vaccines (Basel). 2021;9(3):300.
Sallam M. COVID-19 vaccine hesitancy worldwide: a concise systematic review of vaccine acceptance rates. Vaccines (Basel). 2021;9(2):160.
Patwary MM, Bardhan M, Disha AS, Hasan M, Haque MZ, Sultana R, Hossain MR, Browning M, Alam MA, Sallam M. Determinants of COVID-19 Vaccine Acceptance among the Adult Population of Bangladesh Using the Health Belief Model and the Theory of Planned Behavior Model. Vaccines (Basel). 2021;9(12):1393.
Patwary MM, Alam MA, Bardhan M, Disha AS, Haque MZ, Billah SM, Kabir MP, Browning M, Rahman MM, Parsa AD, et al. COVID-19 vaccine acceptance among low- and lower-middle-income countries: a rapid systematic review and meta-analysis. Vaccines (Basel). 2022;10(3):427.
Wang J, Jing R, Lai X, et al. Acceptance of COVID-19 vaccination during the COVID-19 pandemic in China. Vaccines (Basel). 2020;8(3):482.
Lin Y, Hu Z, Zhao Q, Alias H, Danaee M, Wong LP. Understanding COVID-19 vaccine demand and hesitancy: a nationwide online survey in China. PLoS Negl Trop Dis. 2020;14(12): e0008961.
Vallee A, Fourn E, Majerholc C, Touche P, Zucman D. COVID-19 vaccine hesitancy among French people living with HIV. Vaccines (Basel). 2021;9(4):302.
Teixeira da Silva D, Biello K, Lin WY, et al. COVID-19 vaccine acceptance among an online sample of sexual and gender minority men and transgender women. Vaccines (Basel). 2021;9(3):204.
World Health Organization. Draft landscape of COVID-19 candidate vaccines. 2020.
Tu H, Tu S, Gao S, Shao A, Sheng J. Current epidemiological and clinical features of COVID-19; a global perspective from China. J Infect. 2020;81(1):1–9.
Cheng W, Cai Y, Tang W, et al. Providing HIV-related services in China for men who have sex with men. Bull World Health Organ. 2016;94(3):222–7.
Reiter PL, Pennell ML, Katz ML. Acceptability of a COVID-19 vaccine among adults in the United States: How many people would get vaccinated? Vaccine. 2020;38(42):6500–7.
Kourlaba G, Kourkouni E, Maistreli S, et al. Willingness of Greek general population to get a COVID-19 vaccine. Glob Health Res Policy. 2021;6(1):3.
Al-Mohaithef M, Padhi BK. Determinants of COVID-19 vaccine acceptance in Saudi Arabia: a web-based national survey. J Multidiscip Healthc. 2020;13:1657–63.
Wang K, Wong EL, Ho KF, et al. Change of willingness to accept COVID-19 vaccine and reasons of vaccine hesitancy of working people at different waves of local epidemic in Hong Kong, China: repeated cross-sectional surveys. Vaccines (Basel). 2021;9(1):62.
Li Z, Hsieh E, Morano JP, Sheng Y. Exploring HIV-related stigma among HIV-infected men who have sex with men in Beijing, China: a correlation study. AIDS Care. 2016;28(11):1394–401.
Arya BK, Khan T, Das RS, Guha R, Das BS. Determinants of vaccine uptake in HIV-affected families from West Bengal. Hum Vaccin Immunother. 2021;17(7):2036–42.
Castro A, Farmer P. Understanding and addressing AIDS-related stigma: from anthropological theory to clinical practice in Haiti. Am J Public Health. 2005;95(1):53–9.
Tang W, Mao J, Tang S, et al. Disclosure of sexual orientation to health professionals in China: results from an online cross-sectional study. J Int AIDS Soc. 2017;20(1):21416.
Metheny N, Stephenson R. Disclosure of sexual orientation and Uptake of HIV testing and hepatitis vaccination for rural men who have sex with men. Ann Fam Med. 2016;14(2):155–8.
Balan IC, Carballo-Dieguez A, Frasca T, Dolezal C, Ibitoye M. The impact of rapid HIV home test use with sexual partners on subsequent sexual behavior among men who have sex with men. AIDS Behav. 2014;18(2):254–62.
Zhang KC, Fang Y, Cao H, et al. Behavioral intention to receive a COVID-19 vaccination among Chinese factory workers: cross-sectional online survey. J Med Internet Res. 2021;23(3): e24673.
Nagata JM, Hernandez-Ramos I, Kurup AS, Albrecht D, Vivas-Torrealba C, Franco-Paredes C. Social determinants of health and seasonal influenza vaccination in adults >/=65 years: a systematic review of qualitative and quantitative data. BMC Public Health. 2013;13:388.
Fisher KA, Bloomstone SJ, Walder J, Crawford S, Fouayzi H, Mazor KM. Attitudes toward a potential SARS-CoV-2 vaccine: a survey of U.S adults. Ann Intern Med. 2020;173(12):964–73.
Pazol K, Robbins CL, Black LI, et al. Receipt of selected preventive health services for women and men of reproductive age - United States, 2011–2013. MMWR Surveill Summ. 2017;66(20):1–31.
Central People's Government of the People's Republic of China. The COVID-19 vaccines are free for all people. 2021 [1/9/2021]; Available at: http://www.gov.cn/xinwen/2021-01/09/content_5578406.htm. Accessed on 26 May 2021.
UNAIDS. COVID-19 vaccines and HIV. 2021 [2/14/2021]; Available at: https://www.unaids.org/en/resources/documents/2021/covid19-vaccines-and-hiv. Accessed on 26 May 2021.
Central People's Government of the People's Republic of China. Technical Guidelines for the COVID-19 Vaccination (First Edition). 2021 [3/29/2021]; Available at: http://www.gov.cn/xinwen/2021-03/29/content_5596577.htm. Accessed on 26 May 2021.
Xu J, TW. COVID-19 vaccination willingness and actual uptake among People Living with HIV in China. UNC Project-China 2021 Meeting, Guangzhou, China, 2021.
Robinson E, Jones A, Lesser I, Daly M. International estimates of intended uptake and refusal of COVID-19 vaccines: a rapid systematic review and meta-analysis of large nationally representative samples. Vaccine. 2021;39(15):2024–34.
Nguyen KH, Srivastav A, Razzaghi H, et al. COVID-19 vaccination intent, perceptions, and reasons for not vaccinating among groups prioritized for early vaccination - United States, September and December 2020. Am J Transplant. 2021;70(6):217–22.
Acknowledgements
Not applicable.
Funding
This work was supported by the National Key Research and Development Program of China (2017YFE0103800), the National Nature Science Foundation of China (81903371), NIMH (R34MH119963), the National Science and Technology Major Project (2018ZX10101-001–001-003), and Special Found on Prevention and Control of New Coronary Pneumonia in Guangdong Universities (2020KZDZX1047), Medical Science and Technology Innovation Platform Support Project of Zhongnan Hospital, Wuhan University (PTXM2020008), The Non-profit Central Research Institute Fund of Chinese Academy of Medical Sciences (2020-PT320-004), Science and Technology Innovation Cultivation Fund of Zhongnan Hospital, Wuhan University (cxpy2017043). Medical Science Advancement Program (Basic Medical Sciences) of Wuhan University (TFJC2018004).
Author information
Authors and Affiliations
Contributions
WT and LK conceived and designed this investigation and YXM, XYS, and XHF helped to design the study. YF, HZG, GYZ, ZYR, YZR, YHK, and SB collected the data, and WSJ and ZSH analyzed the data. WSJ, TWM, and LK contributed to the interpretation of the data. WSJ, TWM, and LK contributed to the writing of the paper. The author(s) read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by Ethics Committee of Guangzhou Center for Disease Control and Prevention (GZCDC-ER-P2019001) and followed the recommendations of Helsinki Declaration. Signed electronic informed consent forms were obtained from all participants involved in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wu, S., Zhu, S., Yan, X. et al. Willingness to receive the COVID-19 vaccine among HIV positive men who have sex with men in China: a cross-sectional study. BMC Public Health 23, 64 (2023). https://doi.org/10.1186/s12889-022-14961-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-022-14961-5