Abstract
Background
There is a continuing risk for COVID-19 transmission in school settings while transmission is ongoing in the community, particularly among unvaccinated populations. To ensure that schools continue to operate safely and to inform implementation of prevention strategies, it is imperative to gain better understanding of the risk behaviors of staff and students. This secondary analysis describes the prevalence of COVID-19 risk behaviors in an exposed population of students and school staff in the pre-vaccine era and identifies associations between these behaviors and testing positive for SARS-CoV-2.
Methods
From December 2020–January 2021, school staff and students exposed to confirmed COVID-19 cases in a Georgia school district were tested for SARS-CoV-2 and surveyed regarding risk behaviors in and out of school. Prevalence of risk behaviors was described by age group and school level, and associations with SARS-CoV-2 positivity were identified using chi squared tests.
Results
Overall, 717 students and 79 school staff participated in the investigation; SARS-CoV-2 positivity was 9.2%. In the 2 weeks prior to COVID-19 exposure, 24% of participants reported unmasked indoor time at school, 40% attended social gatherings with non-household members, and 71% visited out-of-school indoor locations, including 19% who ate indoors in restaurants. Frequencies of risk behaviors increased by age. Among students, 17% participated in school sports, of whom 86% participated without a mask. SARS-CoV-2 positivity was significantly associated with school sports and unmasked time in sports. Among K-5 students, positivity was associated with exposure to a teacher index case.
Conclusions
This analysis highlights the high prevalence of risk behaviors in an unvaccinated population exposed to COVID-19 in school and identifies an association between student sports participation and SARS-CoV-2 positivity. These findings illustrate the importance of school-level prevention measures to reduce SARS-CoV-2 transmission, including limiting close-contact indoor sports and promoting consistent mask use in unvaccinated individuals. Future research could explore the role of community vaccination programs as a strategy to reduce COVID-19 transmission and introductions into school settings.
Similar content being viewed by others
Background
In March 2020, the COVID-19 pandemic caused widespread closures of schools throughout the U.S., impacting up to 55 million students in 124,000 schools [1, 2]. Studies suggested that these closures may have negatively impacted student learning and the mental health of children and families, [3,4,5] and due to the importance of in-person education for children, families, and communities, many schools reopened for face-to-face instruction in the 2020/2021 academic year [6, 7]. However, due to their potential for high population density and frequency of close contact between students or staff, risks for introductions and transmission within the school setting persist while transmission of SARS-CoV-2 is ongoing in the community, particularly in populations where vaccination remains low [7, 8]. Instances of widespread secondary transmission of SARS-CoV-2 have been documented in school settings when comprehensive prevention strategies are not implemented [9]. To ensure that schools remain open, can continue to operate as safely as possible during the COVID-19 pandemic, and to inform implementation of prevention strategies, better understanding of the risk behaviors of staff and students relevant to in-school transmission is imperative.
Prevention strategies such as mask use and physical distancing have been identified as significant protective factors for reducing SARS-CoV-2 transmission in schools, while risk factors have included close-contact indoor sports, eating meals in close proximity, and attending social gatherings with persons outside the household [10,11,12,13,14]. Similarly, the effectiveness of prevention strategies in the community are well documented, while activities such as dining in restaurants, attending church, and group fitness classes have been identified as risk factors for transmission [15,16,17,18,19,20,21,22,23,24,25]. However, information on the prevalence of risk behaviors among school populations and how these behaviors impact risk of transmission in educational settings is sparse, and few studies have formally assessed the direct relationship between individual behaviors and SARS-CoV-2 transmission in schools. Understanding the extent to which students and school staff engage in risk behaviors may contribute to developing policies and practices that could help to reduce introductions and transmission of SARS-CoV-2 in school settings in order to limit school closures and maximize opportunities for in-person learning.
To describe the extent of transmission of SARS-CoV-2 in schools, the Centers for Disease Control and Prevention (CDC) partnered with the Georgia Department of Health and Cobb & Douglas Public Health to investigate transmission in a Georgia public school district. Results of this investigation showed that teacher-to-teacher and teacher-to-student transmission were a central element of transmission chains in this district [26, 27]. To further inform school and community efforts to reduce SARS-CoV-2 transmission in schools, this secondary analysis utilized data collected during the school transmission investigation to describe the prevalence of risk behaviors relevant for SARS-CoV-2 transmission in this population of unvaccinated students and school staff and to identify associations between these behaviors and testing positive for SARS-CoV-2 in the era prior to widespread vaccination availability.
Methods
Population and Setting
The population under investigation included all 12 public schools in a school district located in the Atlanta metropolitan area in the US. The school district includes approximately 1,400 staff and 8,500 students across one high school (grades 9-12), two middle schools (grades 6-8), eight elementary schools (grades K-5), and one early learning center (pre-K). The period of investigation was December 1, 2020–January 26, 2021, including a 10-day holiday break. Seven-day county incidence of COVID-19 was peaking at this time, with a high of 705 cases per 100,000 on January 13, 2021 [27]. By the end of the investigation period, educational staff and children were still not eligible for COVID-19 vaccination in Georgia, and the state vaccination rate was only 2.6% [28].
During the investigation period, parents or guardians chose whether their children went to school fully online or fully in-person four days per week, with all students attending online on Fridays. All students had the option to participate in school sports in person. In accordance with public health recommendations, [7] the district used a number of measures to reduce the risk of transmission in schools, which are described in detail elsewhere [27]. In brief, these included mandatory mask use indoors and on the school bus, enhanced hand hygiene, three-sided plastic dividers on student desks, and spacing desks further apart. There were exceptions to mandatory mask use during meals, mask breaks (times students could remove their masks for short periods), outdoor recess, and indoor and outdoor physical activity.
Investigation Procedures
During the study period, school staff or students in the school district with confirmed SARS-CoV-2 infection were identified by the health department or self-report and are included here as index cases. School district staff conducted contact tracing to identify all persons who were exposed to an index case in a school setting, defined as being within six feet for a cumulative ≥15 minutes within 24 hours during the infectious period (starting 48 hours prior to the case’s positive test if asymptomatic, or 48 hours prior to symptom onset) [29]. These individuals are referred to as contacts. Methods for contact tracing included interviews with index cases and review of classroom and bus seating charts. This process helped determine characteristics of exposure, including location (e.g., classroom, bus), school role of the index case, and whether the contact was exposed to multiple index cases concurrently [27]. The school district then reported the contact and their characteristics of exposure to the CDC investigation team.
The CDC team called each contact/their guardian to explain the investigation, request verbal informed consent, and offer the contact COVID-19 testing at no cost. To collect additional information on the contact and the context of their in-school exposure, a brief survey was administered over the phone in English, Spanish, or Portuguese. The survey was developed for the purposes of this study in consultation with subject matter experts and included questions on demographics, behaviors in school that might modify their exposure level (e.g., mask use), and a variety of behaviors in and out of school that have previously been identified as high-risk (e.g., dining in restaurants) [10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25]. All behaviors were collected for the two weeks prior to the exposure event in order to best capture any factors that could inform risk in the epidemiologically relevant time period. The survey tool can be found in supplementary materials. Questions were asked directly to the student if they were in high school and the parent consented, otherwise they were asked to the parent with the student present. Responses were entered into Epi Info version 7.2.3.1 (CDC, Atlanta, GA), and testing date was recorded in a call log. If the investigation team was unable to reach the contact, they attempted to call back at least twice.
Drive-through COVID-19 testing was provided two hours per day during December 4–24, 2020, and January 8–26, 2021, for a total of 40 testing days. Appointments for testing were preferentially scheduled five to seven days post-exposure per standard guidelines but could be scheduled up to ten days from last exposure if necessary [30]. At the testing site, adult contacts or guardians provided written informed consent, and the investigation team collected anterior nasal swabs. Samples were placed in a cooler and transported to the Georgia Public Health Laboratory for analysis within three hours of collection. This activity was reviewed by CDC IRB, and was approved to be conducted as a public health activity consistent with applicable federal law and CDC policy, e.g. 45 C.F.R. part 46, 21 C.F.R. part 56; 42 U.S.C. §241(d); 5 U.S.C. §552a; 44 U.S.C. §3501 et seq.
Laboratory Methods
All samples were refrigerated at 2-8°C and were tested within 24 hours of receipt at the Georgia Public Health Laboratory. Viral nucleic acid material was extracted using a PerkinElmer Chemagic 360 platform (PerkinElmer, Waltham, MA). Real-time reverse transcriptase polymerase chain reaction (RT-PCR) testing was conducted using the PerkinElmer New Coronavirus Nucleic Acid Detection Kit on a 7500 Fast Dx Real-Time PCR system (Applied Biosystems, Foster City, CA) for qualitative detection of SARS-CoV-2 nucleic acid. All contacts received RT-PCR results by email within 48 hours of sample collection.
Data Management
Data from call logs, RT-PCR testing, and participant surveys were merged into a master dataset. Participants were included in this analysis if they completed the survey and had complete information on their staff vs. student role and school level (Fig. 1). For analyses involving SARS-CoV-2 positivity, participants were retained if they also had a recorded COVID-19 test from CDC testing or another source within 5-10 days of their in-school exposure. If a previously negative participant had an independent exposure in school more than two weeks after their first exposure and completed an additional survey and test, that participant was included in the dataset separately for each exposure. In the rare instance that a participant was exposed to multiple index cases concurrently, this was counted as a single exposure event in the analysis, but the number of index cases was recorded.
Flowchart of participation among staff and students participating in an investigation on in-school transmission in a school district in Georgia, December 2020–January 2021. Participants were eligible for bivariate comparisons if they had a SARS-CoV-2 test result and the characteristics of their index case were known. Reasons for non-participation marked with an asterisk indicate participant refusal of survey and/or test
Statistical Analyses
Data were analyzed using SAS 9.4 (SAS Institute, Cary, NC) and R 3.6.1 statistical software (The R Foundation). All analyses were stratified by school role and school level, with the three categories defined as staff, elementary school students (grades pre-K–5), and middle/high school students (grades 6–8 and 9–12). Frequencies are presented for demographics, school-reported exposure characteristics (e.g., exposure setting, staff vs. student index case role), and self-reported risk behaviors in and out of school in the two weeks before exposure (e.g., mask use, participation in school sports, visits to non-school indoor locations). Middle/high school students may have reported sports participation as either formal inter-school sports leagues or informal in-school athletics, while elementary school students had only informal in-school athletics. Staff reported participation in sports as a coach or sponsor. For staff, frequencies also are presented for in-school interactions with other staff, including in-person meetings, indoor lunch, other social time, and unmasked time with other staff.
For students, bivariate comparisons were conducted by school level using chi-squared or Fisher’s exact tests to identify associations between SARS-CoV-2 positivity, demographic factors, characteristics of exposure, and self-reported behaviors. Small sample size precluded bivariate comparisons for staff participants, so frequencies were calculated by SARS-CoV-2 test result and are presented in supplementary materials. Multivariate logistic regression was attempted among all variables significant at the P = 0.1 level using stepwise regression and Akaike information criterion optimization methods, [31] however results are not presented in the primary analysis due to small sample sizes and multicollinearity between sports-related significant predictors.
Results
Population and SARS-CoV-2 Positivity
During the investigation period, the school district identified 1,177 eligible contacts from grades K–12 (129 staff, 1,048 students) who were exposed to 90 school-associated index cases (Fig. 1). No in-school exposures were reported from the early learning center (pre-K). A total of 796 (68%) contacts completed the survey. Among these 796, 404 (51%) were male, 363 (46%) were Hispanic or Latino/a, 231 (29%) were non-Hispanic Black, and 178 (22%) were non-Hispanic White (Table 1). Ten percent of survey participants were staff and 90% were students (469 elementary, 121 middle, and 127 high school students); 483 (61%) participants were exposed to a student index case and 296 (37%) to a staff index case. All elementary school students and 94% of middle/high school students reported attending school in person, with 15 middle/high school students attending school only for athletics. Additional characteristics of participants are presented in Table 1.
Detailed reasons for non-participation among the 381 contacts who did not complete the survey are included in Figure S1 in supplementary materials. Where data were available, the people who refused testing were similar to consenting participants by gender, staff vs. student role, and school level. Race/ethnicity differed between these populations; nearly half (49%) of people who refused were non-Hispanic White, 10% were non-Hispanic Black, and 36% were Hispanic or Latino/a compared to 22%, 29% and 46%, respectively, among participants.
Of the 796 surveyed participants, 628 (79%) completed COVID-19 testing (Fig. 1). Of these, 58 tested positive, for a positivity rate of 9.2%. Positivity was 5.9% (4/68) for staff, 9.0% (32/354) for elementary school students, and 10.7% (22/206) for middle/high school students (chi-squared P=0.5). Overall, 199 contacts refused COVID-19 testing (142 refused all participation, 57 refused testing only). The most frequent reason for refusal was the belief that testing was not necessary since the contact was asymptomatic (n=48, 24%). Detailed reasons for why participants refused are presented in Figure S1.
Frequencies of Self-Reported Risk Behaviors in the 14 Days before In-School Exposure to a COVID-19 Case
Staff and students reported several in-school behaviors that could modify their exposure to SARS-CoV-2 or are known to be high risk for SARS-CoV-2 transmission. In the two weeks prior to exposure, 16% of the 796 participants reported participating in sports in school, including 3% (16/469) of elementary school students, 42% (103/248) of middle/high school students, and 11% (9/79) of staff (Table 2). The most frequent sports reported included indoor basketball and wrestling. Nearly half (49%) of participants reported unmasked time at school, including 24% who reported unmasked time indoors (not including meals); 13% reported unmasked time during school sports, which comprised 69% of elementary and 88% of middle/high school students who reported any sports participation. Among staff members, 65% reported indoor time with other staff, including 39% who had in-person meetings, 30% who ate lunch indoors, and 30% who reported other staff social time; 30% of staff reported unmasked time indoors with other staff, but all staff reported always wearing masks during in-person meetings.
Staff and students also reported a range of out-of-school behaviors that have been identified as high risk for SARS-CoV-2 transmission. Four percent of participants reported travel outside of Georgia, including 11% of staff (Table 2, Fig. 2). Over 70% of participants reported visiting non-school indoor locations, including grocery/retail (43%), indoor restaurants (19%), church/religious locations (11%), and gyms (5%). These proportions increased by age group, with staff reporting the highest rates (90%) followed by middle/high school students (71%). Rates of unmasked time in indoor locations were 22% and also increased by age group. Forty percent of participants reported social visits with persons outside their household; 41% of staff reported ≥2 social visits and 24% attended gatherings of ≥6 people, versus 19-25% and 14-19% among students, respectively. Likewise, 51% of staff, 39% of middle/high, and 32% of elementary school students reported unmasked time indoors during social visits.
Associations between SARS-CoV-2 Positivity, Self-Reported Behaviors, and Exposure Characteristics
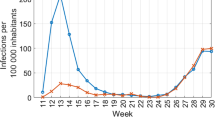
For elementary school students, positivity was 14% (24/172) among students exposed to a staff index case compared with 4% (8/182) if the index case was a student (odds ratio [OR=3.5], 95% confidence interval [CI]=1.5-8.1) (Table 3, Fig. 3). Positivity was 36% (5/14) among students who reported playing sports in school compared with 8% (27/339) among those who did not (OR=6.4, 95% CI=2.0-20.5), and positivity was 44% (4/9) among students who reported any unmasked time playing sports compared to 8% (28/344) among all other students (OR=9.0, 95% CI=2.3-35.5). When restricting this comparison to only the 14 tested students who reported playing sports, positivity remained 44% (4/9) among students who played sports without masks compared to 20% (1/5) among students who always wore a mask during sports.
Associations between SARS-CoV-2 test positivity and participant demographics, school-reported characteristics of exposure, and selected in-school risk behaviors in the 14 days prior to in-school COVID-19 exposure among K–12 students in a school district in Georgia, December 2020–January 2021 (N=560). The dotted line represents an odds ratio of 1, and predictors with 95% confidence intervals that do not cross this line indicate statistical significance at the P=0.05 level
For middle/high school students, positivity was 27% (13/49) among students whose school-reported exposure setting was during sports compared to 6% (8/128) if reported exposure setting was the classroom (OR=5.4, 95% CI=2.1-14.1) or 4% (1/25) if reported exposure setting was on the school bus (OR=8.7, 95% CI=1.1-70.4) (Table 3, Fig. 3). The difference in positivity between exposure on the bus compared to the classroom was not statistically significant. Similarly, positivity was 18% (15/85) among students who reported playing sports in school compared to 6% (7/121) among students who did not (OR=3.5, 95% CI=1.4-9.0), and was 20% (15/74) among students who reported any unmasked time playing sports compared to 6% (7/127) among all other students (OR=4.3, 95% CI=1.7-11.3). When restricting this comparison to only the 85 tested students who reported playing sports, positivity remained 20% (15/74) among students who played sports without masks but was 0% (0/11) among students who always wore a mask during sports. Close-contact indoor sports were the most commonly reported among the 15 SARS-CoV-2 positive sports players, including basketball (53%, 8/15) and wrestling (33%, 5/15). Positivity was also higher among non-Hispanic Black students (18%) compared to non-Hispanic White students (5%) (OR=4.5, 95% CI=1.2-16.9); however, the proportion of Black students was three times higher among students who played sports (74%) than those who did not (26%), so this correlation is likely due to confounding and was not observed in multivariate analyses (Table S1).
There was no association for students of any age between SARS-CoV-2 positivity and gender, taking the school bus, participation in non-sports extracurriculars, general indoor mask use in school, or exposure to multiple cases in school (Table 3). Among elementary school students, there was also no association with race/ethnicity or reported exposure location, and there was no association with staff vs. student index case role for middle/high school students. Frequencies of risk behaviors by test result among staff and results of multivariate analyses are found in the appendices (Tables S1, S2).
Discussion
This analysis builds on a previous investigation of in-school SARS-CoV-2 transmission to examine prevalence of risk behaviors among 717 students and 79 school staff originally identified as contacts of a COVID-19 case in a school setting. High rates of risk behaviors for school and community transmission were reported in this population despite high community incidence and lack of vaccine availability. A large proportion of participants reported unmasked time at school indoors, and most students who participated in sports did not wear masks during these activities. The majority of participants reported visiting indoor locations in the community, and large numbers reported social gatherings with people outside their household, including groups of ≥6 people.
This analysis also identified factors associated with SARS-CoV-2 positivity in this population of unvaccinated staff and students exposed to COVID-19 in school, including self-reported behaviors and school-reported characteristics of exposure. Nearly 10% of participants tested positive for SARS-CoV-2. Across student age groups, the strongest associations with SARS-CoV-2 positivity were with participation in school sports, especially unmasked time in sports, exposure to an index case during sports (middle/high only), and exposure to a staff index case (elementary only).
These results highlight behaviors that might increase or modify the risk of in-school transmission and introductions of SARS-CoV-2 into schools and help to demonstrate the connections between the school environment, in-school behaviors, and out-of-school behaviors. Since people who work in or attend schools are part of the community at-large, risk behaviors out of school could lead to increased opportunities for introductions in school and vice versa when community vaccination is low [8, 32, 33]. For instance, the high proportion of respondents who reported dining indoors at restaurants or having large social gatherings has implications for introductions in the school setting, particularly due to the high level of community transmission in winter of 2020-2021 and unvaccinated status of staff and students [27]. Correspondingly, although in-person education has not consistently been shown to increase community transmission, [8, 34,35,36,37] this investigation and others have found substantial transmission from positive contacts to their families [26, 27, 38, 39].
Few studies have examined behaviors in and out of school among a school population in the pre-vaccine era, which highlights the importance of these data in the literature. In October 2020, 65% of surveyed US middle and high school students reported consistent mask use in classrooms among their peers, and only 28% reported consistent mask use during sports or extracurricular activities [40]. In four studies from May-November 2020, 74-89% of surveyed US adults reported wearing a mask in public, 80-89% tried to keep 6 feet apart, 66-82% avoided restaurants, and 38% avoided socializing with people outside their household, with lower rates in rural areas [22,23,24, 41]. However, it is challenging to directly compare these studies to the current results due to varying study populations and the potential for changes in behavior patterns over the course of the pandemic.
One of the key results from this analysis was the strong association between participation in indoor sports and SARS-CoV-2 positivity. Indoor sports (basketball, wrestling) were the most frequently reported by participants, likely due to the winter sports season, and associations with SARS-CoV-2 positivity were very robust across age groups. Among middle/high school students, this result was consistent between self-reported sports behaviors and the exposure source identified by the school district. This was a surprising result for elementary school students, who do not have formal interscholastic sports leagues and were not generally identified as having predominantly sports-related exposures by the school district; however, the association with self-reported sports participation was very strong despite small sample sizes. This could be explained because, unlike in middle and high school, students in elementary school stay together in a cohort throughout the day including activities like recess, so the school district may have identified the classroom as the predominant exposure location due to the long duration of time in this setting. However, this designation does not preclude additional exposures during other activities. Thereby, although it is not known whether participants played sports directly with the index case, the strong associations between SARS-CoV-2 positivity and self-reported sports participation among this population of children with a known exposure suggests that playing sports unmasked conferred an additional risk to sitting in the classroom.
These findings of potential increased risk associated with sports are consistent with previous reports, which provide a growing body of evidence that there is limited ability to prevent transmission in unvaccinated individuals during high-intensity, close-contact indoor sports [12, 27, 32, 42,43,44]. When community transmission is high, other athletic activities could be considered where comprehensive multilayered prevention strategies can be implemented, including correct and consistent mask use, vaccination of eligible staff and students, adequate physical distancing, avoidance of large crowds, and improved ventilation [7]. Students can thereby continue to experience the physical and mental health benefits of school athletic activities while mitigating the risk to themselves and others [45]. Mask use during sports did appear to be protective in this unvaccinated population, an important finding that could be incorporated into future prevention practices; however, results should be verified with larger studies.
These results also support previous findings that school staff are central to transmission in elementary schools [8, 26, 27, 46, 47]. Close interactions between teachers and younger students are necessary for learning but provide more opportunities for transmission among unvaccinated staff or students, particularly if mask use is not consistent. Despite school policies requiring mask use indoors, our findings and others indicate that these policies may not be followed with 100% fidelity, particularly among younger students [14, 40]. This issue is compounded by the finding that risk behaviors in the community were highest among staff. Interventions to reduce risks of staff-related transmission include vaccination of eligible staff and students, activities to reinforce appropriate mask use, reducing unnecessary in-person interaction among unvaccinated staff, and taking measures to reduce community exposures.
As a final note, the high prevalence of risk behaviors identified in this investigation underscore the importance of comprehensive school, state, and local policies to reduce transmission, in keeping with guidelines to prioritize schools remaining open for in-person instruction over nonessential activities [7]. At the time of the investigation, vaccination was not available to staff or students, and Georgia COVID-19 regulations did not include any universal mask mandate or prohibit dining indoors in restaurants or the operation of indoor gyms and bars, [48] despite demonstrated efficacy in reducing community transmission [15,16,17,18,19]. The frequency of these behaviors in our population are therefore not unexpected given the proximity to holidays, cold winter weather, and ongoing effects of isolation, particularly among staff who may live alone or have responsibilities outside of the home [49, 50]. Similarly, although CDC recommends limiting sports and extracurricular activities when community transmission is high, [7] the Georgia High School Association did not impose restrictions on school sports or require mask use during sports at the time of the investigation [51]. Without this guidance, it may have been challenging for local school boards to independently limit sports or require mask use during athletics. Implementing structural policies at the state or local level during periods of high transmission would likely improve adherence to behavioral recommendations, reduce community acquisition of SARS-CoV-2, and therefore reduce introductions of COVID-19 into schools [16, 52]. Improving vaccination rates among eligible populations may also reduce introductions into schools and in-school transmission. However, until vaccination is available to persons of all ages, continued adherence to in-school prevention measures such as appropriate mask use will continue to be important to prevent in-school transmission.
This investigation had several limitations. Enrollment was limited to known contacts of a positive SARS-CoV-2 case and occurred in a single school district, which constrains generalizability to other populations. Similarly, the investigation occurred prior to widespread vaccine availability, and both behaviors and risk factors have likely shifted since this time. The sample size of SARS-CoV-2 positive participants was also small, which limited the ability to conduct statistical comparisons, and the use of self-reported survey data rather than direct observation of risk behaviors increases the chance of recall bias and social desirability bias. Due to the sampling design of recruiting only people exposed in school, it was not feasible to assess associations between SARS-CoV-2 positivity and out-of-school behaviors due to the risk of selection bias. Furthermore, for all self-reported in-school behaviors, it is not known whether the participant was exposed to the positive case during those activities, so this investigation could only identify associations but cannot determine causality. A sizeable percent of the population also could not be reached or declined participation, with the leading reason for refusals being belief that testing was not needed for asymptomatic contacts. This may indicate that contacts who refused were different than participants regarding behaviors for SARS-CoV-2 prevention. Finally, although SARS-CoV-2 positivity was associated with sports participation, comparisons between individual sports activities or settings could not be conducted due to low sample size and the limited number of sports in season during the investigation. Future studies could attempt to discern which sports activities are associated with the highest risk for transmission.
Despite these limitations, this investigation is one of the more comprehensive reports of school staff and student behaviors relevant to COVID-19 in the literature to date and identifies several characteristics and behaviors associated with probable SARS-CoV-2 transmission in school settings. These findings may be valuable to guide implementation of interventions in and out of schools to improve the safety of staff and student populations. Furthermore, COVID-19 vaccination is still not available for children under 5 years, and vaccination rates remain low in many US counties and internationally. Additional studies are needed to assess the impact of behaviors in school and the community on transmission in school populations, including the role of vaccination status.
Conclusions
The results of this investigation underscore the importance of both in-school prevention measures and individual behaviors for COVID-19 in school settings. In a population of staff and students with an in-school exposure, risk behaviors were common despite high community transmission, and SARS-CoV-2 positivity was associated with several of these behaviors including participation in sports. It is possible that these behaviors may thereby contribute to in-school transmission or introductions of SARS-CoV-2 into the school. To mitigate these risks and maintain the safety of in-person learning, comprehensive school and community prevention measures are needed. These include vaccination of eligible staff and students and measures to reduce transmission in unvaccinated populations including correct and consistent mask use, reduction of high-risk activities such as indoor school sports, and limiting social gatherings outside of school. Future research is also needed to continue to examine the impact of risk behaviors on school transmission where vaccination is widely available.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available to protect the confidentiality of study participants including minor children but are available from the corresponding author upon reasonable request.
Abbreviations
- CDC:
-
Centers for Disease Control and Prevention
- OR:
-
Odds ratio
- CI:
-
Confidence Intervals
References
Number and Enrollment of Public Elementary and Secondary Schools, by School Level, Type, and Charter, Magnet, and Virtual Status: Selected Years, 1990–91 Through 2017–18 [https://nces.ed.gov/programs/digest/d19/tables/dt19_216.20.asp]. Accessed 19 Apr 2021.
Martin EG, Sorensen LC. Protecting the Health of Vulnerable Children and Adolescents During COVID-19–Related K-12 School Closures in the US. JAMA Health Forum. 2020;1(6):e200724.
Verlenden JV, Pampati S, Rasberry CN, Liddon N, Hertz M, Kilmer G, et al. Association of Children's Mode of School Instruction with Child and Parent Experiences and Well-Being During the COVID-19 Pandemic - COVID Experiences Survey, United States, October 8-November 13, 2020. MMWR Morb Mortal Wkly Rep. 2021;70(11):369–76.
Engzell P, Frey A, Verhagen MD. Learning loss due to school closures during the COVID-19 pandemic. Proc Natl Acad Sci U S A. 2021;118(17).
Barnett WS, Jung K. Seven Impacts of the Pandemic on Young Children and their Parents: Initial Findings from NIEER’s December 2020 Preschool Learning Activities Survey. In: In. New Brunswick, NJ: National Institute for Early Education Research; 2021.
COVID-19 impact: school district status—updates for fall 2020 [https://www.mchdata.com/covid19/schoolclosings]. Accessed 19 Apr 2021.
Operational Strategy for K-12 Schools through Phased Prevention [https://www.cdc.gov/coronavirus/2019-ncov/community/schools-childcare/operation-strategy.html]. Accessed 21 May 2021.
Ismail SA, Saliba V, Lopez Bernal J, Ramsay ME, Ladhani SN. SARS-CoV-2 infection and transmission in educational settings: a prospective, cross-sectional analysis of infection clusters and outbreaks in England. Lancet Infect Dis. 2021;21(3):344–53.
Stein-Zamir C, Abramson N, Shoob H, Libal E, Bitan M, Cardash T, et al. A large COVID-19 outbreak in a high school 10 days after schools' reopening, Israel, May 2020. Euro Surveill. 2020;25(29).
Falk A, Benda A, Falk P, Steffen S, Wallace Z, Høeg TB. COVID-19 Cases and Transmission in 17 K-12 Schools - Wood County, Wisconsin, August 31-November 29, 2020. MMWR Morb Mortal Wkly Rep. 2021;70(4):136–40.
Zimmerman KO, Akinboyo IC, Brookhart MA, Boutzoukas AE, McGann K, Smith MJ, Maradiaga Panayotti G, Armstrong SC, Bristow H, Parker D et al: Incidence and Secondary Transmission of SARS-CoV-2 Infections in Schools. 2021:e2020048090.
Atherstone C, Siegel M, Schmitt-Matzen E, Sjoblom S, Jackson J, Blackmore C, et al. SARS-CoV-2 Transmission Associated with High School Wrestling Tournaments - Florida, December 2020-January 2021. MMWR Morb Mortal Wkly Rep. 2021;70(4):141–3.
Hobbs CV, Martin LM, Kim SS, Kirmse BM, Haynie L, McGraw S, et al. Factors Associated with Positive SARS-CoV-2 Test Results in Outpatient Health Facilities and Emergency Departments Among Children and Adolescents Aged <18 Years - Mississippi, September-November 2020. MMWR Morb Mortal Wkly Rep. 2020;69(50):1925–9.
Gillespie DL, Meyers LA, Lachmann M, Redd SC, Zenilman JM. The Experience of 2 Independent Schools With In-Person Learning During the COVID-19 Pandemic. J Sch Health. 2021;91(5):347–55.
Guy GP Jr, Lee FC, Sunshine G, McCord R, Howard-Williams M, Kompaniyets L, et al. Association of State-Issued Mask Mandates and Allowing On-Premises Restaurant Dining with County-Level COVID-19 Case and Death Growth Rates - United States, March 1-December 31, 2020. MMWR Morb Mortal Wkly Rep. 2021;70(10):350–4.
Lyu W, Wehby GL. Community Use Of Face Masks And COVID-19: Evidence From A Natural Experiment Of State Mandates In The US. Health Aff (Millwood). 2020;39(8):1419–25.
Joo H, Miller GF, Sunshine G, Gakh M, Pike J, Havers FP, et al. Decline in COVID-19 Hospitalization Growth Rates Associated with Statewide Mask Mandates - 10 States, March-October 2020. MMWR Morb Mortal Wkly Rep. 2021;70(6):212–6.
Courtemanche C, Garuccio J, Le A, Pinkston J, Yelowitz A. Strong Social Distancing Measures In The United States Reduced The COVID-19 Growth Rate. Health Aff (Millwood). 2020;39(7):1237–46.
Fisher KA, Tenforde MW, Feldstein LR, Lindsell CJ, Shapiro NI, Files DC, et al. Community and Close Contact Exposures Associated with COVID-19 Among Symptomatic Adults ≥18 Years in 11 Outpatient Health Care Facilities - United States, July 2020. MMWR Morb Mortal Wkly Rep. 2020;69(36):1258–64.
Groves LM, Usagawa L, Elm J, Low E, Manuzak A, Quint J, et al. Community Transmission of SARS-CoV-2 at Three Fitness Facilities - Hawaii, June-July 2020. MMWR Morb Mortal Wkly Rep. 2021;70(9):316–20.
Lendacki FR, Teran RA, Gretsch S, Fricchione MJ, Kerins JL. COVID-19 Outbreak Among Attendees of an Exercise Facility - Chicago, Illinois, August-September 2020. MMWR Morb Mortal Wkly Rep. 2021;70(9):321–5.
Hutchins HJ, Wolff B, Leeb R, Ko JY, Odom E, Willey J, et al. COVID-19 Mitigation Behaviors by Age Group - United States, April-June 2020. MMWR Morb Mortal Wkly Rep. 2020;69(43):1584–90.
Callaghan T, Lueck JA, Trujillo KL, Ferdinand AO. Rural and Urban Differences in COVID-19 Prevention Behaviors. J Rural Health. 2021;37(2):287–95.
Czeisler M, Tynan MA, Howard ME, Honeycutt S, Fulmer EB, Kidder DP, et al. Public Attitudes, Behaviors, and Beliefs Related to COVID-19, Stay-at-Home Orders, Nonessential Business Closures, and Public Health Guidance - United States, New York City, and Los Angeles, May 5-12, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(24):751–8.
James A, Eagle L, Phillips C, Hedges DS, Bodenhamer C, Brown R, et al. High COVID-19 Attack Rate Among Attendees at Events at a Church - Arkansas, March 2020. MMWR Morb Mortal Wkly Rep. 2020;69(20):632–5.
Gold JAW, Gettings JR, Kimball A, Franklin R, Rivera G, Morris E, et al. Clusters of SARS-CoV-2 Infection Among Elementary School Educators and Students in One School District - Georgia, December 2020-January 2021. MMWR Morb Mortal Wkly Rep. 2021;70(8):289–92.
Gettings JR, Gold JAW, Kimball A, Forsberg K, Scott C, Uehara A, et al. SARS-CoV-2 transmission in a Georgia school district - United States, December 2020-January 2021. Clin Infect Dis. 2021. https://doi.org/10.1093/cid/ciab332.
COVID Data Tracker [https://covid.cdc.gov/covid-data-tracker/#datatracker-home]. Accessed 26 Apr 2021.
Contact Tracing for COVID-19 [https://www.cdc.gov/coronavirus/2019-ncov/php/contact-tracing/contact-tracing-plan/contact-tracing.html]. Accessed 25 June 2021.
Overview of Testing for SARS-CoV-2 (COVID-19) [https://www.cdc.gov/coronavirus/2019-ncov/hcp/testing-overview.html]. Accessed 19 Apr 2021.
Yamashita T, Yamashita K, Kamimura R. A Stepwise AIC Method for Variable Selection in Linear Regression. Commun Stat – Theory Methods. 2007;36(13):2395–403.
Honein MA, Barrios LC, Brooks JT. Data and Policy to Guide Opening Schools Safely to Limit the Spread of SARS-CoV-2 Infection. JAMA. 2021;325(9):823–4.
Flasche S, Edmunds WJ. The role of schools and school-aged children in SARS-CoV-2 transmission. Lancet Infect Dis. 2021;21(3):298–9.
Harris D, Ziedan E, Hassig S: The Effects of School Reopenings on COVID-19 Hospitalizations. In.: National Center for Research on Education Access and Choice (REACH); 2021.
Auger KA, Shah SS, Richardson T, Hartley D, Hall M, Warniment A, et al. Association Between Statewide School Closure and COVID-19 Incidence and Mortality in the US. JAMA. 2020;324(9):859–70.
Goldhaber D, Imberman SA, Strunk K, Hopkins B, Brown N, Harbatkin E, Kilbride T: To What Extent Does In-Person Schooling Contribute to the Spread of COVID-19? Evidence from Michigan and Washington. In.: CALDER Working Paper No. 247-1220-2; 2020.
Gandini S, Rainisio M, Iannuzzo ML, Bellerba F, Cecconi F, Scorrano L: No evidence of association between schools and SARS-CoV-2 second wave in Italy. In.: [Preprint]. [Accessed April 18, 2021]. Available from https://www.medrxiv.org/content/10.1101/2020.12.16.20248134v2; 2021.
Lessler J, Grabowski MK, Grantz KH, Badillo-Goicoechea E, Metcalf CJE, Lupton-Smith C, et al. Household COVID-19 risk and in-person schooling. Science. 2021;372(6546):1092–7.
Vlachos J, Hertegard E, H BS: The effects of school closures on SARS-CoV-2 among parents and teachers. Proc Natl Acad Sci U S A 2021, 118(9).
Arvelo W, Fahrenbruch M, Hast M, Puddy R. COVID-19 Stats: Percentage of Middle and High School Students Aged 13-21 Years Attending In-Person Classes Who Reported Observing Fellow Students Wearing a Mask All the Time, by School Setting and Activity - United States, October 2020. MMWR Morb Mortal Wkly Rep. 2021;70(6):223.
Crane MA, Shermock KM, Omer SB, Romley JA. Change in Reported Adherence to Nonpharmaceutical Interventions During the COVID-19 Pandemic, April-November 2020. Jama. 2021;325(9):883–5.
Atrubin D, Wiese M, Bohinc B. An Outbreak of COVID-19 Associated with a Recreational Hockey Game - Florida, June 2020. MMWR Morb Mortal Wkly Rep. 2020;69(41):1492–3.
Moreno GK, Braun KM, Pray IW, Segaloff HE, Lim A, Poulson K, Meiman J, Borcher J, Westergaard RP, Moll MK et al: SARS-CoV-2 transmission in intercollegiate athletics not fully mitigated with daily antigen testing. In.: [Preprint]. [Accessed April 18, 2021]. Available from https://www.medrxiv.org/content/10.1101/2021.03.03.21252838v1.full; 2021.
Watson AM, Haraldsdottir K, Biese K, Goodavish L, Stevens B, McGuine T: The Association of COVID-19 Incidence with Sport and Face Mask Use in United States High School Athletes. In.: [Preprint]. [Accessed April 18, 2021]. Available from https://www.medrxiv.org/content/10.1101/2021.01.19.21250116v1; 2021.
McGuine TA, Biese K, Hetzel SJ, Schwarz A, Kliethermes S, Reardon CL, et al. High School Sports During the CoVID-19 Pandemic: The Impact of Sport Participation on the Health of Adolescents. J Athl Train. 2021.https://doi.org/10.4085/1062-6050-0121.21.
Schoeps A, Hoffmann D, Tamm C, Vollmer B, Haag S, Kaffenberger T, Ferguson-Beiser K, Kohlhase-Griebel B, Basenach S, Missal A et al: COVID-19 transmission in educational institutions August to December 2020 in Germany: a study of index cases and close contact cohorts. In.: [Preprint]. [Accessed April 18, 2021]. Available from https://www.medrxiv.org/content/10.1101/2021.02.04.21250670v2.full; 2021.
Varma JK, Thamkittikasem J, Whittemore K, Alexander M, Stephens DH, Arslanian K, Bray J, Long TG. COVID-19 Infections among Students and Staff in New York City Public Schools. Pediatrics. 2021;147(5):e2021050605. Available from https://pediatrics.aappublications.org/content/early/2021/03/05/peds.2021-050605. Accessed 18 Apr 2021.
2020 Executive Orders: 12.30.20.02: Providing additional guidance for Empowering a Healthy Georgia in response to COVID-19. In.: Governor Brian P. Kemp, Office of the Governor; December 31, 2020.
Loades ME, Chatburn E, Higson-Sweeney N, Reynolds S, Shafran R, Brigden A, et al. Rapid Systematic Review: The Impact of Social Isolation and Loneliness on the Mental Health of Children and Adolescents in the Context of COVID-19. J Am Acad Child Adolesc Psychiatry. 2020;59(11):1218–1239 e1213.
Saltzman LY, Hansel TC, Bordnick PS. Loneliness, isolation, and social support factors in post-COVID-19 mental health. Psychol Trauma. 2020;12(S1):S55–7.
Latest GHSA Statements on Coronavirus Situation [https://www.ghsa.net/latest-ghsa-statements-coronavirus-situation]. Accessed 19 Apr 2021.
Betsch C, Korn L, Sprengholz P, Felgendreff L, Eitze S, Schmid P, et al. Social and behavioral consequences of mask policies during the COVID-19 pandemic. Proc Natl Acad Sci U S A. 2020;117(36):21851–3.
Acknowledgements
We would like to thank the students, families, and school staff who participated in this investigation, principals and administrators at Marietta City Schools, the Georgia Public Health Laboratory, the CDC COVID-19 epidemiology task force, and the COVID-19 Georgia K–12 school team, including Abirami Balajee, CDC; Rebecca J. Chancey, CDC; Deanna Crosby, CDPH; Morgane Donadel, CDC; Cherie Drenzek, GDPH; Catherine Espinosa, CDC; Mary E. Evans, CDC; Katherine Fleming-Dutra, CDC; Catalina Forero, CDC; Kaitlin Forsberg , CDC; Jenna R. Gettings, CDC; Jeremy A. W. Gold, CDC; Esther Kukielka, CDC; Janet Memark, CDPH; Kiren Mitruka, CDC; Sam Moeller, GDPH; Jasmine Y. Nakayama, CDC; Yoshinori Nakazawa, CDC; Michelle O'Hegarty, CDC; Caroline Pratt, CDC; Marion E. Rice, Katelin Reishus, GDPH; Grand Rivera, MCS; CDC; Gurleen Roberts, CDPH; Roxana Rodriguez Stewart, CDC; Raquel Sabogal, CDC; Emanny Sanchez, CDC; Ebony S. Thomas, GDPH; Katerine Topf, GDPH; Snigdha Vallabhaneni, CDC; Andres Velasco-Villa, CDC; Mark K. Weng, CDC
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official positions of Cobb & Douglas Public Health, Georgia Department of Public Health, or the Centers for Disease Control and Prevention.
Funding
None, all work done within routine duties for all authors
Author information
Authors and Affiliations
Contributions
Conceptualization and design of the study: MH, MS, CS, LM, JM, RF, JET, HLK, EM; methods development: MH, MS, CS, DM, LM, JM, RF, EM; data collection: MH, MS, CS, EO, CE, EB, EAK, MER, EM; data management and analysis: MH, MS, EA, EAK, EB; lab analysis: DM; writing: MH, MS, CS, CE, MER, DM, EM; supervision/oversight: MH, MS, JET, HLK, EM. All authors read, provided feedback on, and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This activity was reviewed by the CDC IRB, and was approved to be conducted as a public health activity consistent with applicable federal law and CDC policy, e.g. 45 C.F.R. part 46, 21 C.F.R. part 56; 42 U.S.C. §241(d); 5 U.S.C. §552a; 44 U.S.C. §3501 et seq. Written informed consent was collected from all participants or the guardians of minor children, and verbal informed assent was provided from all participants including minor children.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hast, M., Swanson, M., Scott, C. et al. Prevalence of risk behaviors and correlates of SARS-CoV-2 positivity among in-school contacts of confirmed cases in a Georgia school district in the pre-vaccine era, December 2020–January 2021. BMC Public Health 22, 101 (2022). https://doi.org/10.1186/s12889-021-12347-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-021-12347-7