Abstract
Since the beginning of the pandemic, there has been a great deal of controversy regarding the role of schools in the spread of SARS-CoV-2 infection, and the relative contribution of students, teachers, and others. To quantify the clustering effect of SARS-CoV-2 infection within classes and schools considering the seroprevalence of specific antibodies among students and school staff (teachers and non-teachers) evaluated in schools located in the Northern region of Portugal. 1517 individuals (1307 students and 210 school staff) from 4 public and 2 private schools, comprising daycare to secondary levels, were evaluated. A rapid point-of-care test for SARS-CoV-2 specific IgM and IgG antibodies was performed and a questionnaire was completed providing sociodemographic and clinical information. We calculated the seroprevalence of IgM and IgG antibodies and estimated the Median Odds Ratio (OR) and 95% confidence interval (CI) to assess the clustering effect, using a multilevel (school and class) logistic regression. SARS-CoV-2 seroprevalence (IgM or IgG) was 21.8% and 23.8% (p = 0.575) in students and school staff, respectively. A total of 84 (8.6%) students and 35 (16.7%) school staff reported a previous molecular diagnosis. Among students, those who reported high-risk contacts only at school (OR = 1.13; 95% CI 0.72–1.78) had a seroprevalence similar to those without high-risk contacts; however, seroprevalence was significantly higher among those who only reported a high-risk contact outside the school (OR = 6.56; 95% CI 3.68–11.72), or in both places (OR = 7.83; 95% CI 5.14–11.93). Similar associations were found for school staff. The median OR was 1.00 (95% CI 1.00, 1.38) at the school-level and 1.78 (95% CI 1.40, 2.06) at the class-level. SARS-CoV-2 seroprevalence was similar between students and staff, without a clustering effect observed at the school level, and only a moderate clustering effect documented within classes. These results indicate that the mitigation measures in the school environment can prevent the spread of class outbreaks to the remaining school community.
Similar content being viewed by others
Introduction
Since the identification of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in December 20191, most countries implemented measures of school closure. This involved nationwide or regional closures and total or partial closure of schools (in which schools were either closed for some grade levels or were working with restricted capacity). In March 2020, the United Nations Educational, Scientific and Cultural Organization estimated that more than 100 countries had implemented national school closures2, and in April 2020, more than 90% of the students worldwide were in remote learning3.
The rationale for school closures followed evidence from the influenza outbreaks where the reduction of social contact between students led to a reduction of the transmissibility index4. It was assumed that this holds for SARS-CoV-2. However, school closures can be accompanied by increased social mixing of children and adults and among children from different schools5, which might undermine the expected effects. In addition, school closures—particularly if prolonged—widen inequalities, disproportionately affecting socially disadvantaged children and adolescents. These groups are less likely to have access to digital technologies required for remote learning, to healthy and nutritious food choices, and are more likely to be exposed to social (e.g. violence) and environmental hazards (e.g. overcrowding) in the residential environment2, 6. So, given the possible deleterious effects of school closures, we must understand the extent of transmission in the school environment.
In fact, in the case of SARS-CoV-2 infection, the role of schools in the spreading of the infection remains controversial7, with some studies indicating substantial increases in case rates associated with school openings8, while others document a small impact9. Additionally, a nationwide, population-based seroepidemiological study conducted between February and March 2021 in Portugal showed that seroprevalence in children and adolescents was similar to that of persons aged between 20 and 69 years, suggesting a similar risk of infection10. In addition, several tracing studies within education settings identified only a few outbreaks11, 12.
Currently, available data did not quantify the magnitude of the effect of children-to-children transmission within classrooms and schools (the so-called cluster effects). The detection of clustering at the school or classroom would indicate that the school setting is important in understanding individual differences in infection. Therefore, this knowledge may help public health authorities to direct their efforts toward specific classrooms and schools. If no clustering is identified, this suggests that mitigation measures should be targeted at individuals, families, and social networks outside the school community.
In this study, we aimed to quantify the seroprevalence of specific antibodies to SARS-CoV-2 among students and school staff in six schools located in the Northern region of Portugal and to quantify the clustering effect of SARS-CoV-2 within classes and schools.
Methods
Setting and participants
The study protocol was approved by the ethics committee of the Institute of Public Health of the University of Porto (ID 20154). Participation was voluntary and written informed consent was given by the participants, or the respective legal guardian in case of those aged less than 16. All methods were carried out in accordance with relevant guidelines and regulations.
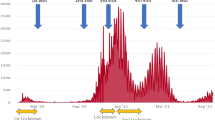
In the study conducted from March to April 2021, we invited a total of six schools (four public schools and two private schools) located in two municipalities of the Porto Metropolitan Area (Santa Maria da Feira and Paredes) to participate, using quota sampling. These two municipalities were selected because they both belong to the Porto Metropolitan Area—the second largest metropolitan area of the country and one of the Portuguese regions most affected by the epidemic—and presented high incidence rates of SARS-CoV-2 as depicted in the map from Fig. 1.
All students and school staff (teachers and non-teachers) of 84 classes from the six schools were offered a serological point-of-care test for SARS-CoV-2 specific IgM and IgG antibodies between March 25 and April 9, 2021 (Fig. 1). The study was conducted prior to the vaccination of both students and school staff.
From a total of 1617 students and 253 school staff, 1307 (81%) and 210 (83%), respectively, accepted to participate and had valid tests. The students’ age ranged from 0 to 18 years old and the ages of the school staff ranged from 22 to 65 years old. Participants’ characteristics are presented in Table 1.
Questionnaire
A questionnaire was completed as part of the testing procedure. Each participant was given an ID, and on the day of the testing or the previous day, the participants, if 12 or older, or their legal guardian, were invited by email to complete an online questionnaire addressing clinical aspects of SARS-CoV-2 infection and sociodemographic characteristics. The questionnaire included information on SARS-CoV-2 cases among cohabitants (parents, grandparents, children, siblings, others), and non-cohabitants and type of relationship (namely, family or friend, a colleague at school, student, teacher, other school workers); having been quarantined since beginning 2020; symptoms since the beginning of 2020 (abdominal pain, anosmia, arthralgia, asthenia, chest pain, cough, diarrhea, dysgeusia, fever, headache, myalgia, nausea, rhinorrhea, shortness of breath, sore throat); previous SARS-CoV-2 testing and diagnosis; and COVID-19 vaccination. The sociodemographic section inquired about sex, age, educational level, professional category (in the case of school staff), and number of cohabitants aged less than 10 years, between 10 and 19 years, 20 and 69 years, and aged 70 years or more.
The questionnaire used in this study was adapted from a previous version applied to university students and workers13, 14. To ensure its appropriateness for assessing SAR-CoV-2 symptoms, experts in infectious diseases, such as medical professionals and researchers, evaluated its content validity and face validity.
The classes were re-coded into: Daycare [1–2 years old], Preschool [3–6 years old], first cycle [1–4 years school], second cycle [5–6 years school], third cycle [7–9] and secondary [10–12 years school].
The information about known high-risk contact with SARS-CoV-2 cases was categorized into the following four categories: no contact, contact inside school only, outside school only, and at both settings.
Seroprevalence of SARS-CoV-2 specific antibodies
To determine the presence of SARS-CoV-2 specific IgM and IgG antibodies the STANDARD Q COVID-19 IgM/IgG Combo (reported sensitivity of 94.5% based on samples obtained 7 or more days after symptoms onset and specificity of 95.7% for both IgG and IgM) was performed according to manufacturer instructions by trained researchers.
Statistical analysis
The seroprevalence was computed as the proportion of individuals with a reactive result in the IgM or IgG band. We compared proportions using the Pearson Chi-Square or the Fisher exact test when the assumptions for the Chi-Square test did not hold. P-values lower than 0.05 were considered statistically significant.
The map from Fig. 1 was generated using the software ArcGIS Pro version 2.3.0. ArcGIS Pro is a Geographic Information System (GIS) platform developed by Esri, used for creating, analyzing, and visualizing geospatial data (For more information about ArcGIS Pro 2.3.0, you can visit the following link: https://www.esri.com/en-us/arcgis/about-arcgis/overview).
The adjusted odds ratios (aOR) were used to estimate the association between having a reactive IgM or IgG test result and known high-risk contact with confirmed cases, after accounting for sex, age, and presence of symptoms (any of the listed). The aOR and respective 95% confidence intervals were estimated using unconditional logistic regression.
Multilevel mixed-effects logistic regression was fitted with a random effect at the class- and school-level. Multilevel mixed-effects logistic regression is a statistical model that is specifically designed to analyze binary data with a nested structure. In this framework, the data is organized in a way that students are nested within higher-level units (e.g., classes and schools). This type of regression model allows for the examination of both within-group (individual) and between-group (class and school) effects. The inclusion of random effects at the class and school levels in the regression model allows us to account for the potential clustering of observations within the same class or school. In other words, students within the same class or school may be more alike than students in other classes or schools. The random effects allow for the estimation of the variability or heterogeneity between classes and schools.
Crude and adjusted median odds ratio (MOR) and the corresponding bootstrap 95% CI were calculated to quantify the magnitude of the clustering effect at the class- and school-level. The clustering effect, and the MOR, quantify the variation between clusters (second-level variation—classes, third-level—schools) by comparing two individuals from two randomly chosen clusters. When the MOR is equal to one, it means there are no differences between classrooms or between schools. The MOR can be conceptualized as the increased risk that (in median) one would have if moving to another class/school with a higher risk15. Multilevel models were adjusted for age, sex, presence of symptoms (any of the asked symptoms), and known high-risk contact with confirmed cases.
Data sharing
Data and statistical analyses code can be obtained upon request from other researchers. Requests should be sent to the first author Milton Severo (milton@ispup.up.pt).
Results
Among the 1517 participants, 86 (6.6%) out of the 1307 students and 31 (14.8%) out of the 210 school staff members were reactive for IgM. For IgG, 275 (21.0%) students and 38 (18.1%) school staff members were reactive, and 285 (21.8%) students and 50 school staff members (23.8%) were reactive for either IgM or IgG (Table 1). Previous diagnosis of SARS-CoV-2 infection was higher among school staff (16.7%) compared to students (8.6%). On the same note, over half of the students had never been tested for SARS-CoV-2 compared to 28.6% among school staff (Table 1).
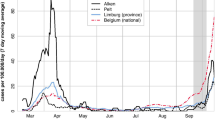
In general, students had a prevalence of any symptoms since the beginning of 2020 of 48.4%, while in school staff it was 65.2%. Figure 2 presents the prevalence of different symptoms since January 2020, according to the results for IgM and IgG. The presence of symptoms was higher among students with a reactive result (56.4%) compared to those with a non-reactive status (46.1%). This difference was larger among school staff (80.0% compared to 60.6%). Similar results were found for the presence of dysgeusia, anosmia, myalgia, fever, and cough.
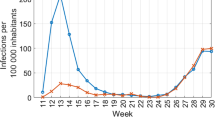
Figure 3 presents the adjusted association between having had high-risk contacts and IgM or IgG reactive status for students and school staff separately. Having had high-risk contacts inside the school only was not significantly associated with having a reactive IgM or IgG test in students (OR = 1.10; 95% CI 0.70, 1.74) and school staff (OR = 0.76; 95% CI 0.29, 1.98), while having high-risk contacts outside school only was strongly associated with having a reactive IgM or IgG test in students (OR = 6.91; 95% CI 3.73, 12.82) and school staff (OR = 9.15; 95% CI 2.04, 40.93). A similarly strong positive association was found for having high-risk contacts both inside and outside schools for both groups (students: OR = 7.30; 95% CI 4.74, 11.34; school staff: OR = 5.18; 95% CI 1.9, 14.64). There was no association with sex or age in both strata. Reporting symptoms was positively associated with being reactive (OR = 2.36; 95% CI 1.07, 5.61) among school staff, while among students no association was observed (OR = 1.24; 95% CI 0.88, 1.73).
Figure 4 shows the seroprevalence in students within each class and school from the two municipalities. The median prevalence and interquartile range was very similar between schools, and one to two classes showed extreme values of prevalence in each school (values higher than 40% of seroprevalence within classes). From a total of 84 classes, eight (9.5%) had more than 40% of students with reactive results. The median odds ratio at the school-level was estimated at 1.00 (95% CI 1.00, 1.39) and 1.78 (95% CI 1.40, 2.06) at class-level. After adjusting for sex, age, being symptomatic, and high-risk contact (outside, inside school, or both) the median odds ratio at the school-level was estimated at 1.00 (95% CI 1.00, 1.92) and 2.20 (95% CI 1.66, 2.66) at the class-level.
Discussion
Our study is the first that quantified the seroprevalence of specific antibodies to SARS-CoV-2 among students and school staff to assess the magnitude of the clustering effect of cases within schools and classes. The risk of infection was estimated to be 2 times higher within some classes compared to others, showing a clustering effect at class-level. This result was independent of sex, age, presence of symptoms, and high-risk contact (outside, inside school, or both), and schools. A similar study in school children in Switzerland16 at an earlier phase of the pandemic (July 2020) showed no significant clustering effect within classes. In this study, most classes had only a single seropositive child among the tested children. The main reason for this difference may be that the prevalence in Switzerland was very low in that phase of the pandemic (2.8%). In our study, approximately 10% of classes had more than 40% of students with reactive results, with as much as 14 reactive in 20 students in the class.
By April 2021, one-fifth of school students and staff had evidence of prior infection based on antibody seropositivity. These estimates were close to those reported in Northern France17, but lower than those found in England18, with approximately one-third of students and staff, or in the Czech Republic19, where almost half of the secondary students had detectable antibodies on a similar timeframe. On the other hand, our estimates were higher than those reported in Montreal, Canada20 (circa 6%) and Indiana, USA21(circa 3%). However, these studies were conducted at different time periods than ours, which limits our capacity to establish direct comparisons. Additionally, the SARS-CoV-2 epidemic waves occurred at different times in each country; therefore, the seropositivity of the population could differ even if the studies were conducted at the same time.
Our results suggest that, under circumstances of careful control of contacts and hygiene measures, the school setting play a small role in SARS-CoV-2 transmission as evidenced by the absence of a clustering effect at the school-level. The schools in our study implemented specific control measures for SARS-CoV-2, such as not mixing students from different classes. This approach could potentially explain why we did not observe significant school-level effects.
Supporting the same idea, a study conducted in 2021 in the UK, found that SARS-CoV-2 infections and outbreaks were uncommon in educational settings and that COVID-19 school incidence mirrored the incidence observed at the regional and community-level22.
Also, the fact that seroprevalence was 7 to 9 times higher (students and school staff, respectively) when the high-risk contact occurred outside the school only (versus 1.1 times higher when the contact occurred inside the school only) supports the idea that educational settings play a small role in SARS-CoV-2 dissemination. Even when individuals had both types of contact, the odds ratio was like that observed amongst those with high-risk contacts outside school only. Our result is similar to the one found in Milan, where no differences were found in the seroconversion rate between students who attended school compared to those who started remote learning, with 61% of students diagnosed with the infection reporting that the contact occurred within the household23.
Seroprevalence was similar between students and school staff, and the ratio between seroprevalence and the diagnosed cases was between 1.5 and 2.0, respectively for school staff and students. Even compared to the age-specific incidence in the municipalities (ranged from 7.2 to 11.1%) where schools were located as reported by the National Surveillance System, this ratio was between 2 and 3, which was lower than what was found in a previous study in three Portuguese public higher education schools13, and in the first national serological survey (ISNCOVID-19) where the ratio was approximately 5–6 times higher24. A possible explanation is that there was an increase in the availability of diagnostic tests and improved screening compared to the initial phase of the pandemic. This could account for the lower ratio between seroprevalence and diagnosed cases.
While we were able to evaluate over 80 classes, the inclusion of only 6 schools could have limited the capacity for detection of a school clustering effect. Nevertheless, our criteria to select the municipalities—having high incidence and belonging to Porto Metropolitan Area—increased the power of the study to detect clustering effects. Besides, the high participation rate in the study, higher than 80%, and the fact that the sample was assembled before the vaccination of school staff and students increases the relevance of the results and their strength. Finally, we did not explore the factors—e.g., class size, socioeconomic characteristics of the participants, room conditions such as ventilation, mask use25, sun exposure, physical distancing26, and hygiene—behind the clustering effect observed at the class level, which could give important insights on the additional measures that need to be implemented to prevent outbreaks within particular classrooms.
Another potential limitation is the presence of bias in reporting symptoms or high-risk contacts. In the case of young children, they may not recall whether they experienced symptoms during the study assessment period. However, efforts were made to mitigate this bias by collecting information from their legal guardians, predominantly parents. Additionally, it is possible that students and school staff were more aware of high-risk situations outside of school, primarily at home, which could explain the stronger association found when high-risk contacts occurred outside of school. Nevertheless, when considering the clustering effect (MOR) at the class and school level, this bias is less likely and the risk appears to be significantly smaller, confirming that schools provided a safer environment.
The observation that the schools may play a small role in SARS-CoV-2 transmission is relevant information to accurately ponder the pros and cons of school openings and to determine the most effective measures to mitigate transmission in schools and classrooms. However, the clustering effect found at the class level poses additional challenges to reduce the risk of infection among students, staff, and particularly to the community. For that, and although we cannot directly infer it from our study, measures such as improved ventilation, stricter hygiene protocols, vaccination promotion, and screening testing, among others27, might help to reduce within-class SARS-CoV-2 transmission.
In conclusion, there was a clustering effect within the classes but not within the school setting and the seroprevalence was much higher among individuals who had high-risk contacts outside school than among individuals who had high-risk contacts inside the school setting. Such findings indicate that it was possible to prevent the spread of outbreaks within classes to the rest of the school community.
References
Zhu, N. et al. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 382(8), 727–733 (2020).
UNESCO. Adverse consequences of school closures 2021. Available from: https://en.unesco.org/covid19/educationresponse/consequences.
Viner, R. M. et al. School closure and management practices during coronavirus outbreaks including COVID-19: A rapid systematic review. Lancet Child Adolesc. Health 4(5), 397–404 (2020).
Jackson, C., Vynnycky, E. & Mangtani, P. The relationship between school holidays and transmission of influenza in England and wales. Am. J. Epidemiol. 184(9), 644–651 (2016).
Eames, K. T., Tilston, N. L. & Edmunds, W. J. The impact of school holidays on the social mixing patterns of school children. Epidemics 3(2), 103–108 (2011).
Van Lancker, W. & Parolin, Z. COVID-19, school closures, and child poverty: A social crisis in the making. Lancet Public Health 5(5), e243–e244 (2020).
Ertem, Z. et al. The impact of school opening model on SARS-CoV-2 community incidence and mortality. Nat. Med. 27, 2120–2126 (2021).
Courtemanche, C. J., Le, A. H., Yelowitz, A. & Zimmer, R. School Reopenings, Mobility, and COVID-19 Spread: Evidence from Texas (National Bureau of Economic Research, 2021).
Bravata, D., Cantor, J. H., Sood, N. & Whaley, C. M. Back to School: The Effect of School Visits During COVID-19 on COVID-19 Transmission (National Bureau of Economic Research, 2021).
Lai, C. C., Wang, J. H. & Hsueh, P. R. Population-based seroprevalence surveys of anti-SARS-CoV-2 antibody: An up-to-date review. Int. J. Infect Dis. 101, 314–322 (2020).
Macartney, K. et al. Transmission of SARS-CoV-2 in Australian educational settings: A prospective cohort study. Lancet Child Adolesc. Health 4(11), 807–816 (2020).
Brandal, L. T. et al. Minimal transmission of SARS-CoV-2 from paediatric COVID-19 cases in primary schools, Norway, August to November 2020. Euro Surveill. 26(1), 2002011 (2021).
Meireles, P. et al. Prevalence of SARS-CoV-2 antibodies among workers of the public higher education institutions of Porto, Portugal: A cross-sectional study. Occup. Environ. Med. 78(9), 648–53 (2021).
Meireles, P. et al. The SARS-CoV-2 infection among students in the University of Porto: A cross-sectional study. Int. J. Public Health 67, 1604548 (2022).
Larsen, K. & Merlo, J. Appropriate assessment of neighborhood effects on individual health: Integrating random and fixed effects in multilevel logistic regression. Am. J. Epidemiol. 161(1), 81–88 (2005).
Ulyte, A. et al. Variation in SARS-CoV-2 seroprevalence across districts, schools and classes: baseline measurements from a cohort of primary and secondary school children in Switzerland. BMJ Open 11(7), e047483 (2021).
Fontanet, A. et al. SARS-CoV-2 infection in schools in a northern French city: A retrospective serological cohort study in an area of high transmission, France, January to April 2020. Eurosurveillance 26(15), 2001695 (2021).
Ladhani, S. N. et al. Emergence of SARS-CoV-2 Alpha (B.1.1.7) variant, infection rates, antibody seroconversion and seroprevalence rates in secondary school students and staff: Active prospective surveillance, December 2020 to March 2021, England. J. Infect. 83, 573–580 (2021).
Fejt, V., Kratka, Z., Zelena, H. & Komarek, A. What is the immunity of high school students to coronavirus?. Cas Lek Cesk 160(4), 133–138 (2021).
Zinszer, K. et al. Seroprevalence of SARS-CoV-2 antibodies among children in school and day care in Montreal, Canada. JAMA Netw. Open 4(11), e2135975 (2021).
Lopez, L. et al. Seroprevalence of anti-SARS-CoV-2 IgG antibodies in the staff of a public school system in the midwestern United States. PLOS ONE 16(6), e0243676 (2021).
Ismail, S. A., Saliba, V., Bernal, J. L., Ramsay, M. E. & Ladhani, S. N. SARS-CoV-2 infection and transmission in educational settings: A prospective, cross-sectional analysis of infection clusters and outbreaks in England. Lancet Infect. Dis 21(3), 344–353 (2021).
Barcellini, L. et al. Does school reopening affect SARS-CoV-2 seroprevalence among school-age children in Milan?. PLOS ONE 16(9), e0257046 (2021).
Kislaya, I. et al. Seroprevalence of SARS-CoV-2 infection in Portugal in May–July 2020: Results of the First National Serological Survey (ISNCOVID-19). Acta Med Port. 34(2), 87–94 (2021).
Ma, X., Luo, X. F., Li, L., Li, Y. & Sun, G. Q. The influence of mask use on the spread of COVID-19 during pandemic in New York City. Results Phys. 34, 105224 (2022).
Asamoah, J. K. K. et al. Optimal control and comprehensive cost-effectiveness analysis for COVID-19. Results Phys. 33, 105177 (2022).
For Immunization NC. Science Brief: Transmission of SARS-CoV-2 in K-12 Schools and Early Care and Education Programs–Updated. CDC COVID-19 Science Briefs [Internet]: Centers for Disease Control and Prevention (US); 2021.
Funding
This work was funded by national funds through FCT—Fundação para a Ciência e Tecnologia, I.P., under the Projects UIDB/04750/2020 and LA/P/0064/2020. AIR was supported by National Funds through FCT, under the “Stimulus of Scientific Employment—Individual Support” program within the contract CEECIND/02386/2018.
Author information
Authors and Affiliations
Contributions
M.S., P.M., V.M. and H.B. designed the study and wrote the research protocol. M.S. analyzed the data and wrote the first the draft of the manuscript. P.M. and V.M. managed participants and collected the data. A.I.R. collaborated with the data analysis. H.B. coordinated the study. All authors revised the manuscript for important intellectual content, read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Severo, M., Meireles, P., Ribeiro, A.I. et al. Measuring the clustering effect of the SARS-CoV-2 transmission in a school population: a cross-sectional study in a high incidence region. Sci Rep 13, 16300 (2023). https://doi.org/10.1038/s41598-023-42470-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-42470-x
- Springer Nature Limited