Abstract
Background
Understanding the impact of food insecurity on HIV outcomes is critical for the development and implementation of effective, evidence-based interventions to address food insecurity and improve the HIV care cascade. We conducted a prospective, longitudinal study to determine the impact of food insecurity on HIV outcomes in Senegal, West Africa.
Methods
HIV-infected individuals presenting for care and initiation of ART through the Senegalese National AIDS program in Dakar and Ziguinchor were eligible for enrollment. Data were collected using interviews, clinical evaluations, laboratory analyses, and chart review at enrollment, month 6, and month 12. Logistic regression was used to determine the association between food insecurity and HIV outcomes.
Results
Among the 207 participants in this study, 70% were female and the median age was 37 years. The majority (69%) were food insecure at enrollment, 29% were severely food insecure, and 38% were undernourished. Nearly a third (32%) had no formal education, 23% practiced agriculture, and 40% owned livestock. The median daily food expenditure per person was $0.58. The median round trip transportation time to clinic was 90 min (IQR 30–240). The median cost of transportation to clinic was $1.74. At month 12, 69% were food insecure, 23% were severely food insecure, and 14% were undernourished. At month 12, 43% had not disclosed their HIV status; food insecurity was associated with non-disclosure of HIV-status due to fear of stigmatization and feelings of shame. Severe food insecurity was a strong predictor of loss to follow-up (OR 3.13 [1.08–9.06]) and persistent severe food insecurity was associated with virologic failure (OR 5.14 [1.01–26.29]) and poor adherence to ART 8.00 [1.11–57.57]. Poor nutritional status was associated with poor immunologic recovery (OR 4.24 [1.56–11.47]), virologic failure (OR 3.39 [1.13–10.21]), and death (OR 3.35 [1.40–8.03]).
Conclusion
Severity and duration of food insecurity are important factors in understanding the relationship between food insecurity and HIV outcomes. Our findings highlight the importance of nutritional status, socioeconomic opportunity, and self-stigmatization in the complex pathway between food insecurity and HIV outcomes. Interdisciplinary, multisectoral efforts are needed to develop and implement effective interventions to address food insecurity among people living with HIV.
Similar content being viewed by others
Background
Food security exists when people have consistent physical, social and economic access to sufficient, safe and nutritious food that meets their dietary needs and food preferences for an active and healthy life [1]. According to the United Nations Food and Agriculture Program, food insecurity is increasing globally, driven primarily by climate change, conflict, economic downturns, and more recently, the COVID-19 pandemic [1].
Sub-Saharan Africa (SSA) is disproportionately affected by both food insecurity and HIV. It is home to nearly a third of the 2 billion people worldwide who are moderately or severely food insecure and two-thirds of the 38 million people living with HIV (PLHIV) [1, 2]. Although PLHIV are particularly vulnerable to the negative consequences of food insecurity [3,4,5,6,7,8], prospective longitudinal studies to evaluate the associations between food insecurity and HIV outcomes in SSA are limited. Findings from predominantly cross-sectional studies have shown that food insecurity is associated with poor adherence to antiretroviral therapy (ART) among PLHIV in SSA [9,10,11,12,13,14,15,16,17,18,19] and one study conducted in SSA reported an association between food insecurity and lower CD4 cell counts [12, 20]. To our knowledge there has been only one prospective, longitudinal study to determine the association between food insecurity and virologic failure in SSA [12] and there have been no longitudinal studies to evaluate the association between food insecurity and mortality or loss to follow-up (LTFU) among PLHIV in SSA.
Our previous work has shown that the majority of PLHIV in Senegal, West Africa are food insecure [21,22,23]. Here we report the results of a prospective, longitudinal study to determine the impact of food insecurity on HIV outcomes in Senegal. Understanding the impact of food insecurity on HIV outcomes, and elucidating the mechanisms by which food insecurity impacts PLHIV in SSA, is critical for the development and implementation of effective, evidence-based interventions to address food insecurity and improve the HIV care cascade.
Methods
All HIV-infected individuals presenting for care and initiation of ART through the Senegalese National AIDS program (ISAARV) at the Clinique des Maladies Infectieuses, Centre Hospitalier National Universitaire de Fann, located in Dakar, and the Centre de Santé de Ziguinchor, located in the Casamance Region, were eligible for enrollment. Informed consent was conducted by the social worker. For participants < 18 years of age, consent was obtained from their legal guardian. Study procedures were approved by the University of Washington Institutional Review Board and the Senegal Comité National d’Ethique pour la Recherche en Santé.
Enrollment took place from April 2017 to April 2018. Data were collected using semi-structured interviews, clinical evaluations, laboratory analyses, and chart review at enrollment, month 6 (M6) and month 12 (M12) (Supplementary file 1). Food insecurity was determined using the Household Food Insecurity Access Scale (HFIAS) [24]. Not food insecure was defined as a HFIAS score of 1 on a scale of 1–4, food insecure was defined as a HFIAS score of 2–4, mildly food insecure was defined as a HFIAS score of 2, moderately food insecure was defined as a HFIAS score of 3, and severely food insecure was defined as a HFIAS score of 4.
HIV-1, HIV-2, and dually infected individuals were enrolled. HIV type was determined using SD Bioline HIV-1/2 3.0 (Alere). Clinical evaluations were performed to determine WHO clinical stage [25]. Nutritional status was determined using body mass index (BMI) and mid-upper arm circumference (MUAC). Undernourished was defined as a BMI < 18.5 kg/m2 for non-pregnant participants ≥18 years of age or BMI for age < − 2 z-scores below the median of the WHO Child Growth Standard for participants < 18 years of age [26]. For pregnant women, undernourished was defined as MUAC < 230 mm [27]. For the purposes of this study, the terms undernourishment and undernutrition were used interchangeably. CD4 cell count was measured at enrollment, M6, and M12 using the BD FACSCount system (Becton Dickinson) or the PIMA analyser (Alere).
ART adherence was measured at M6 and M12. Participants were asked by the physician how many times in the past 7 days they failed to take one or more doses of ART, how many times in the past 7 days they failed to take all of their doses of ART, how many times in the past 4 weeks they failed to take one or more doses of ART, and how many times in the past 4 weeks they failed to take all of their doses of ART. They were also asked by both the social worker and the physician if they were always adherent to their ART, not always adherent to their ART, or not adherent to their ART. Those who responded that they were not adherent or not always adherent were classified as poorly adherent. Because more individuals reported poor adherence to ART when asked by the social worker and because this was the only adherence measure that was predictive of virologic failure, adherence as determined by the social worker questionnaire was used for subsequent analysis.
HIV outcomes were determined at the end of the 12 month follow-up period. HIV-1 and HIV-2 plasma RNA viral loads were measured using RealTime HIV-1 and HIV-2 Abbott m2000 platform assays. Virologic failure was defined as > 1000 copies/mL for HIV-1 and > 250 copies/mL for HIV-2. Medical records and family report were used to ascertain mortality. Patients who had no contact with the clinic for > 6 months [28, 29] and could not be traced by phone call or home visit were considered lost to follow-up.
Participants who were retained in care at the end of the 12 month follow-up period were categorized into four main categories according to longitudinal food insecurity status: not severely food insecure at enrollment, severely food insecure at enrollment only, severely food insecure at M0 and M6, and severely food insecure at M0, M6, and M12. This last category is referred to as “persistent severe food insecurity”. Two separate categories included those who were not severely food insecure at enrollment but were severely food insecure at both M6 and M12, and those who were severely food insecure at enrollment and M12 but not M6. Individuals who were not severely food insecure at enrollment but were severely food insecure at one of two follow-up visits were included in the category, not severely food insecure at enrollment. Individuals who were severely food insecure at enrollment but were missing follow-up data for M6 or M12 were classified as missing data and were not included in any of the above categories.
Data were analyzed using SPSS Statistics 26. Descriptive analysis was performed for all variables. Chi-square and Fisher’s Exact tests were used to identify differences in outcomes between individuals who were severely food insecure at enrollment versus those who were not severely food insecure, and between individuals who were undernourished at enrollment versus those who were not undernourished. Logistic regressions were used to identify predictors of HIV outcomes. Missing data were excluded from analysis. P-values < 0.05 were considered significant.
Results
A total of 207 participants were enrolled, 84 (41%) were enrolled in Dakar and 123 (59%) were enrolled in Ziguinchor (Table 1). The majority (70%) were female. The median age was 37 years (IQR 31–46). Approximately 61% of participants were 26–45 years of age, 13% were ≤ 25 years of age, including 6 participants < 18 years of age, and 25% were ≥ 46 years of age. The majority (87%) were infected with HIV-1, 11% were infected with HIV-2, and 2% were dually infected with both HIV-1 and HIV-2. The median CD4 cell count at enrollment was 181 cells/mm3 (IQR 63–382), 53% of participants had a baseline CD4 cell count < 200 cells/mm3, and 53% had WHO clinical stage 3 or 4 disease.
The majority (69%) of participants were food insecure at enrollment; 8% were mildly food insecure, 32% were moderately food insecure, and 29% were severely food insecure (Fig. 1). The median baseline BMI among non-pregnant participants ≥18 years of age was 19.6 (IQR 16.7–23.0) and 38% of participants were undernourished at enrollment. Neither baseline BMI nor proportion undernourished at baseline were significantly different among those who were food insecure versus those who were not food insecure at enrollment (BMI:19.75 versus 18.87, p = 0.76; undernourished: 35% versus 44%, p = 0.26).
Nearly a third (32%) of participants had no formal education, 39% had attended some primary school, and 29% had attended secondary school. The majority (87%) had no formal employment. Approximately 23% of participants practiced agriculture, 40% owned livestock, and 4% practiced fishing. Among those who practiced agriculture, 41% raised crops for food and 59% raised crops for both food and income. Crops included rice, peanuts, millet, corn, beans, vegetables, and bananas. Among those who owned livestock, 44% raised livestock for food, 9% raised livestock for income, 40% raised livestock for both food and income, and 7% raised livestock for neither food nor income. Livestock included chickens, ducks, pigeons, sheep, goats, pigs, and cows.
The majority (55%) of participants were married, of which 71% were monogamous and 29% were polygamous. The median number of children was 2 (IQR 1–4; range 0–10). The median household size was 7 (IQR 5–12). The median household daily food expenditure per person was $0.58 (IQR $0.27–$0.97), 22% of participants spent less than $0.25 per day on food per person and 76% of participants spent less than $1.00 per day on food per person. Food expenditure was lower among those who practiced agriculture ($0.35) or owned livestock ($0.36) compared to those who did not practice agriculture ($0.62, p < 0.01) or own livestock ($0.70, p < 0.01). The median round trip transportation time to the HIV clinic was 90 min (IQR 30–240). Transportation time did not differ among those who practiced agriculture or owned livestock compared to those who did not. The median cost of transportation to the HIV clinic was $1.74 (IQR $0.70–$1.83), which was three times the median daily food expenditure per person.
At the time of enrollment, 47% of participants had not told anyone that they were HIV-positive, of which 31% reported that they had not disclosed their status due to fear of stigmatization or because they were ashamed. At M12, 43% had not shared their status, of which 32% reported that they had not disclosed their status due to fear of stigmatization or because they were ashamed. Non-disclosure of HIV-status due to self-stigmatization, which included fear of stigmatization and being ashamed, was more common among those who were food insecure versus not foot insecure (48% versus 8%, p = 0.02). The median household daily food expenditure per person was lower among those who did not share their status compared to those who did ($0.50 [$0.28 - $0.70] versus $0.73 [$0.39 - $1.30], p = 0.048). Nutritional status did not differ between groups.
Following 12 months of ART, 131 participants (63%) were retained in care, 27 (13%) were alive but not retained in care at the enrollment clinic, 19 (9%) were LTFU, and 30 (15%) had died. M12 viral loads were available for 107 participants, of which 16 (15%) experienced VF (Table 2). Poor adherence to ART was reported by 8% of participants and 26% had CD4 cell counts < 200.
Those with severe food insecurity at baseline were more likely to be LTFU than those without severe food insecurity at baseline (16% vs. 5%; p = 0.02). VF, death, poor adherence to ART, and CD4 count < 200 at M12 were similar in those with and without severe food insecurity at baseline.
Those who were undernourished at baseline were more likely to have VF (25% vs. 9%; p = 0.02), more likely to die (21% vs. 7%, p = 0.01; OR 3.35 [95% CI 1.40–8.03], p = 0.01), and more likely to have a CD4 count < 200 at M12 (44% vs. 16%; p < 0.01) than those who were not undernourished at baseline. Loss to follow-up and poor adherence to ART were similar among those who were undernourished versus not undernourished at baseline.
Six months after initiating ART, 68% of participants were food insecure, 37% were moderately food insecure, and 26% were severely food insecure. Twelve months after initiating ART, 69% of participants were food insecure, 35% were moderately food insecure, and 23% were severely food insecure. The median BMI at M6 among non-pregnant participants ≥18 years of age was 20.71 (IQR 18.39–24.94) and 27% were undernourished. The median BMI at M12 among non-pregnant participants ≥18 years of age was 21.51 (IQR 19.60–24.90) and 14% were undernourished.
The median BMI at both M6 and M12 was lower among those who were food insecure at M6 or M12 compared to those who were not food insecure at M6 or M12 (M6 BMI: 20.47 versus 23.51, p = 0.03; M12 BMI: 20.61 versus 23.51, p = 0.04). The proportion undernourished at M6 did not differ significantly among those who were food insecure at M6 versus those who were not food insecure at M6 (30% versus 20%, p = 0.23), nor did proportion undernourished at M12 differ among those who were food insecure at M12 versus those who were not food insecure at M12 (16% versus 13%, p = 0.77). However, those who were food insecure at M12 were more likely to have been undernourished at M0 compared to those who were not food insecure at M12 (45% versus 20%, p = 0.01).
Among the 118 participants who had follow-up food insecurity scores, 84 (71%) were not severely food insecure at enrollment. Among those who were severely food insecure at enrollment and had follow-up food insecurity scores for M6 and M12, 12 (10%) were severely food insecure at enrollment but not M6 or M12, 5 (4%) were severely food insecure at enrollment and M6 but not M12, and 8 (7%) were severely food insecure at enrollment, M6, and M12 (referred to as “persistent severe food insecurity”). Four individuals (3%) were not severely food insecure at enrollment but were severely food insecure at M6 and M12, and 5 (4%) were severely food insecure at enrollment and M12 but not M6.
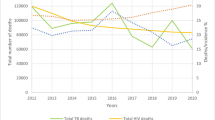
Among those retained in care who had follow-up food insecurity scores, the frequency of poor HIV outcomes at 12 months increased with increased duration of severe food insecurity (Fig. 2a). Poor adherence to ART at M12 was reported by 4% of those who were not severely food insecure at enrollment, 9% who were severely food insecure at enrollment only, 0% who were severely food insecure at M0 and M6 only, and 25% who were severely food insecure at M0, M6, and M12. Those who were severely food insecure at M0, M6, and M12 were more likely to report poor adherence compared to those who were not severely food insecure at enrollment (OR 8.00 [1.11–57.57]. Virologic failure (VF) occurred in 10% of participants who were not severely food insecure at enrollment, 20% who were severely food insecure at enrollment only, 25% who were severely food insecure at M0 and M6 only, and 38% who were severely food insecure at M0, M6, and M12.
a Percent of HIV-infected individuals who were lost to follow-up (LTFU) within 12 months of starting ART, or reported poor adherence to ART, or experienced virologic failure (VF) at 12 months of ART according to food insecurity status. *OR for LTFU 3.13 [1.08–9.06] compared to not severely food insecure at enrollment. **OR for poor adherence 8.00 [1.11–57.57] compared to not severely food insecure at enrollment. ***OR for VF 5.14 [1.01–26.29] compared to not severely food insecure at enrollment. aN = 141 at baseline, 84 among those retained in care; bN = 58 at baseline,12 among those retained in care; cN = 5; dN = 8. b Percent of HIV-infected individuals who died within 12 months of initiating ART, or had CD4 cell counts < 200 following 12 months of ART, or experienced virologic failure (VF) at 12 months of ART according to nutritional status. *OR for DCD 3.35 [1.40–8.03] compared to not undernourished at enrollment. **OR for CD4 < 200 4.24 [1.56–11.47] compared to not undernourished at enrollment; ***OR for CD4 < 200: 5.84 [1.93–17.67] compared to not undernourished at M6. αOR for VF 3.39 [1.13–10.21] compared to not undernourished at enrollment; βOR for VF 7.41 [1.99–27.59] compared to not undernourished at M6; γOR for VF 4.14 [1.13–15.11] compared to not undernourished at M12. aN = 122 at baseline, 87 among those retained in care; bN = 76 at baseline, 44 among those retained in care; cN = 31; dN = 15
Among those retained in care, 87 (66%) were not undernourished at enrollment, 44 (34%) were undernourished at enrollment, 31 (27%) were undernourished at M6, and 15 (14%) were undernourished at M12. Among those retained in care, a CD4 cell count < 200 at M12 occurred in 16% of participants who were not undernourished at enrollment, 44% who were undernourished at enrollment, 48% who were undernourished at M6, and 42% who were undernourished at M12 (Fig. 2b).
Those who were undernourished at M0 or M6 were more likely to have M12 CD4 cell counts < 200 compared to those who were not undernourished at M0 or M6 (OR for M0: 4.24 [1.56–11.47] compared to not undernourished at enrollment; OR for M6: 5.84 [1.93–17.67] compared to not undernourished at M6; OR for M12: 3.16 [0.85–11.67] compared to not undernourished at M12). Among those retained in care, VF occurred in 9% of participants who were not undernourished at enrollment, 25% who were undernourished at enrollment, 32% who were undernourished at M6, and 36% who were undernourished at M12.
The strongest predictors of loss to follow-up were severe food insecurity at enrollment (OR 3.13 [1.08–9.06]) and daily food expenditure per person <$0.25 (OR 4.32 [1.07–17.42]) (Table 3).
The strongest predictors of VF were severe food insecurity at M0, M6, and M12, referred to as “persistent severe food insecurity” (OR 5.14 [1.01–26.29]), undernourished at enrollment or any follow-up visit (OR for M0: 3.39 [1.13–10.21] compared to not undernourished at enrollment; OR for M6: 7.41 [1.99–27.59] compared to not undernourished at M6; OR for M12: 4.14 [1.13–15.11] compared to not undernourished at M12) and the practice of agriculture (OR 4.29 [1.41–13.07]) (Table 4).
Discussion
In this prospective longitudinal study conducted in Senegal, West Africa, we followed HIV-positive individuals during the first 12 months of ART to evaluate the impact of food insecurity on HIV outcomes. We found that severe food insecurity is a strong predictor of LTFU and persistent severe food insecurity is associated with VF and poor adherence to ART.
Food insecurity and HIV are tightly linked in a bidirectional relationship [3] whereby each condition is exacerbated by the other. Individuals with poorly controlled HIV are at greater risk of food insecurity, and individuals who are food insecure may be at increased risk of HIV infection and poor HIV outcomes [3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21, 30,31,32,33,34,35,36,37,38,39,40,41,42]. HIV can contribute to food insecurity as individuals with poorly controlled disease may have decreased physical, social, and economic productivity, compounded by a degradation of household resources due to health related expenses [4, 43,44,45,46,47,48]. These conditions can lead to weaknesses in the four dimensions of food security, namely, food availability, access, utilization, and stability over time [1]. While the focus of this study was the impact of food insecurity on HIV outcomes, it is noteworthy that neither the prevalence nor severity of food insecurity decreased following 12 months of ART. Further studies, including rigorous qualitative studies, are indicated to identify and characterize the factors that drive and maintain food insecurity in this population.
We hypothesized that food insecurity would contribute to poor HIV outcomes through three interrelated pathways, mediated by poor nutritional status, socioeconomic vulnerability, and self-stigmatization (Fig. 3).
Poor nutritional status
A comprehensive understanding of the multidirectional relationships between food insecurity, nutritional status, and HIV requires consideration of the severity and duration of food insecurity, nutritional status over time, and the extent of control over HIV-infection. Furthermore, attention to the measure of food insecurity utilized is important. We used the HFIAS, which focuses on the dimension of food access [24]. We measured food insecurity at three time points during the first 12 months of ART in an effort to capture the dimension of stability over time.
We found that poor nutritional status was associated with poor immunologic recovery, VF, and death. Although food insecurity and nutritional status were not associated at baseline, those who were undernourished at baseline were more likely to be food insecure following 12 months of ART and persistent food insecurity was associated with lower BMI. These findings are consistent with the bidirectional relationship between food insecurity and nutritional status. Weaknesses in any one of the four dimensions of food insecurity can contribute to poor nutritional status. Similarly, poor nutritional status can exacerbate food insecurity. Individuals with poor nutritional status may be unable to participate in activities that ensure access to sufficient, safe and nutritious food, and undernutrition and its associated conditions can impede the body’s ability to adequately utilize nutrients.
While food insecurity can be an important factor contributing to undernutrition, undernutrition can be caused by other factors. As such, the impact of poor nutritional status on HIV outcomes can result from pathways that are independent of food insecurity [4, 49]. Undernutrition, which is defined as, “the outcome of poor nutritional intake in terms of quantity and/or quality, and/or poor absorption and/or poor biological use of nutrients consumed,” [1] is a direct cause of poor immune function and is associated with malabsorption, which can diminish the effects of ART [50,51,52,53]. Similarly, poorly controlled HIV can contribute to undernutrition, as HIV infection and associated inflammation can impair appetite, digestion, metabolic function, and absorption and utilization of nutrients [4, 49,50,51, 54].
Socioeconomic vulnerability
Socioeconomic vulnerability is a fundamental factor driving the complex interactions in our theoretical framework, as individuals who are socioeconomically vulnerable are at increased risk of food insecurity, poor nutritional status, stigmatization, and poor health outcomes. In this study, individuals with lower daily food expenditures were more likely to be LTFU. In a setting where the cost of transportation to the HIV clinic is three times the daily food expenditure, individuals who are socioeconomically vulnerable are faced with conflicting demands on insufficient resources. Confronted by the decision to purchase food for the household or pay for transportation to clinic, some individuals may prioritize food expenditure over transportation expenditure, resulting in greater LTFU. Similarly, socioeconomically vulnerable individuals may be faced with conflicting demands on time. They may prioritize time spent earning income to pay for food rather than spending a substantial amount of time traveling to clinic and waiting for their clinic appointment. Findings from qualitative studies conducted among food insecure PLHIV in SSA have described similar conflicting demands on resources and time; the cost of transportation to clinic in the setting of limited resources for household food, and lost wages due to travel and clinic wait times, are reported barriers to HIV treatment and ART adherence [37,38,39,40].
Conflicting demands on time may also contribute to the association between the practice of agriculture and VF, as socioeconomically vulnerable farmers may prioritize time spent on agricultural needs rather than traveling to clinic or returning home to take their ART during intensive planting and harvesting periods. In previous studies conducted among PLHIV in SSA, agricultural work responsibilities have been reported as a barrier to ART adherence [36]. The association between the practice of agriculture and VF is an important finding that warrants further investigation and identifies farmers as a vulnerable population in Senegal, at high risk of poor HIV outcomes.
Self-stigmatization
We found that non-disclosure of HIV status, even among married participants, was common among participants in this study. Non-disclosure of HIV status is considered a “proximate consequence” of self-stigmatization [55, 56]. Self-stigmatization includes enacted stigma, anticipated stigma and internalized stigma. Internalized stigma is the development of self-defacing beliefs and perceptions about oneself resulting from the acceptance of the negative attitudes of others as valid [55,56,57,58,59]. Anticipated stigma can manifest as fear of disclosing one’s HIV status and internalized stigma can lead to feelings of shame. In this study, food expenditure was lower among those who did not disclose their status and food insecurity was associated with non-disclosure of HIV-status due to fear of stigmatization and feelings of shame.
Multiple prior studies have shown that non-disclosure of HIV status is associated with poor HIV outcomes, including decreased adherence to ART and increased risk of HIV transmission [55, 60, 61]. Furthermore, self-stigmatization can lead to decreased social engagement, depression, and decreased quality of life [55,56,57,58,59,60,61]. In this study, self-stigmatization was determined using open-ended interview questions related to non-disclosure of HIV status. Future studies employing a standardized stigma scale may be more effective in capturing and characterizing the relationship between self-stigmatization and HIV outcomes in this community.
The primary limitations of our study were small sample size and incomplete data. HIV-1 viral loads were not available for 14 of the 115 participants with HIV-1 who were retained in care and 10 of the 12 participants with HIV-2 who were retained in care. We evaluated only two HIV clinics in Senegal, which could limit the generalizability of our findings. Although self-reported adherence was associated with virologic outcomes, measurement of ART levels in patient blood or urine would have provided a more reliable measure. Finally, our findings would have been strengthened by the use of a validated quantitative measure of stigma.
Conclusion
Prospective longitudinal studies are necessary to accurately delineate the impact of food insecurity on HIV outcomes. In this study, severity and duration of food insecurity were important factors in understanding the relationship between food insecurity and HIV. We found that individuals with severe or persistent food insecurity were at increased risk of poor outcomes. Furthermore, our findings highlight the importance of nutritional status, socioeconomic opportunity, and self-stigmatization in the complex pathway between food insecurity and HIV outcomes. Interdisciplinary, multisectoral efforts are needed to develop and implement effective interventions to address food insecurity among PLHIV in SSA.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ART:
-
Antiretroviral therapy
- BMI:
-
Body mass index
- DCD:
-
Deceased
- HFIAS:
-
Household Food Insecurity Access Scale
- IQR:
-
Interquartile range
- ISAARV:
-
Initiative sénégalaise d’accès aux antirétroviraux
- LTFU:
-
Loss to follow-up
- M0:
-
Month 0
- M6:
-
Month 6
- M12:
-
Month 12
- MUAC:
-
Mid-upper arm circumference
- OR:
-
Odds ratio
- PLHIV:
-
People living with HIV
- SSA:
-
Sub-Saharan Africa
- VF:
-
Virologic failure
References
Food and Agricultural Organization of the United Nations. The State of Food Security and Nutrition in the World, Rome (2020). Available at: http://www.fao.org/state-of-food-security-nutrition/en/.
UNAIDS Data 2020. Available at: http://www.unaids.org/en/resources/documents/2020/unaids-data. Accessed 20 Feb 2021.
Weiser SD, Young SL, Cohen CR, Kushel MB, Tsai AC, Tien PC, et al. Conceptual framework for understanding the bidirectional links between food insecurity and HIV/AIDS. Am J Clin Nutr. 2011;94(6):1729S–39S.
Ivers LC, Cullen KA, Freedberg KA, Block S, Coates J, Webb P. HIV/AIDS, undernutrition, and food insecurity. Clin Infect Dis. 2009;49(7):1096–102.
Anema A, Vogenthaler N, Frongillo EA, Kadiyala S, Weiser SD. Food insecurity and HIV/AIDS: current knowledge, gaps, and research priorities. Curr HIV/AIDS Rep. 2009;6(4):224–31.
Himmelgreen DA, Romero-Daza N, Turkon D, Watson S, Okello-Uma I, Sellen D. Addressing the HIV/AIDS-food insecurity syndemic in sub-Saharan Africa. Afr J AIDS Res. 2009;8(4):401–12.
Frega R, Duffy F, Rawat R, Grede N. Food insecurity in the context of HIV/AIDS: a framework for a new era of programming. Food Nutr Bull. 2010;31(4):S292–312.
The Lancet HIV. The syndemic threat of food insecurity and HIV. Lancet HIV. 2020;7(2):e75.
Singer AW, Weiser SD, McCoy SI. Does food insecurity undermine adherence to antiretroviral therapy? A systematic review. AIDS Behav. 2015;19(8):1510–26.
Musumari PM, Wouters E, Kayembe PK, Kiumbu Nzita M, Mbikayi SM, Suguimoto SP, et al. Food insecurity is associated with increased risk of non-adherence to antiretroviral therapy among HIV-infected adults in the Democratic Republic of Congo: a cross-sectional study. PLoS One. 2014;9(1):e85327.
Hong SY, Fanelli TJ, Jonas A, Gweshe J, Tjituka F, Sheehan HM, et al. Household food insecurity associated with antiretroviral therapy adherence among HIV-infected patients in Windhoek, Namibia. J Acquir Immune Defic Syndr. 2014;67(4):e115–22.
Weiser SD, Palar K, Frongillo EA, Tsai AC, Kumbakumba E, Depee S, et al. Longitudinal assessment of associations between food insecurity, antiretroviral adherence and HIV treatment outcomes in rural Uganda. AIDS. 2014;28(1):115–20.
Berhe N, Tegabu D, Alemayehu M. Effect of nutritional factors on adherence to antiretroviral therapy among HIV-infected adults: a case control study in northern Ethiopia. BMC Infect Dis. 2013;13:233.
Sasaki Y, Kakimoto K, Dube C, Sikazwe I, Moyo C, Syakantu G, et al. Adherence to antiretroviral therapy (ART) during the early months of treatment in rural Zambia: influence of demographic characteristics and social surroundings of patients. Ann Clin Microbiol Antimicrob. 2012;11:34.
Birbeck GL, Kvalsund MP, Byers PA, Bradbury R, Mang'ombe C, Organek N, et al. Neuropsychiatric and socioeconomic status impact antiretroviral adherence and mortality in rural Zambia. Am J Trop Med Hyg. 2011;85(4):782–9.
Boyer S, Clerc I, Bonono CR, Marcellin F, Bile PC, Ventelou B. Non-adherence to antiretroviral treatment and unplanned treatment interruption among people living with HIV/AIDS in Cameroon: individual and healthcare supply-related factors. Soc Sci Med. 2011;72(8):1383–92.
Van Dyk AC. Treatment adherence following national antiretroviral rollout in South Africa. Afr J AIDS Res. 2010;9(3):235–47.
Marcellin F, Boyer S, Protopopescu C, Dia A, Ongolo-Zogo P, Koulla-Shiro S, et al. Determinants of unplanned antiretroviral treatment interruptions among people living with HIV in Yaounde, Cameroon (EVAL survey, ANRS 12-116). Tropical Med Int Health. 2008;13(12):1470–8.
Au JT, Kayitenkore K, Shutes E, Karita E, Peters PJ, Tichacek A, et al. Access to adequate nutrition is a major potential obstacle to antiretroviral adherence among HIV-infected individuals in Rwanda. AIDS. 2006;20(16):2116–8.
Aibibula W, Cox J, Hamelin AM, Mamiya H, Klein MB, Brassard P. Food insecurity and low CD4 count among HIV-infected people: a systematic review and meta-analysis. AIDS Care. 2016 Dec;28(12):1577–85.
Benzekri NA, Sambou J, Diaw B, el HI S, Sall F, Niang A, et al. High prevalence of severe food insecurity and malnutrition among HIV-infected adults in Senegal, West Africa. PLoS One. 2015;10(11):e0141819.
Benzekri NA, Sambou JF, Diaw B, Sall EHI, Sall F, Niang A, et al. The dimensions of food insecurity and malnutrition among people living with HIV in Senegal, West Africa. AIDS Care. 2017;29(12):1510–6.
Benzekri NA, Sambou JF, Ndong S, Tamba IT, Faye D, Diallo MB, et al. Prevalence, predictors, and management of advanced HIV disease among individuals initiating ART in Senegal, West Africa. BMC Infect Dis. 2019;19(1):261.
Coates J, Swindale A, Bilinsky P. Household food insecurity access scale (HFIAS) for measurement of household food access: Indicator guide (v. 3). Washington, D.C.: Food and Nutrition Technical Assistance Project, Academy for Educational Development; 2007.
World Health Organization 2007. WHO case definitions of HIV for surveillance and revised clinical staging and immunological classification of HIV-related disease in adults and children. Available at: http://www.who.int/hiv/pub/guidelines/HIVstaging150307.pdf.
World Health Organization. Child Growth Standards. Available at: http://www.who.int/childgrowth/standards/en/. Accessed 20 Feb 2021.
UNHCR. Guidelines for selective feeding: The management of malnutrition in emergencies: United Nations High Commissioner for Refugees; 2011. http://www.unhcr.org/4b7421fd20.html. Accessed 20 Feb 2021.
Chi BH, Yiannoutsos CT, Westfall AO, Newman JE, Zhou J, Cesar C, et al. Universal definition of loss to follow-up in HIV treatment programs: a statistical analysis of 111 facilities in Africa, Asia, and Latin America. PLoS Med. 2011;8(10):e1001111.
Grimsrud AT, Cornell M, Egger M, Boulle A, Myer L. Impact of definitions of loss to follow-up (LTFU) in antiretroviral therapy program evaluation: variation in the definition can have an appreciable impact on estimated proportions of LTFU. J Clin Epidemiol. 2013;66(9):1006–13.
Weiser SD, Leiter K, Bangsberg DR, Butler LM, Percy-de Korte F, Hlanze Z, et al. Food insufficiency is associated with high-risk sexual behavior among women in Botswana and Swaziland. PLoS Med. 2007;4(10):1589–97 discussion 98.
Chop E, Duggaraju A, Malley A, Burke V, Caldas S, Yeh PT, et al. Food insecurity, sexual risk behavior, and adherence to antiretroviral therapy among women living with HIV: a systematic review. Health Care Women Int. 2017;38(9):927–44.
Willie TC, Kershaw TS, Callands TA. Examining relationships of intimate partner violence and food insecurity with HIV-related risk factors among young pregnant Liberian women. AIDS Care. 2018;30(9):1156–60.
McCoy SI, Buzdugan R, Mushavi A, Mahomva A, Cowan FM, Padian NS. Food insecurity is a barrier to prevention of mother-to-child HIV transmission services in Zimbabwe: a cross-sectional study. BMC Public Health. 2015;15:420.
Koss CA, Natureeba P, Nyafwono D, Plenty A, Mwesigwa J, Nzarubara B, Clark TD, Ruel TD, Achan J, Charlebois ED, Cohan D, Kamya MR, Havlir DV, Young SL. Brief report: food insufficiency is associated with lack of sustained viral suppression among HIV-infected pregnant and breastfeeding Ugandan women. J Acquir Immune Defic Syndr. 2016 Mar 1;71(3):310–5.
Weiser SD, Tuller DM, Frongillo EA, Senkungu J, Mukiibi N, Bangsberg DR. Food insecurity as a barrier to sustained antiretroviral therapy adherence in Uganda. PLoS One. 2010;5(4):e10340.
Nagata JM, Magerenge RO, Young SL, Oguta JO, Weiser SD, Cohen CR. Social determinants, lived experiences, and consequences of household food insecurity among persons living with HIV/AIDS on the shore of Lake Victoria, Kenya. AIDS Care. 2012;24(6):728–36.
Hardon AP, Akurut D, Comoro C, Ekezie C, Irunde HF, Gerrits T, et al. Hunger, waiting time and transport costs: time to confront challenges to ART adherence in Africa. AIDS Care. 2007;19(5):658–65.
Musumari PM, Feldman MD, Techasrivichien T, Wouters E, Ono-Kihara M, Kihara M. "if I have nothing to eat, I get angry and push the pills bottle away from me": a qualitative study of patient determinants of adherence to antiretroviral therapy in the Democratic Republic of Congo. AIDS Care. 2013;25(10):1271–7.
Merten S, Kenter E, McKenzie O, Musheke M, Ntalasha H, Martin-Hilber A. Patient-reported barriers and drivers of adherence to antiretrovirals in sub-Saharan Africa: a meta-ethnography. Tropical Med Int Health. 2010;15(Suppl 1):16–33.
Tuller DM, Bangsberg DR, Senkungu J, Ware NC, Emenyonu N, Weiser SD. Transportation costs impede sustained adherence and access to HAART in a clinic population in southwestern Uganda: a qualitative study. AIDS Behav. 2010;14(4):778–84.
Young S, Wheeler AC, McCoy SI, Weiser SD. A review of the role of food insecurity in adherence to care and treatment among adult and pediatric populations living with HIV and AIDS. AIDS Behav. 2014;18(Suppl 5):S505–15.
Aibibula W, Cox J, Hamelin AM, McLinden T, Klein MB, Brassard P. Association between food insecurity and HIV viral suppression: a systematic review and meta-analysis. AIDS Behav. 2017;21(3):754–65.
Bachmann MO, Booysen FL. Health and economic impact of HIV/AIDS on south African households: a cohort study. BMC Public Health. 2003;3:14.
Bachmann MO, Booysen FL. Economic causes and effects of AIDS in south African households. AIDS. 2006;20(14):1861–7.
Laar A, Manu A, Laar M, El-Adas A, Amenyah R, Atuahene K, et al. Coping strategies of HIV-affected households in Ghana. BMC Public Health. 2015;15:166.
Masuku MBSM. The impact of HIV/AIDS on food security and household vulnerability in Swaziland. Agrekon. 2009;48:200–22. https://doi.org/10.1080/03031853.2009.9523824.
Kaschula S. Using people to cope with the hunger: social networks and food transfers amongst HIV/AIDS afflicted households in KwaZulu-Natal, South Africa. AIDS Behav. 2011;15:1490–502. https://doi.org/10.1007/s10461-011-0006-z.
Parker DC, Jacobsen KH, Komwa MK. A qualitative study of the impact of HIV/AIDS on agricultural households in southeastern Uganda. Int J Environ Res Public Health. 2009;6(8):2113–38.
de Pee S, Semba RD. Role of nutrition in HIV infection: review of evidence for more effective programming in resource-limited settings. Food Nutr Bull. 2010;31(4):S313–44.
Semba RD, Tang AM. Micronutrients and the pathogenesis of human immunodeficiency virus infection. Br J Nutr. 1999 Mar;81(3):181–9.
Duggal S, Chugh TD, Duggal AK. HIV and malnutrition: effects on immune system. Clin Dev Immunol. 2012;2012:784740.
Scrimshaw NS, SanGiovanni JP. Synergism of nutrition, infection, and immunity: an overview. Am J Clin Nutr. 1997;66(2):464S–77S.
Schaible UE, Kaufmann SH. Malnutrition and infection: complex mechanisms and global impacts. PLoS Med. 2007;4(5):e115.
Mangili A, Murman DH, Zampini AM, Wanke CA. Nutrition and HIV infection: review of weight loss and wasting in the era of highly active antiretroviral therapy from the nutrition for healthy living cohort. Clin Infect Dis. 2006;42(6):836–42.
Katz IT, Ryu AE, Onuegbu AG, Psaros C, Weiser SD, Bangsberg DR, Tsai AC. Impact of HIV-related stigma on treatment adherence: systematic review and meta-synthesis. J Int AIDS Soc. 2013;16(3 Suppl 2):18640.
Tsai AC, Bangsberg DR, Kegeles SM, Katz IT, Haberer JE, Muzoora C, Kumbakumba E, Hunt PW, Martin JN, Weiser SD. Internalized stigma, social distance, and disclosure of HIV seropositivity in rural Uganda. Ann Behav Med. 2013 Dec;46(3):285–94.
Ma PHX, Chan ZCY, Loke AY. Self-Stigma Reduction Interventions for People Living with HIV/AIDS and Their Families: A Systematic Review. AIDS Behav. 2019;23(3):707–41.
Pantelic M, Steinert JI, Park J, Mellors S, Murau F. 'Management of a spoiled identity': systematic review of interventions to address self-stigma among people living with and affected by HIV. BMJ Glob Health. 2019;4(2):e001285.
Bennett DS, Traub K, Mace L, Juarascio A, O'Hayer CV. Shame among people living with HIV: a literature review. AIDS Care. 2016;28(1):87–91.
Pinkerton SD, Galletly CL. Reducing HIV transmission risk by increasing serostatus disclosure: a mathematical modeling analysis. AIDS Behav. 2007;11(5):698–705.
Yigit I, Modi RA, Weiser SD, Johnson MO, Mugavero MJ, Turan JM, Turan B. Effects of an intervention on internalized HIV-related stigma for individuals newly entering HIV care. AIDS. 2020;34(Suppl 1):S73–82.
Acknowledgements
The authors would like to thank the study participants and the staff of the Services des Maladies Infectieuses et Tropicales, including the Centre Régional de Recherche et de Formation à la Prise en Charge Clinique de Fann and the Centre de Traitement Ambulatoire, Centre Hospitalier Universitaire de Fann and the Centre de Santé de Ziguinchor. Members of the University of Washington-Senegal Research Collaboration can be found at: http://www.uwsenegalresearch.com.
Funding
This study was supported by grants NIH-NIAID K23 AI120761 to N.A.B. The funding body had no role in the design of the study, collection, analysis, or interpretation of data, or in writing the manuscript.
Author information
Authors and Affiliations
Contributions
All authors have approved this manuscript. N.A.B., J.F.S., S.N., M.B.D., I.T.T., D.F., O.C., J.P.D., K.F., and I.S. performed the research. F.S., N.G., C.T.N., J.J.M., and M.S. contributed essential resources. N.A.B, P.S.S., M.S., S.E.H., and G.S.G designed the research study. N.A.B, S.E.H., and G.S.G analyzed the data and wrote the paper.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Study procedures were approved by the University of Washington Institutional Review Board (46735-EJ) and the Senegal Comité National d’Ethique pour la Recherche en Santé (SEN16/64). Written informed consent was obtained for participation in this study. For participants < 18 years of age, consent to participate was obtained from their legal guardian.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests related to this work. N.A.B receives research support from the US National Institutes of Health. G.S.G has received research grants and research support from the US National Institutes of Health, University of Washington, Bill and Melinda Gates Foundation, Gilead Sciences, Alere Technologies, Merck & Co., Inc., Janssen Pharmaceutica, Cerus Corporation, ViiV Healthcare, Bristol-Myers Squibb, Thera technologies/TAI Med Biologics and Abbott Molecular Diagnostics. P.S.S is currently employed at Gilead Sciences. S.E.H has received research grants and support from the US National Institutes of Health, University of Washington, and Bill and Melinda Gates Foundation. All other authors have nothing to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
English translation of study questionnaire
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Benzekri, N.A., Sambou, J.F., Ndong, S. et al. The impact of food insecurity on HIV outcomes in Senegal, West Africa: a prospective longitudinal study. BMC Public Health 21, 451 (2021). https://doi.org/10.1186/s12889-021-10444-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-021-10444-1