Abstract
Background
In 2014, Vietnam was the first Southeast Asian country to commit to achieving the World Health Organization’s 90–90-90 global HIV targets (90% know their HIV status, 90% on sustained treatment, and 90% virally suppressed) by 2020. This pledge represented further confirmation of Vietnam’s efforts to respond to the HIV epidemic, one feature of which has been close collaboration with the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR). Starting in 2004, PEPFAR supported community outreach programs targeting high-risk populations (people who inject drugs, men who have sex with men, and sex workers). To provide early evidence on program impact, in 2007–2008 we conducted a nationwide evaluation of PEPFAR-supported outreach programs in Vietnam. The evaluation focused on assessing program effect on HIV knowledge, high-risk behaviors, and HIV testing among high-risk populations—results relevant to Vietnam’s push to meet global HIV goals.
Methods
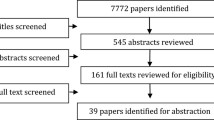
We used a mixed-methods cross-sectional evaluation design. Data collection encompassed a quantitative survey of 2199 individuals, supplemented by 125 in-depth interviews. Participants were members of high-risk populations who reported recent contact with an outreach worker (intervention group) or no recent contact (comparison group). We assessed differences in HIV knowledge, risky behaviors, and HIV testing between groups, and between high-risk populations.
Results
Intervention participants knew significantly more about transmission, prevention, and treatment than comparison participants. We found low levels of injection drug-use-related risk behaviors and little evidence of program impact on such behaviors. In contrast, a significantly smaller proportion of intervention than comparison participants reported risky sexual behaviors generally and within each high-risk population. Intervention participants were also more likely to have undergone HIV testing (76.1% vs. 47.0%, p < 0.0001) and to have received pre-test (78.0% vs. 33.7%, p < 0.0001) and post-test counseling (80.9% vs. 60.5%, p < 0.0001). Interviews supported evidence of high impact of outreach among all high-risk populations.
Conclusions
Outreach programs appear to have reduced risky sexual behaviors and increased use of HIV testing services among high-risk populations in Vietnam. These programs can play a key role in reducing gaps in the HIV care cascade, achieving the global 90–90-90 goals, and creating an AIDS-free generation.
Similar content being viewed by others
Background
In Vietnam, HIV is concentrated among people who inject drugs (PWID), female sex workers (FSW), and men who have sex with men (MSM). Prevalence in the overall adult population has remained low, peaking in 2005 and remaining stable at 0.4% among adults aged 15–49 years [1]. By comparison, prevalence among PWID, FSW, and MSM is estimated to be 10.3, 2.6, and 3.7%, respectively [2], with PWID comprising 60% of all reported HIV-infected individuals [3]. Although these marginalized populations remain disproportionately affected, Vietnam has made impressive strides in reducing vulnerability and new infections since 2001, when prevalence peaked at 29.3% among male PWID and nearly 7.0% among FSW [4]. Data are limited for MSM, who have become a higher priority population in the last few years [5].
In 2014, Vietnam was the first Southeast Asian country to commit to achieving the 90-90-90 global HIV targets by 2020: 90% of population knowing HIV status, 90% on sustained antiretroviral therapy (ART), and 90% with suppressed viral load [6]. In June 2016 at the United Nations High Level General Assembly Meeting on Ending AIDS, Vietnam pledged to reach zero new infections by 2030 [6]. The United States government (USG) has invested in HIV prevention, testing, treatment, and care in Vietnam since the 1990s; in 2004, Vietnam was named one of fifteen focus countries by the President’s Emergency Plan for AIDS Relief (PEPFAR) [7]. Since then, PEPFAR investments have provided ART to 57,000 Vietnamese citizens, care and support to 62,000 children and adults, and methadone support for 25,000 PWID. In 2016, the USG committed $26 million through 2021 to help Vietnam meet the 90-90-90 targets. While support from other international sources, including direct bilateral aid from a number of governments (including Australia, Denmark, France, and the United Kingdom), United Nations organizations, and multilateral assistance (the Asian Development Bank, The Global Fund to Fight AIDS, Tuberculosis, and Malaria, and the World Bank) has played an important role in Vietnam’s HIV and AIDS achievements in meeting the 90-90-90 goals, PEPFAR has provided the greatest support. [8] According to the 2016 Country Operation Plan, Vietnam’s government has set an additional goal of independently funding 75% of the country’s HIV programming by 2020 [5].
In 2007–2008, we conducted a nationwide mixed-methods cross-sectional evaluation of the impact of PEPFAR-supported community-based outreach programs. The evaluation was designed to assess program effect on HIV knowledge, high-risk behaviors, and HIV testing among Vietnam’s key high-risk populations: PWID, FSW, and MSM. It also examined use of peer educators versus health educators, and made specific recommendations for program improvements. Initial findings were shared at a national workshop in Hanoi and in a USAID report [9, 10]; select descriptive results have been published elsewhere [11]. We focus here on the key findings related to the impact of the outreach programs on knowledge, risk-taking, and HIV testing uptake. Because this study was conducted 7 years before Vietnam committed to the 90–90-90 goals, it provides useful, detailed insight into the peer outreach efforts that have been central to government and development partner interventions.
While outreach efforts focused primarily on HIV testing and prevention, or what would later be articulated as the first 90 target, accompanying measures have been designed to increase capacity across all of the 90-90-90 goals. These capacity-strengthening measures include reducing stigma and discrimination, training physicians in clinical care and treatment of HIV-positive patients, developing a care and treatment coordination unit within the Ministry of Health, and establishing a national surveillance and monitoring system [12].
Overview of Vietnam’s long-term peer outreach programming
Peer-driven community outreach efforts have been a core component of Vietnam’s domestic and international response to HIV. Vietnam first employed peer educators for HIV prevention among high-risk populations in 1993 [13]. In 2004, use of outreach workers was expanded in accordance with Vietnam’s National Strategic Plan on HIV/AIDS Prevention for 2004–2010, the country’s first HIV national plan [14]. With PEPFAR support, several internationally recognized best practices were adopted, including increasing voluntary HIV testing, implementing harm reduction measures for high-risk populations, and employing outreach workers to expand community-based HIV prevention measures focused on increasing HIV knowledge and reducing high-risk behaviors among key populations, primarily PWID, FSW, and MSM [15]. By 2007, PEPFAR-supported outreach programs had expanded in seven focus provinces (all high-prevalence provinces), and aimed to reach 30,000 individuals annually [16]. In the years since then, these programs have recruited, trained, and deployed cadres of peer educators (individuals who currently engage in injection drug use or sex work, or have in the past) and health educators (usually college graduates trained in health education). These outreach workers were trained to provide HIV-prevention information, skills, and supplies (such as condoms), as well as links to HIV testing, treatment, and other services, based on globally-recommended best practices for HIV prevention [12, 14].
Several studies have documented the impact of specific interventions based on use of peer outreach workers to engage with particular vulnerable populations in Vietnam. Hammett et al. (2012) described projects that have trained peer outreach workers to use personal education techniques and needle/syringe distribution to reduce HIV risk behaviors and infection among PWID in northern Vietnam and southern China [3]. In another study focused on adolescents and young adults aged 15–24 years, Ngo et al. (2013) described a combination of peer-employed education and integrated HIV and sexual and reproductive health services that successfully expanded HIV testing among youth [17]. A third study employed a pre-test, post-test design and found a positive association between engagement with peer educators and willingness to use pre-exposure prophylaxis among male sex workers in Ho Chi Minh City [18]. While these studies indicate the potential for specific interventions to make use of community outreach to contribute to desired behavior change, each was limited in scope to specific research questions, either focusing on one high-risk population or a single setting. None was designed to evaluate the broad impacts of community-based HIV prevention outreach programs operating across the country according to their original mission: to engage with all three of the major high-risk populations to increase their knowledge, reduce risky behaviors, and engage in HIV testing services.
While the data reported here were collected just over 10 years ago, the limited evidence published on this topic underscores the usefulness of this study for HIV researchers, program designers, and policy makers. To our knowledge, no other study in Vietnam has assessed the impact of community-based outreach programs at the national level among all of the primary high-risk populations and across multiple risk behaviors. Thus, these findings contribute vital evidence from which Vietnam and its development partners can build in the quest to reach the 90-90-90 targets by 2020 and achieve zero new infections, zero AIDS-related deaths, and zero stigma by 2030.
Methods
Design overview
Because outreach programs had been underway for several years, our design options were limited. To conduct an evaluation that could yield meaningful data on program impact, we used a mixed-methods, cross-sectional design that would permit comparison of relevant quantitative outcomes between an intervention group (individuals in each high-risk group with recent exposure to the outreach programs) and a comparison group (individuals in each high-risk group without recent exposure to the outreach programs). This was achieved through a comprehensive quantitative survey with members in each high-risk group. We supplemented the survey with qualitative in-depth interviews with survey participants to allow probing on important topics and triangulation of multiple sources of data. Our goal was to collect a rich set of quantitative and qualitative data to assess program impact related to knowledge and behaviors of populations known to engage in high-risk behaviors.
Study sites and participants
Quantitative survey data were collected from members of high-risk populations in two northern provinces (Ha Noi, Hai Phong) and two southern provinces (Ho Chi Minh City (HCMC), An Giang). Qualitative data were gathered from individuals in the same populations in these four provinces and in two additional provinces (Quang Ninh in the north and Can Tho in the south). These provinces were selected because, due to their major HIV epidemics, they were focal provines of the PEPFAR-funded community outreach programs described above, and they provided geographic diversity across Vietnam. Ha Noi and HCMC are large, densely populated cities with modern economies, diverse populations from an influx of domestic migrants, and well-educated workforces. Hai Phong and Quang Ninh, on the northeastern coast, have relatively advanced infrastructure and large industrial workforces. Can Tho and An Giang are inland provinces with mainly agricultural economies and substantial migrant populations from neighboring Cambodia. All six provinces historically have had a relatively high HIV prevalence, particularly among PWID, for whom prevalence has recently ranged from 15 to 25% [19, 20].
Participants were recruited in collaboration with agencies implementing PEPFAR-funded outreach programs, including FHI 360 (formerly Family Health International), Ministry of Health/LIFEGAP, Médecins du Monde France, and Care International, using a snowball sampling approach. Peer outreach workers employed by the agencies made initial introductions to their regular clients, who in turn shared study information with their peers among PWID, FSW, and MSM. In accordance with our evaluation design, this included introductions to individuals who had had recent contact with an outreach worker in the previous 6 months and those who had not. These peers continued to introduce the study in subsequent rounds to their acquaintences until the desired sample size was achieved. Individuals were eligible if they were aged 18 years or older and could be categorized into one of four populations on the basis of self-reported behavior(s): 1) using injection drugs in the past month (PWID); 2) identifying as female, selling sex in the past month, and working on the street (SSW); 3) identifying as female, selling sex in the past month, and working in an establishment (KSW); or 4) identifying as a man who engaged in sex with another man in the past year (MSM). Participants who met multiple criteria were placed into a single primary group for recruitment purposes in this order: MSM, SSW/KSW, PWID.
The qualitative in-depth interviews (IDIs) were designed to collect supplemental in-depth information from survey participants about their personal experiences engaging with community outreach workers. Thus, in the four survey provinces, we randomly identified participants in the intervention group for IDI participation. In Quang Ninh and Can Tho (where no survey was conducted), we recruited IDI participants who reported recent contact with an outreach worker using the same snowball sampling approach described above.
All procedures performed in this study were in accordance with the relevant ethical standards of the institutional and national research committees and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study protocol was approved by the Institutional Review Boards of Boston University Medical Center, the Hanoi School of Public Health, and the HCMC AIDS Committee. All participants provided written informed consent.
Data collection
Data were collected from November 2007 to September 2008, supervised by senior researchers at the HCMC Statistical Office. Trained supervisors from this office conducted workshops covering study purpose, methods, and ethical issues with the quantitative and qualitative research teams in each province. Field supervisors oversaw daily data collection. For the IDIs, six interviewers from Hanoi’s Institute of Sociology trained in qualitative methods collected data in Ha Noi, Hai Phong, Quang Ninh, and Can Tho. Six similarly trained interviewers from the Institute of Sociology in HCMC conducted IDIs in HCMC and An Giang. Two interviewers, one posing questions and the second taking notes, performed each IDI.
All surveys and IDIs were conducted face-to-face in Vietnamese in offices, club locales, or other locations convenient to participants. Each activity lasted 1.5–2 h. All participants received a stipend of 50,000 Vietnamese Dong (VND) (US$ 3.12) to cover the costs of travel and/or lost work time. In addition, participants who identified up to three other eligible survey participants were given an incentive stipend of 20,000 VND (US$ 1.25) per participant.
Survey questions were drawn from validated instruments previously used in Vietnam [21] that addressed HIV knowledge, health-risk behaviors, HIV testing, and interactions with outreach workers. Knowledge queries covered transmission (16 yes/no questions), prevention (17 yes/no questions), and treatment (8 yes/no questions). Health-risk behaviors included drug use, and needle sharing and cleaning; and protective behaviors related to condom access and use with primary, casual, and commercial partners in the previous 6 months. HIV testing questions asked about testing, as well as pre- and post-test counseling.
The IDIs employed semi-structured interview guides that allowed for open-ended responses and follow-up questioning. Questions covered program strengths and weaknesses, interactions with outreach workers, and perceived program impact. Survey and IDI instruments were pilot-tested and revised prior to data collection.
Quantitative data analysis
High-risk populations and outreach programs were larger in Ha Noi and HCMC (“large provinces”) than in Hai Phong and An Giang (“small provinces”). In large provinces, we based sample size calculations on the ability to identify differences of 20 percentage-points or more in knowledge and high-risk behaviors between intervention and comparison groups for each population (using the most conservative estimate of 50% levels of correct knowledge for the comparison group), with a confidence interval of 95% (α = 0.05) and 80% power. In the small provinces, sample sizes for PWID, SSW, and KSW were half of those of the large provinces; because MSM programs were limited, we did not recruit MSM in small provinces.
Survey data were entered into Microsoft Visual FoxPro 9 by research staff in HCMC and analyzed in Boston using SAS version 9.0 (The SAS Institute, Cary, NC). We summarized responses using means, medians, and interquartile ranges for continuous variables; and frequencies and proportions for categorical variables. For knowledge questions, we constructed three sets of scores from the 16 yes/no transmission questions, 17 yes/no prevention questions, and 8 true/false treatment questions, respectively; each correct answer received one point. We calculated total proportion correct of the total possible score, and separate treatment and combined transmission/prevention scores, since the latter were the primary focus of outreach programs at the time of data collection. For sexual behavior questions, we defined consistent condom use as “always” (100%), based on the most conservative measure of condom use (anything below 100% use was considered inconsistent) [22].
In order to assess program impact related to HIV knowledge and behaviors, we disaggregated participants’ data into “intervention” vs. “comparison” groups based on whether they reported contact with an outreach worker in the most recent 6 months (intervention) or did not report such recent contact (comparison). We then compared intervention vs. comparison group differences in HIV/AIDS knowledge, high-risk behaviors, and HIV counseling and testing (HCT). We also compared responses among groups, with groups categorized by recruitment category (PWID, SSW, KSW, MSM) and by self-reported behaviors (injection-drug use, sex work, male-to-male sex). Because recruitment categories aimed to ensure an adequate number of participants within each of the population groups, whereas the behavior-based analysis encompassed all participants who reported a given behavior (allowing for overlap in behaviors when multiple behaviors were reported), we report findings based on self-reported behaviors as we believe they are more meaningful. We also report the results of analyses that stratify the FSW by SSW vs. KSW. We compared responses using χ2 tests for categorical variables and Student’s t tests for continuous variables.
Qualitative data analysis
We aimed to conduct 6–10 IDIs with each of three high-risk populations (PWID, SSW/KSW, and MSM) in each province to assure a wide range of opinions. A professional translator translated audio-recordings into English; a Boston University Medical Center researcher checked each transcript and clarified unclear responses with the translator. Bilingual team members spot-checked transcripts for consistency with audio-recordings. One Boston-based analyst coded transcripts using a thematic approach and analyzed themes in Microsoft Excel 2010 [23]. We examined responses by population group and location. In addition to identifying common themes, we explored divergent views. We also identified illustrative statements to contextualize the results of the quantitative findings.
Results
Background characteristics of participants
We surveyed 2199 individuals, including 1100 intervention and 1099 comparison participants. Participants were generally young (mean age 29 years), evenly divided between male and female, and employed either full-or part-time (Table 1). Approximately one-fourth had no education beyond primary school. One-third reported “sex worker” as their main daily activity; others had a salaried job (14.3%) or performed manual labor (11.1%). Intervention participants were slightly older than comparison participants, and more likely to have tested positive for HIV (21.8% vs. 15.5%) and to have had sex with someone who is HIV-positive (13.1% vs. 5.7%) or a PWID (24.1% vs. 14.7%).
We conducted a total of 125 IDIs, 18–21 per province except in HCMC, where 25 IDIs were conducted (detailed data not shown). Qualitative participants’ characteristics were similar to those of survey participants: the mean age was 30.1 years; 48.0% were male; and one-fourth had no schooling above the primary level.
Effectiveness of community outreach
Knowledge of HIV/AIDS
Overall knowledge of HIV transmission and prevention was high (mean score = 83.4%); treatment knowledge was poor (mean = 41.7) (Table 2). Across all knowledge categories, intervention participants scored significantly higher than comparison participants, particularly on treatment questions (48.2% vs. 35.2%, p < 0.0001). Within each separate key population group, intervention group scores were also significantly higher than comparison group scores for each knowledge category. Analysis by key population group found significantly higher scores among PWID on overall knowledge and on treatment, particularly compared to other key population groups; MSM scored highest on transmission/prevention knowledge. Among FSW, KSW participants scored higher than SSW in every category.
Qualitative data from interviews underscored the ability of outreach workers to reach individuals at high risk of HIV infection with effective information about HIV transmission and ways to reduce HIV vulnerability. The majority of participants spoke of enhanced knowledge about HIV and risk reduction. Increased knowledge was also associated with behavior change, new attitudes about living with HIV, and reduced fear: “I’ve changed … now that I know a little more, I’m not afraid anymore.” (FSW in Ha Noi) More illustrative statements by participants are in Table 3.
High-risk injection behaviors
Among survey participants who reported using injection drugs in the previous 6 months (n = 694, 31.6%), we found low proportions of high-risk injection-related behaviors (Table 4). Only 14% reported having shared injection equipment in the previous 6 months; of those, 36% reported re-using a needle/syringe at last injection (data not shown). Few differences between intervention and comparison groups emerged. However, when asked about measures taken to reduce infection risk, a significantly higher proportion of intervention vs. comparison participants reported various actions, most notably, stopping sharing of injection equipment (74.6% vs. 67.9%, p = 0.05) and starting or increasing cleaning of equipment (62.2% vs. 52.1%, p < 0.001). A within-group analysis comparing PWID who were also SSW (n = 67), KSW (n = 23), or MSM (n = 8) vs. those who were only PWID (n = 596) showed that the latter were significantly more likely to have stopped sharing needles (59.1% vs. 34.8–46.3% for the overlapping groups, p = 0.029) or to have started/increased cleaning of equipment (59.7% vs. 25.0–47.8%, p = 0.009) (data not shown).
Analysis of qualitative data (Table 3) found evidence supporting changed behaviors, particularly regarding sharing of syringes and needles and sterilization of equipment. Typical statements were: “After meeting [the peer educator], I think I am more knowledgeable. If I want to inject, I have to do it carefully” (PWID in Can Tho) and “In the past, I thought: what would be, would be. I used drugs rashly until I was informed. I was also scared, [but] now I never share injection syringes and needles” (PWID in Ha Noi).
High-risk sexual behavior: inconsistent condom use
Among the 2040 participants (92.8%) who reported having had vaginal or anal sex in the previous 6 months, large proportions reported high-risk sexual behaviors (see Table 5). Overall, only 37.5% reported “always” using a condom, while 16.7% “occasionally” used them (data not shown). We also found that a significantly higher proportion of intervention participants reported more frequent condom use, in general, and with each type of sexual partner—primary, casual, and client—in the previous 6 months. Among population groups, a higher proportion of FSW reported “always using” condoms (38.7%) compared to other groups; PWID reported the lowest consistent condom use (31.3%). Within each group, consistent condom use was highest when having sex with a client, with proportions ranging from a low of 42.7% (PWID) to a high of 63.8% (FSW). Additionally, the differences in consistent condom use between intervention and comparison participants were greatest with client sex partners for both FSW (69.9% v. 57.8%, p < 0.01) and PWID (61.5% v. 46.0%, p = 0.09); among MSM, however, this difference was highest for sex with casual partners (42.2% v. 32.3%, p = 0.01). MSM also reported similar levels of condom use across partner categories: approximately 40% reported “always use condoms” regardless of partner, whereas PWID and FSW reported much lower consistent condom use for casual partners (7–13%) and primary partners (24–28%) than for clients. Among FSW only, SSW tended to report somewhat higher consistent condom use than KSW, including with clients (67.8% v. 64.9%). Less than one-half (45.6%) of all participants reported “always carry condom,” with a significant difference between intervention and comparison participants (49.7% v. 41.4%, p < 0.01). This difference remained significant for FSW overall (55.9% v. 46.6%, p < 0.01), and for SSW (65.0% v. 55.2%, p = 0.02), whose reported “always carry condom” proportion was the highest of all groups.
Qualitative data (see Table 3) support these findings of effective messaging by outreach workers. Intervention participants described changing their attitudes and behaviors regarding condom use, with typical statements including, “After talking to them [peer educators], I know a lot. After reading the papers they give, I changed my habits to be safer” (FSW in Quang Ninh) and “My partner has sex with others, so I use condoms all the time. Believe him or not, I still have to use condoms to be safe first” (MSM in HCMC). Several participants revealed less than consistent condom use, however. One PWID in Ha Noi explained that sometimes late at night, when he was craving drugs, he would “go out with friends and girls, and no one brings condoms.”
HIV counseling and testing behaviors
More than half of respondents reported receiving pre-test counseling (55.8%) and having been tested for HIV (61.6%) (Table 6). Among those tested, 73.1% received post-test counseling and 89.9% received results. We found significant differences between intervention and comparison participants for each service except for receipt of results. The intervention group was significantly more likely to have been tested for HIV (76.1% vs. 47.0%, p < 0.0001) and to have received both pre-test (78.0% vs. 33.7%, p < 0.0001) and post-test counseling (80.9% vs. 60.5%, p < 0.0001). There were no differences in reported receipt of results or sharing of results. Within populations (encompassing intervention and comparison groups), testing ranged from 50.4% among MSM to 64.3% among FSW. Testing was highest among FSW sub-groups, for both the intervention (80.7 and 78.3% for SSW and KSW, respectively) and comparison (52.4 and 53.2%) groups. In addition, of those who were tested and received results, PWID participants reported the highest rates of HIV+ diagnoses across intervention and comparison groups (49.6 and 43.2%, respectively, difference not significant).
The qualitative data underscored both the impact of outreach efforts on encouraging HIV testing, and persistent barriers in reaching key populations with testing services; attitudes towards health workers revealed a strong sense of continued stigmatization of individuals suspected of engaging in sex work, gay sex, and drug use (see Table 3). Several IDI participants admitted continued fear of learning their status. One PWID in Ha Noi noted that sometimes he lied to the outreach workers, saying that he had been tested when that was not true; he remained too fearful to be tested.
Discussion
This mixed methods evaluation provides important evidence of the value of community outreach interventions deploying peers and other health educators for improving knowledge of HIV transmission, prevention, and treatment. Community members who interacted with peer and health educators demonstrated significantly greater HIV/AIDS knowledge, particularly on treatment questions, than those who did not. Intervention participants were more likely to have been tested for HIV and to have received counselling before and after testing. Likewise, outreach programs appear to have reduced risky sexual behaviors and increased uptake of HIV testing services among high-risk populations. As Vietnam and development partners plan funding and programmatic priorities to meet the 90-90-90 targets by 2020 and to end new infections by 2030, gaps in treatment knowledge, HIV testing, and consistent condom use demand sustained focus and funding. Our 2007–2008 evaluation data, combined with other recent research, offer critical guidance for national strategy and future program implementation.
Sustained treatment & adherence
While intervention participants had higher levels of treatment knowledge than comparison participants in this study, treatment knowledge was still low among those receiving outreach. This is consistent with studies in Vietnam that have found numerous misconceptions regarding treatment—including one study which found that most respondents (70%) incorrectly believed that ART could cure HIV [24]. At the time of this evaluation, outreach workers were not regularly giving treatment information to clients, which may explain the low scores on HIV treatment knowledge questions among those receiving outreach [11]. However, recent research suggests that this gap in treatment knowledge persists [17, 24]. Looking forward, education about both the benefits and management of side effects of ART must remain a top priority. All stakeholders must remain vigilant about dispelling misconceptions about treatment, which negatively affect patients’ engagement, adherence to treatment, and clinical outcomes [25, 26].
Engagement in HIV counseling and testing services
On the topic of HCT, we found that the intervention group was significantly more likely to receive voluntary pre- and post-test counseling, and HIV testing than the comparison group. These findings suggest that community outreach is a valuable strategy for increasing uptake of HIV testing services across key populations. This observation is consistent with findings from another study in Vietnam, which found that receiving voluntary HIV testing services, condoms, and injection equipment from the local HIV prevention program was significantly associated with lower reported HIV risk behavior [27]. Previous research has also found that HCT is an effective prevention strategy, and can be an entry point to support and care for key populations [28,29,30]. Nonetheless, key populations may still be reluctant to seek HIV testing even though they are aware of its importance [31]. We documented a number of reasons for this, including judgmental attitudes of clinical staff, fear of learning of one’s status, failure to prioritize testing given busy lives and perceived good health, and cost of related services.
Getting to zero
Interventions focused on improving consistent condom use with all partners will also need to remain a high priority looking forward to the 2030 goal of ending AIDS. Although we found strong evidence of effectiveness of outreach in the higher condom use of intervention participants vis-à-vis comparison participants, over half of intervention participants reported inconsistent condom use, except with sex work clients. This is worrisome given more recent evidence that condom use has remained low in Vietnam [32, 33]. Assessments from India are informative, indicating similar patterns of low condom use among regular partners, and by men when having sex with women [34, 35]. This suggests that condom negotiation with repeat clients and regular partners is more difficult than with casual/new partners, and that this complexity may not be addressed easily via community-outreach programs [35]. Other approaches—such as empowerment, increased self-esteem, and community mobilization—may have a role in increasing condom use among regular sexual partners, and might be considered when developing interventions [36]. Strategies shown to be successful in increasing condom use with regular partners include providing high-intensity peer and clinical services for high-risk MSM and transgender people, and increasing condom availability among key populations [35]. Given rising concern about HIV among MSM, reaching this subpopulation will be critical [37]. Outreach efforts that make use of social media with MSM in other settings, including in sub-Saharan Africa, may hold lessons for places like Vietnam that are highly “wired,” with broad internet availability and mobile phone use [38,39,40]. Regardless of specific approach, prevention programs need to stress the importance of consistent condom use with all partners, regardless of sex, sexual orientation, or gender identity.
Limitations
Several study limitations may bear on these findings. First, while the mixed methods approach allowed for triangulation of findings, the survey was cross-sectional, and thus cause and effect cannot be confirmed. Second, because sampling was respondent-driven rather than randomized, our results may be biased due the socio-demographic composition of either or both key population groups (intervention or comparison). In particular, reliance on social networks to recruit participants may have produced a sample with similar characteristics and similar behavioral tendencies, thus leading to skewed results [41]. Third, due to the self-reporting nature of the study, social desirability may have influenced our findings, as participants may have answered questions based on what they thought interviewers wanted to hear. Fourth, despite its breadth, our sample may not be representative of Vietnam’s at-risk population nationally since no sampling frame exists that lists these individuals by behavioral characteristics. Fifth, it is conceivable that participants had benefited from other interventions beyond the peer-outreach programs we assessed. However, to our knowledge, there were no other similar programs operating in Vietnam at that time. There may have been small programs distributing condoms in some of these places, but the individuals who participated in our study were all engaged in one or more illegal and heavily-stigmatized behaviors that meant they were a fairly hidden population and receiving HIV-related information and support primarily through the outreach programs. Moreover, were there other programs, individuals in both groups would have accessed them, and thus they would not be the source of systematic bias.
Finally, the study was conducted over 10 years ago, and its relevance may be questioned. We would posit that the study had important strengths that warrant attention: a strong mixed-methods design with collection of rich, in-depth qualitative data; a creative design to yield robust comparisons between intervention and comparision group participants; a broad national scope; and inclusion of all three critical vulnerable populations in Vietnam (PWID, FSW, and MSM). To our knowledge, there is no published study with anything near the comprehensive scope of this evaluation in geographic, participant, and outcome data terms. Given that little has been published on HIV prevention outreach programs in Vietnam, where the epidemic continues to pose a major challenge and key populations continue to be highly vulnerable, we believe our findings may inform efforts to improve outcomes in the HIV care cascade in Vietnam and perhaps elsewhere in Asia.
Conclusions
This national evaluation led to important findings about the effectiveness of PEPFAR-supported community-based outreach programs targeting key populations of PWID, MSM, and FSW. The program appeared successful on numerous fronts, including increased HIV knowledge, high-risk injection and sexual behavior, and uptake of testing services. However, our evaluation identified important gaps which must be addressed in future prevention efforts, whether through large-scale community-outreach or through more intensive and clinic-based programming. Priorities should target low knowledge of HIV treatment among key populations, the complexity of sexual patterns and low condom use with regular partners, and inadequate awareness of and engagement with HCT services.
Availability of data and materials
The datasets generated and analysed during the current study are not publicly available currently because analyses of data by team members are still underway. Once these are completed, we will make data available from the corresponding author on reasonable request.
Abbreviations
- ART:
-
Antiretroviral therapy
- FGD:
-
Focus group discussion
- FSW:
-
Female sex workers
- HCMC:
-
Ho Chi Minh City
- HCT:
-
HIV counseling and testing
- IDI:
-
In-depth interview
- KSW:
-
Female sex workers who work in establishments
- MSM:
-
Men who have sex with men
- PEPFAR:
-
President’s Emergency Plan for AIDS Relief
- PWID:
-
People who inject drugs
- SSW:
-
Female sex workers who work on the street
- USG:
-
United States Government
- VND:
-
Vietnamese Dong
References
The World Bank. Prevalence of HIV, total (% of population ages 15–49). Available from: https://data.worldbank.org/indicator/SH.DYN.AIDS.ZS. Accessed 7 Aug 2019.
Socialist Republic of Vietnam. Vietnam AIDS Response Progress Report 2014. Following Up the 2011 Political declaration on HIV AIDS. Hanoi; 2014. Available from: https://www.aidsdatahub.org/sites/default/files/publication/Vietnam_narrative_report_2014.pdf. Cited 1 Feb 2017.
Hammett TM, Des Jarlais DC, Kling R, et al. Controlling HIV epidemics among injection drug users: eight years of cross-border HIV prevention interventions in Vietnam and China. PLoS One. 2012;7(8):e43141.
Viet Nam authority of HIV/AIDS control. An annual update on the HIV epidemic in Viet Nam Hanoi: 2014. Available from: https://aidsdatahub.org/sites/default/files/country_review/An_annual_update_on_HIV_epidemic_in_Viet_Nam_2014.pdf. Cited 15 Mar 2018.
President’s Emergency Plan for AIDS Relief (PEPFAR). VIETNAM Country/Regional Operational Plan (COP/ROP) 2016: Strategic Direction Summary, Version May 27, 2016. 2016. Available from: https://www.pepfar.gov/documents/organization/257625.pdf. Cited 15 Feb 2017.
UNAIDS. Viet Nam is key partner at high-level meeting on ending AIDS. Available from: http://unaids.org.vn/en/viet-nam-key-partner-high-level-meeting-ending-aids/. Accessed 15 Mar 2017.
U.S. Department of State: ARCHIVE. Vietnam. Available from: https://2001-2009.state.gov/s/gac/countries/fc/vietnam/. Accessed 7 Aug 2019.
Socialist Republic of Vietnam. Vietnam AIDS response Progress report 2014: following up on the 2011 political declaration on HIV AIDS. 2014. Available from: https://www.unaids.org/sites/default/files/country/documents/VNM_narrative_report_2014.pdf. Cited 20 Oct 2018.
Sabin L, Vian T, Hamer D, et al. Evaluation of President’s emergency plan for AIDS relief (PEPFAR)-funded community outreach HIV prevention programs in Vietnam: report on findings, 2008. United States Agency for International Development, Boston University, PACT. 2009.
Sabin LL, Loan LTT, Trong DQ, et al. Evaluation of PEPFAR-Funded Community outreach HIV prevention programs in Vietnam: initial assessment with suggestions for program improvements. Abstract #1031. Oral presentation. 2008 HIV/AIDS implementers’ meeting; 2008 June. Kampala, Uganda.
Vian T, Semrau K, Hamer DH, Loan le TT, Sabin LL. HIV/AIDS-related knowledge and behaviors among Most-at-risk populations in Vietnam. Open AIDS J. 2012;6:259–65.
PEPFAR (President’s Emergency Plan for AIDS Relief). Country profile: Vietnam. Washington DC; 2006. Available from: https://www.pepfar.gov/documents/organization/90114.pdf.
Khoat DV, West GR, Valdiserri RO, Phan NT. Peer education for HIV prevention in the Socialist Republic of Vietnam: a national assessment. J Community Health. 2003;28(1):1–17.
World Health Organization (WHO). Vietnam: summary country profile for HIV/AIDS treatment scale-up. Geneva; 2005. Available from: https://www.who.int/hiv/HIVCP_VNM.pdf. Cited 4 Nov 2018.
General Statistical Office (GSO), National Institute of Hygiene and Epidemiology (NIHE) [Vietnam], and ORC Macro. Vietnam population and AIDS Indicator survey. Calverton: GSO, NIHE, and ORC Macro; 2006.
PEPFAR (President’s Emergency Plan for AIDS Relief). Populated Printable COP (Country Operating Plan): Vietnam. 2007. Available from: https://www.pepfar.gov/documents/organization/272025.pdf. Cited 9 Nov 2018.
Ngo AD, Ha TH, Rule J, Dang CV. Peer-based education and the integration of HIV and sexual and reproductive health services for young people in Vietnam: evidence from a project evaluation. PLoS One. 2013;8(11):e80951.
Oldenburg CE, Biello KB, Colby D, et al. Engagement with peer health educators is associated with willingness to use pre-exposure prophylaxis among male sex workers in Ho Chi Minh City, Vietnam. AIDS Patient Care STDs. 2014;28(3):109–12.
Ministry of Health - Vietnam. Results from the HIV/STI integrated biological and behavioral surveillance (IBBS) in Vietnam -- round II 2009. Hanoi; 2011. Available from: https://www.aidsdatahub.org/sites/default/files/documents/Vietnam_IBBS_Round_II_2009.pdf. Cited 17 Mar 2017.
Des Jarlais DC, Thi Huong D, Thi Hai Oanh K, et al. Prospects for ending the HIV epidemic among persons who inject drugs in Haiphong, Vietnam. Int J Drug Policy. 2016;32:50–6.
Ministry of Health - Vietnam. Results from the 2006 Integrated biological and behavioral survey (IBBS) in Vietnam. 2007. Available from: https://www.aidsdatahub.org/sites/default/files/documents/Results_from_the_from_the_IBBS_in_Vietnam_2006.pdf.pdf. Cited 16 Mar 2017.
Noar SM, Cole C, Carlyle K. Condom use measurement in 56 studies of sexual risk behavior: review and recommendations. Arch Sex Behav. 2006;35(3):327–45.
Meyer DZ, Avery LM. Excel as a qualitative data analysis tool. Field Methods. 2009;21(1):91–112.
Hoang D, Dinh AT, Groce N, Sullivan LE. Knowledge and perceptions of HIV-infected patients regarding HIV transmission and treatment in Ho Chi Minh City, Vietnam. Asia Pac J Public Health. 2015;27(2):NP746–57.
Liu Y, Osborn CY, Qian HZ, et al. Barriers and facilitators of linkage to and engagement in HIV care among HIV-positive men who have sex with men in China: a qualitative study. AIDS Patient Care STDs. 2016;30(2):70–7.
Mayer KH. Introduction: linkage, engagement, and retention in HIV care: essential for optimal individual- and community-level outcomes in the era of highly active antiretroviral therapy. Clin Infect Dis. 2011;52(Suppl 2):S205–7.
Thanh DC, Hien NT, Tuan NA, et al. HIV risk behaviours and determinants among people living with HIV/AIDS in Vietnam. AIDS Behav. 2009;13(6):1151–9.
US Agency for International Development, Commonwealth Regional Health Community Secretariat for East, Central and Southern Africa. HIV/AIDS Voluntary Counselling and Testing: Review of Policies, Programmes and Guidelines in East, Central and Southern Africa 2002. Available from: https://www.who.int/hiv/topics/vct/toolkit/components/policy/review_of_policies_programmes_and_guidelines.pdf. Cited 22 Feb 2017.
Kurth AE, Lally MA, Choko AT, Inwani IW, Fortenberry JD. HIV testing and linkage to services for youth. J Int AIDS Soc. 2015;18(2 Suppl 1):19433.
Tsegay G, Edris M, Meseret S. Assessment of voluntary counseling and testing service utilization and associated factors among Debre Markos university students, north West Ethiopia: a cross-sectional survey in 2011. BMC Public Health. 2013;13:243.
Ngo AD, Ratliff EA, McCurdy SA, et al. Health-seeking behaviour for sexually transmitted infections and HIV testing among female sex workers in Vietnam. AIDS Care. 2007;19(7):878–87.
The Body. Vietnam fails to prevent spread of HIV among sex workers. Available from: https://www.thebody.com/article/vietnam-fails-prevent-spread-hiv-among-sex-workers. Accessed 15 Mar 2017.
RMIT Vietnam News. The condom taboo. Available from: https://www.rmit.edu.vn/news/condom-taboo. Accessed 16 Mar 2017.
Kumar GA, Dandona R, Poluru R, et al. Patterns of condom use by men who have sex with men before and after the Avahan intervention in Andhra Pradesh state of India. BMC Public Health. 2014;14:64.
Goswami P, Rachakulla HK, Ramakrishnan L, et al. An assessment of a large-scale HIV prevention programme for high-risk men who have sex with men and transgenders in Andhra Pradesh, India: using data from routine programme monitoring and repeated cross-sectional surveys. BMJ Open. 2013;3:e002183. https://doi.org/10.1136/bmjopen-2012-002183. It is available at: https://bmjopen.bmj.com/content/bmjopen/3/4/e002183.full.pdf.
Reza-Paul S, Beattie T, Syed HU, et al. Declines in risk behaviour and sexually transmitted infection prevalence following a community-led HIV preventive intervention among female sex workers in Mysore, India. AIDS. 2008;22(Suppl 5):S91–100.
Vu NT, Holt M, Phan HT, et al. The prevalence and correlates of HIV and undiagnosed infection among men who have sex with men in Hanoi, Vietnam: findings from a cross-sectional, biobehavioral study. Front Public Health. 2016;4:275.
Girault P, Green K, Clement NF, et al. Piloting a social networks strategy to increase HIV testing and counseling among men who have sex with men in Greater Accra and Ashanti region, Ghana. AIDS Behav. 2015;19(11):1990–2000.
Green K, Girault P, Wambugu S, Clement NF, Adams B. Reaching men who have sex with men in Ghana through social media: a pilot intervention. Digit Cult Educ. 2014; Available from: https://www.popline.org/node/624666. Accessed 7 Aug 2019.
USAID and FHI 360. Facebook over face-to-face time: using social media to access hard-to reach populations of men who have sex with men in Ghana. 2014. Available from: https://www.fhi360.org/resource/facebook-over-face-face-time-using-social-media-access-hard-reach-populations-men-who-have. Accessed 7 Aug 2019.
Shalizi CR, Thomas AC. Homophily and contagion are generically confounded in observational social network studies. Sociol Methods Res. 2011;40(2):211–39.
Acknowledgements
We thank Ahmar Hashmi, Wayland Bergman, Bill MacLeod, and Deirdre Pierotti for their technical advice and assistance. We also acknowledge the Vietnamese government officials who provided their support and assistance to this project. We are grateful to our exceptional team of data collectors in Vietnam based at the Ho Chi Minh City Statistical Office and to the the many individuals in Vietnam who provided information by participating in a survey or interview.
Funding
This work was supported by the Hanoi Mission of the US Agency for International Development through the Country Research Activity GHS-A-00-03-00020 to Boston University. The opinions expressed herein are those of the authors and do not necessarily reflect the views of the U.S. Agency for International Development.
Author information
Authors and Affiliations
Contributions
LLS conceived of the study, led the design and interpretation of findings, and played the lead role in drafting the manuscript; MD, LTTL, DHH, TMH, and TV participated in the design of the study and interpretation of findings; KS, MD, and JT did the statistical and qualitative analyses and participated in interpretation of findings; JJB, NH, MR, and AM contributed to the interpretation of findings and helped draft the manuscript. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study protocol was approved by the Institutional Review Boards of Boston University Medical Center, the Hanoi School of Public Health, and the HCMC AIDS Committee. All participants provided written informed consent.
Consent for publication
Our study protocol and informed consent form (signed by all participants) included language stating that confidentiality would be protected to the greatest degree possible, and that no individual’s identifiable data would be published or used in conference abstracts, teaching materials, etc. This manuscript contains no individual identifiable data. Data are either provided by study group, or in the case of qualitative data, identified only by key population and city or province.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Sabin, L.L., Semrau, K., DeSilva, M. et al. Effectiveness of community outreach HIV prevention programs in Vietnam: a mixed methods evaluation. BMC Public Health 19, 1130 (2019). https://doi.org/10.1186/s12889-019-7418-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-019-7418-5