Abstract
Background
Limited evidence exists to inform physical activity (PA) and sedentary behavior guidelines for older people, especially women. Rigorous evidence on the amounts, intensities, and movement patterns associated with better health in later life is needed.
Methods/Design
The Objective PA and Cardiovascular Health (OPACH) Study is an ancillary study to the Women’s Health Initiative (WHI) Program that examines associations of accelerometer-assessed PA and sedentary behavior with cardiovascular and fall events. Between 2012 and 2014, 7048 women aged 63–99 were provided with an ActiGraph GT3X+ (Pensacola, Florida) triaxial accelerometer, a sleep log, and an OPACH PA Questionnaire; 6489 have accelerometer data. Most women were in their 70s (40%) or 80s (46%), while approximately 10% were in their 60s and 4% were age 90 years or older. Non-Hispanic Black or Hispanic/Latina women comprise half of the cohort. Follow-up includes 1-year of falls surveillance with monthly calendars and telephone interviews of fallers, and annual follow-up for outcomes with adjudication of incident cardiovascular disease (CVD) events through 2020. Over 63,600 months of calendar pages were returned by 5,776 women, who reported 5,980 falls. Telephone interviews were completed for 1,492 women to ascertain the circumstances, injuries and medical care associated with falling. The dataset contains extensive information on phenotypes related to healthy aging, including inflammatory and CVD biomarkers, breast and colon cancer, hip and other fractures, diabetes, and physical disability.
Discussion
This paper describes the study design, methods, and baseline data for a diverse cohort of postmenopausal women who wore accelerometers under free-living conditions as part of the OPACH Study. By using accelerometers to collect more precise and complete data on PA and sedentary behavior in a large cohort of older women, this study will contribute crucial new evidence about how much, how vigorous, and what patterns of PA are necessary to maintain optimal cardiovascular health and to avoid falls in later life.
Clinical trials registration
ClinicalTrials.gov identifier NCT00000611. Registered 27 October 1999.
Similar content being viewed by others
Background
Due to their longevity advantage, women outnumber men in later life [1]. By the year 2060, the number of women ages 65 years and older in the United States (US) is estimated to be 52.7 million [2]. Despite their greater longevity, women have more morbidity and disability than men [3], resulting in higher frequency of outpatient visits and hospitalizations, use of long-term care services, and health care expenditures [4–6].
Regular physical activity (PA) provides remarkable health benefits for older adults, including reducing the risk of mortality, developing many chronic diseases, functional limitations, and fall-related injuries [7]. The 2008 PA Guidelines for Americans recommends that adults of all ages get a minimum of 150 min per week of moderate-intensity aerobic activity [7], however, accelerometer-measured PA data estimated that only 2% of older Americans met this guideline [8] and they sat up to 11 h per day [9–11]. Women, especially older women, were underrepresented in the evidence reviewed to derive these guidelines. This paper describes the study design, methods, and baseline data for a diverse cohort of postmenopausal women in the “Objective PA and Cardiovascular Health in Older Women” (OPACH) Study [R01 HL105065; PI: A LaCroix]. This study will contribute crucial new evidence about how much, how vigorous, and what patterns of PA are necessary to maintain optimal cardiovascular health in later life and whether PA levels are associated with incident falls.
Methods
Study population
The Women’s Health Initiative, Extension Studies and Long Life Study
The OPACH Study is an ancillary study to the WHI study, a major National Institutes of Health (NIH) research program that began in the early 1990s. Postmenopausal women ages 50 to 79 years were enrolled in the WHI Clinical Trials or the Observational Study from 40 clinical sites throughout the US from 1993 to 1998. Details about WHI have been extensively described [12, 13]. Protocols were approved by institutional review boards at participating institutions and all women gave written informed consent. WHI participants continue to be followed annually for disease events, changes in functional status, and death through the main program that ended in 2005, and three Extension Studies (2005–2010; 2010–2015; 2015–2020). Enrollment in the Extension Studies required that eligible women (alive and willing to be contacted) provide informed consent for continued follow-up in WHI. In the first Extension, 76.9% of 150,075 eligible women consented to further follow-up. In the second Extension, 86.8% of 107,706 eligible women consented to further follow-up without a defined end date.
The WHI Long Life Study was conducted during the second WHI Extension Study among a subcohort of 7,875 WHI participants from March 2012 to May 2013 from all 40 original US clinical centers in their homes to collect new data to support research on factors associated with healthy aging and changing levels of biomarkers of CVD risk. Data collection included a brief clinical assessment (height, weight, waist circumference, blood pressure, and pulse), assessment of functional status (Short Physical Performance Battery (SPPB), [14, 15] and grip strength), and phlebotomy.
A total of 7,048 WHI women who consented to participate in both the Long Life Study and the OPACH study were provided with an ActiGraph GT3X+ (Pensacola, Florida) triaxial accelerometer, a sleep log, and an OPACH PA Questionnaire (Additional file 1) between March 2012 and April 2014 either during the home visit or via express mail afterwards.
Cardiovascular disease outcomes
The primary outcomes for the OPACH Study are total cardiovascular disease (CVD) events and total mortality. WHI Extension Study participants are mailed forms annually to ascertain updates to their medical history. Medical records are obtained for reported outcomes and adjudicated by trained study physicians. Definitions of CVD outcomes are described in detail elsewhere [16] and summarized in Table 1. Deaths are ascertained when a family member informs the WHI staff, and through National Death Index searches and obituary notices. Participants are followed until they die, are lost-to-follow-up, or request no further contact. Vital status was known for 98% of women as of the end of 2014. Causes of death are determined based on available medical records, autopsy reports, and the death certificate in a blinded fashion by local and central physician adjudicators.
OPACH falls surveillance and data collection
To monitor safety, the OPACH study conducted surveillance on incident falls for one year after accelerometry and collected information about all injuries and fall-related injuries that required medical care. Incident falls were ascertained using a 13-month calendar distributed to OPACH participants to record daily if they had a fall (“no fall” or “yes, I fell”). Calendar pages were sent back monthly, data were entered and dates of reported falls were tracked. Participants were mailed a reminder postcard if calendars were not returned and, if a woman lost or misplaced any calendar pages, a new calendar was sent. The first month of each woman’s calendar corresponded to the month that she wore the accelerometer. Falls surveillance began in March 2012 and was completed in March 2015.
When a fall was reported on a calendar page, participants were interviewed by telephone about the circumstances of the fall, including events leading up to the fall, physical activities (both leisure and non-leisure) engaged in at the time of the fall, location of the fall (inside or outside of the home), whether injuries resulted and, if so, the body region and type of injury (particularly, any fractures), and the highest level of medical care received for all injuries. For women who fell multiple times within a month, data collection was limited to the first two injury falls and first two non-injury falls. Participants could be contacted multiple times if they reported falling on more than one calendar page over the 13-month follow-up period. Due to limited resources, beginning in April 2013, interviews were conducted among 100% of falls reported by the most physically active women - defined as those in the highest quintile (≥21 MET-hours/week) of self-reported total recreational PA - and 20% of falls reported from all other women were selected to be interviewed [17].
As shown in Fig. 1, 6,580 women received a 13-month calendar for falls surveillance, of whom, 6,118 (93%) returned an accelerometer with usable data. Of these, 5,776 (94%) women returned at least 1 month of calendar pages and 4,246 (69%) women returned 12–13 months of calendar pages. Among the over 63,600 pages of calendar months returned, 5,980 falls were reported and 3,375 of these falls were sent for interviews. A total of 2,577 (76%) fall interviews were completed from 1,492 women, 416 (28%) of whom were among the most physically active. Reasons that fall interviews were not completed included that the participant did not remember falling, could not be contacted, refused the interview, or was deceased.
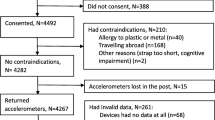
Accelerometer data collection
The hip-worn accelerometer was placed at the iliac crest and secured with a belt. Women were asked to wear the accelerometer for 7 days during both waking and sleeping hours, except when bathing or swimming, starting the day after they complete their home visit or received their mailed package. To isolate sleeping time, participants recorded time in and out of bed on the OPACH sleep log [18]. The accelerometer was preset to begin data collection at a specified date and time. The device provided no feedback to the participant about their PA. As shown in Fig. 2, 6,721 (95%) women returned their accelerometers and of these, 6,489 (92%) had some data for analysis. The 569 women who did not return accelerometers with usable data were somewhat more likely to be African-American, had poorer self-reported health, lower physical function scores, higher levels of depressive symptoms and higher prevalence of past cardiovascular disease, but were less likely to report a fall in the past year when compared to the women with accelerometer data.
Accelerometer data processing
Accelerometer data were measured and saved at a rate of 30 times per second (i.e., at 30 hertz). When devices were returned from participants, the data were downloaded and saved for long-term storage. Over the data collection phase of the study, the ActiGraph software (ActiLife) versions 6.0.0 to 6.101 were used. Data were processed using ActiLife Firmware v2.4 and the activity counts for the three orthogonal axes at which acceleration was measured were output for every 15-s epoch using the normal frequency filter mode and the low frequency filter mode, separately. Data from the three axes were used to compute the vector magnitude (VM) by taking the square root of the sum of the vertical axis squared, the anterior-posterior axis squared, and the medial-lateral axis squared.
A computer-based automated algorithm, in alignment with the sleep logs and visual inspection, was used to identify the window of days with the maximum amount wear over a consecutive 7 day period [18]. When available, the sleep log data were used to identify periods when the participant reported being out of bed (vs. in bed). To maximize the use of accelerometer data when sleep logs were missing or were suspected to have reporting error, mean values for in-bed and out-of-bed times were imputed for each participant if at least one day of sleep log data were recorded. Population mean in-bed and out-of-bed times were used for women with no sleep log data. Automated methods for identifying in-bed periods are currently being explored [19, 20].
Accelerometer non-wear was defined by an interval of at least 90 consecutive minutes of zero VM counts per minute, with allowance for 2-min windows including nonzero VM counts as long as no counts were detected during the 30 min upstream and downstream of each window and that the cumulative duration of consecutive upstream and downstream zeros were ≥90 min [21, 22]. Any nonzero VM counts (except the allowed short intervals) were considered wear time.
An adherent day was defined as ≥10 h of accelerometer wear time during periods the participant was out-of-bed.
Covariate data collection
The OPACH PA Questionnaire [see Additional File 1] was completed by women in their homes and mailed back to the WHI Clinical Coordinating Center for data entry. Table 2 (below) summarizes the measures included in the questionnaire and the origin of validated scales.
The health status of OPACH participants has been extensively and continuously characterized since their WHI enrollment in 1993–1998. Information was collected by interview and/or self-administered questionnaires for all participants on age, race/ethnicity, education, age at menopause, hormone therapy use, medication use (e.g., statins, lipid-lowering drugs, antihypertensive drugs), treated diabetes, personal and parental history of major chronic diseases, and physical functioning using the RAND SF-36 instrument [23]. A medication inventory was collected by mail just prior to the start of the Long Life Study.
As part of the Long Life Study protocol, a fasting blood draw was collected during the participant’s home visit. Biomarkers (glucose, insulin, creatinine, high-sensitivity C-reactive protein, high and low density lipoprotein cholesterol, triglyceride, total cholesterol) were measured at the University of Minnesota. Of the 7,875 Long Life Study participants, 7,325 (93%) have biomarker data available. Of these, 5,100 (70%) participated in the OPACH study.
OPACH calibration study
No standard was available to classify intensity of PA, and to distinguish sedentary behavior from light PA, using accelerometer data in older adults. Therefore, we conducted a separate laboratory-based calibration study in women ages 60 to 91 years to determine accelerometer count cutpoints that best distinguish levels of PA volume intensity in older women. Details of the calibration study design and results have been published previously [24].
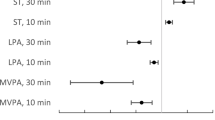
Traditional accelerometer cutpoints were found to be too high for older women resulting in PA being underestimated [11, 25]. Traditional cutpoints were derived using vertical axis accelerometer counts, so Fig. 3a and b present OPACH vertical axis count cutpoints to allow for accurate comparisons. Figure 3a displays two different vertical axis count cutpoints for light intensity PA in OPACH calibration study participants. The traditional cutpoint for sedentary behavior of <100 counts per minute on the vertical axis [10] results in more light intensity PA minutes being misclassified as sedentary (false negatives) causing an underestimation of light intensity PA minutes and overestimation of sedentary minutes among OPACH participants. Similarly, Fig. 3b shows that the vertical axis count cutpoint for moderate-to-vigorous PA (MVPA) from the calibration study (> = 1320 counts/minute) was lower than a commonly used cutpoint (> = 1952 counts/minute) [26]. Again, using the higher cutpoint would cause an underestimation of MVPA for women in the OPACH study.
The OPACH Calibration Study reported intensity cutpoints derived from different methods of analyzing the data [24]. OPACH chose the method that defined a MET as 3.0 ml/kg/min and with data processed using the normal frequency filter, where cutpoints were derived by balancing false positive and false negatives. A MET value of 3.0 ml/kg/min is slightly lower than the traditionally defined value of 1 MET = 3.5 ml/kg/min, but better reflects observed resting energy expenditure of older adults studied with indirect calorimetry [24, 27, 28]. This resulted in the categorization of PA intensity as shown in Table 3 .
Baseline characteristics
Table 4 describes demographic, health behavior and health status characteristics by four age groups for the 6,489 women with accelerometer data. Most women were in their 70s (40%) or 80s (46%), while approximately 10% were in their 60s and 4% were age 90 years or older. Non-Hispanic Black and Hispanic/Latina women represented half of the sample and were generally younger than the Non-Hispanic White women in the study. Physical functioning, measured both through the RAND SF-36 survey [23] and the SPPB test [14], decreased as age increased. Likewise, self-reported PA levels decreased across incremental age groups. As women aged, they were more likely to have fallen in the past year and were more concerned about falling in the future. Average resting systolic blood pressure (SBP) was higher as age increased; however, average resting diastolic blood pressure, waist circumference, weight, and body mass index (BMI) were lower.
Of the 6,489 women with accelerometer data, 6,126 wore the accelerometer while out of bed for at least 4 days for at least 10 h each day. Table 5 shows the characteristics of adherent women by quartiles of average VM counts per 15-s epoch. Consistent with the self-reported PA levels in Table 4, younger women had higher levels of PA. White women were more likely (30%) to be in the lowest PA quartile compared with Black women (24%) and Hispanic/Latina women (13%). Women in the highest quartile of PA had a higher frequency of excellent or very good self-rated health (33 vs. 16% among women in the lowest quartile of PA) and of not falling in the past year. Furthermore, physical functioning and self-reported PA were higher and average SBP, waist circumference, weight, and BMI were lower among women in the highest quartile of PA.
Discussion
The OPACH Study is one of the first, large prospective studies in older women to measure PA objectively using a state-of-the-science triaxial accelerometer. The cohort is unique in its diversity (2,187 Non-Hispanic Black and 1,097 Hispanic/Latina women) and in the richness of adjudicated CVD, cancer, hip fracture and other outcomes. Moreover, physical function, activities of daily living disability, quality of life, and incident hospitalizations are being measured annually through at least the year 2020.
The OPACH study will address gaps in knowledge about PA, falls, and fall-related injuries. Injuries are the most common adverse event from participation in PA [7]. However, evidence is limited about how overall risk of major injuries requiring medical care depends upon level of PA [29]. Despite an extensive literature on exercise and falls in older adults [30], there are no data quantifying fall and fall-related injury risk in relation to accelerometer-measured PA in older women. RCT data clearly show that exercise programs reduce risk of falls in older adults [7], but it is unknown whether these programs might increase risk of other types of injury, for example, through increased exposure to road traffic as an exercising pedestrian. Observational data in older populations performing their usual activities (as opposed to a supervised intervention) are needed to characterize more completely both the benefits and risks of PA, particularly the habitual low levels of PA not typically captured by self-reported questionnaires.
The OPACH Calibration study results clearly showed that traditional cutpoints underestimate the amount of MVPA and overestimate sedentary time in older women [24]. Although we are providing novel information on age and gender appropriate intensity cutpoints for PA, we were unable to design a study that would provide individualized “relative-intensity” cutpoints that account for individual cardiorespiratory fitness. This is an important direction for future research. Our capture of raw accelerometer data in this large population is leading to novel uses of that go beyond defining intensity levels to capture types of PA (walking, sit-to-stand transitions, standing time) using machine-learning algorithms [31], latent class patterns of PA and sedentary behavior, and other inventive summaries. We strongly recommend the capture and storage of raw accelerometer data in all future studies so that new strategies for analyzing the data can be further developed and employed.
The OPACH Study is a cost-effective approach to creating an unparalleled dataset for understanding the health benefits of PA for older women. Our primary objectives focus first on CVD health and falls in older women. However, the addition of accelerometer data to the WHI Program will have tremendous value in studying other phenotypes related to healthy aging, including inflammatory biomarkers, breast and colon cancer, diabetes, and physical disability.
References
U.S. Department of Health and Human Services, Health Resources and Services Administration. Women’s Health USA 2013. Rockville: U.S. Department of Health and Human Services; 2013. [http://mchb.hrsa.gov/whusa13/dl/pdf/whusa13.pdf], Accessed 03 May 2015.
U.S. Census Bureau. National population projections: summary tables. 2014. [https://www.census.gov/population/projections/data/national/2014/summarytables.html] Accessed 02 Apr 2015.
Crimmins EM, Beltran-Sanchez H. Mortality and morbidity trends: is there compression of morbidity? J Gerontol B Psychol Sci Soc Sci. 2011;66(1):75–86.
Harris-Kojetin L, Sengupta M, Park-Lee E, Valverde R, Caffrey C, Rome V, et al. Long-term care providers and services users in the United States: data from the national study of long-term care providers, 2013–2014. National center for health statistics. Vital Health Stat 3. 2016;38(38):1–118.
Rice DP. Older women’s health and access to care. Women’s Health Issues. 2000;10(2):42–6.
Spillman BC, Lubitz J. The effect of longevity on spending for acute and long-term care. N Engl J Med. 2000;342(19):1409–15.
U.S. Department of Health and Human Services. Physical Activity Guidelines for Americans. Washington, DC: U.S. Dept. of Health and Human Services; 2008.
Tucker JM, Welk GJ, Beyler NK. Physical activity in U.S.: adults compliance with the physical activity guidelines for Americans. Am J Prev Med. 2011;40(4):454–61.
Dunlop DD, Song J, Arnston EK, Semanik PA, Lee J, Chang RW, et al. Sedentary time in US older adults associated with disability in activities of daily living independent of physical activity. J Phys Act Health. 2015;12(1):93–101.
Matthews CE, Chen KY, Freedson PS, Buchowski MS, Beech BM, Pate RR, et al. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol. 2008;167(7):875–81.
Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–8.
Design of the Women’s Health Initiative clinical trial and observational study. The Women’s Health Initiative Study Group. Control Clin Trials. 1998; 19(1):61–109.
Anderson GL, Manson J, Wallace R, Lund B, Hall D, Davis S, et al. Implementation of the women’s health initiative study design. Ann Epidemiol. 2003;13(9 Suppl):S5–17.
Guralnik JM, Ferrucci L, Pieper CF, Leveille SG, Markides KS, Ostir GV, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci. 2000;55(4):M221–31.
Simonsick EM, Newman AB, Nevitt MC, Kritchevsky SB, Ferrucci L, Guralnik JM, et al. Measuring higher level physical function in well-functioning older adults: expanding familiar approaches in the health ABC study. J Gerontol A Biol Sci Med Sci. 2001;56(10):M644–9.
Curb JD, McTiernan A, Heckbert SR, Kooperberg C, Stanford J, Nevitt M, et al. Outcomes ascertainment and adjudication methods in the women’s health initiative. Ann Epidemiol. 2003;13(9 Suppl):S122–8.
Meyer AM, Evenson KR, Morimoto L, Siscovick D, White E. Test-retest reliability of the women’s health initiative physical activity questionnaire. Med Sci Sports Exerc. 2009;41(3):530–8.
Rillamas-Sun E, Buchner DM, Di C, Evenson KR, LaCroix AZ. Development and application of an automated algorithm to identify a window of consecutive days of accelerometer wear for large-scale studies. BMC Res Notes. 2015;8:270.
McVeigh JA, Winkler EAH, Healy GN, Slater J, Eastwood PR, Straker LM. Validity of an automated algorithm to identify waking and in-bed wear time in hip-worn accelerometer data collected with a 24-hour wear protocol in young adults. Physiol Meas. 2016. (in press).
Tracy DJ, Xu Z, Choi L, Acra S, Chen KY, Buchowski MS. Separating bedtime rest from activity using waist or wrist-worn accelerometers in youth. PloS One. 2014;9(4):e92512.
Choi L, Liu Z, Matthews CE, Buchowski MS. Validation of accelerometer wear and nonwear time classification algorithm. Med Sci Sports Exerc. 2011;43(2):357–64.
Choi L, Ward SC, Schnelle JF, Buchowski MS. Assessment of wear/nonwear time classification algorithms for triaxial accelerometer. Med Sci Sports Exerc. 2012;44(10):2009–16.
Ware Jr JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–83.
Evenson KR, Wen F, Herring AH, Di C, LaMonte MJ, Tinker LF, Lee IM, et al. Calibrating physical activity intensity for hip-worn accelerometry in women age 60 to 91 years: The women’s health initiative OPACH calibration study. Prev Med Rep. 2015;2:750–6.
Evenson KR, Buchner DM, Morland KB. Objective measurement of physical activity and sedentary behavior among US adults aged 60 years or older. Prev Chronic Dis. 2012;9:E26.
Freedson PS, Melanson E, Sirard J. Calibration of the Computer Science and Applications, Inc accelerometer. Med Sci Sports Exerc. 1998;30(5):777–81.
Hall KS, Howe CA, Rana SR, Martin CL, Morey MC. METs and accelerometry of walking in older adults: standard versus measured energy cost. Med Sci Sports Exerc. 2013;45(3):574–82.
Kozey S, Lyden K, Staudenmayer J, Freedson P. Errors in MET estimates of physical activities using 3.5 ml x kg(−1) x min(−1) as the baseline oxygen consumption. J Phys Act Health. 2010;7(4):508–16.
Buchner DM, Campbell AJ. Inactivity as a risk factor for activity-related injuries. Am J Prev Med. 2010;39(1):102–3.
Sherrington C, Whitney JC, Lord SR, Herbert RD, Cumming RG, Close JC. Effective exercise for the prevention of falls: a systematic review and meta-analysis. J Am Geriatr Soc. 2008;56(12):2234–43.
Kerr J, Marshall SJ, Godbole S, Chen J, Legge A, Doherty AR, et al. Using the SenseCam to improve classifications of sedentary behavior in free-living settings. Am J Prev Med. 2013;44(3):290–6.
Lee IM, Sesso HD, Oguma Y, Paffenbarger Jr RS. Relative intensity of physical activity and risk of coronary heart disease. Circulation. 2003;107(8):1110–6.
Wisen AG, Farazdaghi RG, Wohlfart B. A novel rating scale to predict maximal exercise capacity. Eur J Appl Physiol. 2002;87(4–5):350–7.
Gibbs BB, Reis JP, Schelbert EB, Craft LL, Sidney S, Lima J, et al. Sedentary screen time and left ventricular structure and function: the CARDIA study. Med Sci Sports Exerc. 2014;46(2):276–83.
Rosenberg DE, Norman GJ, Wagner N, Patrick K, Calfas KJ, Sallis JF. Reliability and validity of the Sedentary Behavior Questionnaire (SBQ) for adults. J Phys Act Health. 2010;7(6):697–705.
Kempen GI, Yardley L, van Haastregt JC, Zijlstra GA, Beyer N, Hauer K, et al. The short FES-I: a shortened version of the falls efficacy scale-international to assess fear of falling. Age Ageing. 2008;37(1):45–50.
Cummings SR, Nevitt MC, Kidd S. Forgetting falls. The limited accuracy of recall of falls in the elderly. J Am Geriatr Soc. 1988;36(7):613–6.
Berrigan D, Troiano RP. The association between urban form and physical activity in U.S. adults. Am J Prev Med. 2002;23(2 Suppl):74–9.
Saelens BE, Sallis JF, Black JB, Chen D. Neighborhood-based differences in physical activity: an environment scale evaluation. Am J Public Health. 2003;93(9):1552–8.
Stewart AL, Mills KM, King AC, Haskell WL, Gillis D, Ritter PL. CHAMPS physical activity questionnaire for older adults: outcomes for interventions. Med Sci Sports Exerc. 2001;33(7):1126–41.
Acknowledgments
The authors acknowledge the following investigators in the WHI Program: Program Office: (National Heart, Lung, and Blood Institute, Bethesda, Maryland) Jacques E. Rossouw, Shari Ludlam, Dale Burwen, Joan McGowan, Leslie Ford, and Nancy Geller Clinical Coordinating Center: Women’s Health Initiative Clinical Coordinating Center: (Public Health Sciences, Fred Hutchinson Cancer Research Center, Seattle, WA) Garnet L. Anderson, Ross L. Prentice, Andrea Z. LaCroix, and Charles L. Kooperberg Investigators and Academic Centers: (Brigham and Women’s Hospital, Harvard Medical School, Boston, MA) JoAnn E. Manson; (MedStar Health Research Institute/Howard University, Washington, DC) Barbara V. Howard; (Stanford Prevention Research Center, Stanford, CA) Marcia L. Stefanick; (The Ohio State University, Columbus, OH) Rebecca Jackson; (University of Arizona, Tucson/Phoenix, AZ) Cynthia A. Thomson; (University at Buffalo, Buffalo, NY) Jean Wactawski-Wende; (University of Florida, Gainesville/Jacksonville, FL) Marian C. Limacher; (University of Iowa, Iowa City/Davenport, IA) Robert M. Wallace; (University of Pittsburgh, Pittsburgh, PA) Lewis H. Kuller; (Wake Forest University School of Medicine, Winston-Salem, NC) Sally A. Shumaker. Women’s Health Initiative Memory Study: (Wake Forest University School of Medicine, Winston-Salem, NC) Sally A. Shumaker. For a list of all the investigators who have contributed to WHI science, please visit: https://www.whi.org/researchers/Documents%20%20Write%20a%20Paper/WHI%20Investigator%20Long%20List.pdf. Decisions concerning study design, data collection and analysis, interpretation of the results, the preparation of the manuscript, and the decision to submit the manuscript for publication resided with committees comprised of WHI investigators that included NHLBI representatives. The contents of the paper are solely the responsibility of the authors.
Funding
This work was supported by the National Heart, Lung, and Blood Institute, National Institutes of Health, U.S. Department of Health and Human Services (contracts HHSN268201100046C, HHSN268201100001C, HHSN268201100002C, HHSN268201100003C, HHSN268201100004C, and HHSN271201100004C) and National Heart, Lung and Blood Institute (grant R01HL105065).
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available now, but will be made available in approximately 2018 after the main study results have been published. Data will be accessible through our established data sharing policies described at https://www.whi.org/SitePages/WHI%20Home.aspx. Until that time, the data are available from the corresponding author on reasonable request.
Authors’ contributions
All authors participated in selected portions or all of the planning, design and execution of the study protocol described in this manuscript. AZL drafted this manuscript in close collaboration with all co-authors, each of whom have reviewed, edited, and approved of the final manuscript.
Competing interests
No potential conflicts of interest have been reported by any author of this manuscript.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The study was reviewed and approved by the Fred Hutchinson Cancer Research Center Institutional Review Board (Protocol 3467-EXT), Seattle, WA, USA. All participants provided informed consent either in writing, or via a telephone-based consent process.
Author information
Authors and Affiliations
Corresponding author
Additional files
Additional file 1:
OPACH PA Questionnaire. (DOCX 351 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
LaCroix, A.Z., Rillamas-Sun, E., Buchner, D. et al. The Objective Physical Activity and Cardiovascular Disease Health in Older Women (OPACH) Study. BMC Public Health 17, 192 (2017). https://doi.org/10.1186/s12889-017-4065-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-017-4065-6