Abstract
Background
Tuberculosis (TB) is a global concern for both developing and developed countries. Currently it becomes more complex due to increasing levels of drug resistance and HIV co-infection. Delayed diagnosis and high case load are major factors contributing to continued transmission and failure to the treatment outcome. The study was conducted to determine the profile and treatment outcomes of TB patients at Felege-Hiwot Referral Hospital.
Methods
We analyzed the records of 1761 TB patients registered for treatment in Felege Hiwot Referral Hospital from July 2010 to June 2015. Data on patients’ socio-demographic characteristics, type of TB, HIV status and treatment outcome were analysed. Descriptive statistics and binary logistic regression models were used to present data. The odds ratio and the 95 % confidence intervals were calculated. A p-value of < 0.05 was considered statistical significant.
Results
The proportion of smear positive, smear-negative and extra-pulmonary TB were 205 (11.6 %), 548 (31.1 %) and 1008 (57.2 %), respectively. The overall treatment success rate accounts 542(80.8 %) with unsuccessful treatment of 129(19.2 %). The treatment outcome varied by the years from 68.9 to 97.4 %. Among tuberculosis patients, 459(26.1 %) of them were HIV positive. Being HIV positive (AOR = 4.29, 95 % CI, 2.20–8.37 P = 0.001), retreatment (AOR = 5.32, 95 % CI, 1.92–14.3, P = 0.001), rural residency (AOR = 18.0, 95 % CI, 9.06–37.82, P = 0.001) and the age group of 15–24 years (AOR = 2.91, 95%CI, 1.00–8.45, P = 0.04) showed statistical significant association for poor treatment outcome.
Conclusions
In the studied region, the overall treatment success rate was still below the WHO target of success rate, 85 %. However, the trend of treatment success rate showed a promising increment. Patients at high risk of unsuccessful treatment outcome should be identified early and given additional follow-up, medical intervention and social support.
Similar content being viewed by others
Background
Tuberculosis (TB) is a global concern and recently it becomes more complex due to increasing levels of drug resistance and HIV co-infection [1]. Developing countries, like Ethiopia, have high burden of TB, one of the most serious public health challenges [2]. An increased incidence of TB is found mostly in Africa and Asia, where the highest prevalence of co-infection with HIV is reported [3, 4]. Ethiopia is highly affected by TB and it is ranked 7th among the 22 high TB burden countries by the world health Organization (WHO) [5]. In developing countries, there is high burden of TB and HIV, delayed diagnosis which is a major contributing factor to the continued transmission and failure to the treatment outcome [6]. Patient non-adherence to the anti-TB treatment is also interpreted as a failure of the health care system [7].
Currently, Ethiopia reports treatment success and case detection rates of 83 and 62 % of all forms of TB, respectively (8). The TB control program in Ethiopia introduced the standardized Directly Observed Treatment, Short Course (DOTS) as a pilot programme in 1992 and at Felege Hiwot Referral Hospital in 2000. The standardized DOTS/Stop TB Strategy geographical coverage reached at 100 %. Moreover, at the health facility level, it reached 95 % [8]. However, reports showed that the treatment outcome of TB patients treated under the DOTS program was unsatisfactory [9]. Reports showed that several factors such as male sex, age ≥ 65 years, drug resistance, HIV co-infection, previously treated TB cases and cavitation affect treatment success rate [10–16]. In addition, various social, behavioral, and economic characteristics have been found to be associated with lower treatment success rate [14, 15]. Although the purpose of TB treatment is curing the patient, preventing the spread of TB infection and preventing the emergence of new drug resistant strains, these plans are not achieved in Ethiopia. There is a limited report on the DOTS experiences in Northwest Ethiopia. This study is aimed at evaluating the treatment outcome and associated risk factors for new smear positive pulmonary TB (PTB+), extra pulmonary TB (EPTB) and smear negative pulmonary TB (PTB-) cases registered at Felege-Hiwot Referral Hospital (FHRH) DOTS programme.
Methods
Study design, period and population
With a cross sectional retrospective study, all patients diagnosed and treated during the period of July 2010 to June 2015 at FHRH were included in the study to assess TB profile and treatment outcome. The hospital is found in Bahir Dar, the capital city of Amhara National Regional State, which is located 565 km away from Addis Ababa. The current TB diagnosis and treatment strategy in Ethiopia is the stop TB or DOTS strategy. Sputum samples were collected using spot-morning-spot strategy and other clinical samples were collected depending on the site of infection. The collected clinical specimens were examined using the standard Ziehl-Neelsen (ZN) acid fast bacilli (AFB) staining technique, Fluorescent Microscopy (FM) or GeneXpert MTB/RIF assay [8]. Moreover, imaging and pathological techniques might have been used for those PTB- and EPTB cases before being admitted to DOTS programme. For those diagnosed with new active TB, the standard TB treatment regimen such as, 2 months of intensive treatment with Rifampicin, Isoniazid, Pyrazinamide and Ethambutol (2RHZE) followed by 4 months of continuation phase with Rifampicin and Isoniazid (4RH). Likewise for those retreated cases, the intensive phase contains 2 months of streptomycin and the combination of HRZE drugs (2S (HRZE)) and additional 1 month of treatment without streptomycin; 1 (HRZE). Then the continuation phase contains 5 months of treatment with the combination of RH and E; 5 (HR) E [17, 18].
Human immunodeficiency virus test
The anti-HIV antibody test was used for the screening of HIV/AIDS and it was done according to the manufacturer’s instruction (rapid test currently used in national algorithm for Ethiopia; KHB, Shanghai Kehua Bio-engineering Co., Ltd. China) for screening and positive samples were re-tested with STAT-PACK (Chembio HIV 1/2 STAT-PAK™ Assay, CHEMBIO DIAGNOSTIC SYSTEMS, INC., MEDFORD, NY, USA). Samples giving discordant results in the two tests were re-examined using the tiebreaker (Uni-Gold HIV, Trinity Biotech PLC, Co. Wicklow, Ireland).
Operational definitions
According to the standard definitions of the National Tuberculosis and Leprosy Control Program guideline (NLCP) adopted from the WHO [19], the following clinical case and treatment outcome definitions were used:
-
Cured: A patient with bacteriologically confirmed pulmonary TB at the beginning of treatment who was smear or culture-negative in the last month of treatment
-
Treatment completed: A patient with TB who completed treatment without evidence of failure, but with no record of sputum smear or culture results, in the last month of treatment.
-
Successful treatment outcome: If PTB patients were cured (i.e., negative smear microscopy at the end of treatment and on at least one previous follow-up test) or completed treatment with resolution of symptoms.
-
Unsuccessful treatment outcome: If treatment of PTB/EPTB/ patients resulted in treatment failure (i.e., remaining smear-positive after 5 months of treatment), default (i.e., patients who interrupted their treatment for two consecutive months or more after registration), or death.
-
Died: A TB patient who died from any cause during treatment.
-
Failure: A TB patient whose sputum smear or culture is positive at month 5 or later during treatment.
-
Lost to follow-up: A TB patient whose treatment was interrupted for two consecutive months or more.
-
Pulmonary TB, smear-positive: A patient with at least two sputum specimens which were positive for AFB by microscopy, or a patient with only one sputum specimen which was positive for AFB by microscopy, and chest radiographic abnormalities consistent with active pulmonary TB.
-
Pulmonary TB, smear-negative: A patient with symptoms suggestive of TB, with at least two sputum specimens which were negative for AFB by microscopy, and with chest radiographic abnormalities consistent with active pulmonary TB (including interstitial or miliary abnormal images), or a patient with two sets of at least two sputum specimens taken at least two weeks apart, and which were negative for AFB by microscopy, and radiographic abnormalities consistent with pulmonary TB and lack of clinical response to one week of broad spectrum antibiotic therapy.
-
Extra pulmonary TB: This included TB of organs other than the lungs, such as lymph nodes, abdomen, genitourinary tract, skin, joints and bones, meninges, etc. Diagnosis of EPTB was based on fine needle aspiration cytology or biochemical analyses of cerebrospinal/pleural/ascitic fluid or histopathological examination or strong clinical evidence consistent with active EPTB, followed by a decision of a clinician to treat with a full course of anti-tuberculosis chemotherapy. In all the cases of EPTB, sputum examinations and chest radiographs were used to investigate the involvement of lung parenchyma.
Inclusion and exclusion criteria
All TB patients with complete data like age, sex, treatment outcome were included. Missing of either of these variables were the exclusion criteria.
Data collection and tools
Demographic and clinical data such as age, sex, type of TB, TB treatment outcome, status of HIV infection, Co-trimoxazole prophylaxis (CPT) and antiretroviral therapy (ART) status were retrieved from TB registry using data extraction sheet.
Data analysis
All data were entered in to Epi Info 3.1 and analysed using SPSS statistical software package (IBM Corp. Released 2011. IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp.). Descriptive statistics was used to determine differences within the data of variables. All explanatory variables with a p value ≤0.2 in the bivariate analysis were included in the multivariate logistic regression model to identify independent predictive variables. Odds ratio (OR) and 95 % confidence intervals (CI) were calculated and the results were considered statistically significant at p < 0.05.
Results
Socio demographic characteristics of patients
A total of 1761 patients’ document has been reviewed. Of which 1054 (59.9 %) were males. The highest numbers of study participants were urban dwellers, 1142 (64.8 %). The mean age of the study subjects was 28.11 (SD. ±14.25). The proportion of smear positive, smear-negative and extra-pulmonary TB was 205 (11.6 %), 548 (31.1 %) and 1008 (57.2 %), respectively. The age group 15–34 years accounted more than half of the study subjects and the peak age group of 15–24 years presented about one-third of the total TB patients, (Table 1).
Tuberculosis treatment outcomes
Of the total TB patients, 1090 (61.9 %) were transferred out to other health facilities. Thus, their treatment outcome status were not known and excluded from the treatment outcome analysis. Of the total TB patients with known treatment outcome, the treatment success rate was 542(80.8 %) with unsuccessful treatment of 129(19.2 %). The unsuccessful treatment outcomes shared to 30(4.5 %) defaulted, 98(14.6 %) died and 1(0.001 %) failed. Among all TB patients, 459(26.1 %) of them were sero-positive for HIV/AIDS (Table 1). The majority of TB patients who have unsuccessful treatment outcome were among HIV positive patients, 70 (38.7 %) (Fig. 1). The death rate of PTB+, PTB- and EPTB were 13(13.3 %), 29(29.6 %) and 56(57.1 %), respectively (Table 1).
Trend of tuberculosis treatment outcomes
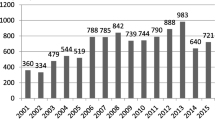
Over a period of 5 years, the treatment outcomes under DOTS program of TB patients varied from years to years. The successful treatment outcomes from 2010 to 2012 were decreased from 83.3 to 68.9 %. But, from 2013 onwards it showed an increase of successful treatment outcomes from 80.1 to 97.4 %. The detail information is described in Fig. 2.
Factors associated with TB treatment success rate
In the multivariate logistic regression model, HIV positive TB patients were about 4 times more likely to have unsuccessful TB treatment than whose sero-status was unknown (AOR = 4.29, 95 % CI, 2.20–8.37 P = 0.001), while a decreased treatment success rate was observed with the patients’ age group 15–24 years (AOR = 2.91, 95 % CI, 1.00–8.45, P = 0.04). Furthermore, a lower treatment success rate was documented among retreated TB patients (AOR = 5.32, 95 % CI, 1.92–14.3, P = 0.001). On the other hand, patients from urban areas had a significantly higher treatment success rate compared to cases from rural locations (AOR = 18.0, 95 % CI, 9.06–37.82, P = 0.001) (Table 2).
Discussion
In our study with the microscopically confirmed TB cases in FHRH DOTS clinic, we observed a successful outcome of TB treatment in 80.8 % of the patients, which is less than the target level set by the WHO for successful outcomes of 85 %. However, it is comparable to the national report of the successful outcome of TB treatment in Ethiopia (83 %) [8]. Moreover the treatment success rate among the 22-high TB burden countries varied from 60 to 93 %, with an average of 83 % [4, 8, 20]. On the other hand, our finding is still below other findings reported in Tigray, Ethiopia, 89.2 % [21] and in Spain, 89 % [22]. But the treatment success in our study was better than the studies conducted in Southern Ethiopia, 49 % [23], and Finland, 70.1 % [24].
The treatment success rate was poor in 2010–2012, although a prominent improvement was observed in 2013–2015. This improvement could be due to an improved access to TB control services, particularly community-based interventions, the expansion of TB treatment centers and a regimen change of the continuation phase to RH, which lasts 4 months. This finding is supported by the study conducted at the Southern Ethiopia [25].
The proportion of PTB+, PTB− and EPTB were 205 (11.6 %), 548 (31.1 %) and 1008 (57.2 %), respectively. This is in line with other studies reported elsewhere in the country [9, 21, 26, 27]. However, the vice versa result has been declared from Gambella region [28]. The high level of EPTB in this study might be due to the over diagnosis of EPTB using clinical data, imaging and pathologic evidence. Moreover, the large number of PTB− and EPTB cases might be due to the high proportion of TB - HIV co-infection which is quite common among these patients in a high TB and HIV burden setting [29].
Unsuccessful treatment outcome was more frequent (AOR = 5.32, 95 % CI, 1.92–14.3, P = 0.001) among retreated cases than among those newly treated. This was similar to the study conducted in Tigray region, Ethiopia [21]. Among TB patients, the majority of them were EPTB cases and the most unsuccessful outcome of TB treatment at (23.2 %) was observed in these patients.
In this study, the proportion of TB/HIV co-infection was found to be 459 (26.0 %). The majority of HIV positive patients (29.9 %) were among PTB- patients, indicating that HIV testing before treatment is crucial. This finding was higher than the study conducted in India [30]. However, previous studies conducted at Gondar University Hospital showed that high proportions (52.5 %) of TB patients were co-infected with HIV. [31, 32]. Moreover, multivariate logistic regression analysis showed that, being HIV positive was one of the independently associated risk factor for poor treatment outcome (AOR = 4.29, 95 % CI, 2.20–8.37, P = 0.001). This finding was in agreement to other study in Zimbabwe [33]. This might be due to the low level of immunity and drug mal-absorption among HIV patients. This is supported by other studies [27, 34, 35]. Our results indicate the necessity of strengthening interventions to reduce TB-HIV co-infection in the study region.
It is well studied that retreated patients are more vulnerable for the development of MDR-TB and poor treatment outcome [36]. In our finding, unsuccessful treatment outcome was higher among retreated TB cases than new TB patients (AOR = 5.32, 95 % CI, 1.92–14.3, P = 0.001). Similar finding was declared from the study conducted in South India [37]. Rural residence was also significantly associated with the poor treatment outcome of TB patients (AOR = 18.0, 95 % CI, 9.06–37.82, P = 0.001). The same finding was reported by Hailu MD et al. [25]. This might be due to awareness differences between rural and urban populations. Tuberculosis patients in the age group 15–24 years were more likely for the unsuccessful treatment outcome than other age group (AOR = 2.91, 95 % CI, 1.00–8.45, P = 0.04). However, Berhe G et al. in 2012 [21] and Tessema et al. in 2009 [9] reported different pattern. This finding is unusual and it is recommended to be more studied. In this study, there was no difference in success rates by sex. This was also supported by other studies conducted elsewhere in Ethiopia [21, 38].
In this study, we observed a default rate at 4.5 %, which was found to be lower compared to other studies in Ethiopia, 18 % [9], Switzerland, 16 % [39], Germany, 10 % [40], and Sweden, 7 % [41]. In Ethiopia a standardized TB prevention and control programme is incorporating DOTS. This might be one of the reasons for the smaller proportions of default rate in this study. However, the presence of default is a major public health problem that the patients may remain infectious and even develop MDR-TB.
Conclusions
In conclusion, the overall treatment success rate in the current study (80.8 %) was still below the WHO target of success rate (85 %). However, the prominent improvement has been observed in 2013–2015. In the studied region, HIV-TB co-infection, young age (15–24 years), rural residence and retreatment of patients were found to be predictors for the poor treatment outcome. Based on our finding, we recommend that patients at high risk of unsuccessful treatment outcome should be identified early and given additional follow-up, medical intervention and social support.
References
Vijay S, Kumar P, Chauhan LS, Narayan Rao SV, Vaidyanathan P. Treatment outcome and mortality at one and half year follow-up of HIV infected TB patients under TB control programme in a district of South India. PLoS ONE. 2011;6(7):e21008.
WHO. Global tuberculosis report 2013. In: WHO/HTM/TB/2013.11. Geneva: World Health Organization; 2013.
Issar S. Mycobacterium tuberculosis pathogenesis and molecular determinants of virulence. J Clin Microbiol. 2003;16:463–96.
World Health Organization. Global tuberculosis control: surveillance, planning, and Financing. Geneva: World Health Organization; 2008. http://apps.who.int/bookorders/anglais/detart1.jsp?codlan=1&codcol=15&codcch=3659. Accessed 28 July 2016.
World Health Organization. Global tuberculosis control: Surveillance, planning and financing. WHO report. WHO/HTM/TB/2008.393 (2008). Geneva: World Health Organization; 2008.
Tsai K, Chang H, Chien S, Chen K, Chen K, Mai M, Chen K. Childhood tuberculosis: epidemiology, diagnosis, treatment, and vaccination. Pediatr Neonato. 2013;54(5):295–302.
Sumartojo E. When tuberculosis treatment fails. A social behavioral account of patient adherence. Am Rev Respir Dis. 1993;147:1311–20.
Federal Ministry of Health. Overview of National TB Control Implementation status. Gondar: Sixth National TB Research Workshop, Gondar University, 6–8 June 2011; 2011.
Tessema B, Muche A, Bekele A, Reissig D, Emmrich F, Sack U. Treatment outcome of tuberculosis patients at Gondar University Teaching Hospital, Northwest Ethiopia. A five - year retrospective study. BMC Public Health. 2009;9:371.
Antoine D, French CE, Jones J, Watson JM. Tuberculosis treatment outcome monitoring in England, Wales and Northern Ireland for cases reported in 2001. J Epidemiol Community Health. 2007;61:302–7.
Farah MG, Tverdal A, Steen TW, Heldal E, Brantsaeter AB, Bjune G. Treatment outcome of new culture positive pulmonary tuberculosis in Norway. BMC Public Health. 2005;5:14.
Lefebvre N, Falzon D. Risk factors for death among tuberculosis cases: analysis of European surveillance data. Eur Respir J. 2008;31:1256-260.
Bao OS, Du YH, Lu CY. Treatment outcome of new pulmonary tuberculosis in Guangzhou, China 1993–2002: a register-based cohort study. BMC Public Health. 2007;7:344.
Garrido MS, Penna ML, Perez-Porcuna TM, et al. Factors associated with tuberculosis treatment default in an endemic area of the Brazilian Amazon: a case control-study. PLoS One. 2012;7(6):e39134.
Wobeser W, Yuan L, Naus M, and the Tuberculosis Treatment Completion Study Group. Outcome of pulmonary tuberculosis treatment in the tertiary care setting - Toronto 1992/93. CMAJ. 1999;160:789–94.
World Health Organization (WHO). Global Tuberculosis Control. WHO Report. WHO/CDS/TB/20012001, 2001;287:1–181.
Lawn D, Zumla I. Tuberculosis. Lancet. 2011;378:57–72.
Federal Democratic Republic of Ethiopia. Ministry of Health. Guideline for Clinical and Programmatic Management of TB, Leprosy and TB/HIV in Ethiopia. Addis Ababa, Ethiopia 2012. www.etharc.org/resources/download/finish/33/709. Accessed 13 May 2015.
Ministry of Health of Ethiopia (MOH). Tuberculosis, Leprosy and TB/HIV Prevention and Control Programme Manual. 4th ed. Addis Ababa: MOH; 2008.
Boogaard VJ, Lyimo R, Irongo CF, Boeree MJ, Schaalma H, Aarnoutse RE, Kibiki GS. Community vs facility-based directly observed treatment for tuberculosis in Tanzania’s Kilimanjaro Region. Int J Tuberc Lung Dis. 2009;13(12):1524–9.
Berhe G, Enquselassie F, Aseffa A. Treatment outcome of smear-positive pulmonary tuberculosis patients in Tigray Region, Northern Ethiopia. BMC Public Health. 2012;12:537.
Joan AC, Rodrigo T, Ruiz-Manzano J, et al. Tuberculosis treatment adherence and fatality in Spain. Respir Res. 2009;10:121.
Shargie EB, Lindtjørn B. DOTS improves treatment outcomes and service coverage for tuberculosis in South Ethiopia: a retrospective trend analysis. BMC Public Health. 2005;5:1471–7.
Vasankari T, Holmström P, Ollgren J, Liippo K, Kokki M, Ruutu P. Risk factors for poor tuberculosis treatment outcome in Finland: a cohort study. BMC Public Health. 2007;7:291.
Hailu MD, Gemechu DD, Lindtjørn B. Trends of tuberculosis case notification and treatment outcomes in the Sidama Zone, Southern Ethiopia: ten-year retrospective trend analysis in urban rural settings. PLoS ONE. 2014;9(12):e114225.
World Health Organization. Global tuberculosis report. WHO/HTM/TB/2014.08 (2014). Geneva: WHO; 2014.
Hailu D, Erku WA, Belay M. Childhood tuberculosis and its treatment outcomes in Addis Ababa: a 5-years retrospective study. BMC Pediatr. 2014;14:61.
Sisay S, Mengistu B, Erku W, et al. Directly Observed Treatment Short-course for tuberculosis control program in Gambella Regional State, Ethiopia: ten years’ experience. BMC Res Notes. 2014;7:44.
World Health Organization. Global Tuberculosis Control - Epidemiology, Strategy, Financing. Geneva: World Health Organisation; 2009.
Manjareeka M, Nanda S. Prevalence of HIV infection among tuberculosis patients in Eastern India. J Infect Public Health. 2013;6(5):358–62.
Kassu A, Mengistu G, Ayele B, Diro E, Mekonnen F, Ketema D, Moges F, Mesfin T, Getachew A, Ergicho B, Elias D, Aseffa A, Wondmikun Y, Ota F. Coinfection and clinical manifestations of tuberculosis in human immunodeficiency virus- infected and –uninfected adults at a teaching hospital, northwest Ethiopia. J Microbiol Immunol Infect. 2007;40:116–22.
Zenebe Y, Anagaw B, Tesfay W, Debebe T, Gelaw B. Smear positive extra pulmonary tuberculosis disease at University of Gondar Hospital, Northwest Ethiopia. BMC Res Notes. 2013;6:21.
Gabida M, Tshimanga M, Chemhuru M, Gombe N, Bangure D. Trends for Tuberculosis Treatment Outcomes, New Sputum Smear Positive Patients in Kwekwe District, Zimbabwe, 2007–2011: A Cohort Analysis. J Tuberc Res. 2015;3:126–35.
Dingeta TA, Abdosh TA. Risk factors for unsuccessful tuberculosis treatment outcome (failure, default and death) in public health institutions, Eastern Ethiopia. Pan Afr Med J. 2015;20:247.
Tweya H, Feldacker C, Phiri S, Ben-Smith A, Fenner L, Jahn A, Kalulu M, Weigel R, Kamba C, Banda R, Egger M, Keiser O. Comparison of Treatment outcomes of new smearpositive pulmonary tuberculosis patients by HIV and antiretroviral status in a TB/HIV clinic. Malawi PLOS ONE. 2013;8(2):e56248.
Choi H, Lee M, Chen RY, et al. Predictors of pulmonary tuberculosis treatment outcomes in South Korea: a prospective cohort study, 2005–2012. BMC Infect Dis. 2014;14:360.
Ananthakrishnan R, Kumar K, Ganesh M, Kumar AMV, Krishnan N, et al. The Profile and Treatment Outcomes of the Older (Aged 60 Years and Above) Tuberculosis Patients in Tamilnadu, South India. PLoS ONE. 2013;8(7):e67288.
Endris M, Moges F, Belyhun Y, Woldehana E, Esmael A, Unakal C. Treatment Outcome of Tuberculosis Patients at Enfraz Health Center, Northwest Ethiopia: A Five-Year Retrospective Study. Tuberc Res Treat. 2014;2014:Article ID 726193. doi:10.1155/2014/726193.
Zellweger JP, Coulon P. Outcome of patients treated for tuberculosis in Vaud County, Switzerland. Int J Tuberc Lung Dis. 1998;2:372–7.
Diel R, Nieman S. Outcome of tuberculosis treatment in Hamburg: a survey, 1997–2001. Int J Tuberc Lung Dis. 2003;7:124–31.
Romanus V, Julander I, Blom-Bulow B, Larsson LO, Normann B, Boman G. Shortages in Swedish tuberculosis care. Good results only in 71 percent of cases after 12-month treatment as shown in a current study [in Swedish]. Läkartidningen. 2000;97:5613–6.
Acknowledgements
We the authors forward deep appreciation to Amhara National Regional Health Bureau Research and technology department for approving the proposal. Moreover, we also thank FHRH TB clinic staffs for their support during data collection.
Funding
There was no specific grant from any funding agency. We the authors were extensively involved on each activity of the research work.
Availability of data and materials
The findings of this study is generated from the data collected and analyzed based on the stated methods and materials. The original data supporting this finding will be available at any time up on request.
Authors’ contributions
YZ was the primary researcher, YZ, DM, FB, YA, AD, DH conceived, designed the study, analysis and interpretation of data and drafting the manuscript. YZ, DM, AD, MB, FB participated in sample collection, data analysis, interpretation of the results, YZ wrote the manuscript, and FB, BT, AD reviewed the initial and final drafts of the manuscript. All authors read and approved the final manuscript.
Competing interest
The authors declare that they have no competing interests.
Consent for publication
Even though there is no individual data details like images or videos, consent to publish this manuscript was obtained from the organization.
Ethics approval and consent to participate
Institutional ethical permission was obtained from Amhara Regional Ethical Review Committee, Bahir Dar Ethiopia. We followed all chains of command to get support letter from legally authorized representatives to the study subjects’ data. Moreover, the legally authorized representatives were not member of the study and gave the consent with support letter intended to promote the health of the target population. By the retrospective nature of the study, it was impossible to obtain written/informed consent from the subject directly. However, the patients’ data were not identified by name. The registry data were collected serially, kept confidential and used for the purpose of the study only. After clearing the data, numbers have been removed and participants were de-identified prior to analysis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Zenebe, Y., Adem, Y., Mekonnen, D. et al. Profile of tuberculosis and its response to anti-TB drugs among tuberculosis patients treated under the TB control programme at Felege-Hiwot Referral Hospital, Ethiopia. BMC Public Health 16, 688 (2016). https://doi.org/10.1186/s12889-016-3362-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-016-3362-9