Abstract
Background
Colour Doppler analysis of ophthalmic vessels has been proposed as a promising tool in the diagnosis of various eye diseases, but the available diagnostic evidence has not yet been assessed systematically. We performed a comprehensive systematic review of the literature on the diagnostic properties of Colour Doppler imaging (CDI) assessing ophthalmic vessels and provide an inventory of the available evidence.
Methods
Eligible papers were searched electronically in (Pre) Medline, Embase and Scopus, and via cross-checking of reference lists. The minimum requirement to be included was the availability of original data and the possibility to construct a two-by-two table. Study selection, critical appraisal using the QUADAS II instrument and extraction of salient study characteristics was made in duplicate. Sensitivity and specificity was computed for each study.
Results
We included 11 studies (15 two-by-two tables) of moderate methodological quality enrolling 820 participants (range 30 to 118). In 44.4% participants were female (range 37–59% in specific subgroups). CDI was assessed for internal carotid stenosis, diabetic retinopathy, glaucoma, and branch or central retinal vein occlusion diagnosis. There was insufficient data to pool the results for specific illnesses. For the assessments of ophthalmic arteries, mean sensitivity was 0.69 (range 0.27–0.96) with a corresponding mean specificity of 0.83 (range 0.70–0.96). Mean sensitivity of the central retinal artery assessments was 0.58 (range 0.31–0.84) and the corresponding mean specificity was 0.82 (range 0.63–0.94).
Conclusions
Robust assessments of the diagnostic value of colour Doppler analysis remain uncommon, limiting the possibilities to extrapolate its true potential for clinical practice.
PROSPERO 2014:CRD42014014027.
Similar content being viewed by others
Background
Colour Doppler analysis of ophthalmic vessels has been proposed as a promising tool in the diagnosis of various eye diseases [1]. Colour Doppler imaging (CDI) enables ophthalmologists to examine ocular blood flow, even in presence of dense ocular opacities preventing a direct view to the posterior eye segment [2]. Compared to fluorescein angiography (FA), CDI allows for assessing the ocular blood flow in a non-invasive manner. Numerous studies have examined changes in ocular blood flow velocities in various diseases affecting the eye such as carotid artery and retinal vein occlusion, diabetic retinopathy (DRP) and glaucoma, and have revealed significant differences compared to healthy subjects even in early stages of disease (reviewed in [3, 4]). As an example, Evans and colleagues [5] demonstrated that diabetic patients with minimal or no retinopathy demonstrate irregular flow levels in the major vessels feeding the eye.
However, despite several potential benefits, CDI has not accomplished to make the leap into daily ophthalmic routine. Inter-observer variability issues could be a possible explanation [6]. Although updated assessment protocols have enhanced CDI inter-observer variability performance, [7] this remains a limiting factor for implementation in daily clinical use. Another problem relates to the fact that evidence on diagnostic accuracy is scattered among the various clinical fields and presumably not easy to access. For this reason we performed a comprehensive systematic review of the diagnostic literature on ophthalmic Doppler analysis, with special reference to the diagnostic merits of the technique, and provide an inventory of the available evidence.
Methods
This review has been conducted according to the PRISMA statement recommendations. The review protocol has been registered on Prospero [8] (PROSPERO 2014:CRD42014014027).
Literature search
An information specialist performed electronic searches without any language restrictions on (pre)MEDLINE (PubMed interface), Scopus and Embase (Ovid-Interface). The full search algorithms for the three databases are provided in the Appendix. Searches were performed on the 11th November 2014 and updated on the 4th of May 2016.
Eligibility criteria
We excluded studies assessing only healthy subjects, animal studies and studies without primary focus on eye diseases. We included case-control and cohort studies. The minimum requirement was the availability of original data and the possibility to construct a two-by-two table. We accepted the following reference tests classifying disease presence: carotid angiography, carotid ultrasound, fundoscopy, Humphrey visual field analyser, fluorescein angiography and Heidelberg retina optical coherence tomography.
Study selection, data extraction and quality assessment
Based on the QUADAS II criteria all eligible papers were judged for their quality using four suggested domains (patient selection, index test, reference standard and flow and timing) [9]. The instrument assesses the risk of bias of each domain. Moreover, the analysis of patient selection, the index test and the reference test examine the extent of applicability. The tool is broadly applied to standardise the rating of bias and to weigh applicability of diagnostic accuracy studies. We followed the recommendations of Whiting and colleagues [9] and refrained from rating or ranking of studies. Two reviewers independently read and assessed papers and extracted data using a standardized data abstraction form. Discrepancies were resolved by consensus between the two reviewers.
Statistical analysis
For each study, we constructed a two-by-two contingency table consisting of true-positive (TP), false-positive (FP), false-negative (FN), and true-negative (TN) results. For the analysis, we called a result a true positive if the CDI finding was concordant and in agreement with the reference standard findings. We calculated sensitivity as TP/(TP + FN) and specificity as TN/(FP + TN).
Meta- analysis
Formal pooling was only planned if at least four studies reported accuracy parameters for the diagnosis of a specific illness. However, in an exploratory meta-analysis of sensitivity and specificity using a multilevel mixed-effects logistic regression model (metandi command in Stata), we calculated diagnostic summary estimates mainly of the resistance index measured either in the ophthalmic or the central retinal artery irrespective of the underlying condition. This was done to gain an overall impression about the discriminatory potential of the technology rather than to inform clinical practice.
All analyses were done using the Stata 14.1 statistical software package (StataCorp. 2015. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP.).
Results
Study selection
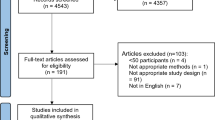
Electronic searches retrieved 3471 records. After excluding duplicates, 2239 records remained. Screening of titles and abstracts excluded 2224 studies as they did not investigate the diagnostic accuracy of tests, investigated other conditions, or contained no primary data. Full texts of fifteen articles were read. Five of these studies did not meet the inclusion criteria and were excluded. The ten remaining articles were completed by addition of another study found via the screening of reference lists. In total, thus, 11 studies were included in this systematic review. Figure 1 shows the study selection process.
Quality of included studies
We assessed the quality of the included studies using the QUADAS II tool considering four criteria (patient selection, index test, reference standard and flow and timing). The reference standard was appropriate in all selected trials, whereas flow and timing of the studies was inconsistent, mostly due to long periods of disease onset to performance of index- and reference tests. Most studies scored low for the items patient selection and rating of the index test. In case of patient selection this was partly due to a lack of age and sex matched study groups and partly due to not describing exclusion criteria. Low ratings regarding the index test were related to cut-off points that were not pre-specified and to the fact that not all investigators performed the index test being unaware of the diagnosis. Table 1 outlines the results of the quality assessment according to QUADAS II criteria.
Patients’ characteristics, design features
The 11 selected studies enrolled 820 patients. Among the studies which reported this, 44.4% of participants were women ranging from 11 to 75%. Study size ranged between 30 and 118 subjects. Four studies included patients consecutively. The most commonly described co-morbidities (other than the assessed illness) were hypertension and diabetes. Patients’ characteristics are summarized in Table 1.
Index and reference tests
Two studies assessed the possibility of a >75% or >80% internal carotid stenosis (ICS) diagnosis [10, 11]. Another two trials assessed the diagnosis of DRP. Whereas Arai et al. [12] examined the diagnosis of DRP among patients suffering from non-insulin-dependent diabetes, Basturk and colleagues [13] investigated the diagnosis of DRP in patients suffering from diabetes type II with microalbuminuria. Prediction of glaucoma progression was investigated in three studies two using the Humphrey field analyser and one the Heidelberg retina tomography as the reference test [14–16]. One study aimed to distinguish normal tension glaucoma from healthy eyes [17]. In another two studies, fluorescein angiography was set as the reference test assessing diagnosis of branch or central retinal vein occlusion (BRVO, CRVO) and diagnosis of ischemic CRVO respectively [18, 19]. Arséne et al. [18] aimed to distinguish eyes with CRVO from eyes with BRVO. Gonioscopy and slit lamp examination were set as reference tests in one study predicting iris vascularization 1 year after CRVO onset [6]. Table 2 shows the applied index and reference tests of each study.
Index test parameters assessed
Of the four studies assessing glaucoma, two used the resistive index (RI) to evaluate test accuracy of glaucoma progression [15, 16]. Another study used diastolic velocity to distinguish between normal tension glaucoma (NTG) and healthy eyes [6] and one study used a logistic discrimination function to predict the progression of glaucomatous damage [14]. Of the two studies assessing ICS, one used peak flow velocity [10] and one the RI [11]. Both studies examining the diagnostic value of CDI in DRP used RI as investigational parameter [12, 13]. Two studies assessing ischemia and neovascularization after CRVO, used the parameter “minimum velocity” [6, 19]. One study assessed the possibility to distinguish between CRVO and BRVO used the RI [18].
Test performance characteristics
Among studies assessing the ophthalmic artery (OA) flow, mean sensitivity was 0.69 (range 0.27–0.96) with a corresponding mean specificity of 0.83 (range 0.70–0.96), whereas for central retinal artery (CRA) flow measurements, mean sensitivity was 0.58 (range 0.31–0.84) with a corresponding specificity of 0.82 (range 0.63–0.94). The range of the number of eyes assessed in studies examining OA was 49 to 132, and 52 to 132 in studies assessing CRA. Assessments of the central retinal vein (CRV) reported sensitivities ranging from 0.67 to 0.75 and specificities of 0.65 to 0.86 in 30 and 69 eyes respectively. All test performance characteristics are outlined in Table 3.
Results from exploratory meta-analysis
Formal pooling of results for specific illnesses was impossible due to the limited number of studies. In the exploratory meta-analysis of studies investigating the OA across different illnesses, the pooled estimated sensitivity was 0.72 (95% CI; 0.52 to 0.86) with a corresponding specificity of 0.85 (95% CI; 0.76 to 0.90). The analysis of the CRA revealed a lower sensitivity of 0.58 (95% CI; 0.43 to 0.72) and a comparable specificity of 0.85 (95% CI; 0.74 to 0.91) (see Fig. 2).
Discussion
Main findings
The results of a small number of studies with only few patients suggest that the diagnostic value of colour Doppler analysis in ophthalmology is limited. Diagnostic performance varies considerably between studies illnesses with slightly better results when assessing the OA. Even though alterations of ocular blood flow could be used as a valuable tool in diagnosing ocular pathologies their acquisition remains a technical challenge and a no gold standard for assessment exists due to inherent limitations of the available techniques [4, 20]. Another problem in daily business is the lack of standardized methods in CDI assessment as Stalmans et al. already indicated [21]. Despite the vast amount of studies assessing ocular diseases, only a minority quantifies the CDI’s accuracy, impeding judgments regarding its value in the diagnostic work-up of ocular pathologies.
Results in context of existing literature
To our knowledge, this is the first comprehensive assessment of studies examining the diagnostic value of CDI in ocular diseases. We are aware of one meta-analysis of studies dealing with hemodynamic changes in ophthalmic artery and central retinal artery using CDI in Chinese patients with glaucoma [22]. However, this meta-analysis does not assess the diagnostic value using test accuracy data of CDI in glaucomatous patients [23]. In contrast to our findings, Dimitrova et al. [2] published a review stating CDI as a valuable tool in a wide range of ophthalmologic diseases for research and as a potentially useful diagnostic tool in the clinical setting. Although CDI appears to be a useful tool in the research of ocular blood flow changes, especially in glaucoma, diabetic retinopathy and age related macular degeneration [24–29], implementation in daily use as a diagnostic tool concerning the pathologies assessed in our study cannot be recommended yet.
Strengths and limitations
Our study applied up-to-date systematic review methodology, allowing a comprehensive description of the existing diagnostic literature on CDI test accuracy in ophthalmology. Due to the limited number of studies and the small number of participants in the included studies more upstream and formally sound (statistical) analyses were not feasible. We performed exploratory analyses to give an overview of the diagnostic performance of the CDI. However, the analysis has major limitations due to the mix of studies investigating different conditions and some methodological weaknesses of the underlying studies. Also, no analysis of the impact of different CDI systems on diagnostic performance could be performed due to the paucity of data. Hence we could not go beyond a mere description of the evidence.
Implications for further research
For successful implementation in clinical care, standards of CDI assessment need to be introduced to form the basis of a consistent assessment tool and to decrease the potential inter-rater reliability issues. There are promising results of altered ocular blood flow in common ocular diseases like diabetic retinopathy, age related macular disease and several forms of glaucoma [24, 27–31] and growing evidence showing that ocular blood flow alterations are associated with the development and progression of ophthalmologic diseases confirm the notion that abnormalities in vessel function exist before the development of structural changes occur. Considering this exciting point of view it seems promising to focus research of preclinical changes of ocular blood flow and prediction of progression of respective diseases. In order to fully understand underlying pathophysiological mechanisms and to offer timely treatments further studies are needed to fill in the current lack of knowledge.
Implications for practice
For the pathologies assessed in our analysis, implementation of CDI as a diagnostic tool in clinical practice does not seem helpful. Current available diagnostic tools like slit lamp examination, fluorescence angiography, visual field analysers and scanning laser polarimetry seem to be superior and more practicable compared with CDI. In case of glaucoma, the diagnosis relies on the assessment of intraocular changes occurring in the visual field, the optic nerve head, and the retinal nerve fibre layer. Perimetry is the current gold standard of progression as it enables the detection of small glaucomatous changes to the visual field. However, perimetry is limited by low diagnostic sensitivity in early stages of the disease [32] and there is a need for assessment techniques capable of detecting preclinical stages of the disease. In case of retinal vein occlusion fundoscopy and fluorescence angiography are satisfying diagnostic tools. However, predicting ischemic areas using alterations of ocular blood flow could be a valuable non-invasive tool. Regarding diabetic retinopathy, again, slit lamp examination and fluorescence angiography are valuable diagnostic tools superior to CDI. However, early detection of altered blood flow could improve implementation of therapy in early stages of the disease.
Conclusions
The possible role of colour Doppler analysis in routine ophthalmologic care remains unclear. The relative lack of robust assessments of the diagnostic value of colour Doppler analysis, limits the possibilities to extrapolate its true potential for clinical practice.
Abbreviations
- BRVO:
-
Branch vein occlusion
- CDI:
-
Colour Doppler imaging
- CRVO:
-
Central retinal vein occlusion
- DRP:
-
Diabetic retinopathy
- FA:
-
Fluorescein angiography
- FN:
-
False-negative
- FP:
-
False-positive
- HSROC:
-
Hierarchical summary receiver operating characteristics curve
- ICS:
-
Internal carotid stenosis
- NTG:
-
Normal tension glaucoma
- RI:
-
Resistive index
- TN:
-
True-negative
- TP:
-
True-positive
References
Tranquart F, Berges O, Koskas P, Arsene S, Rossazza C, Pisella PJ, Pourcelot L. Color Doppler imaging of orbital vessels: personal experience and literature review. J Clin Ultrasound. 2003;31(5):258–73.
Dimitrova G, Kato S. Color Doppler imaging of retinal diseases. Surv Ophthalmol. 2010;55(3):193–214.
Harris A, Kagemann L, Ehrlich R, Rospigliosi C, Moore D, Siesky B. Measuring and interpreting ocular blood flow and metabolism in glaucoma. Can J Ophthalmol. 2008;43(3):328–36.
Harris APS, Siesky B, Zore M, Tobe LA. Ophthalmic imaging of ocular circulation for detecting disease. Biomed Imaging. 2014;2014:163–85.
Evans DW, Harris A, Danis RP, Arend O, Martin BJ. Altered retrobulbar vascular reactivity in early diabetic retinopathy. Br J Ophthalmol. 1997;81(4):279–82.
Williamson TH, Baxter GM. Central retinal vein occlusion, an investigation by color Doppler imaging. Blood velocity characteristics and prediction of iris neovascularization. Ophthalmology. 1994;101(8):1362–72.
Nagahara M, Tomidokoro A, Sando S, Araie M, Tanaka S. An apparatus for color Doppler imaging in seated subjects. Am J Ophthalmol. 2002;133(2):270–2.
Bittner B, Faes L, Bachmann LM, Böhni SC, Howell J, Schmid MK. Diagnostic concepts to determine regional blood flow in ophthalmologic diseases: a systematic review. PROSPERO 2014:CRD42014014027 Available from http://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42014014027.
Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, Leeflang MM, Sterne JA, Bossuyt PM, Group Q. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155(8):529–36.
Hu HH, Sheng WY, Yen MY, Lai ST, Teng MM. Color Doppler imaging of orbital arteries for detection of carotid occlusive disease. Stroke. 1993;24(8):1196–203.
Paivansalo M, Riihelainen K, Rissanen T, Suramo I, Laatikainen L. Effect of an internal carotid stenosis on orbital blood velocity. Acta Radiol. 1999;40(3):270–5.
Arai T, Numata K, Tanaka K, Kiba T, Kawasaki S, Saito T, Satoh S, Sekihara H. Ocular arterial flow hemodynamics in patients with diabetes mellitus. J Ultrasound Med. 1998;17(11):675–81.
Basturk T, Albayrak R, Ulas T, Akcay M, Unsal A, Toksoy M, Koc Y. Evaluation of resistive index by color Doppler imaging of orbital arteries in type II diabetes mellitus patients with microalbuminuria. Ren Fail. 2012;34(6):708–12.
Jimenez-Aragon F, Garcia-Martin E, Larrosa-Lopez R, Artigas-Martin JM, Seral-Moral P, Pablo LE. Role of color Doppler imaging in early diagnosis and prediction of progression in glaucoma. Biomed Res Int. 2013;2013:871689.
Martinez A, Sanchez M. Predictive value of colour Doppler imaging in a prospective study of visual field progression in primary open-angle glaucoma. Acta Ophthalmol Scand. 2005;83(6):716–22.
Suprasanna K, Shetty CM, Charudutt S, Kadavigere R. Doppler evaluation of ocular vessels in patients with primary open angle glaucoma. J Clin Ultrasound. 2014;42(8):486–91.
Plange N, Kaup M, Weber A, Harris A, Arend KO, Remky A. Performance of colour Doppler imaging discriminating normal tension glaucoma from healthy eyes. Eye. 2009;23(1):164–70.
Arsene S, Giraudeau B, Le Lez ML, Pisella PJ, Pourcelot L, Tranquart F. Follow up by colour Doppler imaging of 102 patients with retinal vein occlusion over 1 year. Br J Ophthalmol. 2002;86(11):1243–7.
Tranquart F, Arsene S, Giraudeau B, Piquemal R, Eder V, Le Lez ML, Rossazza C, Pourcelot L. Initial color Doppler findings in retinal vein occlusion. J Clin Ultrasound. 2000;28(1):28–33.
Schmetterer L, Garhofer G. How can blood flow be measured? Surv Ophthalmol. 2007;52 Suppl 2:S134–8.
Stalmans I, Vandewalle E, Anderson DR, Costa VP, Frenkel RE, Garhofer G, Grunwald J, Gugleta K, Harris A, Hudson C, et al. Use of colour Doppler imaging in ocular blood flow research. Acta Ophthalmol. 2011;89(8):e609–30.
Meng N, Zhang P, Huang H, Ma J, Zhang Y, Li H, Qu Y. Color Doppler imaging analysis of retrobulbar blood flow velocities in primary open-angle glaucomatous eyes: a meta-analysis. PLoS One. 2013;8(5):e62723.
G Z: Meta-analysis of hemodynamic characteristics in ocular artery and central retinal artery of diabetic retinopathy. Int J Ophthalmol. 2007, 7:1049–1055.
Butt Z, O’Brien C, McKillop G, Aspinall P, Allan P. Color Doppler imaging in untreated high- and normal-pressure open-angle glaucoma. Invest Ophthalmol Vis Sci. 1997;38(3):690–6.
Dimitrova G, Tamaki Y, Kato S. Retrobulbar circulation in patients with age-related maculopathy. Eye. 2002;16(5):580–6.
Hosal BM, Karakoc G, Gursel E, Camur M. Color Doppler imaging of the retrobulbar circulation in age-related macular degeneration. Eur J Ophthalmol. 1998;8(4):234–8.
MacKinnon JR, McKillop G, O’Brien C, Swa K, Butt Z, Nelson P. Colour Doppler imaging of the ocular circulation in diabetic retinopathy. Acta Ophthalmol Scand. 2000;78(4):386–9.
Nicolela MT, Drance SM, Rankin SJ, Buckley AR, Walman BE. Color Doppler imaging in patients with asymmetric glaucoma and unilateral visual field loss. Am J Ophthalmol. 1996;121(5):502–10.
Rankin SJ. Color Doppler imaging of the retrobulbar circulation in glaucoma. Surv Ophthalmol. 1999;43 Suppl 1:S176–82.
Pemp B, Schmetterer L. Ocular blood flow in diabetes and age-related macular degeneration. Can J Ophthalmol. 2008;43(3):295–301.
Yilmaz Ovali G, Ersoy B, Tuncyurek O, Urk V, Ozkol M, Ozhan B, Baser E, Pabuscu Y. Doppler ultrasonography imaging of hemodynamic alteration of retrobulbar circulation in type 1 diabetic children and adolescents without retinopathy. Diabetes Res Clin Pract. 2008;79(2):243–8.
Harwerth RS, Carter-Dawson L, Shen F, Smith 3rd EL, Crawford ML. Ganglion cell losses underlying visual field defects from experimental glaucoma. Invest Ophthalmol Vis Sci. 1999;40(10):2242–50.
Availability of data and materials
All data supporting the findings are available in the paper.
Authors’ contributions
MB, LF, and SB: Acquisition and interpretation of data, LMB: analysis and interpretation of data, MKS, ROS: interpretation of data, LF, SB, MB, LMB: drafting the manuscript, MB, LF, SB, LMB, ROS, MKS: Critical revision for important intellectual content; and final approval of the version to be published.
Competing interests
The authors declare that they have no competing interest.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Not applicable.
Author information
Authors and Affiliations
Corresponding author
Appendix

Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Bittner, M., Faes, L., Boehni, S.C. et al. Colour Doppler analysis of ophthalmic vessels in the diagnosis of carotic artery and retinal vein occlusion, diabetic retinopathy and glaucoma: systematic review of test accuracy studies. BMC Ophthalmol 16, 214 (2016). https://doi.org/10.1186/s12886-016-0384-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-016-0384-0