Abstract
Introduction
This study aimed to determine whether there was any correlation between coronary artery disease (CAD) and retinal artery diameter at an academic tertiary medical center in Trinidad and Tobago.
Methods
This prospective study evaluated patients (n = 77) with recent invasive coronary angiography (CAG) and the Synergy between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery (SYNTAX) score who subsequently underwent optical coherence tomography–angiography (OCT–A) at the Eric Williams Medical Sciences Complex (EWMSC) from January 2021 to March 2021. Routine medical history and cardiovascular medications were also recorded. Spearman’s rank correlation coefficient and Mann–Whitney U-tests were used to compare correlations and medians between groups.
Results
The average patient age was 57.8 years old, with the majority being male [n = 55 (71.4%)] and of South Asian ethnicity [n = 53 (68.8%)]. Retinal artery diameter was negatively correlated with the SYNTAX score (−0.332 for the right eye, p = 0.003 and −0.237 for the left eye, p = 0.038). A statistically significant relationship was also demonstrated in females and diabetic patients. There were no serious adverse events (SAEs).
Conclusion
A significantly negative correlation was observed between retinal artery diameter and SYNTAX score. This study alludes to the practical use of optical coherence tomography–angiography (OCT–A) as a noninvasive diagnostic modality for patients with cardiovascular disease (CVD). Further large-scale, multicentric studies are required to confirm these exploratory findings.
Trial registration number
NCT04233619.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Currently, there is a paucity of data that correlates coronary artery disease (CAD) and retinal artery diameter among ethnic minorities within the Caribbean region. |
Recent studies have alluded to a bidirectional relationship between retinal microvasculature and incipient cardiovascular risk. |
What was learned from this study? |
Optical coherence tomography–angiography (OCT–A) may prove a feasible, noninvasive tool for patients with cardiovascular disease (CVD) in a limited-resource setting. |
Retinal artery diameter was negatively correlated with the SYNTAX score (−0.332 for the right eye, p = 0.003 and −0.237 for the left eye, p = 0.038). |
A statistically significant relationship was also demonstrated in females and diabetic patients. |
Introduction
Cardiovascular disease (CVD) is the leading cause of mortality globally, with an estimated 18 million deaths annually [1]. This significant disease burden requires intensive research and resource allocation into screening and risk stratification to enhance early detection and facilitate therapeutic intervention.
CVD was primarily ascribed to epicardial coronary artery disease (CAD); however, coronary microvascular dysfunction (CMD) also plays a crucial maladaptive role [2]. Current techniques to assess coronary microvascular perfusion are limited and fraught with challenges, such as being invasive and requiring the administration of stress agents or continuous monitoring [3].
Retinal microvasculature, however, can be easily visualized with a noninvasive technique, optical coherence tomography–angiography (OCT–A). Two recent studies have alluded to a bidirectional relationship between retinal microvasculature and incipient cardiovascular risk [6; 5]. Several scoring systems have been developed to angiographically estimate coronary artery disease (CAD) burden [6]. The Synergy between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery (SYNTAX) score was designed through expert consultation, and integrates previous angiographic scores that assess lesion complexity, and it is widely utilized [7, 8].
This study aimed to determine whether there was any correlation between CAD and retinal artery diameter at an academic tertiary medical center in Trinidad and Tobago.
Methods
Compliance with Ethics Guidelines
This study complied with the Declaration of Helsinki, the International Conference on Harmonization–Good Clinical Practice (ICH–GCP). Ethical approval was obtained from the Campus Research Ethics Committee (CREC) of the University of the West Indies, St. Augustine (UWI STA), at the Eric Williams Medical Sciences Complex (EWMSC) (CEC819/01/19). Signed informed consent was obtained from each participant. No rewards or incentives were given to encourage participation, nor were any penalties for declining participation.
Study Design and Patient Population
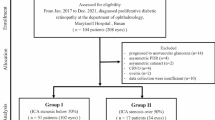
This was a prospective cross-sectional study of patients who underwent invasive coronary angiography (CAG) at the cardiac catheterization laboratory and OCT–A (within 1 month from index CAG) at the Eric Williams Medical Sciences Complex, Trinidad and Tobago, from January 2021 to March 2021. These patients (elective, urgent, and emergent) were referred to the cardiac catheterization laboratory for coronary angiography and included acute and chronic patients with acute coronary syndromes (ACS), chronic coronary syndromes (CCS) and heart failure (HF), and moderate–severe valvular heart disease (VHD). Routine medical history and cardiovascular medications were also recorded. Of note, ethnicity was self-reported at the time of CAG. Predefined selection criteria included patients ≥ 18 years with documented informed consent, while exclusion criteria comprised patients with severe cataracts, pregnancy, or those who declined participation.
Coronary Angiography
Patients underwent appropriately indicated coronary angiography (Allura Xper FD20, Philips Healthcare, Amsterdam, the Netherlands) as determined by an American Board of Internal Medicine (ABIM) certified interventional cardiologist who also calculated the Synergy between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery (SYNTAX) score after the procedure. These scores were calculated as previously described [9,10,11]. The general definition for obstructive CAD is heterogeneous; however, for this study, a luminal stenosis was defined as > 50% [12]. All participants were scheduled for an OCT–A (Triton plus, Topcon Healthcare, Tokyo, Japan) within 1 month of index CAG.
Optical Coherence Tomography–Angiography
The OCT–A was performed by a qualified ophthalmologist (credentialed by the certificate of completion of training CCT from the UK) and the retinal artery diameter was measured per the standard OCT–A technique utilized by Arnould et al.[4] They were followed-up 30 days later via telephone to assess whether they had experienced any SAEs.
Statistical Analysis
The sample size was calculated using the Massachusetts General Hospital Biostatistics Calculator based on the study performed by Arnould et al., which enrolled 237 patients [4, 5, 13]. The sample size was calculated as 77 patients based on a paired-proportion sample, an alpha (α) value of 0.05, a power (β) of 80%, and a correlation coefficient of 0.8. The study’s biostatistician performed routine statistical analyses with IBM SPSS Statistics version 27.0. Descriptive methods included percentage, frequency, and summary statistics. Continuous variables such as age, SYNTAX score, and retinal artery diameter were presented as means ± standard deviation. The SYNTAX score and retinal artery diameter were not normally distributed and showed skewed data; hence, the median values were used for analysis. Spearman’s rank correlation coefficient was used for correlations, and Mann–Whitney U-tests were done to compare medians between groups. All p-values were two-tailed, and a p-value of < 0.05 was accepted as statistically significant.
Results
A total of eighty (80) patients were approached for participation in the study, and seventy-seven (77) of them agreed to participate (Table 1). The average age of the sample was 57.8 years, ranging from 23 to 88 years (median age 60 years). There were more males [n = 55 (71.4%)] and South Asians [n = 53 (68.8%)]. The most common comorbidity was preexisting cardiovascular disease (CVD) [n = 64 (83.1%)] followed by hypertension (HTN) [n = 46 (59.7%)], dyslipidemia (HLD) [n = 36 (46.8%)], and diabetes mellitus (DM) [n = 33 (42.9%)]. SYNTAX scores ranged from 0 to 36, with a mean score of 12.0 (± 9.3) and a median of 11 (interquartile range 4.5–11). Right retinal artery diameter ranged from 146 to 313 μm with a mean of 196.83 μm (± 37.142 μm) and median of 188 μm. Left retinal artery diameter ranged from 24 to 471 μm with a mean of 193.45 μm (± 53.465 μm) and a median of 187 μm. A statistically significant negative correlation was observed between retinal artery diameter and SYNTAX score for both eyes among all participants (Fig. 1 and Table 2). This was also demonstrated for the female gender (Table 2). DM, insulin and oral hypoglycemic therapy and SYNTAX score were also found to have a significant relationship (p = 0.005, 0.015, and 0.006, respectively) (Table 3). No other comorbidities, such as hypertension and dyslipidemia, displayed a statistically significant relationship.
Discussion
The pathophysiology of acute coronary syndromes (ACS) was traditionally attributed to obstructive CAD, whereas CMD primarily results from architectural changes and endothelial dysfunction [2]. They can both co-occur due to shared incipient cardiovascular risk factors. CMD may accentuate inducible ischemia from epicardial CAD with sequelae of increased major adverse cardiovascular events (MACE) [2]. Emerging data support that CMD may affect other vascular territories due to similar caliber size [14]. Retinal artery atherosclerosis has been shown to correlate with CAD [15]. Previous studies have implied that viewing retinal artery microvasculature could be a looking glass for latent CAD, and be utilized in assessing cardiovascular risk [4, 5, 16]. The eye offers direct access to the microvasculature and through high-fidelity OCT–A, the retinal artery may be evaluated with high reproducibility [17, 18]. Several studies have demonstrated that changes in retinal vessel diameter reflect an accentuated risk of CVD and cerebrovascular events (CVE)[15, 19, 20]. It is pertinent to study the role of microvasculature because of the established link between small vessels and diseases such as T2DM [21].
OCT–A is a novel imaging technique that rapidly generates volumetric angiographic images (within seconds), which are integral in evaluating retinal and systemic vascular diseases. Compared with gold-standard fluorescein angiography (FA) and indocyanine green angiography (ICGA), advantages of OCT–A are that it is noninvasive, can attain specific depths, uses motion contrast instead of intravenous dye, provides accurate size and localization information, visualizes both the retinal and choroidal vasculature, and shows structural and blood flow information in tandem. The disadvantages include a limited field of view, inability to view leakage, increased artifacts, and inability to detect blood flow below the slowest detectable flow [22]. An Israeli study in which the age of the patients was 25–47 years without ocular pathology or comorbidities, revealed a mean diameter of the retinal artery of 135.73 ± 15.64 μm [23]. The diameter of retinal vessels measured from OCT–A scans are generally wider than other modalities such as adaptive optics ophthalmoscopy, likely attributed to different scanning protocols [24]. The OCT–A retinal imaging community is urged to define and harmonize best practices to enhance accuracy, reliability, and wider collaboration [25].
Several studies demonstrated conflicting results between retinal vasculature and CAD, albeit with the major caveat of employing different CAD scoring and ocular assessment modalities, excluding OCT–A [26]. In a large Danish study, retinal vessel diameters were classically associated with traditional cardiovascular risk factors; however, they were not associated with all-cause mortality despite adjusting for confounding factors [27]. Allon et al. reported in a systematic review that a narrower central retinal artery was associated with an increased incidence of ACS but not SYNTAX or coronary artery calcium (CAC) scores [5; 5]. More recent studies have evaluated this relationship using OCT–A, and the majority revealed an association between vascular density and CAD. Xu et al. established that retinal artery lumen diameter, retinal artery outer diameter, and arteriovenous ratio had a statically significant negative correlation with the severity of CAD [28]. The EYE-Myocardial Infarction (EYE-MI) study concluded that retinal vasculature density was associated with higher cardiovascular risk factor burden, and was associated with a higher SYNTAX score. Wang et al. found that reduced retinal vascular density and choroidal blood flow were associated with CAD [29]. Our study evaluated retinal artery diameter via OCT–A and determined the severity of CAD, calculated by the SYNTAX score. Retinal artery diameter was negatively correlated with the SYNTAX score, with p-values of 0.0038 and 0.003 for the left and right eyes, respectively. This result was consistent with previous studies utilizing OCT–A [4, 5].
There was also a statistically significant negative correlation between retinal artery diameter and SYNTAX score in women but not men. This trend was not noted in other OCT–A studies; however, more extensive population studies assessing alternative retinal microvasculature metrics utilizing other assessment modalities alluded to a similar signal [4, 5, 28, 30, 31]. The Atherosclerosis Risk in Communities Study (ARIC) study demonstrated that narrower retinal arterioles had a higher risk of CAD and cerebrovascular disease in females but not males [31, 32]. A meta-analysis performed in 2010, which evaluated over 20,000 patients, found that retinal disease was independently associated with an increased risk of CAD in women but not men [33]. Conversely, Kromer et al. employed OCT–A to evaluate retinal microvasculature in male-only patients with ACS and found no difference compared with controls [34]. There is a disparity between cardiovascular mortality between sexes, with women receiving less guideline-recommended pharmacotherapy and invasive strategies [35]. Although most women experience obstructive CAD as their culprit etiology for ACS, they also have a higher incidence of myocardial infarction with nonobstructive CAD (MINOCA), spontaneous coronary artery dissection (SCAD), and CMD compared with men [35, 36].
There is a compelling link between DM and CAD [37, 38]. Our study displayed a statistically significant relationship between DM and right eye retinal artery diameter, concordant with the EYE-MI study [4, 5]. Retinal atherosclerosis was associated with DM; however, hypertension, smoking, and age did not demonstrate an association, likewise in our study [39]. In DM, a complex milieu of proinflammatory cytokines, VEGF, activated protein C, platelet-derived growth factor, and advanced glycation end-products result in endothelial dysfunction, which is crucial in developing CAD and CMD [37]. Subsequently, macrophage and vascular smooth muscle cell proliferation lead to atheroma formation. As this process advances, the lumen becomes compromised, detected on CAG. Several studies have revealed that although men may have higher absolute rates of MACE and sudden cardiac death (SCD), relative rates were substantially higher for women across all age ranges [40,41,42]. Diabetic angiopathy can lead to negative remodeling and, as sequelae, smaller caliber vasculature [43].
This study is novel in that it is the first in the Caribbean to demonstrate a statistically significant negative correlation between SYNTAX score and retinal artery diameter. The literature is not replete about potential ethnic variations and retinal artery diameter and CAD [44]. Trinidad has a population of 1.4 million and is considered to be multi-ethnic and diverse. The vast majority of adult mortality is attributed to CVD [45,46,47]. The large burden of CVD in low- and middle-income countries (LMICs) requires opportunistic screening, and OCT–A provides a potential avenue as it is relatively rapid and inexpensive to perform. OCT–A is an emerging and powerful technology that has tremendous potential to shift the paradigm in detecting retinal disease.
This study has several limitations. This monocentric study is based at an academic medical center, the only one that can perform CAG and OCT–A in Trinidad. As a result, these clinically informative data may not be externally valid to other subpopulations.
Potentially, there can be elements of observer, measurement, reporting, and misclassification bias; for example, the interventional cardiologist inaccurately calculating a SYNTAX score or the ophthalmologist inaccurately calibrating retinal artery diameter, despite being fully trained and qualified by their respective specialty boards. This could have been improved upon with team consensus; however, Trinidad is limited with respect to available specialist personnel. Data entry by the study team could have also been compromised due to factors such as fatigue or clinical caseload, despite being quality controlled and assured by a biostatistician.
This study displayed a similar prevalence of DM compared with other local studies (circa 45–55%) in Trinidad; however, there was a preponderance of male and South Asian patients (both approximately 70%), which may infer an inherent selection bias [45, 48]. As mentioned, DM is implicated in negative remodeling and may confound results in an unadjusted analysis [49].
This study did not include a comprehensive assessment of other baseline retinal metrics or parameters such as retinal venule dimensions, arteriovenous ratio and arteriovenous nicking, vessel tortuosity, or retinopathy [4, 5]. Additionally, it has been demonstrated that Trinidadian South Asian patients have accentuated platelet reactivity and a smaller caliber of coronary arteries, which may contribute to decreased retinal artery diameter [45]. Most studies, such as EYE-MI, are predominantly based on Caucasian populations, and these results may not be applicable if ethnic-related disparities occur with respect to the prevalence of comorbidities and retinal artery diameter [4, 5, 50].
Conclusion
A significantly negative correlation was observed between retinal artery diameter and SYNTAX score. This study alludes to the practical use of optical coherence tomography–angiography (OCT–A) as a noninvasive diagnostic modality for patients with cardiovascular disease (CVD). Further large-scale, multicentric studies are required to confirm these exploratory findings.
References
Cardiovascular diseases (CVDs). https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds). Cited 2 Jan 2023.
Taqueti VR, Di Carli MF. Coronary microvascular disease pathogenic mechanisms and therapeutic options: JACC state-of-the-art review. J Am Coll Cardiol. 2018;72:2625–41.
Chung KS, Nguyen PK. Non-invasive measures of coronary microcirculation: taking the long road to the clinic. J Nucl Cardiol. 2018. https://doi.org/10.1007/s12350-017-0972-2.
Arnould L, Guenancia C, Azemar A, Alan G, Pitois S, Bichat F, et al. The EYE-MI pilot study: a prospective acute coronary syndrome cohort evaluated with retinal optical coherence tomography angiography. Investig Opthalmol Vis Sci. 2018. https://doi.org/10.1167/iovs.18-24090.
Allon R, Aronov M, Belkin M, Maor E, Shechter M, Fabian ID. Retinal microvascular signs as screening and prognostic factors for cardiac disease: a systematic review of current evidence. Am J Med. 2021. https://doi.org/10.1016/j.amjmed.2020.07.013.
Neeland IJ, Patel RS, Eshtehardi P, Dhawan S, McDaniel MC, Rab ST, et al. Coronary angiographic scoring systems: an evaluation of their equivalence and validity. Am Heart J. 2012;164:547-552.e1.
Head SJ, Farooq V, Serruys PW, Kappetein AP. The SYNTAX score and its clinical implications. Heart. 2014;100:169–77.
Bundhun PK, Sookharee Y, Bholee A, Huang F. Application of the SYNTAX score in interventional cardiology: a systematic review and meta-analysis. Medicine. 2017;96: e7410.
Neumann F-J, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, et al. 2018 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J. 2019;40:87–165.
Farooq V, van Klaveren D, Steyerberg EW, Meliga E, Vergouwe Y, Chieffo A, et al. Anatomical and clinical characteristics to guide decision making between coronary artery bypass surgery and percutaneous coronary intervention for individual patients: development and validation of SYNTAX score II. Lancet. 2013;381:639–50.
Serruys PW, Morice M-C, Kappetein AP, Colombo A, Holmes DR, Mack MJ, et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360:961–72.
Andersson HB, Pedersen F, Engstrøm T, Helqvist S, Jensen MK, Jørgensen E, et al. Long-term survival and causes of death in patients with ST-elevation acute coronary syndrome without obstructive coronary artery disease. Eur Heart J. 2018;39:102–10.
Studio. Welcome!. http://hedwig.mgh.harvard.edu/biostatistics/. Cited 11 Apr 2023.
Godo S, Suda A, Takahashi J, Yasuda S, Shimokawa H. Coronary microvascular dysfunction. Arterioscler Thrombosis Vasc Biol. 2021. https://doi.org/10.1161/atvbaha.121.316025.
Tedeschi-Reiner E, Strozzi M, Skoric B, Reiner Z. Relation of atherosclerotic changes in retinal arteries to the extent of coronary artery disease. Am J Cardiol. 2005. https://doi.org/10.1016/j.amjcard.2005.05.070.
Weerts J, Mourmans SGJ, BarandiaránAizpurua A, Schroen BLM, Knackstedt C, Eringa E, et al. The role of systemic microvascular dysfunction in heart failure with preserved ejection fraction. Biomolecules. 2022. https://doi.org/10.3390/biom12020278.
Ikram MK, de Jong FJ, Vingerling JR, Witteman JCM, Hofman A, Breteler MMB, et al. Are retinal arteriolar or venular diameters associated with markers for cardiovascular disorders? The Rotterdam Study. Investig Ophthalmol Vis Sci. 2004;45:2129–34.
Nguyen TT, Wang JJ, Sharrett AR, Islam FMA, Klein R, Klein BEK, et al. Relationship of retinal vascular caliber with diabetes and retinopathy: the Multi-Ethnic Study of Atherosclerosis (MESA). Diabetes Care. 2008;31:544–9.
McGeechan K, Liew G, Macaskill P, Irwig L, Klein R, Klein BEK, et al. Meta-analysis: retinal vessel caliber and risk for coronary heart disease. Ann Intern Med. 2009;151:404–13.
McGeechan K, Liew G, Macaskill P, Irwig L, Klein R, Klein BEK, et al. Prediction of incident stroke events based on retinal vessel caliber: a systematic review and individual-participant meta-analysis. Am J Epidemiol. 2009;170:1323–32.
Mutlu U, Ikram MK, Wolters FJ, Hofman A, Klaver CCW, Ikram MA. Retinal microvasculature is associated with long-term survival in the general adult Dutch population. Hypertension. 2016;67:281–7.
de Carlo TE, Romano A, Waheed NK, Duker JS. A review of optical coherence tomography angiography (OCTA). Int J Retina Vitreous. 2015;1:5.
Goldenberg D, Shahar J, Loewenstein A, Goldstein M. Diameters of retinal blood vessels in a healthy cohort as measured by spectral domain optical coherence tomography. Retina. 2013;33:1888–94.
Yao X, Ke M, Ho Y, Lin E, Wong DWK, Tan B, et al. Comparison of retinal vessel diameter measurements from swept-source OCT angiography and adaptive optics ophthalmoscope. Br J Ophthalmol. 2021;105:426–31.
Sampson DM, Dubis AM, Chen FK, Zawadzki RJ, Sampson DD. Towards standardizing retinal optical coherence tomography angiography: a review. Light Sci Appl. 2022;11:63.
Wang N, Liang C. Relationship of Gensini score with retinal vessel diameter and arteriovenous ratio in senile CHD. Open Life Sci. 2021;16:737–45.
Drobnjak D, Munch IC, Glümer C, Faerch K, Kessel L, Larsen M, et al. Retinal vessel diameters and their relationship with cardiovascular risk and all-cause mortality in the Inter99 eye study: a 15-year follow-up. J Ophthalmol. 2016;2016:6138659.
Xu BL, Zhou WL, Zhu TP, Cheng KY, Li YJ, Zhan HJ, et al. A full-width half-maximum method to assess retinal vascular structural changes in patients with ischemic heart disease and microvascular angina. Sci Rep. 2019. https://doi.org/10.1038/s41598-019-47194-5.
Wang J, Jiang J, Zhang Y, Qian YW, Zhang JF, Wang ZL. Retinal and choroidal vascular changes in coronary heart disease: an optical coherence tomography angiography study. Biomed Opt Express. 2019. https://doi.org/10.1364/boe.10.001532.
Wang JJ, Liew G, Wong TY, Smith W, Klein R, Leeder SR, et al. Retinal vascular calibre and the risk of coronary heart disease-related death. Heart. 2006;92:1583–7.
Gopinath B, Chiha J, Plant AJH, Thiagalingam A, Burlutsky G, Kovoor P, et al. Associations between retinal microvascular structure and the severity and extent of coronary artery disease. Atherosclerosis. 2014;236:25–30.
Seidelmann SB, Claggett B, Bravo PE, Gupta A, Farhad H, Klein BE, et al. Retinal vessel calibers in predicting long-term cardiovascular outcomes: The Atherosclerosis Risk in Communities Study. Circulation. 2016;134:1328–38.
McClintic BR, McClintic JI, Bisognano JD, Block RC. The relationship between retinal microvascular abnormalities and coronary heart disease: a review. Am J Med. 2010;123(374):e1-7.
Kromer R, Tigges E, Rashed N, Pein I, Klemm M, Blankenberg S. Association between optical coherence tomography based retinal microvasculature characteristics and myocardial infarction in young men. Sci Rep. 2018;8:5615.
Minissian MB, Mehta PK, Hayes SN, Park K, Wei J, Bairey Merz CN, et al. Ischemic heart disease in young women: JACC review topic of the week. J Am Coll Cardiol. 2022;80:1014–22.
Sinha A, Rahman H, Perera D. Coronary microvascular disease: current concepts of pathophysiology, diagnosis and management. Cardiovasc Endocrinol Metab. 2021;10:22–30.
Poznyak A, Grechko AV, Poggio P, Myasoedova VA, Alfieri V, Orekhov AN. The diabetes mellitus-atherosclerosis connection: the role of lipid and glucose metabolism and chronic inflammation. Int J Mol Sci. 2020. https://doi.org/10.3390/ijms21051835.
Aronson D, Rayfield EJ. How hyperglycemia promotes atherosclerosis: molecular mechanisms. Cardiovasc Diabetol. 2002;1:1.
Tabatabaee A, Asharin MR, Dehghan MH, Pourbehi MR, Nasiri-Ahmadabadi M, Assadi M. Retinal vessel abnormalities predict coronary artery diseases. Perfusion. 2013. https://doi.org/10.1177/0267659112473173.
Malmborg M, Schmiegelow MDS, Nørgaard CH, Munch A, Gerds T, Schou M, et al. Does type 2 diabetes confer higher relative rates of cardiovascular events in women compared with men? Eur Heart J. 2020;41:1346–53.
Woodward M, Peters SAE, Huxley RR. Diabetes and the female disadvantage. Womens Health. 2015;11:833–9.
Peters SAE, Huxley RR, Woodward M. Diabetes as risk factor for incident coronary heart disease in women compared with men: a systematic review and meta-analysis of 64 cohorts including 858,507 individuals and 28,203 coronary events. Diabetologia. 2014;57:1542–51.
Spinetti G, Kraenkel N, Emanueli C, Madeddu P. Diabetes and vessel wall remodelling: from mechanistic insights to regenerative therapies. Cardiovasc Res. 2008;78:265–73.
Kawasaki R, Cheung N, Wang JJ, Klein R, Klein BE, Cotch MF, et al. Retinal vessel diameters and risk of hypertension: the Multiethnic Study of Atherosclerosis. J Hypertens. 2009;27:2386–93.
Seecheran NA, Maharaj A, Boodhai B, Seecheran R, Seecheran V, Persad S, et al. Prevalence of clOpidogrel “resIstaNce” in a selected population of patients undergoing elective percutaneous coronary intervention at a tertiary cardiovascular centre in Trinidad: the POINT pilot study. Open Heart. 2019;6: e000841.
Seecheran N, Baldeo S, Balbosa K, Baksh S, Bethelmy S, Balkaran S, et al. Epidemiologic insight into Trinidad’s awareness and prevention of heart disease. The EPITAPH study—a trinidadian cardiovascular health literacy survey. Int J Community Med Public Health. 2017. https://doi.org/10.18203/2394-6040.ijcmph20171305.
Seecheran N, Nandlal N, Nankissoon S, Nancoo C, Nelson C, Nkemakolam A, et al. A trinidadian cardiovascular medication adherence survey: the ADHERE TNT study. Int J Community Med Public Health. 2017. https://doi.org/10.18203/2394-6040.ijcmph20174218.
Seecheran N, Jagdeo C-L, Seecheran R, Seecheran V, Persad S, Peram L, et al. Screening for depressive symptoms in cardiovascular patients at a tertiary centre in Trinidad and Tobago: investigation of correlates in the SAD CAT study. BMC Psychiatry. 2020;20:498.
Rask-Madsen C, King GL. Vascular complications of diabetes: mechanisms of injury and protective factors. Cell Metab. 2013;17:20–33.
Welch T, Rampersad F, Motilal S, Seecheran NA. Comparison of cardiac CT angiography coronary artery dimensions and ethnicity in Trinidad: the CADET pilot study. Open Heart. 2022. https://doi.org/10.1136/openhrt-2021-001922.
Acknowledgements
We would like to thank the patients for their participation in the study.
Funding
No funding or sponsorship was received for this study or publication of this article. The Rapid Service Fee was funded by the authors.
Medical Writing and Editorial Assistance
No medical writing or editorial assistance services were utilized.
Author Contributions
Naveen Seecheran and Salma Rafeeq conceptualized the study. Naveen Seecheran, Salma Rafeeq, and Robin Seemongal-Dass designed the study. Salma Rafeeq, Nicole Maharaj, Steven Swarath, Valmiki Seecheran, Rajeev Seecheran, Victoria Seebalack, Cathy-Lee Jagdeo, Rajiv Seemongal-Dass, and Abel Yoandri Levya Quert conducted the study. Stanley Giddings, Anil Ramlackhansingh, Sherry Sandy, and Shastri Motilal reviewed the study. Salma Rafeeq and Naveen Seecheran wrote the manuscript. Stanley Giddings, Anil Ramlackhansingh, Sherry Sandy, Shastri Motilal, Robin Seemongal-Dass, and Naveen Seecheran revised the manuscript. All authors approved the final manuscript.
Disclosures
Naveen Seecheran, Salma Rafeeq, Nicole Maharaj, Steven Swarath, Valmiki Seecheran, Rajeev Seecheran, Victoria Seebalack, Cathy-Lee Jagdeo, Rajiv Seemongal-Dass, Abel Yoandri Levya Quert, Stanley Giddings, Anil Ramlackhansingh, Sherry Sandy, Shastri Motilal, Robin Seemongal-Dass have nothing to disclose.
Compliance with Ethics Guidelines
All participants provided verbal consent to participate in the study. Full ethical approval was granted by the campus research ethics committee (CREC) of the University of the West Indies, St. Augustine (UWI STA) (CEC819/01/19). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Seecheran, N.A., Rafeeq, S., Maharaj, N. et al. Correlation of RETINAL Artery Diameter with Coronary Artery Disease: The RETINA CAD Pilot Study—Are the Eyes the Windows to the Heart?. Cardiol Ther 12, 499–509 (2023). https://doi.org/10.1007/s40119-023-00320-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40119-023-00320-x