Abstract
Background
Chimeric antigen receptor T (CAR-T) cell therapy, a new adoptive cell therapy, has been widely used to treat lymphoma patients. Immune checkpoint blockade may improve the cytotoxicity of CAR-T cells by reducing the failure of CAR-T cells and improving antitumor activity. It has shown promising efficacy.
Method
We searched PubMed, the Cochrane Library, Embase and Web of Science from January 2012 to August 2022 to find data reporting the results of CAR-T cells therapy combined with PD-1 in tumor patients. An updated search was conducted in October 2023. The partial response rate (PR), complete response rate (CR), objective response rate (ORR), mortality rate, and incidence of adverse reactions were calculated.
Results
We analyzed 57 lymphoma patients from 5 clinical trials. The pooled partial, complete and overall response rates were 21% (95% CI 0.06–0.39, I2 = 0.37%), 27% (95% CI 0.03–0.60, I2 = 60.43%) and 65% (95% CI 0.23–0.98, I2 = 76.31%), respectively. The pooled incidence of cytokine release syndrome, neutropenia, fever, and fatigue was estimated to be 57% (95% CI 0.08–0.99, I2 = 85.20%), 47% (95% CI 0.14–0.81, I2 = 74.17%), 59% (95% CI 0.27–0.89, I2 = 60.23%), and 50% (95% CI 0.13–0.87, I2 = 73.89%), respectively.
Conclusion
CAR-T-cell therapy combined with anti-PD-1 immunotherapy in the treatment of lymphoma patients has efficacy, and the most common adverse effect is fever.
Registration
The protocol was registered in prospero, with the registration number CRD42022342647.
Similar content being viewed by others
Introduction
Hematologic malignancies include all types of leukemia, multiple myeloma, and malignant lymphoma, including Hodgkin’s lymphoma (HL) and non-Hodgkin’s lymphoma (NHL). The incidence rate of severe disease is 13.9% in patients diagnosed as hematological malignancy within one year [1, 2], and the prognosis is unfavorable [3]. With the application of molecular targeted drugs and immunotherapy, the prognosis of many patients with hematological malignancies has improved [4, 5]. Chimeric antigen receptor-T (CAR-T) cell therapy, as a new popular method in cancer treatment, has been approved by the US Food and Drug Administration for the treatment of some hematologic malignancies, such as Kymriah (tisagenlecleucel) [6], Yescarta (axicabtagene ciloleucel) [7], Tecartus (brexucabtagene autoleucel) [8], and lisocabtagene maraleucel (liso cel) [9]. It has achieved good clinical therapeutic effects [10].
CAR-T cells are genetically engineered T cells. They are composed of the extracellular antigen binding domain of scFv and transmembrane domain and intracellular signal transduction or costimulatory domain (usually CD3ξ) [11, 12], which trigger a cell activation signal when it encounters a target antigen [13]. Single variable domains on a heavy chain (VHH) are called nanobodies and have now been applied to targeted domains in CARs [14]. However, due to off-target effects, antigen escape, inadequate T-cell proliferation and persistence enhance the inhibitory tumor microenvironment [15, 16]. According to many international and clinical studies, some patients still do not respond to CAR-T therapy [17,18,19] and experience serious side effects (such as cytokine release syndrome (CRS) and neurotoxicity) [20, 21]. Improving the efficacy of CAR-T cells, reducing the occurrence of side effects, and improving the long-term treatment rate of disease are currently the most concerning issues of CAR-T therapy at present.
Early failure of CAR-T cells is one of the main factors limiting the antitumor efficacy of CAR-expressing T cells. The expression of multiple coinhibitory receptors on T cells may be related to the failure of CAR-T cells [22]. Studies have shown that the expression of programmed cell death protein-1 (PD-1) is upregulated on CAR-T cells [23, 24]. It may reduce the advantage of 4-1BB costimulated CD8 + CAR-T cells in central memory accumulation and long-term antitumor effects [25]. Targeting multiple inhibitory pathways may enhance the efficacy of CAR-T cells [22]. PD-1 is a cell surface receptor that inhibits T-cell inflammatory activity by binding to ligands [25]. Tumor-induced downregulation of T-cell function can be reversed by immune checkpoint inhibitors [26]. It has been reported that PD-1 destruction by genome editing can enhance the antitumor activity of CAR-T cells [27,28,29] and can also save CAR-T cells from exhaustion and senescence [30, 31]. The overall survival of patients with CAR-T cells was prolonged [32]. CAR-T cells combined with PD-1 have been widely used in preclinical models and clinical trials to enhance the efficacy of cancer therapy. PD-1 blockade is regarded as a promising new idea to improve the function of CAR-T cells. However, the literature still lacks sufficient experimental evidence, and the combined application of the two new immunotherapies is still controversial due to the adverse expansion and short-term clinical remission of T cells and other reasons [33, 34]. Many clinical trials have been conducted to verify the feasibility of CAR-T cells combined with PD-1 in the treatment of lymphoma patients. Our objective was to evaluate the efficacy and safety of this treatment through our systematic review.
Method
Literature search strategy
We searched PubMed, the Cochrane Library, Embase and Web of Science from January 2012 to August 2022 to find data reporting the results of CAR-T cells therapy combined with PD-1 in tumor patients. An updated search was conducted in October 2023. The method of combining subject and free words was used for the literature search. The search terms included “Chimeric Antigen Receptor Therapy”, “Immune Checkpoint Inhibitors” and “CAR T-Cell Therapies”. Detailed search strategies are provided in Supplement 1.
Literature screening and data extraction
The included literature met the following criteria: (1) tumor patients; (2) the experimental group received CAR-T cells combined with PD-1; (3) clinical research; and (4) relevant outcome indicators: partial response rate (PR); complete response rate (CR); objective response rate (ORR); mortality rate; and incidence of adverse reactions. Repeated publications of articles and reviews, conference reports, case reports and animal experiments were excluded.
According to the inclusion and exclusion criteria, two independent researchers selected studies. The third person chose the differences. The extracted literature information included basic information (author, publication year), trial design type, sample size, intervention measures, outcome indicators, etc.
Statistical analysis
We used Stata 16.0 software for the meta-analysis. The effect size and 95% confidence interval were synthesized by software. p < 0.05 was considered statistically significant. The obtained effect values were analyzed for heterogeneity. If there was no significant statistical heterogeneity among studies (p > 0.1, p < 50%), the fixed effects model was adopted; if statistical heterogeneity existed (p < 0.1, p ≥ 50%), the random effects model was used to combine the effect size. Only descriptive analysis was performed if the heterogeneity was too obvious and the source could not be determined. Sensitivity analysis was used to determine the stability of each study. All included studies were evaluated using the Joana Brigg’s Institute (JBI) quality assessment scale [35]. (Supplement 2) The methodological quality of each report was evaluated by ranking the risk of bias as high, medium and low. A score of more than 6 out of 9 items was considered low risk.
Results
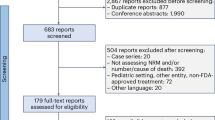
We finally included 5 randomized controlled trials [2, 31, 36,37,38], which included a total of 57 patients with lymphoma. Twenty patients were excluded due to the absence of combined PD-1 treatment, and 37 patients were eventually included. All patients had adult lymphoma pretreated with low-dose chemotherapy (patient characteristics are shown in Table 1). The indications of the patients in the included studies are as follows: patients with progressive B-cell non-Hodgkin’s lymphoma after anti-CD19 CAR-T-cell infusion [31]; patients with CD19-positive B-cell lymphoma who have progressed or relapsed after chemotherapy [2]; relapsed or refractory diffuse large B-cell lymphoma [36]; relapsed/refractory B-cell lymphoma after CAR-T-cell therapy [36]; and CD30-positive relapsed/refractory patients with lymphoma [38]. Five patients were treated with single-dose autologous anti-CD30 CAR-T cells intravenously, and 32 were treated with 4-1BB costimulated anti-CD19 CAR-T cells. Twenty-one patients were given pembrolizumab, and 11 patients were given nivolumab. The screening process is shown in Fig. 1.
PR rate: Five studies reported PR, including 37 patients. The heterogeneity analysis results were as follows: p = 0.40, I2 = 0.37%, indicating low heterogeneity. Therefore, a fixed-effect model was used. The results of the meta-analysis showed that the effect size (95% CI = 0.21 [0.06, 0.39], z = 3.65, p < 0.05) was statistically significant. This result suggested that the PR rate of CAR-T cells combined with PD-1 in tumor patients was 21% (Fig. 2A).
CR rate: CR rates were reported in all 5 studies. Thirty-seven patients were included, and 11 patients experienced a complete response. The results of the heterogeneity analysis were as follows: p = 0.04, I2 = 60.43%, indicating high heterogeneity. Therefore, the random effects model was adopted. The results of the meta-analysis showed that the effect size (95% CI = 0.27 [0.03, 0.60], z = 2.56, p < 0.05) was statistically significant. This result suggested that the CR rate of CAR-T cells combined with PD-1 in tumor patients was 27% (Fig. 2B). The CR of 32 patients treated only with anti-CD19 CAR-T cells was 16% [95% CI 0.02,0.35, I2 = 30.04%]. (Supplement 3)
The overall ORR was reported in 5 studies, including 37 patients and 20 patients with objective response. The results of the heterogeneity analysis were as follows: p < 0.1, I2 = 76.31%, indicating high heterogeneity. Therefore, the random effects model was adopted. The results of the meta-analysis showed that the effect size (95% CI = 0.65 [0.23, 0.98], z = 3.76, p < 0.05) was statistically significant, suggesting that the objective response rate of CAR-T cells combined with PD-1 therapy in tumor patients was 65% (Fig. 2C). Among them, 6 patients died. The mortality rate of tumor patients treated with CAR-T cells combined with PD-1 was 6% [95% CI 0.00, 0.35], z = 0.99, p = 0.32 (Fig. 2D).
Adverse reactions
CRS is a common side effect of CAR-T therapy. CRS of any grade was reported in 5 studies, and 17 patients were enrolled. The results of the heterogeneity analysis were as follows: p < 0.1, I2 = 85.20%, indicating high heterogeneity. Therefore, we adopted the random effects model. The results of the meta-analysis showed that the effect size (95% CI = 0.57[0.08, 0.99], z = 2.70, p = 0.01) was statistically significant. It was suggested that the incidence of CRS of any grade in tumor patients treated with CAR-T cells combined with PD-1 was 57% (Fig. 3A). Fifteen patients developed grade 1–2 CRS. The results of the heterogeneity analysis were as follows: p < 0.1, I2 = 85.23%, indicating high heterogeneity, so the random effects model was adopted. The results of the meta-analysis showed that the effect size (95% CI = 0.43 [0.01, 0.92], z = 2.17, p = 0.03) was statistically significant (Supplement 4). These results suggest that the incidence of grade 1–2 CRS in tumor patients treated with CAR-T cells combined with PD-1 was 43%. Only two patients reported grade 3–4 CRS.
Many reports have confirmed that neutropenia is the most common grade 3/4 adverse event. Our study found that 4 studies reported complications of grade 3–4 neutropenia, which occurred in 14 patients (47%) of the 36 patients included. The results of the heterogeneity analysis were p = 0.01 and I2 = 74.17%, indicating high heterogeneity. Therefore, the random effects model was adopted, and the results of the meta-analysis showed that the effect size (95% CI = 0.47 [0.14, 0.81], z = 3.62, p < 0.01) was statistically significant (Fig. 3B).
Other adverse effects were also found. A total of 20 (59% [95% CI 0.27, 0.89, I2 = 60.23%] p < 0.01) of the 37 patients were found to have a fever (Fig. 3C). Of the 28 patients, 13 (50% [95% CI 0.13, 0.87, I2 = 73.89%] p < 0.01) had fatigue symptoms (Fig. 3D).
Sensitivity analysis and the evaluation of the bias were performed to eliminate studies using a one-by-one method. We found that the results of the research were not significantly different after excluding and removing the results one by one (Figs. 4 and 5). This finding suggests that the meta-analysis result is stable and reliable. The risk of bias was assessed as low risk in all studies.
Discussion
Our meta-analysis showed that CAR-T cells combined with PD-1 showed good safety and efficacy in patients with hematologic tumors. The ORR was 65% [95% CI 0.23, 0.98], and the CR was 27% [95% CI 0.03, 0.60]. The CR of anti-CD19 CAR-T cells constructed with 4-1BB costimulation was 16% [95% CI 0.02, 0.35, I2 = 30.04%], which was lower than that of all CAR-T-cell treatments. This may be due to the better efficacy of CD30 CAR-T therapy in the treatment of relapsed or refractory HL [39]. However, due to the long cycle of CAR-T therapy, current clinical trials are mostly used in patients with relatively stable hematologic tumors, so the true efficacy of all patients using such therapy may be lower than our results. A meta-analysis revealed that CAR-T therapy resulted in a 46% CR and 66% ORR for B-cell non-Hodgkin lymphoma [40], which is a better clinical outcome than our study. Currently, combination therapy is mainly applied to patients with clinical relapse and no response to single CAR-T therapy or other immunotherapies. Their disease is more complex, and the formation of a tumor immunosuppressive microenvironment affects the amplification of CAR-T cells [37], so the CR is lower than that in other studies on single CAR-T-cell therapy for hematologic tumors. However, studies have shown that the combination of PD-1 inhibitors in patients who do not respond to CAR-T therapy can improve the ORR of some patients [2].
The most common acute toxicity of CAR-T cells is CRS [41]. The incidence of CRS of any grade was 57% (95% CI 0.08, 0.99), and the rating was mainly based on the PENN scale [42]. Class 1–2 CRS accounted for 43% (95% CI 0.01, 0.92). Most grade 1–2 adverse events can be managed with drugs, and the incidence of severe autoimmune events is low. Nonsteroidal anti-inflammatory drugs [43] and corticosteroids can relieve symptoms and control CRS to a certain extent. However, there may be a risk of damage to CAR-T cells [44, 45]. No significant difference was found between anti-CD30 and anti-CD19 outcomes using different surface targets.
Continuous tumor attack can lead to the high expression of PD-1 on the surface of T cells. This leads to the exhaustion of CAR-T cells and the weakening of antitumor effects [46]. By adopting anti-PD-1 CAR-T cells in NSG mice, mouse CAR-T cells showed enhanced antitumor reactivity, and the amplification effect of CAR-T cells was enhanced [32], promoting tumor regression and reducing the incidence of adverse reactions [47, 48]. GUO et al. found that the destruction of endogenous PD-1 in CAR-T cells could enhance the toxicity of T cells, the production of the cytokines IFN-γ and IL-2, and the antitumor effect and survival time of CAR-T cells [49]. The PD-1 pathway may also affect the efficacy of CAR-T cell immunotherapy by preventing CAR-T cells from entering the tumor area [50]. With pembrolizumab after CAR-T cell treatment, all responding patients experienced more than one CAR-T cell amplification peak, and the CAR-T cells lasted longer than nonresponding patients, with only one peak [2]. One case report also showed that PD-1 inhibition could effectively increase diffuse large B-cell lymphoma that did not respond to CAR-T therapy and enhance the expansion of CD19 CAR-T cells [31]. Therefore, it is reasonable to think that PD-1 inhibitors may partially prevent the depletion and functional deterioration of anti-CD19 CAR-T cells.
This systematic review and meta-analysis provides some reference value for clinical treatment. To our knowledge, this is the first study to systematically analyze the efficacy of CAR-T cell therapy combined with PD-1 in the treatment of lymphoma patients. This meta-analysis has some limitations as well. First, the heterogeneous nature of the included studies (paucity of the available literature, dosing differences, lines of prior therapy differences, etc.) might introduce bias. Second, due to the small number of included studies, the sample size was not large enough. Nevertheless, this meta-analysis will be useful to design and prioritize future clinical trials for CAR-T-cell therapy combined with anti-PD-1 immunotherapy.
Data Availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
de Vries VA, Müller MCA, Arbous MS, Biemond BJ, Blijlevens NMA, Kusadasi N, Span LRF, Vlaar APJ, van Westerloo DJ, Kluin-Nelemans HC, et al. Long-term outcome of patients with a hematologic malignancy and multiple organ failure admitted at the Intensive Care. Crit Care Med. 2019;47(2):e120–8.
Cao Y, Lu W, Sun R, Jin X, Cheng L, He X, Wang L, Yuan T, Lyu C, Zhao M. Anti-CD19 Chimeric Antigen Receptor T Cells in Combination with Nivolumab are safe and effective against Relapsed/Refractory B-Cell non-hodgkin Lymphoma. Front Oncol. 2019;9:767.
Chow VA, Shadman M, Gopal AK. Translating anti-CD19 CAR T-cell therapy into clinical practice for relapsed/refractory diffuse large B-cell Lymphoma. Blood. 2018;132(8):777–81.
Miller JS, Soignier Y, Panoskaltsis-Mortari A, McNearney SA, Yun GH, Fautsch SK, McKenna D, Le C, Defor TE, Burns LJ, et al. Successful adoptive transfer and in vivo expansion of human haploidentical NK cells in patients with cancer. Blood. 2005;105(8):3051–7.
Craddock C, Friedberg JW. Immunotherapy for Hematologic Malignancies. J Clin Oncol. 2021;39(5):343–5.
Ali S, Kjeken R, Niederlaender C, Markey G, Saunders TS, Opsata M, Moltu K, Bremnes B, Grønevik E, Muusse M, et al. The European Medicines Agency Review of Kymriah (Tisagenlecleucel) for the treatment of Acute lymphoblastic Leukemia and diffuse large B-Cell Lymphoma. Oncologist. 2020;25(2):e321–7.
Neelapu SS, Locke FL, Bartlett NL, Lekakis LJ, Miklos DB, Jacobson CA, Braunschweig I, Oluwole OO, Siddiqi T, Lin Y, et al. Axicabtagene Ciloleucel CAR T-Cell Therapy in Refractory large B-Cell Lymphoma. N Engl J Med. 2017;377(26):2531–44.
Fournier C, Martin F, Zitvogel L, Kroemer G, Galluzzi L, Apetoh L. Trial Watch: Adoptively transferred cells for anticancer immunotherapy. Oncoimmunology. 2017;6(11):e1363139.
Siddiqi T, Maloney DG, Kenderian SS, Brander DM, Dorritie K, Soumerai J. Lisocabtagene maraleucel in chronic lymphocytic Leukaemia and small lymphocytic Lymphoma (TRANSCEND CLL 004): a multicentre, open-label, single-arm, phase 1–2 study. Lancet. 2023;402(10402):641–54.
June CH, O’Connor RS, Kawalekar OU, Ghassemi S, Milone MC. CAR T cell immunotherapy for human cancer. Science. 2018;359(6382):1361–5.
Kershaw MH, Westwood JA, Darcy PK. Gene-engineered T cells for cancer therapy. Nat Rev Cancer. 2013;13(8):525–41.
Long AH, Haso WM, Shern JF, Wanhainen KM, Murgai M, Ingaramo M, Smith JP, Walker AJ, Kohler ME, Venkateshwara VR, et al. 4-1BB costimulation ameliorates T cell exhaustion induced by tonic signaling of chimeric antigen receptors. Nat Med. 2015;21(6):581–90.
Zah E, Lin MY, Silva-Benedict A, Jensen MC, Chen YY. T cells expressing CD19/CD20 Bispecific Chimeric Antigen Receptors Prevent Antigen Escape by malignant B cells. Cancer Immunol Res. 2016;4(6):498–508.
Safarzadeh Kozani P, Naseri A, Mirarefin SMJ, Salem F, Nikbakht M, Evazi Bakhshi S. Safarzadeh Kozani P: Nanobody-based CAR-T cells for cancer immunotherapy. Biomark Res. 2022;10(1):24.
Li H, Zhao Y. Increasing the safety and efficacy of chimeric antigen receptor T cell therapy. Protein Cell. 2017;8(8):573–89.
Figueroa JA, Reidy A, Mirandola L, Trotter K, Suvorava N, Figueroa A, Konala V, Aulakh A, Littlefield L, Grizzi F, et al. Chimeric antigen receptor engineering: a right step in the evolution of adoptive cellular immunotherapy. Int Rev Immunol. 2015;34(2):154–87.
Schuster SJ, Bishop MR, Tam CS, Waller EK, Borchmann P, McGuirk JP, Jäger U, Jaglowski S, Andreadis C, Westin JR, et al. Tisagenlecleucel in adult relapsed or refractory diffuse large B-Cell Lymphoma. N Engl J Med. 2019;380(1):45–56.
Rossig C, Pule M, Altvater B, Saiagh S, Wright G, Ghorashian S, Clifton-Hadley L, Champion K, Sattar Z, Popova B, et al. Vaccination to improve the persistence of CD19CAR gene-modified T cells in relapsed pediatric acute lymphoblastic Leukemia. Leukemia. 2017;31(5):1087–95.
Xu J, Chen LJ, Yang SS, Sun Y, Wu W, Liu YF, Xu J, Zhuang Y, Zhang W, Weng XQ, et al. Exploratory trial of a biepitopic CAR T-targeting B cell maturation antigen in relapsed/refractory Multiple Myeloma. Proc Natl Acad Sci U S A. 2019;116(19):9543–51.
Park JH, Rivière I, Gonen M, Wang X, Sénéchal B, Curran KJ, Sauter C, Wang Y, Santomasso B, Mead E, et al. Long-term follow-up of CD19 CAR therapy in Acute Lymphoblastic Leukemia. N Engl J Med. 2018;378(5):449–59.
Maude SL, Laetsch TW, Buechner J, Rives S, Boyer M, Bittencourt H, Bader P, Verneris MR, Stefanski HE, Myers GD, et al. Tisagenlecleucel in Children and Young adults with B-Cell lymphoblastic Leukemia. N Engl J Med. 2018;378(5):439–48.
Chen N, Morello A, Tano Z, Adusumilli PS. CAR T-cell intrinsic PD-1 checkpoint blockade: a two-in-one approach for solid Tumor immunotherapy. Oncoimmunology. 2017;6(2):e1273302.
Anwer F, Shaukat AA, Zahid U, Husnain M, McBride A, Persky D, Lim M, Hasan N, Riaz IB. Donor origin CAR T cells: graft versus malignancy effect without GVHD, a systematic review. Immunotherapy. 2017;9(2):123–30.
Li F, Zhang Z, Xuan Y, Zhang D, Liu J, Li A, Wang S, Li T, Shi X, Zhang Y. PD-1 abrogates the prolonged persistence of CD8(+) CAR-T cells with 4-1BB co-stimulation. Signal Transduct Target Ther. 2020;5(1):164.
Latchman Y, Wood CR, Chernova T, Chaudhary D, Borde M, Chernova I, Iwai Y, Long AJ, Brown JA, Nunes R, et al. PD-L2 is a second ligand for PD-1 and inhibits T cell activation. Nat Immunol. 2001;2(3):261–8.
Pardoll DM. The blockade of immune checkpoints in cancer immunotherapy. Nat Rev Cancer. 2012;12(4):252–64.
Gubin MM, Zhang X, Schuster H, Caron E, Ward JP, Noguchi T, Ivanova Y, Hundal J, Arthur CD, Krebber WJ, et al. Checkpoint blockade cancer immunotherapy targets tumour-specific mutant antigens. Nature. 2014;515(7528):577–81.
Tumeh PC, Harview CL, Yearley JH, Shintaku IP, Taylor EJ, Robert L, Chmielowski B, Spasic M, Henry G, Ciobanu V, et al. PD-1 blockade induces responses by inhibiting adaptive immune resistance. Nature. 2014;515(7528):568–71.
Ribas A, Shin DS, Zaretsky J, Frederiksen J, Cornish A, Avramis E, Seja E, Kivork C, Siebert J, Kaplan-Lefko P, et al. PD-1 blockade expands Intratumoral Memory T cells. Cancer Immunol Res. 2016;4(3):194–203.
Kamphorst AO, Wieland A, Nasti T, Yang S, Zhang R, Barber DL, Konieczny BT, Daugherty CZ, Koenig L, Yu K, et al. Rescue of exhausted CD8 T cells by PD-1-targeted therapies is CD28-dependent. Science. 2017;355(6332):1423–7.
Chong EA, Melenhorst JJ, Lacey SF, Ambrose DE, Gonzalez V, Levine BL, June CH, Schuster SJ. PD-1 blockade modulates chimeric antigen receptor (CAR)-modified T cells: refueling the CAR. Blood. 2017;129(8):1039–41.
Li S, Siriwon N, Zhang X, Yang S, Jin T, He F, Kim YJ, Mac J, Lu Z, Wang S, et al. Enhanced Cancer Immunotherapy by Chimeric Antigen Receptor-Modified T Cells Engineered to secrete checkpoint inhibitors. Clin Cancer Res. 2017;23(22):6982–92.
Hunter BD, Rogalski M, Jacobson CA. Chimeric antigen receptor T-cell therapy for the treatment of aggressive B-cell non-hodgkin Lymphomas: efficacy, toxicity, and comparative chimeric antigen receptor products. Expert Opin Biol Ther. 2019;19(11):1157–64.
Jiang Y, Li Y, Zhu B. T-cell exhaustion in the Tumor microenvironment. Cell Death Dis. 2015;6(6):e1792.
Munn Z, Moola S, Lisy K, Riitano D, Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int J Evid Based Healthc. 2015;13(3):147–53.
Chen X, Li X, Liu Y, Zhang Z, Zhang X, Huang J, Li H, Li F, Zhang L, Li L, et al. A phase I clinical trial of chimeric antigen receptor-modified T cells in patients with relapsed and refractory Lymphoma. Immunotherapy. 2020;12(10):681–96.
Chong EA, Alanio C, Svoboda J, Nasta SD, Landsburg DJ, Lacey SF, Ruella M, Bhattacharyya S, Wherry EJ, Schuster SJ. Pembrolizumab for B-cell Lymphomas relapsing after or refractory to CD19-directed CAR T-cell therapy. Blood. 2022;139(7):1026–38.
Sang W, Wang X, Geng H, Li T, Li D, Zhang B, Zhou Y, Song X, Sun C, Yan D, et al. Anti-PD-1 therapy enhances the efficacy of CD30-Directed Chimeric Antigen Receptor T Cell Therapy in patients with Relapsed/Refractory CD30 + Lymphoma. Front Immunol. 2022;13:858021.
Wang CM, Wu ZQ, Wang Y, Guo YL, Dai HR, Wang XH, Li X, Zhang YJ, Zhang WY, Chen MX, et al. Autologous T cells expressing CD30 chimeric Antigen receptors for relapsed or refractory Hodgkin Lymphoma: an open-label phase I Trial. Clin Cancer Res. 2017;23(5):1156–66.
Wang N, Meng Y, Wu Y, He J, Liu F. Efficacy and safety of chimeric antigen receptor T cell immunotherapy in B-cell non-hodgkin Lymphoma: a systematic review and meta-analysis. Immunotherapy. 2021;13(4):345–57.
Brudno JN, Kochenderfer JN. Toxicities of chimeric antigen receptor T cells: recognition and management. Blood. 2016;127(26):3321–30.
Porter D, Frey N, Wood PA, Weng Y, Grupp SA. Grading of cytokine release syndrome associated with the CAR T cell therapy tisagenlecleucel. J Hematol Oncol. 2018;11(1):35.
Yang M, Wang L, Ni M, Neuber B, Wang S, Gong W, Sauer T, Schubert ML, Hückelhoven-Krauss A, Xia R, et al. Dual effects of cyclooxygenase inhibitors in Combination with CD19.CAR-T cell immunotherapy. Front Immunol. 2021;12:670088.
Maude SL, Frey N, Shaw PA, Aplenc R, Barrett DM, Bunin NJ, Chew A, Gonzalez VE, Zheng Z, Lacey SF, et al. Chimeric antigen receptor T cells for sustained remissions in Leukemia. N Engl J Med. 2014;371(16):1507–17.
Davila ML, Riviere I, Wang X, Bartido S, Park J, Curran K, Chung SS, Stefanski J, Borquez-Ojeda O, Olszewska M, et al. Efficacy and toxicity management of 19-28z CAR T cell therapy in B cell acute lymphoblastic Leukemia. Sci Transl Med. 2014;6(224):224ra225.
Wherry EJ. T cell exhaustion. Nat Immunol. 2011;12(6):492–9.
Wang J, Deng Q, Jiang YY, Zhang R, Zhu HB, Meng JX, Li YM. CAR-T 19 combined with reduced-dose PD-1 blockade therapy for treatment of refractory follicular Lymphoma: a case report. Oncol Lett. 2019;18(5):4415–20.
John LB, Devaud C, Duong CP, Yong CS, Beavis PA, Haynes NM, Chow MT, Smyth MJ, Kershaw MH, Darcy PK. Anti-PD-1 antibody therapy potently enhances the eradication of established tumors by gene-modified T cells. Clin Cancer Res. 2013;19(20):5636–46.
Guo X, Jiang H, Shi B, Zhou M, Zhang H, Shi Z, Du G, Luo H, Wu X, Wang Y, et al. Disruption of PD-1 enhanced the anti-tumor activity of Chimeric Antigen Receptor T Cells against Hepatocellular Carcinoma. Front Pharmacol. 2018;9:1118.
Jaspers JE, Brentjens RJ. Development of CAR T cells designed to improve antitumor efficacy and safety. Pharmacol Ther. 2017;178:83–91.
Funding
This work was supported by the Postdoctoral Science Startup Foundation of the Heilongjiang Provincial Science (Grant 21042180268).
Author information
Authors and Affiliations
Contributions
Yuxin Zhou, Wenjing Mu, and Chen Wang contributed equally to this article, including investigation, data curation, and writing - original draft. Zipeng Zhuo: investigation, data curation. Yu Xin and Hongxu Li: data curation, writing - original draft. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Conflict of Interest
None.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Additional File 2: Supplement 2. JBI critical appraisal quality assessment of the case series study.
12885_2023_11536_MOESM3_ESM.pdf
Additional File 3: Supplement 3. (A). Sensitivity analysis of complete response (CR) for patients with anti-CD19 CAR-T therapy. (B) Forest plot of complete response (CR) for patients with anti-CD19 CAR-T therapy.
12885_2023_11536_MOESM4_ESM.pdf
Additional File 4: Supplement 4. (A). Sensitivity analysis of 1–2 grade CRS for patients. (B) Forest plot of 1–2 grades CRS for patients.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhou, Y., Mu, W., Wang, C. et al. Ray of dawn: Anti-PD-1 immunotherapy enhances the chimeric antigen receptor T-cell therapy in Lymphoma patients. BMC Cancer 23, 1019 (2023). https://doi.org/10.1186/s12885-023-11536-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-023-11536-4