Abstract
Background
Glioblastoma (GBM) is the most malignant primary tumor in the brain, with poor prognosis and limited effective therapies. Although Bevacizumab (BEV) has shown promise in extending progression-free survival (PFS) treating GBM, there is no evidence for its ability to prolong overall survival (OS). Given the uncertainty surrounding BEV treatment strategies, we aimed to provide an evidence map associated with BEV therapy for recurrent GBM (rGBM).
Methods
PubMed, Embase, and the Cochrane Library were searched for the period from January 1, 1970, to March 1, 2022, for studies reporting the prognoses of patients with rGBM receiving BEV. The primary endpoints were overall survival (OS) and quality of life (QoL). The secondary endpoints were PFS, steroid use reduction, and risk of adverse effects. A scoping review and an evidence map were conducted to explore the optimal BEV treatment (including combination regimen, dosage, and window of opportunity).
Results
Patients with rGBM could gain benefits in PFS, palliative, and cognitive advantages from BEV treatment, although the OS benefits could not be verified with high-quality evidence. Furthermore, BEV combined therapy (especially with lomustine and radiotherapy) showed higher efficacy than BEV monotherapy in the survival of patients with rGBM. Specific molecular alterations (IDH mutation status) and clinical features (large tumor burden and double-positive sign) could predict better responses to BEV administration. A low dosage of BEV showed equal efficacy to the recommended dose, but the optimal opportunity window for BEV administration remains unclear.
Conclusions
Although OS benefits from BEV-containing regimens could not be verified in this scoping review, the PFS benefits and side effects control supported BEV application in rGBM. Combining BEV with novel treatments like tumor-treating field (TTF) and administration at first recurrence may optimize the therapeutic efficacy. rGBM with a low apparent diffusion coefficient (ADCL), large tumor burden, or IDH mutation is more likely to benefit from BEV treatment. High-quality studies are warranted to explore the combination modality and identify BEV-response subpopulations to maximize benefits.
Similar content being viewed by others
Introduction
Glioblastoma (GBM) is the most aggressive type of primary malignant tumor of the brain in adults [1]. Despite the new combination of Stupp protocol, including radiation and chemotherapy with maximal surgical resection and tumor-treating field (TTF), the prognosis remains unsatisfactory as most tumors recur in situ [1, 2]. Several interventions, including targeted therapies, have been attempted to improve the prognosis of GBM. As GBM is a hyperemic tumor involving the upregulation and activation of VEGFA and HIF [3], VEGFA is a reasonable target molecule in the treatment of GBM. Bevacizumab (BEV), a humanized monoclonal antibody inhibiting VEGFA, was considered a promising candidate for treating GBM, given its clinical benefits in other cancers such as colorectal cancer [4], renal cell carcinoma [5], non-squamous non-small cell lung cancer [6], and cervical cancer [7]. Success in the treatment of other tumors persuaded researchers to conduct phase III AVAglio and RTOG 0825 clinical trials in patients with newly diagnosed GBM. However, both clinical trials didn’t improve the overall survival (OS) in the BEV treatment arm. Further, a randomized phase II TAVAREC clinical study demonstrated that BEV treatment had no significant improvement on progression-free survival (PFS) and OS in Grade 2 and Grade 3 gliomas [8]. A phase III trial by Wick et al. did not find any OS benefits with combined therapy of BEV plus lomustine, compared with lomustine alone [9]. Based on these several clinical trials, BEV is considered ineffective in prolonging OS for recurrent GBM (rGBM) by the European Association Neuro-Oncology (EANO) [10, 11]. Nevertheless, clinical benefits other than the prolongation of survival were possibly observed. The EORTC protocol demonstrated that BEV decreased steroid dependence and relieved para-tumor edema in patients with GBM [8]. Despite a lack of evidence supporting its ability to prolong OS, BEV was approved by the FDA (U.S. Food and Drug Administration) in 2009 as a treatment for rGBM and was included in the 2021 EANO guidelines due to its demonstrated improvement in quality of life and safety [11].
BEV might not be suitable for the treatment of all rGBM patients in general based on the outcome of these randomized trials. In the AVAglio trial, subgroup analysis revealed that the TCGA-proneural GBM subtype had an OS benefit from the administration of BEV. Further, epigenetic mechanisms could also influence the sensitivity of BEV, as demonstrated by Cloughesy et al.‘s finding that methylguanine-DNA methyltransferase (MGMT) methylation may be predictive for onartuzumab (ONA) + BEV outcomes in GBM. It is necessary to perform subgroup analyses to specifically identify the survival benefits of the treatment of BEV. However, no consensus has been reached regarding the subset of rGBM patients who are sensitive to BEV. Furthermore, the optimal combination therapy, dosage efficacy, and correct indication for BEV therapy are still controversial.
Given the considerable uncertainty surrounding BEV treatment strategies, we aimed to systematically review the current evidence associated with BEV therapy by mapping evidence. We aimed to answer the following five questions: (1) Could BEV-containing regimens bring survival benefits to patients with rGBM, compared with non-BEV treatment regimens? (2) Could BEV combined with other therapies prolong the OS of patients with rGBM, compared with BEV monotherapy? (3) Could BEV treatment improve quality of life (QoL) and reduce the adverse events (AEs) in rGBM? (4) Could some subgroups harboring specific clinical or molecular characteristics gain survival benefits from BEV treatment? (5) What are the optimal dosages and indications for the BEV treatment in rGBM?
Methods
Search strategy and study selection
The scoping review and mapping evidence were conducted following the PRISMA extension for scoping reviews [12]. A comprehensive literature search was performed in electronic databases including PubMed, Embase, and the Cochrane Library, on March 27th, 2022.
Inclusion criteria
(1) Patients with recurrent high-grade glioma (WHO grades 3–4) or GBM (WHO grade 4), regardless of age, gender, or pathological type; (2) Patients who were treated with BEV alone or in combination. Treatment types were focused on but were not limited to BEV alone, or BEV plus radiotherapy, chemotherapy (including carmustine implants), chemoradiotherapy, surgery, immunotherapy, and TTFs; (3) The outcomes of interest included OS, PFS, QoL, and AEs (cerebral edema and cognitive deficits) incidence; (4) Study types included randomized controlled trials (RCT), case-control trials (CCT), observational trials, pre- and post-control studies, and systematic reviews.
Exclusion criteria
(1) Case reports and conference abstracts; (2) Protocols but not reports of the study result; (3) Studies that were not reported in English.
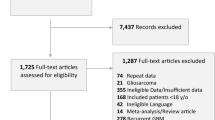
Two reviewers independently screened the titles and abstracts of the retrieved records. Following the initial screening, full texts of the trials that passed title/abstract screening were scrutinized to confirm eligibility for the analyses. Disagreements were resolved by discussion with a third person if necessary. A PRISMA flow diagram was constructed to show the full article-selection process.
Data extraction
Two authors (Minjie Fu and Xiao Huang) independently examined the studies and extracted data using a standardized spreadsheet with the following characteristics: trial type, number of participants, type and administration of interventions, the definition of outcomes, measurement variables, and key findings. In situations of discrepancies, the third author (Zhirui Zhou) was consulted for final decision-making.
Data coding and definition
Selected studies were coded according to the type and administration of interventions (BEV monotherapy or BEV combined therapy). Classification criteria were discussed by the professional group. The term “Beneficial” was defined as a finding that had one or more of the following results: prolonged OS or improved QoL or PFS. The term “Harm” was defined as a finding that had one or more of the following results: decreased OS or PFS or worse QoL. The term “No difference” was defined as no significant difference or no difference reported between the groups for OS, PFS, or QoL. “Inconclusive” was defined as a finding that demonstrated both beneficial and harmful results in the studies.
Presentation of evidence mapping
We provided a scoping review and mapping evidence through a descriptive table that consisted of the characteristics of selected studies. The narrative description was presented.
Results
Study selection
A primary search yielded a total of 405 studies. After the removal of 15 duplicated publications, 390 studies were subsequently screened. Subsequently, full texts of 132 studies were scrutinized for eligibility. Ultimately, 90 studies met the eligibility criteria for inclusion in the scoping review and mapping evidence, comprising 2 phase I trials, 22 phase II trials, 2 phase III studies, 5 prospective studies, 36 retrospective studies, and 23 reviews (see Fig. 1).
Could BEV-containing treatment regimens bring survival benefits to patients with rGBM, compared with non-BEV treatment regimens?
In total, 31 studies (2 phase III studies, 5 phase II studies, 2 prospective studies, 9 retrospective studies, and 13 reviews, see Table 1) compared the therapeutic efficacy of BEV-containing treatment regimens with non-BEV treatment regimens. Of these, 17 studies investigated the benefits of adding BEV to chemotherapy (1 phase III trial, 1 phase II trial, 4 retrospective studies, and 11 reviews), while 5 studies investigated the efficacy of BEV plus lomustine (1 phase III trial, 3 phase II trial, and 1 retrospective study). Although a phase II study by Taal et al. showed the OS benefits of BEV plus lomustine versus the lomustine monotherapy group (mOS: LOM vs. BEV/LOM 110 vs. BEV/LOM 90, 8 months vs. 16 months vs. 11 months) [13], the other four randomized studies (including a phase III trial by Wick et al.) didn’t support this finding. Other phase II/III trials did not identify the OS benefits of BEV with a range of other chemotherapy partners (temozolomide (TMZ), trebananib, irinotecan, and nivolumab) compared with the non-BEV regimen.
Four studies (3 retrospective studies and 1 review) reported that the combination of BEV and radiotherapy improved OS, compared with radiotherapy alone. Meanwhile, 1 retrospective study and 1 prospective study on BEV plus re-surgery regimen showed that rGBM patients benefitted from BEV after receiving re-surgery.
Although some randomized clinical trials showed positive effects of the BEV-containing regimen on PFS, other palliative effects, and neurological improvement as meaningful benefits, gain on OS was not observed among the entire patient population in the majority of the trials.
Could BEV combined therapy prolong the OS of patients with rGBM compared with BEV monotherapy?
Because BEV treatment alone lacked evidence to prolong OS of patients with rGBM, 41 studies were further conducted to identify the optimal combination therapies. These studies included 14 phase II trials, 1 phase I trial, 15 retrospective studies, 1 prospective study, and 10 reviews (Table 2).
A range of chemotherapy candidates was studied, including lomustine, ONA, celecoxib, vorinostat, dasatinib, valganciclovir, and trebananib. The phase II trials by Taal et al. and Weathers et al. did not find the OS benefits of the addition of lomustine to BEV [13, 14], while the results varied in the two retrospective studies [15, 16]. Although several studies found that BEV plus lomustine could prolong PFS, compared with BEV monotherapy, its benefits on OS warranted further validation [17, 18]. In addition to lomustine, the OS benefits of Irinotecan (IRI), osimertinib, and valganciclovir were reported in some retrospective studies [19,20,21]. But currently, no high-quality evidence from RCT was found to further verify their positive effect on OS.
Five studies investigated the efficacy of BEV plus radiotherapy versus BEV monotherapy (1 prospective study and 4 retrospective studies) on OS. Although the prospective study found no significant difference in OS between the combination group and monotherapy group [22], the other four retrospective studies stated that radiotherapy plus BEV improved the rGBM prognosis by enhancing OS [23,24,25,26].
A retrospective study by Yamaguchi et al. in 2021 showed that the BEV plus re-surgery improved OS (mOS, Cytoreductive surgery + BEV vs. BEV, 16.3 months vs. 7.4 months, p = 0.0008) [27] while another retrospective study in 2017 did not find any difference between BEV combination and single regimen groups [28].
As TTF has emerged as a promising technique for tumor therapy, the efficacy of TTF plus BEV was also elucidated. A post-analysis of the EF-14 trial demonstrated that the combination of BEV and TTF brought more OS benefits, compared with BEV alone (mOS, TTF + BEV vs. BEV: 11.8 months vs. 9.0 months, p = 0.043) [29].
The combinatory partners of BEV were widely studied, and some BEV combined therapies (especially with lomustine and radiotherapy) were proved to have superior efficacy to BEV monotherapy. But additional research is required to determine the optimal combination of treatment modalities.
Median OS reported in the studies included in the analyses is summarized in Fig. 2. Although it was difficult to prove the OS benefits of BEV treatment through a single study, there was a trend to suggest that rGBM patients treated with BEV combined therapy may experience longer median OS.
Could BEV treatment improve the quality of life and reduce the adverse events in rGBM?
In total, 19 studies (1 phase I trial, 4 phase II trials, 1 phase III trial, 4 retrospective studies, and 9 reviews) investigated the BEV effect on QoL and AEs (edema and cognitive dysfunction) (Table 3). While the effect of BEV monotherapy and combined therapy on OS prolongation remains unclear and controversial, three studies have verified BEV’s potential to reduce steroid use [30,31,32]. Additionally, three studies have reported that BEV could reduce the AEs induced by radiotherapy [33,34,35]. BEV also effectively controlled the tumor mass. However, only two retrospective studies found that the health-related QoL improved after receiving BEV containing therapy [30, 36], while other studies, including a phase II trial, did not find associations between BEV treatment and QoL [37, 38]. A review suggested that BEV combined therapy increased the incidence of side effects compared to BEV monotherapy [39]. Therefore, the potential for BEV to improve QoL remains uncertain and requires further validation.
Could subpopulations harboring some clinical or molecular characteristics gain survival benefits from BEV treatment?
A total of 17 studies (6 phase II trials, 2 prospective studies, and 9 retrospective studies) analyzed the types of rGBM that may favorably benefit from BEV-containing therapies. These studies analyzed the association between different genetic alterations, such as MGMT methylation, IDH mutation, and EGFR alteration and clinical features such as age groups, laboratory examinations, and radiological characteristics (Table 4).
MGMT methylation status
MGMT methylation status was assessed in six studies (4 phase II trials and 2 retrospective studies) to determine its association with responses to BEV [38, 40, 41]. A phase II trial found that BEV plus ONA improved OS in patients with rGBM having unmethylated MGMT (mOS, ONA + BEV vs. PLA + BEV, 10.9 vs. 7.5 months, p = 0.0836), compared with BEV plus placebo while BEV monotherapy favored outcome in patients with rGBM harboring methylated MGMT (mOS, ONA + BEV vs. PLA + BEV, 7.7 months vs. NR, p = 0.0150) [40]. A retrospective study on BEV plus osimertinib treatment was marginally effective in most GB patients with simultaneous EGFR amplification plus EGFRvIII mutation [20]. Another retrospective study compared the post-recurrence survival between patients with MGMT methylation and unmethylation, treated with BEV plus alkylating agents and found no difference between the two groups [41]. Nevertheless, another phase II trial did not find differences in QoL between the groups with GBM having MGMT methylation and unmethylation to BEV plus TMZ [38].
IDH mutation status
The association between IDH mutation status and response to BEV has been investigated in one phase II trial and two retrospective studies. Subgroup analysis of the BELOB trial revealed that patients with IDH mutation had higher OS and PFS compared to the control (mOS, IDH mutant vs. IDH wildtype: 20 vs. 9 months, p = 0.021) [13]. Dono et al. revealed an association between the genetic alterations and response to stereotactic radiosurgery (SRS) and BEV-containing chemotherapy in patients with rGBM carrying IDH-wildtype. Moreover, PTEN mutant subgroup in IDH WT group was found to have longer PFS and OS after combination therapy (mOS, PTEN mutant vs. PTEN wildtype: 22.5 vs. 13.6 months, p = 0.07; mPFS, PTEN mutant vs. PTEN wildtype: 17.5 vs. 8.1 months, p = 0.04) [42]. A retrospective study conducted by Lv et al. revealed that rGBM carrying IDH mutation had a better prognosis (OS and PFS) after receiving a BEV-containing regimen, compared with rGBM without IDH mutation (BEV monotherapy, mOS, IDH mutant vs. IDH wildtype: 10.16 vs. 4.9 months; mPFS, IDH mutant vs. IDH wildtype: 3.23 vs. 1.37 months, p = 0.04; BEV plus sunitinib, mOS, IDH mutant vs. IDH wildtype: 7.53 vs. 4.83 months; mPFS, IDH mutant vs. IDH wildtype: 2.07 vs. 1.10 months, p = 0.06), while no difference was found between IDH wildtype and mutated rGBM receiving non-BEV regimens (cetuximab and sunitinib) [43].
EGFR alteration status
A phase II trial found that EGFR vIII positive rGBM had PFS and OS benefits from BEV plus rindopepimut therapy (HR for BEV plus rindopepimut, 0.58, p = 0.01).
Radiological characteristics
Apart from genetic alterations, the association between radiological examination outcome and response to BEV was elucidated. Cox regression analysis in a phase II trial showed that BEV improved survival in patients with large enhancing tumors with low apparent diffusion coefficient (ADCL). It also revealed that the pretreatment tumor volume was an independent risk factor for the BEV-treated group [44]. A prospective study revealed that patients with hyperintense lesions in T1 and diffusion-weighted restriction (double-positive) benefited more than others from BEV treatment [34, 45]. A retrospective study demonstrated that rGBM with a large tumor burden might be benefitted most favorably from BEV-containing regimens [15].
Laboratory examinations
A prospective trial in 2019 stated that low neutrophil counts (below 3.9 G/L) and high Treg counts (above 0.011 G/L) predicted prolonged OS [46].
Age groups
No consensus was found regarding the association between BEV efficacy and age groups. Two retrospective studies found that there was a better improvement in non-elderly patients with rGBM/recurrent high-grade glioma (rHGG) patients compared with elderly patients treated with BEV-containing regimens [47, 48]. However, another retrospective study concluded controversially that elderly patients had more prognostic benefits compared with younger patients [49].
What are the optimal dosages and indications for BEV administration?
The optimal dosages and indications for BEV administration are still under investigation. In the US, the recommended dosage of BEV in the US is a 10 mg/kg intravenous infusion administered every 2 weeks. However, different studies (2 retrospective studies and 2 reviews, Table 5) have adopted varying dosages, and recent research has elucidated the optimal dosage. Two retrospective studies stated that lower doses were at least equal or even superior to the recommended doses [50, 51]. Two reviews had similar conclusions [37, 49]. Although BEV at the recommended dose and lower dose exhibits equal efficacy on survival, influence on other outcomes such as QoL and side effects reduction needs further investigation.
The window of opportunity for BEV treatment is also still under debate. Matsuoka et al. argued that the initiation of a treatment regimen containing BEV at first recurrence may improve prognosis. However, they also noted that BEV administration could lead to chemotherapy resistance and rapid progression in some cases [34]. Similar conclusions were made in other studies. A retrospective study found that BEV treatment before surgery might be beneficial for young and high-performance patients [52]. No significant difference in OS was identified between patients receiving BEV-containing regimens after the first relapse and the second relapse [53]. However, some studies concluded contrastingly. Funakoshi et al. found that BEV administration after recurrence (post-BEV) improved PFS and deterioration-free survival (DFS) than pre-recurrence BEV administration (pre-BEV) (mPFS, post-BEV vs. pre-BEV: 9.9 vs. 7.5 months, p = 0.0153; mDFS, post-BEV vs. pre-BEV: 13.8 vs. 8.5 months, p = 0.0046) [54]. Therefore, the optimal opportunity window of BEV treatment warrants further validation through future large-scale clinical trials. Table 5 summarizes the different findings across studies.
Discussion
BEV has shown improved PFS in clinical studies, but OS benefits have not been consistently observed. Despite this, BEV has been proposed as a promising drug in GBM due to its ability to reduce side effects from steroid use and radiotherapy. To further maximize benefits from BEV treatment, investigations could be summarized in two ways. One was to combine BEV with other treatment modalities to enhance synergistic anti-tumor effects. The other one was to identify the BEV-response groups which could gain more prognostic benefits from the treatment of BEV. Additionally, we investigated the optimal dosage and treatment opportunity window to maximize the BEV treatment benefits. To the best of our knowledge, BEV-containing multimodality treatment was associated with clinical benefit and is worthy of administration. The outcome depends on the unique clinical and molecular features linked to varied BEV responses.
Despite many efforts in the past, the efficacy of BEV remains to be optimized and needs further investigations focusing on the two mechanisms mentioned above. First, newly emerging therapies for rGBM bring further opportunities for BEV-containing multimodality treatment. TTF was the landmark therapy in the treatment of GBM [55]. Post-hoc analysis of EF-14 in a phase III trial on newly diagnosed GBM revealed that the addition of TTF to BEV could further prolong the median OS by 2 months beyond the period that patients with rGBM achieved with second-line treatment alone [56]. Studies of higher evidence are warranted to investigate the efficacy of BEV plus TTF combination therapies. Besides TTF, an increasing number of combination therapies are currently explored via several clinical trials (e.g., NCT02511405, VB-111 plus BEV; NCT01308684, RO5323441 plus BEV; NCT01349660, BKM120 plus BEV).
Second, biomarker-enrichment strategies are warranted to direct the clinical administration of BEV. While BEV administration has been shown to improve OS in the TCGA-proneural newly diagnosed GBM subtype, characterizing rGBM according to TCGA transcriptome classification in a realistic manner requires further exploration. Moreover, high-quality evidence is lacking regarding the associations between molecular and clinical features with BEV response. Therefore, RCTs focusing on specific subpopulations of rGBM are warranted.
In summary, current RCTs are not sufficient to make a definitive statement that BEV could improve OS and QoL in patients with rGBM although some clinical benefits (including PFS, decreased steroid use, and cognitive ability protection) are observed. Combing BEV with TTF and administration at first recurrence may improve prognosis. In the meantime, rGBM with low ADCL, large tumor burden, or IDH mutation is more likely to benefit from BEV treatment. Of note, observational studies have yielded conflicting results due to heterogeneity. High-quality clinical trials are needed to gain new insights into BEV treatment, and breakthroughs may emerge from the use of BEV-containing multimodality treatment on unique subpopulations of rGBM.
Data Availability
All data generated or analyzed during this study are included in this published article.
Abbreviations
- ADCL:
-
Apparent diffusion coefficient
- AEs:
-
Adverse events
- BEV:
-
Bevacizumab
- BSC:
-
Best supportive care
- CCT:
-
Case-control trial
- DFS:
-
Deterioration-free survival
- EANO:
-
European Association for Neuro-Oncology
- FDA:
-
U.S. Food and Drug Administration
- FSRS:
-
Fractionated stereotactic radiosurgery
- GBM:
-
Glioblastoma
- GKSR:
-
Gamma Knife stereotactic radiosurgery
- HSRS:
-
Hypofractionated stereotactic radiosurgery
- IRI:
-
Irinotecan
- KPS:
-
Karnofsky Performance Status
- MGMT:
-
O6-methylguanine-DNA methyltransferase
- mOS:
-
Median OS
- ORR:
-
Objective response rates
- OS:
-
Overall survival
- PFS:
-
Progression-free survival
- QoL:
-
Quality of life
- RCT:
-
Randomized controlled trial
- RT:
-
Radiotherapy
- rGBM:
-
Recurrent glioblastoma
- rHGG:
-
Recurrent high-grade glioma
- SAEs:
-
Severe adverse events
- SRS:
-
Stereotactic radiosurgery
References
Stupp R, Taillibert S, Kanner A, Read W, Steinberg D, Lhermitte B, Toms S, Idbaih A, Ahluwalia MS, Fink K, et al. Effect of Tumor-Treating Fields Plus maintenance temozolomide vs maintenance temozolomide alone on survival in patients with glioblastoma: a Randomized Clinical Trial. JAMA. 2017;318(23):2306–16.
Kumar AA, Abraham Koshy A. Regression of recurrent High-Grade Glioma with Temozolomide, Dexamethasone, and Levetiracetam: Case Report and Review of the literature. World Neurosurg. 2017;108:990. e911-990 e916.
Seyedmirzaei H, Shobeiri P, Turgut M, Hanaei S, Rezaei N. VEGF levels in patients with glioma: a systematic review and meta-analysis. Rev Neurosci. 2021;32(2):191–202.
Qu CY, Zheng Y, Zhou M, Zhang Y, Shen F, Cao J, Xu LM. Value of bevacizumab in treatment of colorectal cancer: a meta-analysis. World J Gastroenterol. 2015;21(16):5072–80.
Hainsworth JD, Sosman JA, Spigel DR, Edwards DL, Baughman C, Greco A. Treatment of metastatic renal cell carcinoma with a combination of bevacizumab and erlotinib. J Clin Oncol. 2005;23(31):7889–96.
Besse B, Le Moulec S, Mazieres J, Senellart H, Barlesi F, Chouaid C, Dansin E, Berard H, Falchero L, Gervais R, et al. Bevacizumab in patients with Nonsquamous Non-Small Cell Lung Cancer and Asymptomatic, untreated brain metastases (BRAIN): a Nonrandomized, phase II study. Clin Cancer Res. 2015;21(8):1896–903.
Kehoe S. Bevacizumab and treatment of cervical cancer. Maturitas. 2014;79(4):355–6.
van den Bent MJ, Klein M, Smits M, Reijneveld JC, French PJ, Clement P, de Vos FYF, Wick A, Mulholland PJ, Taphoorn MJB, et al. Bevacizumab and temozolomide in patients with first recurrence of WHO grade II and III glioma, without 1p/19q co-deletion (TAVAREC): a randomised controlled phase 2 EORTC trial. Lancet Oncol. 2018;19(9):1170–9.
Wick W, Gorlia T, Bendszus M, Taphoorn M, Sahm F, Harting I, Brandes AA, Taal W, Domont J, Idbaih A, et al. Lomustine and Bevacizumab in Progressive Glioblastoma. N Engl J Med. 2017;377(20):1954–63.
Weller M, van den Bent M, Tonn JC, Stupp R, Preusser M, Cohen-Jonathan-Moyal E, Henriksson R, Le Rhun E, Balana C, Chinot O, et al. European Association for Neuro-Oncology (EANO) guideline on the diagnosis and treatment of adult astrocytic and oligodendroglial gliomas. Lancet Oncol. 2017;18(6):e315–29.
Weller M, van den Bent M, Preusser M, Le Rhun E, Tonn JC, Minniti G, Bendszus M, Balana C, Chinot O, Dirven L, et al. EANO guidelines on the diagnosis and treatment of diffuse gliomas of adulthood. Nat Rev Clin Oncol. 2021;18(3):170–86.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, Moher D, Peters MDJ, Horsley T, Weeks L, et al. PRISMA Extension for scoping reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169(7):467–73.
Taal W, Oosterkamp HM, Walenkamp AM, Dubbink HJ, Beerepoot LV, Hanse MC, Buter J, Honkoop AH, Boerman D, de Vos FY, et al. Single-agent bevacizumab or lomustine versus a combination of bevacizumab plus lomustine in patients with recurrent glioblastoma (BELOB trial): a randomised controlled phase 2 trial. Lancet Oncol. 2014;15(9):943–53.
Weathers SP, Han X, Liu DD, Conrad CA, Gilbert MR, Loghin ME, O’Brien BJ, Penas-Prado M, Puduvalli VK, Tremont-Lukats I, et al. A randomized phase II trial of standard dose bevacizumab versus low dose bevacizumab plus lomustine (CCNU) in adults with recurrent glioblastoma. J Neurooncol. 2016;129(3):487–94.
Nguyen HT, Nguyen N, Liu LY, Dovek L, Lenchner D, Harris R, Ozer B, Ravelo A, Sommer N, Sim MS, et al. Bevacizumab at first recurrence after standard radio-chemotherapy is associated with improved overall survival in glioblastoma patients with large tumor burden. Neuro-oncology Pract. 2019;6(2):103–11.
Heiland DH, Masalha W, Franco P, Machein MR, Weyerbrock A. Progression-free and overall survival in patients with recurrent Glioblastoma multiforme treated with last-line bevacizumab versus bevacizumab/lomustine. J Neurooncol. 2016;126(3):567–75.
Zheng X, Tang Q, Ren L, Liu J, Li W, Fu W, Wang J, Du G. A narrative review of research progress on drug therapies for glioblastoma multiforme. Annals of translational medicine. 2021;9(11):943.
Song J, Xue YQ, Zhao MM, Xu P. Effectiveness of lomustine and bevacizumab in progressive glioblastoma: a meta-analysis. OncoTargets and therapy. 2018;11:3435–9.
Welch M, Lai R. Glioblastoma multiforme. Curr Treat options Neurol. 2009;11(4):297–305.
Cardona AF, Jaramillo-Velásquez D, Ruiz-Patiño A, Polo C, Jiménez E, Hakim F, Gómez D, Ramón JF, Cifuentes H, Mejía JA, et al. Efficacy of osimertinib plus bevacizumab in glioblastoma patients with simultaneous EGFR amplification and EGFRvIII mutation. J Neurooncol. 2021;154(3):353–64.
Peng C, Wang J, Tanksley JP, Mobley BC, Ayers GD, Moots PL, Clark SW. Valganciclovir and bevacizumab for recurrent glioblastoma: a single-institution experience. Mol Clin Oncol. 2016;4(2):154–8.
Bergman D, Modh A, Schultz L, Snyder J, Mikkelsen T, Shah M, Ryu S, Siddiqui MS, Walbert T. Randomized prospective trial of fractionated stereotactic radiosurgery with chemotherapy versus chemotherapy alone for bevacizumab-resistant high-grade glioma. J Neurooncol. 2020;148(2):353–61.
Morris SL, Zhu P, Rao M, Martir M, Zhu JJ, Hsu S, Ballester LY, Day AL, Tandon N, Kim DH, et al. Gamma Knife Stereotactic Radiosurgery in Combination with Bevacizumab for recurrent glioblastoma. World Neurosurg. 2019;127:e523–33.
Palmer JD, Bhamidipati D, Song A, Eldredge-Hindy HB, Siglin J, Dan TD, Champ CE, Zhang I, Bar-Ad V, Kim L, et al. Bevacizumab and re-irradiation for recurrent high grade gliomas: does sequence matter? J Neurooncol. 2018;140(3):623–8.
Schernberg A, Dhermain F, Ammari S, Dumont SN, Domont J, Patrikidou A, Pallud J, Dezamis É, Deutsch É, Louvel G. Reirradiation with concurrent bevacizumab for recurrent high-grade gliomas in adult patients. Cancer radiotherapie: journal de la Societe francaise de radiotherapie oncologique. 2018;22(1):9–16.
Clark GM, McDonald AM, Nabors LB, Fathalla-Shaykh H, Han X, Willey CD, Markert JM, Guthrie BL, Bredel M, Fiveash JB. Hypofractionated stereotactic radiosurgery with concurrent bevacizumab for recurrent malignant gliomas: the University of Alabama at Birmingham experience. Neuro-oncology Pract. 2014;1(4):172–7.
Yamaguchi S, Motegi H, Ishi Y, Okamoto M, Sawaya R, Kobayashi H, Terasaka S, Houkin K. Clinical outcome of cytoreductive surgery prior to Bevacizumab for patients with recurrent glioblastoma: a single-center retrospective analysis. Neurologia medico-chirurgica. 2021;61(4):245–52.
Azoulay M, Santos F, Shenouda G, Petrecca K, Oweida A, Guiot MC, Owen S, Panet-Raymond V, Souhami L, Abdulkarim BS. Benefit of re-operation and salvage therapies for recurrent glioblastoma multiforme: results from a single institution. J Neurooncol. 2017;132(3):419–26.
Kesari S, Ram Z. Tumor-treating fields plus chemotherapy versus chemotherapy alone for glioblastoma at first recurrence: a post hoc analysis of the EF-14 trial. CNS Oncol. 2017;6(3):185–93.
Nagpal S, Harsh G, Recht L. Bevacizumab improves quality of life in patients with recurrent glioblastoma. Chemother Res Pract. 2011;2011:602812.
Diaz RJ, Ali S, Qadir MG, De La Fuente MI, Ivan ME, Komotar RJ. The role of bevacizumab in the treatment of glioblastoma. Journal of neuro-oncology 2017, 133(3):455–467.
Keyrouz VF, Elias E, Chahine GY, Comair YG, Dimassi H, Kamar FG. Updated results of a phase II trial of bevacizumab and irinotecan in relapsed high-grade glioma. Neurooncology. 2010;12:iii47.
Wick W, Osswald M, Wick A, Winkler F. Treatment of glioblastoma in adults. Ther Adv Neurol Disord. 2018;11:1756286418790452.
Kamiya-Matsuoka C, Gilbert MR. Treating recurrent glioblastoma: an update. CNS Oncol. 2015;4(2):91–104.
Larson EW, Peterson HE, Lamoreaux WT, MacKay AR, Fairbanks RK, Call JA, Carlson JD, Ling BC, Demakas JJ, Cooke BS, et al. Clinical outcomes following salvage Gamma Knife radiosurgery for recurrent glioblastoma. World J Clin Oncol. 2014;5(2):142–8.
Liu Y, Feng F, Ji P, Liu B, Ge S, Yang C, Lou M, Liu J, Li B, Gao G, et al. Improvement of health related quality of life in patients with recurrent glioma treated with bevacizumab plus daily temozolomide as the salvage therapy. Clin Neurol Neurosurg. 2018;169:64–70.
Mallick S, Benson R, Hakim A, Rath GK. Management of glioblastoma after recurrence: a changing paradigm. J Egypt Natl Cancer Inst. 2016;28(4):199–210.
Badruddoja MA, Pazzi M, Sanan A, Schroeder K, Kuzma K, Norton T, Scully T, Mahadevan D, Ahmadi MM. Phase II study of bi-weekly temozolomide plus bevacizumab for adult patients with recurrent glioblastoma. Cancer Chemother Pharmacol. 2017;80(4):715–21.
McBain C, Lawrie TA, Rogozińska E, Kernohan A, Robinson T, Jefferies S. Treatment options for progression or recurrence of glioblastoma: a network meta-analysis. Cochrane Database Syst Rev. 2021;5(1):Cd013579.
Cloughesy T, Finocchiaro G, Belda-Iniesta C, Recht L, Brandes AA, Pineda E, Mikkelsen T, Chinot OL, Balana C, Macdonald DR et al. Randomized, Double-Blind, Placebo-Controlled, Multicenter Phase II Study of Onartuzumab Plus Bevacizumab Versus Placebo Plus Bevacizumab in Patients With Recurrent Glioblastoma: Efficacy, Safety, and Hepatocyte Growth Factor and O(6)-Methylguanine-DNA Methyltransferase Biomarker Analyses. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 2017, 35(3):343–351.
Seystahl K, Hentschel B, Loew S, Gramatzki D, Felsberg J, Herrlinger U, Westphal M, Schackert G, Thon N, Tatagiba M, et al. Bevacizumab versus alkylating chemotherapy in recurrent glioblastoma. J Cancer Res Clin Oncol. 2020;146(3):659–70.
Dono A, Amsbaugh M, Martir M, Smilie RH, Riascos RF, Zhu JJ, Hsu S, Kim DH, Tandon N, Ballester LY, et al. Genomic alterations predictive of response to radiosurgery in recurrent IDH-WT glioblastoma. J Neurooncol. 2021;152(1):153–62.
Lv S, Teugels E, Sadones J, Quartier E, Huylebrouck M, S DUF, Salmon MLEMODEW, Michotte I. Correlation between IDH1 gene mutation status and survival of patients treated for recurrent glioma. Anticancer Res. 2011;31(12):4457–63.
Patel KS, Everson RG, Yao J, Raymond C, Goldman J, Schlossman J, Tsung J, Tan C, Pope WB, Ji MS, et al. Diffusion magnetic resonance imaging phenotypes predict overall Survival Benefit from Bevacizumab or surgery in recurrent Glioblastoma with large Tumor Burden. Neurosurgery. 2020;87(5):931–8.
Bähr O, Harter PN, Weise LM, You SJ, Mittelbronn M, Ronellenfitsch MW, Rieger J, Steinbach JP, Hattingen E. Sustained focal antitumor activity of bevacizumab in recurrent glioblastoma. Neurology. 2014;83(3):227–34.
Quillien V, Carpentier AF, Gey A, Avril T, Tartour E, Sejalon F, Campillo-Gimenez B, Vauleon E. Absolute numbers of regulatory T cells and neutrophils in corticosteroid-free patients are predictive for response to bevacizumab in recurrent glioblastoma patients. Cancer Immunol immunotherapy: CII. 2019;68(6):871–82.
Birk HS, Han SJ, Butowski NA. Treatment options for recurrent high-grade gliomas. CNS Oncol. 2017;6(1):61–70.
Barrascout E, Lamuraglia M. Glioblastoma and bevacizumab in elderly patients: monocentric study. J Oncol Pharm practice: official publication Int Soc Oncol Pharm Practitioners. 2021;27(4):842–6.
Hundsberger T, Reardon DA, Wen PY. Angiogenesis inhibitors in tackling recurrent glioblastoma. Expert Rev Anticancer Ther 2017, 17(6):507–15.
Lorgis V, Maura G, Coppa G, Hassani K, Taillandier L, Chauffert B, Apetoh L, Ladoire S, Ghiringhelli F. Relation between bevacizumab dose intensity and high-grade glioma survival: a retrospective study in two large cohorts. J Neurooncol. 2012;107(2):351–8.
Levin VA, Mendelssohn ND, Chan J, Stovall MC, Peak SJ, Yee JL, Hui RL, Chen DM. Impact of bevacizumab administered dose on overall survival of patients with progressive glioblastoma. J Neurooncol. 2015;122(1):145–50.
Blumenthal DT, Kanner AA, Aizenstein O, Cagnano E, Greenberg A, Hershkovitz D, Ram Z, Bokstein F. Surgery for recurrent High-Grade Glioma after treatment with Bevacizumab. World Neurosurg. 2018;110:e727–37.
Sahebjam S, Garoufalis E, Guiot MC, Muanza T, Del Maestro R, Petrecca K, Sharma R, Kavan P. Bevacizumab use for recurrent high-grade glioma at McGill University Hospital. Can J Neurol Sci Le J canadien des Sci neurologiques. 2013;40(2):241–6.
Funakoshi Y, Takigawa K, Hata N, Kuga D, Hatae R, Sangatsuda Y, Fujioka Y, Otsuji R, Sako A, Yoshitake T et al. Changes in the Relapse Pattern and Prognosis of Glioblastoma After Approval of First-Line Bevacizumab: A Single-Center Retrospective Study. World neurosurgery 2021.
Hong P, Kudulaiti N, Wu S, Nie J, Zhuang D. Tumor treating fields: a comprehensive overview of the underlying molecular mechanism. Expert Rev Mol Diagn. 2022;22(1):19–28.
Ram Z, Kim CY, Hottinger AF, Idbaih A, Nicholas G, Zhu JJ. Efficacy and safety of Tumor Treating Fields (TTFields) in Elderly patients with newly diagnosed Glioblastoma: Subgroup Analysis of the phase 3 EF-14 clinical trial. Front Oncol. 2021;11:671972.
Moen MD. Bevacizumab: in previously treated glioblastoma. Drugs. 2010;70(2):181–9.
Chamberlain MC. Emerging clinical principles on the use of bevacizumab for the treatment of malignant gliomas. Cancer. 2010;116(17):3988–99.
Park KJ, Kano H, Iyer A, Liu X, Niranjan A, Flickinger JC, Lieberman FS, Lunsford LD, Kondziolka D. Salvage gamma knife stereotactic radiosurgery followed by bevacizumab for recurrent glioblastoma multiforme: a case-control study. J Neurooncol. 2012;107(2):323–33.
Khasraw M, Ameratunga M, Grommes C. Bevacizumab for the treatment of high-grade glioma: an update after phase III trials. Expert Opin Biol Ther. 2014;14(5):729–40.
Chauffer B, Feuvret L, Bonnetain F, Taillandier L, Frappaz D, Taillia H, Schott R, Honnorat J, Fabbro M, Tennevet I, et al. Randomized phase II trial of irinotecan and bevacizumab as neo-adjuvant and adjuvant to temozolomide-based chemoradiation compared with temozolomide-chemoradiation for unresectable glioblastoma: final results of the TEMAVIR study from ANOCEF. Ann Oncol. 2014;25(7):1442–7.
Tosoni A, Franceschi E, Poggi R, Brandes AA. Relapsed glioblastoma: treatment strategies for initial and subsequent recurrences. Curr Treat Options Oncol. 2016;17(9):49.
Balana C, De Las Penas R, Sepulveda JM, Gil-Gil MJ, Luque R, Gallego O, Carrato C, Sanz C, Reynes G, Herrero A, et al. Bevacizumab and temozolomide versus temozolomide alone as neoadjuvant treatment in unresected glioblastoma: the GENOM 009 randomized phase II trial. J Neurooncol. 2016;127(3):569–79.
Ruiz-Sánchez D, Peinado II, Alaguero-Calero M, Sastre-Heres AJ, Diez BG, Peña-Díaz J. Cost-effectiveness analysis of the bevacizumab-irinotecan regimen in the treatment of primary glioblastoma multiforme recurrences. Oncol Lett. 2016;12(3):1935–40.
Lombardi G, Pambuku A, Bellu L, Farina M, Della Puppa A, Denaro L, Zagonel V. Effectiveness of antiangiogenic drugs in glioblastoma patients: a systematic review and meta-analysis of randomized clinical trials. Crit Rev Oncol/Hematol. 2017;111:94–102.
Reardon DA, Lassman AB, Schiff D, Yunus SA, Gerstner ER, Cloughesy TF, Lee EQ, Gaffey SC, Barrs J, Bruno J, et al. Phase 2 and biomarker study of trebananib, an angiopoietin-blocking peptibody, with and without bevacizumab for patients with recurrent glioblastoma. Cancer. 2018;124(7):1438–48.
Carter TC, Medina-Flores R, Lawler BE. Glioblastoma treatment with Temozolomide and Bevacizumab and overall survival in a rural Tertiary Healthcare Practice. Biomed Res Int. 2018;2018:6204676.
Ameratunga M, Pavlakis N, Wheeler H, Grant R, Simes J, Khasraw M. Anti-angiogenic therapy for high-grade glioma. Cochrane Database of Systematic Reviews 2018, 2018(11).
Kim IH. Appraisal of re-irradiation for the recurrent glioblastoma in the era of MGMT promotor methylation. Radiation Oncol J. 2019;37(1):1–12.
Brandes AA, Gil-Gil M, Saran F, Carpentier AF, Nowak AK, Mason W, Zagonel V, Dubois F, Finocchiaro G, Fountzilas G, et al. A randomized phase II trial (TAMIGA) evaluating the efficacy and safety of continuous Bevacizumab through multiple lines of treatment for recurrent glioblastoma. Oncologist. 2019;24(4):521–8.
Huang YK, Lieu AS. Treatment response of bevacizumab combination chemotherapy in recurrent glioblastoma: a long-term retrospective study in Taiwan. Medicine. 2020;99(8):e19226.
Reardon DA, Brandes AA, Omuro A, Mulholland P, Lim M, Wick A, Baehring J, Ahluwalia MS, Roth P, Bähr O, et al. Effect of Nivolumab vs Bevacizumab in patients with recurrent glioblastoma: the CheckMate 143 phase 3 Randomized Clinical Trial. JAMA Oncol. 2020;6(7):1003–10.
Roth P, Hottinger AF, Hundsberger T, Läubli H, Schucht P, Reinert M, Mamot C, Roelcke U, Pesce G, Hofer S, et al. A contemporary perspective on the diagnosis and treatment of diffuse gliomas in adults. Swiss Med Wkly. 2020;150:w20256.
Tan AC, Ashley DM, Lopez GY, Malinzak M, Friedman HS, Khasraw M. Management of glioblastoma: state of the art and future directions. Cancer J Clin. 2020;70(4):299–312.
Hofmann S, Schmidt MA, Weissmann T, Eyüpoglu I, Strnad A, Semrau S, Fietkau R, Putz F, Lettmaier S. Evidence for improved survival with bevacizumab treatment in recurrent high-grade gliomas: a retrospective study with (“pseudo-randomized”) treatment allocation by the health insurance provider. J Neurooncol. 2020;148(2):373–9.
Lovo EE, Moreira A, Barahona KC, Ramirez J, Campos F, Tobar C, Caceros V, Sallabanda M, Sallabanda K. Stereotactic radiosurgery for recurrent Glioblastoma Multiforme: a retrospective multi-institutional experience. Cureus. 2021;13(10):e18480.
Guan Y, Xiong J, Pan M, Shi W, Li J, Zhu H, Gong X, Li C, Mei G, Liu X, et al. Safety and efficacy of hypofractionated stereotactic radiosurgery for high-grade gliomas at first recurrence: a single-center experience. BMC Cancer. 2021;21(1):123.
Friedman HS, Prados MD, Wen PY, Mikkelsen T, Schiff D, Abrey LE, Yung WK, Paleologos N, Nicholas MK, Jensen R, et al. Bevacizumab alone and in combination with irinotecan in recurrent glioblastoma. J Clin oncology: official J Am Soc Clin Oncol. 2009;27(28):4733–40.
Chinnaiyan P, Chowdhary S, Potthast L, Prabhu A, Tsai YY, Sarcar B, Kahali S, Brem S, Yu HM, Rojiani A, et al. Phase I trial of vorinostat combined with bevacizumab and CPT-11 in recurrent glioblastoma. Neurooncology. 2012;14(1):93–100.
Johansson F, Ekman S, Blomquist E, Henriksson R, Bergström S, Bergqvist M. A review of dose-dense temozolomide alone and in combination with bevacizumab in patients with first relapse of glioblastoma. Anticancer Res. 2012;32(9):4001–6.
Weller M, Cloughesy T, Perry JR, Wick W. Standards of care for treatment of recurrent glioblastoma–are we there yet? Neurooncology. 2013;15(1):4–27.
Soffietti R, Trevisan E, Bertero L, Cassoni P, Morra I, Fabrini MG, Pasqualetti F, Lolli I, Castiglione A, Ciccone G et al. Bevacizumab and fotemustine for recurrent glioblastoma: a phase II study of AINO (Italian Association of Neuro-Oncology). Journal of neuro-oncology 2014, 116(3):533–541.
Wong ET, Lok E, Swanson KD. Clinical benefit in recurrent glioblastoma from adjuvant NovoTTF-100A and TCCC after temozolomide and bevacizumab failure: a preliminary observation. Cancer Med. 2015;4(3):383–91.
Wu J, Puduvalli VK, Yuan Y, Armstrong T, Walker B, Upshaw C, Giglio P, Colman H, Groves MD, Raizer J, et al. Bayesian adaptive randomized phase II trial of bevacizumab plus vorinostat versus bevacizumab alone in adults with recurrent glioblastoma. Neurooncology. 2015;17:v9.
Puduvalli VK, Wu J, Yuan Y, Armstrong TS, Groves MD, Raizer JJ, Giglio P, Colman H, Peereboom DM, Walbert T et al. Brain tumor trials collaborative bayesian adaptive randomized phase II trial of bevacizumab plus vorinostat versus bevacizumab alone in adults with recurrent glioblastoma (BTTC-1102). J Clin Oncol 2015, 33(15).
Galanis E, Anderson SK, Anastasiadis P, Tran DD, Jeyapalan SA, Anderson DM, Kaufmann TJ, Giannini C, Buckner JC, Schiff D. NCCTG N0872 (Alliance): a randomized placebo-controlled phase II trial of bevacizumab plus dasatinib in patients with recurrent glioblastoma (GBM). J Clin Oncol 2015, 33(15).
Field KM, Simes J, Nowak AK, Cher L, Wheeler H, Hovey EJ, Brown CS, Barnes EH, Sawkins K, Livingstone A, et al. Randomized phase 2 study of carboplatin and bevacizumab in recurrent glioblastoma. Neurooncology. 2015;17(11):1504–13.
Gilbert MR, Pugh SL, Aldape K, Sorensen AG, Mikkelsen T, Penas-Prado M, Bokstein F, Kwok Y, Lee RJ, Mehta M. NRG oncology RTOG 0625: a randomized phase II trial of bevacizumab with either irinotecan or dose-dense temozolomide in recurrent glioblastoma. Journal of neuro-oncology 2017, 131(1):193–199.
Lim Fat MJ, Maurice C, Maganti M, Mason WP. Bevacizumab in Recurrent High-Grade Gliomas: a canadian retrospective study. Can J Neurol Sci Le J canadien des Sci neurologiques. 2018;45(1):56–61.
Bota DA, Chung J, Dandekar M, Carrillo JA, Kong XT, Fu BD, Hsu FP, Schonthal AH, Hofman FM, Chen TC, et al. Phase II study of ERC1671 plus bevacizumab versus bevacizumab plus placebo in recurrent glioblastoma: interim results and correlations with CD4(+) T-lymphocyte counts. CNS Oncol. 2018;7(3):CNS22.
Galanis E, Anderson SK, Twohy EL, Carrero XW, Dixon JG, Tran DD, Jeyapalan SA, Anderson DM, Kaufmann TJ, Feathers RW, et al. A phase 1 and randomized, placebo-controlled phase 2 trial of bevacizumab plus dasatinib in patients with recurrent glioblastoma: Alliance/North Central Cancer Treatment Group N0872. Cancer. 2019;125(21):3790–800.
Lee EQ, Zhang P, Wen PY, Gerstner ER, Reardon DA, Aldape KD, deGroot JF, Pan E, Raizer JJ, Kim LJ, et al. NRG/RTOG 1122: a phase 2, double-blinded, placebo-controlled study of bevacizumab with and without trebananib in patients with recurrent glioblastoma or gliosarcoma. Cancer. 2020;126(12):2821–8.
Puduvalli VK, Wu J, Yuan Y, Armstrong TS, Vera E, Wu J, Xu J, Giglio P, Colman H, Walbert T, et al. A bayesian adaptive randomized phase II multicenter trial of bevacizumab with or without vorinostat in adults with recurrent glioblastoma. Neuro Oncol. 2020;22(10):1505–15.
Chen W, Liu D, Liu P, Kong Z, Wang Y, Wang Y, Ma W. Current evidence and challenges of systematic therapies for adult recurrent glioblastoma: results from clinical trials. Chin J cancer research = Chung-kuo yen cheng yen chiu. 2021;33(3):417–32.
Detti B, Scoccianti S, Teriaca MA, Maragna V, Lorenzetti V, Lucidi S, Bellini C, Greto D, Desideri I, Livi L. Bevacizumab in recurrent high-grade glioma: a single institution retrospective analysis on 92 patients. Radiol Med. 2021;126(9):1249–54.
Vredenburgh JJ, Cloughesy T, Samant M, Prados M, Wen PY, Mikkelsen T, Schiff D, Abrey LE, Yung WK, Paleologos N, et al. Corticosteroid use in patients with glioblastoma at first or second relapse treated with bevacizumab in the BRAIN study. Oncologist. 2010;15(12):1329–34.
Kamiya-Matsuoka C, Hamza MA, de Groot JF. Impact of adverse events of bevacizumab on survival outcomes of patients with recurrent glioblastoma. J Clin neuroscience: official J Neurosurgical Soc Australasia. 2020;74:36–40.
Korshoej AR, Lukacova S, Lassen-Ramshad Y, Rahbek C, Severinsen KE, Guldberg TL, Mikic N, Jensen MH, Cortnum SOS, von Oettingen G, et al. OptimalTTF-1: enhancing tumor treating fields therapy with skull remodeling surgery. A clinical phase I trial in adult recurrent glioblastoma. Neuro-oncology Adv. 2020;2(1):vdaa121.
Nghiemphu PL, Liu W, Lee Y, Than T, Graham C, Lai A, Green RM, Pope WB, Liau LM, Mischel PS, et al. Bevacizumab and chemotherapy for recurrent glioblastoma: a single-institution experience. Neurology. 2009;72(14):1217–22.
Bertaut A, Truntzer C, Madkouri R, Kaderbhai CG, Derangère V, Vincent J, Chauffert B, Aubriot-Lorton MH, Farah W, Mourier KL, et al. Blood baseline neutrophil count predicts bevacizumab efficacy in glioblastoma. Oncotarget. 2016;7(43):70948–58.
Burger MC, Breuer S, Cieplik HC, Harter PN, Franz K, Bähr O, Steinbach JP. Bevacizumab for patients with recurrent multifocal glioblastomas. Int J Mol Sci 2017, 18(11).
Piccioni DE, Selfridge J, Mody RR, Chowdhury R, Li S, Lalezari S, Wawrzynski J, Quan J, Zurayk M, Chou AP, et al. Deferred use of bevacizumab for recurrent glioblastoma is not associated with diminished efficacy. Neurooncology. 2014;16(6):815–22.
Schaub C, Tichy J, Schäfer N, Franz K, Mack F, Mittelbronn M, Kebir S, Thiepold AL, Waha A, Filmann N, et al. Prognostic factors in recurrent glioblastoma patients treated with bevacizumab. J Neurooncol. 2016;129(1):93–100.
Prelaj A, Rebuzzi SE, Grassi M, Giròn Berrìos JR, Pecorari S, Fusto C, Ferrara C, Salvati M, Stati V, Tomao S, et al. Multimodal treatment for local recurrent malignant gliomas: Resurgery and/or reirradiation followed by chemotherapy. Mol Clin Oncol. 2019;10(1):49–57.
Acknowledgements
This research was supported by the Medical Research Data Center of Fudan university.
Funding
The study was funded by the National Natural Science Foundation of China (82072784, 82103690).
Author information
Authors and Affiliations
Contributions
M. F., Z. Z., and X. H. contributed equally to the study. All of them were responsible for conceptualization and had full access to all data for the analyses. All authors involved in data analysis and the original draft writing. Z. C., L. Z., and J. Z. made substantial contributions to acquisition, analysis, and interpretation. W. H. and Y. M. took the whole responsibility of supervision, collection of all information, a major revision of the manuscript, conceptualization, and submission of this manuscript. All authors have read and agreed to the submitted version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Fu, M., Zhou, Z., Huang, X. et al. Use of Bevacizumab in recurrent glioblastoma: a scoping review and evidence map. BMC Cancer 23, 544 (2023). https://doi.org/10.1186/s12885-023-11043-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-023-11043-6