Abstract
Background
Oncotype DX® (ODX) is used to assess risk of disease recurrence in hormone receptor positive, HER2-negative breast cancer and to guide decisions regarding adjuvant chemotherapy. Little is known about how physician factors impact treatment decisions. The purpose of this study was to examine patient and physician factors associated with ODX testing and adjuvant chemotherapy for breast cancer patients in New Hampshire.
Methods
We examined New Hampshire State Cancer Registry data on 5630 female breast cancer patients diagnosed from 2010 to 2016. We performed unadjusted and adjusted hierarchical logistic regression to identify factors associated with a patient’s receipt of ODX, being recommended and receiving chemotherapy, and refusing chemotherapy. We calculated intraclass correlation coefficients (ICCs) to examine the proportion of variance in clinical decisions explained by between-physician and between-hospital variation.
Results
Over the study period, 1512 breast cancer patients received ODX. After adjustment for patient and tumor characteristics, we found that patients seen by a male medical oncologist were less likely to be recommended chemotherapy following ODX (OR = 0.50 (95% CI = 0.34–0.74), p < 0.01). Medical oncologists with more clinical experience (reference: less than 10 years) were more likely to recommend chemotherapy (20–29 years: OR = 4.05 (95% CI = 1.57–10.43), p < 0.01; > 29 years: OR = 4.48 (95% CI = 1.68–11.95), p < 0.01). A substantial amount of the variation in receiving chemotherapy was due to variation between physicians, particularly among low risk patients (ICC = 0.33).
Conclusions
In addition to patient clinicopathologic characteristics, physician gender and clinical experience were associated with chemotherapy treatment following ODX testing. The significant variation between physicians indicates the potential for interventions to reduce variation in care.
Similar content being viewed by others
Background
Breast cancer (BC) is the leading cause of cancer in women worldwide and is the second leading cause of cancer death in women [1]. Hormone receptor (HR) positive (defined as estrogen receptor and/or progesterone receptor positive), axillary lymph node (LN) negative BC is the most common subtype in the United States [2]. The treatment paradigm has shifted in the past decade for BC, especially for this subtype [3,4,5]. Adjuvant chemotherapy had previously been recommended for all BC patients and resulted in improved mortality rates [6, 7]. However, risk stratification of women with HR positive, LN negative BC is a priority, because about 85% of these women are at low risk of disease recurrence with endocrine-modulating therapy alone and thus are unlikely to benefit from adjuvant chemotherapy [8, 9].
Currently, there exist multiple methods to predict risk of 10-year disease recurrence and the potential benefit of chemotherapy [10,11,12]. Oncotype DX® (Genomic Health Inc., Redwood City, CA) (ODX) is a widely-used prognostic breast cancer test which analyzes gene expression of 16 tumor-specific genes and 5 reference genes [11, 13]. It was commercially introduced in the United States in 2004 and shortly thereafter was recommended in guidelines released by the American Society for Clinical Oncology (ASCO) and the National Comprehensive Cancer Network (NCCN) [14, 15]. The assay provides an integer Recurrence Score (RS), ranging from 0 to 100, indicating low risk (RS < 18), intermediate risk (RS 18–30), or high risk (RS ≥ 31) of disease recurrence. Low risk patients are recommended to receive endocrine-modulating therapy (tamoxifen or aromatase inhibitors) only, and high risk patients are recommended to receive both endocrine-modulating therapy and adjuvant chemotherapy [11, 13, 16]. Intermediate risk patients, while previously recommended to receive adjuvant chemotherapy, were recently shown by the large prospective TAILORx trial to receive little benefit from chemotherapy, with a notable exception for younger patients [17]. Additional studies have also validated the usefulness of ODX in patients with LN positive disease [18,19,20].
Several studies have suggested that ODX test results influence subsequent treatment decisions. Approximately one-third to one-half of patient-physician pairs make a change in recommended treatment following ODX, generally eschewing adjuvant chemotherapy in favor of the less toxic endocrine-modulating-only regimen [21, 22]. Despite its clinical impact, some eligible patients are not tested, with the most common reason being that ODX was not offered by the physician [23]. Physicians’ lack of familiarity with genomic testing is a known barrier to clinical implementation [24].
Qualitative and quantitative studies have examined patient and physician characteristics associated with use of ODX, yet studies examining subsequent chemotherapy use following ODX testing have primarily focused on patient characteristics [21, 22, 25,26,27,28,29,30,31,32]. In this study, we examined New Hampshire State Cancer Registry data from 2010 to 2016 to identify clinicopathological factors, patient demographics, and physician and hospital characteristics that influenced receipt of the ODX test in BC patients, the physician’s decision to recommend chemotherapy, and the receipt of adjuvant chemotherapy by the patient.
Methods
Data sources
The New Hampshire State Cancer Registry (NHSCR) is maintained by the State of New Hampshire Department of Health and Human Services. This is a population-based database on incident reportable cancers for all New Hampshire residents and includes patient demographics, date and mode of diagnosis, and tumor characteristics including grade and stage [33]. The NHSCR achieved the highest standard (gold) certification of data quality from the North American Association of Central Cancer Registries throughout the study period [34].
We obtained physician characteristics from two sources. The National Plan and Provider Enumeration System (NPPES) Downloadable File from the Centers for Medicare and Medicaid Services (CMS) enumerates the National Provider Identifier (NPI) for all physicians in the United States. All HIPAA-covered entities (clinicians and organizations) have been required to hold an NPI since 2007. The NPPES file is continuously updated and contains nearly 5 million records [35]. The CMS Physician Compare National Downloadable File is another resource providing general information regarding physicians caring for Medicare eligible patients in the United States [36].
Study cohort and definitions
Our study cohort includes women residing in New Hampshire and diagnosed with breast cancer from 2010 to 2016, between the ages of 18 and 99. We excluded patients with ductal carcinoma in situ (DCIS) or unknown stage. We further excluded patients with no recorded medical oncologist in the registry. We included the characteristics of each patient’s primary medical oncologist, identified as having an NPI specialty designation in Gynecologic Oncology, Hematology, Hematology and Oncology, Medical Oncology, or Pediatric Hematology-Oncology.
Study variables
Outcome variables
The NHSCR documents whether patients receive ODX and their test results. It also includes variables describing each patient’s treatment plan including whether chemotherapy was recommended, whether it was given, and whether the patient refused chemotherapy after physician recommendation. This allowed us to examine multiple outcomes: use of ODX, being recommended chemotherapy following ODX, receiving chemotherapy following ODX, and chemotherapy refusal following ODX. We further examined factors associated with receiving chemotherapy stratified by ODX RS classification (low, intermediate, high).
Patient variables
Patient variables include sociodemographic characteristics (patient age at diagnosis, marital status, and payer) and tumor characteristics (year of diagnosis, size, grade, LN status, hormone receptor status, and clinical stage).
Physician variables
Physician variables include gender, clinical experience, and patient volume. To determine years of clinical experience for each physician, the difference between the physician’s graduation year and the patient’s year of diagnosis was calculated. Patient volume was calculated as the average number of BC patients in the NHSCR data treated per year for each physician. Average patient age was calculated as the mean age at diagnosis for all patients seen by the physician in the NHSCR. A binary variable was defined to discriminate between a patient being seen by a surgical oncologist or a general surgeon.
Statistical analysis
We first performed unadjusted analyses for all covariates. We developed multivariable logistic regression models to examine the likelihood of ODX receipt in relation to patient and provider factors. Variables found to be significant at alpha = 0.05 during unadjusted or adjusted analysis were retained for further analysis. Variables found to be non-significant in both were dropped from the final analyses. Finally, we performed hierarchical logistic regressions, specifying hospital or physician as a random effect. We identified the intraclass correlation coefficient (ICC) which quantifies the amount of clustering due to the random effect and not to the observed factors, in order to determine the contribution to the variance from the random effect, as previously reported [37,38,39]. Data analysis was performed with R version 3.6.0 [40].
Results
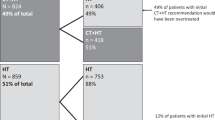
The initial NHSCR dataset contained 10,768 unique breast cancer patients diagnosed from 2010 through 2016 (Table 1). A small number of patients (n = 29) received MammaPrint, a similar genomic test, and these patients were excluded from analysis. A total of 91 patients were excluded due to ineligible age or gender. Patients were then excluded if they had DCIS (n = 2141), unknown stage (n = 341), or if they did not have a recorded medical oncologist (n = 2536), yielding a final cohort of 5630 women (Supplemental Figure S1). There were 225 unique medical oncologists treating the patients in the cohort (Table 2).
Receiving ODX
Of the total cohort, 1512 (26.9%) patients were tested with ODX. Over the course of the study period, overall use of ODX increased from 24.6% in 2010 to 29.1% in 2016 (p = 0.05) (Table 1). In unadjusted analyses, we found patient age, marital status, payer, tumor grade, LN status, tumor size, clinical stage, and being seen by an oncologist with an older average patient age were significantly associated with receiving ODX (Table S1). In the adjusted analysis, patient age, marital status, tumor grade, LN status, tumor size, and clinical stage contributed significantly to the model (Table 3). We then examined patient and physician characteristics associated with ODX testing specifically among patients eligible for ODX. Of the 2604 patients eligible for ODX, defined as stage 1 or 2, LN negative, and HR+/HER2-, 1132 (43.5%) received the test. ODX use in eligible patients ranged from 42.5% in 2010 to 45.4% in 2016 (p = 0.50). In the unadjusted analysis, patient age, marital status, tumor grade, tumor size, tumor stage, physician gender, physician patient volume, and being seen by an oncologist with an older average patient age were significantly associated with ODX use (Table S1). Only patient age, marital status, tumor grade, and tumor size contributed significantly to the adjusted model (Table S2).
Chemotherapy recommendation
Chemotherapy was recommended for 2701 (48.0%) patients in the breast cancer cohort and 459 (30.4%) of patients who received ODX. In the unadjusted analyses, we found year of diagnosis, patient age, tumor grade, LN status, tumor size, clinical stage, physician gender, clinical experience, physician patient volume, and ODX RS stratification to be significantly associated with a recommendation for chemotherapy (Table S1). In the adjusted model, year of diagnosis, patient age, tumor grade, LN status, tumor size, physician clinical experience, physician gender, physician patient volume, and ODX RS stratification were significantly associated with a recommendation for chemotherapy. Notably, we found that patients were less likely to be recommended chemotherapy if they were seen by a male (compared to female) medical oncologist (OR = 0.50 (95% CI = 0.34–0.74), p < 0.01). Compared with patients treated by medical oncologists with fewer than 10 years of clinical experience, patients treated by medical oncologists with more clinical experience were more likely to be recommended chemotherapy (20–29 years: OR = 4.05 (95% CI = 1.57–10.43), p < 0.01; > 29 years: OR = 4.48 (95% CI = 1.68–11.95), p < 0.01) (Table 4).
Receiving chemotherapy
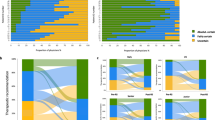
Receipt of chemotherapy was documented in 2264 (40.2%) patients in the breast cancer cohort, and 336 (22.2%) of patients who received ODX. Receipt of chemotherapy among patients who did not receive ODX remained relatively unchanged during the study period (− 3.53% relative change from 2010 to 2016 (p = 0.37)). However, in patients who received ODX, chemotherapy use decreased from 27.3% in 2010 to 18.3% in 2016, a relative change of − 33.0% (p = 0.02) (Fig. 1a). In unadjusted analyses, the significant factors associated with chemotherapy receipt following ODX testing were year of diagnosis, patient age, payer, tumor grade, LN status, tumor size, clinical stage, physician’s average patient age, and ODX RS stratification (Table S1). In the multivariable model, year of diagnosis, patient age, tumor grade, LN status, tumor size, clinical stage, physician clinical experience, physician gender, and ODX RS stratification were significantly associated with patient receipt of chemotherapy (Table S3).
Receiving chemotherapy by ODX risk classification
We then stratified the ODX patients by their RS (low, intermediate, high) and developed a multivariable model for each stratum. Low RS patients comprised 60.6% of the ODX population (n = 917) and 6.4% of these patients received chemotherapy. Chemotherapy use decreased from 11.7% in 2010 to 3.7% in 2016 for a relative change of − 68.4% (p = 0.02) (Fig. 1b). Low risk patients were less likely to receive chemotherapy if they were older (60–69 years vs. < 50 years: OR = 0.17 (95% CI = 0.06–0.49), p < 0.01; > 69 years vs. < 50 years: OR = 0.08 (95% CI = 0.02–0.45), p < 0.01) and were more likely to receive chemotherapy for higher grade (grade III/IV vs. grade I: OR = 7.80 (95% CI = 2.62–23.27), p < 0.01), positive compared to negative LN status (OR = 5.84 (95% CI = 2.61–13.05), p < 0.01), higher clinical stage (Stage 2 vs. Stage 1: OR = 2.96 (95% CI = 1.10–7.98) p = 0.03; Stage 3/4 vs. Stage 1: OR = 6.22 (95% CI = 1.18–32.74), p = 0.03) and larger tumors (> 40 mm vs. 0.1-19 mm: OR = 8.16 (95% CI = 2.37–28.06), p < 0.01). In addition, chemotherapy receipt was less likely among patients treated by male (vs. female) medical oncologists (OR = 0.39 (95% = 0.17–0.88), p = 0.02) (Table 5).
Intermediate RS patients comprised 31.0% of the ODX population (n = 469), and 35.6% of the intermediate RS patients received chemotherapy. Chemotherapy use in this group decreased from 41.8 to 30.4%, a relative change of − 27.3% (p = 0.37) (Fig. 1b). In multivariable models, chemotherapy was less likely in older patients compared to those less than 50 years (60–69 years: OR = 0.29 (95% CI = 0.14–0.59), p < 0.01; > 69 years: OR 0.10 (95% CI = 0.03–0.33), p < 0.01). Chemotherapy was more likely in those with higher tumor grade compared to grade I (Grade II: OR = 2.00 (95% CI = 1.06–3.80), p = 0.03; Grade III/IV: OR = 2.37 (95% CI = 1.10–5.11), p = 0.02), and in those with higher clinical stage (Stage 2 vs. Stage 1: OR = 2.59 (95% CI = 1.04–6.47), p = 0.04) and higher ODX RS (OR = 1.33 (95% CI = 1.22–1.44), p < 0.01) (Table 5).
High RS patients comprised 8.3% of the ODX population (n = 126) and 87.3% of these patients received chemotherapy. Chemotherapy use in the high RS group decreased from 85.7 to 76.9% between 2010 and 2016 (p = 0.88) (Fig. 1b). Of all the high RS patients, 61.9% had grade 3/4 tumors, 81.0% were LN negative, and 63.5% had Stage 1 BC. The high RS classification model failed to converge.
Chemotherapy refusal
A total of 375 patients were reported to have refused a recommended course of adjuvant chemotherapy, 109 of these having received ODX. Of those tested with ODX who later refused recommended chemotherapy, the majority were in intermediate RS range (56.0%), were stage 1 (57.8%), LN negative (66.1%), and had tumors that were grade II (60.6%). In the multivariable model, older patients were more likely to refuse chemotherapy compared to patients less than 50 years (> 69 years: OR = 5.62 (95% CI = 1.72–18.39), p < 0.01). Patients were less likely to refuse recommended adjuvant chemotherapy following ODX testing if they had intermediate or high ODX RS stratification, when compared with low RS (Intermediate: OR 0.30 (95% CI = 0.15–0.60), p < 0.01; High: OR 0.04 (95% CI = 0.01–0.13), p < 0.01). In addition, patients being seen by higher volume oncologists were more likely to refuse chemotherapy (OR 1.02 (95% CI = 1.01–1.04), p = 0.04) (Table S4).
Between-physician and between-hospital variation
Hierarchical modeling for each outcome using hospital and physician as the random effect allowed us to determine the proportion of total variance in clinical decisions that is due to variation between physicians and hospitals. For each model, we calculated the ICC in order to measure the correlation of clinical decisions within physicians or hospitals (Table 6). Overall, between-physician variation accounted for a greater proportion of variance than between-hospital variation. Clustering within treating physicians and hospitals was most pronounced for patients receiving a low ODX RS score: clustering within physicians and within hospitals accounted for 33 and 14% of the total variance in chemotherapy use, respectively. For all patients tested with ODX, clustering within physicians and within hospitals accounted for 18 and 4% of variation in receiving chemotherapy, respectively.
Discussion
Increasing use of ODX is expected to spare low risk patients the short- and long-term adverse effects of adjuvant chemotherapy, while still treating the patients who are most likely to benefit [41]. Previous studies using the National Cancer Data Base report utilization of ODX of 45.7 to 54.0% among eligible patients, which is similar to our finding of 43.5%; however, these rates suggest a national underutilization of ODX [27, 42]. Between 2010 and 2016, ODX use increased among patients with BC in New Hampshire, and low and intermediate risk patients were more often spared chemotherapy while higher risk patients continued to receive chemotherapy at higher rates. These findings suggest that physicians were following ODX recommendations as they became available and sparing chemotherapy in patients who were unlikely to receive any benefit.
Previously identified factors associated with utilization of ODX fall under patient, physician, and organizational level factors, among which our study attempted to differentiate [43]. Our final models indicate that patients with earlier stage, LN negative BC were more likely to be prescribed the test. Patient-level factors for which we did not account but which literature suggests play a role in shared decision-making include education, decision-making style, and attitude towards genetic testing and chemotherapy [23, 44]. Cost is unlikely to have been a major barrier during our study period, as ODX testing has been covered by CMS and most private payers for eligible patients since 2006–2008 [27, 45]. In our study, we did not find physician gender or clinical experience to be associated with use of ODX. Previous work identified physician awareness and familiarity with genomic testing as a barrier to uptake [24]. This is reflected by oncologists reporting a desire to receive additional education regarding genomic tests [46]. Physicians also cite ODX marketing, medical/insurance guidelines, and use among peers as factors contributing to utilization of ODX in their practice [43].
We found that patients who received ODX were more likely to be recommended for chemotherapy if they were younger and had later stage, LN positive BC, and higher ODX RS, consistent with previous work [47]. We observed that the association between absolute RS and odds of chemotherapy treatment to be strongest among intermediate risk patients. Other interesting patterns reflecting the influence of physician characteristics on chemotherapy use following ODX stand out. Patients tested with ODX were significantly more likely to be recommended chemotherapy when treated by physicians with 20 or more years of clinical experience. This may represent aspects of the doctor-patient relationship as well as acceptance of RS score guidelines and engrained practice patterns, as these physicians would have been in practice when guidelines recommending chemotherapy for all patients were established [3, 4]. We observed that female physicians were more likely to recommend and prescribe chemotherapy for all ODX patients, including low risk patients. Additional work to understand the differences in preferences of oncologists accounting for gender and clinical experience may be warranted to reduce variation in treatment decisions following ODX test results, especially given the potential concern of overtreatment among low risk patients.
Our hierarchical models demonstrate the significant heterogeneity in chemotherapy treatment decisions following ODX testing among hospitals and physicians. In this respect, variation between hospitals seemed to be less pronounced than variation between physicians. These results raise questions regarding the extent to which unmeasured physician characteristics impact their interpretation of ODX results and subsequent treatment decisions. The variation identified by the physician ICCs may represent differences in physician training, personal experience and familiarity with genetic tests, and the perceived value of the test, all of which have been reported previously [24, 48].
Our study has several limitations. New Hampshire has a predominantly white and rural population, so our findings may not be generalizable to other states or regions with different patient and provider sociodemographic characteristics. We did not have access to detailed medical records and thus could not analyze outcomes, such as disease-free survival following ODX testing or by treatment modality. Patients missing data on medical oncologists was a limitation, which could also be better addressed in a study that links the registry data to electronic health records. Coder reliability and misclassification are a known issue when analyzing registry data as evidenced by the recent reliability study conducted by the Surveillance, Epidemiology, and End Results (SEER) Program [49]. We lacked data on whether the physician specializes in breast cancer care, which could influence their use of ODX. Finally, due to the observational nature of our study, the associations we identified cannot be interpreted as causal.
Conclusions
In conclusion, these findings indicate potential opportunities to implement interventions and target physicians regarding ODX and adjuvant chemotherapy use in order to reduce variation in patient care. This is especially important, and challenging, as ODX recommendations continue to evolve in light of new findings, such as those from the TAILORx trial [17]. Moreover, the utility of ODX has now extended to a stage modifier according to the American Joint Committee on Cancer staging manual [50]. Future work evaluating guideline-concordant changes in ODX testing and adjuvant chemotherapy prescribing patterns following new guidelines will shed light on physician awareness and adaptability regarding implementation of genomic tests in cancer care. Additional physician training in the availability of genomic tests, interpreting genetic tests, and methods to convey the benefits and results of the tests may be beneficial to increase utilization [23, 48].
Availability of data and materials
The data that support the findings of this study are available from the New Hampshire Department of Health and Human Resources, but restrictions apply to the availability of the data, which were used with permission for the current study, and so are not publicly available. Data are, however, available from the authors upon reasonable request and with permission of the New Hampshire Department of Health and Human Resources.
Abbreviations
- ODX:
-
Oncotype DX
- BC:
-
Breast cancer
- LN:
-
Lymph node
- HR:
-
Hormone receptor
- RS:
-
Recurrence score
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- ICC:
-
Intraclass clustering coefficient
- NHSCR:
-
New Hampshire State Cancer Registry
- CMS:
-
Center for Medicare and Medicaid Services
- NPI:
-
National Provider Identifier
References
Siegel R, Miller K, Jemal A. Cancer statistics, 2017. CA Cancer J Clin. 2017;67(1):7–30. https://doi.org/10.3322/caac.21387.
Howlader N, Altekruse SF, Li CI, Chen VW, Clarke CA, Ries LAG, Cronin KA. US incidence of breast cancer subtypes defined by joint hormone receptor and HER2 status. J Natl Cancer Inst. 2014;106(5). https://doi.org/10.1093/jnci/dju055.
Mansour EG, Gray R, Shatila AH, Osborne C, Tormey DC, Gilchrist KW, et al. Efficacy of adjuvant chemotherapy in high-risk node-negative breast cancer. N Engl J Med. 1989;320(8):485–90.
Mansour EG, Gray R, Shatila AH, Tormey DC, Cooper MR, Osborne CK, Falkson G. Survival advantage of adjuvant chemotherapy in high-risk node-negative breast cancer: ten-year analysis - an intergroup study. J Clin Oncol. 1998;16(11):3486–92. https://doi.org/10.1200/JCO.1998.16.11.3486.
Fisher B, Dignam J, Wolmark N, Decillis A, Wickerham DL, Bryant J, et al. Tamoxifen and chemotherapy for lymph node-negative, estrogen receptor-positive breast Cancer. J Natl Cancer Inst. 1997;89(22):1673–82 Retrieved from https://academic.oup.com/jnci/article-abstract/89/22/1673/2526493.
Abrams J. Adjuvant therapy for breast cancer--results from the USA consensus conference. Breast Cancer. 2001;8(4):298–304.
Munoz D, Near AM, Van Ravesteyn NT, Lee SJ, Schechter CB, Alagoz O, et al. Effects of screening and systemic adjuvant therapy on ER-specific US breast cancer mortality. J Natl Cancer Inst. 2014;106(11). https://doi.org/10.1093/jnci/dju289.
Early Breast Cancer Trialists’ Collaborative Group (EBCTCG), Abe O, Abe R, Enomoto K, Kikuchi K, Koyama H, et al. Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005;365(9472):1687–717. https://doi.org/10.1016/S0140-6736(05)66544-0.
Early Breast Cancer Trialists’ Collaborative Group (EBCTCG), Abe O, Abe R, Enomoto K, Kikuchi K, Koyama H, et al. Relevance of breast cancer hormone receptors and other factors to the effi cacy of adjuvant tamoxifen: patient-level meta-analysis of randomised trials. Lancet. 2011;378:771–84. https://doi.org/10.1016/S0140.
Fan C, Oh DS, Wessels L, Weigelt B, Nuyten DSA, Nobel AB, et al. Concordance among gene-expression-based predictors for breast Cancer a bs tr ac t. N Engl J Med. 2006;355(6):560–9 Retrieved from www.nejm.org.
Sparano JA, Paik S. Development of the 21-gene assay and its application in clinical practice and clinical trials. J Clin Oncol. 2008. https://doi.org/10.1200/JCO.2007.15.1068.
Cardoso F, van’t Veer LJ, Bogaerts J, Slaets L, Viale G, Delaloge S, et al. 70-gene signature as an aid to treatment decisions in early-stage breast Cancer. N Engl J Med. 2016;375(8):717–29. https://doi.org/10.1056/nejmoa1602253.
Paik S, Shak S, Kim C, Baker J, Cronin M, Baehner FL, et al. A multigene assay to predict recurrence of Tamoxifen-treated, node-negative breast Cancer. N Engl J Med. 2004;351(27):2817–43 Retrieved from www.nejm.org.
Harris L, Fritsche H, Mennel R, Norton L, Ravdin P, Taube S, et al. American society of clinical oncology 2007 update of recommendations for the use of tumor markers in breast cancer. J Clin Oncol. 2007;25(33):5287–312. https://doi.org/10.1200/JCO.2007.14.2364.
National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: breast cancer, vol. 1; 2007. p. 2007. Retrieved June 12, 2019, from http://www.nccn.org/professionals/physician_gls/f_guidelines.asp#breast.
Paik S, Tang G, Shak S, Kim C, Baker J, Kim W, et al. Gene expression and benefit of chemotherapy in women with node-negative, estrogen receptor-positive breast cancer. J Clin Oncol. 2006;24(23):3726–34. https://doi.org/10.1200/JCO.2005.04.7985.
Sparano JA, Gray RJ, Makower DF, Pritchard KI, Albain KS, Hayes DF, et al. Adjuvant chemotherapy guided by a 21-gene expression assay in breast Cancer. N Engl J Med. 2018;379(2):111–21. https://doi.org/10.1056/NEJMoa1804710.
Albain KS, Barlow WE, Shak S, Hortobagyi GN, Livingston RB, Yeh IT, et al. Prognostic and predictive value of the 21-gene recurrence score assay in postmenopausal women with node-positive, oestrogen-receptor-positive breast cancer on chemotherapy: a retrospective analysis of a randomised trial. Lancet Oncol. 2010;11(1):55–65. https://doi.org/10.1016/S1470-2045(09)70314-6.
Dowsett M, Cuzick J, Wale C, Forbes J, Mallon EA, Salter J, et al. Prediction of risk of distant recurrence using the 21-gene recurrence score in node-negative and node-positive postmenopausal patients with breast cancer treated with anastrozole or tamoxifen: a TransATAC study. J Clin Oncol. 2010;28(11):1829–34. https://doi.org/10.1200/JCO.2009.24.4798.
Roberts MC, Miller DP, Shak S, Petkov VI. Breast cancer-specific survival in patients with lymph node-positive hormone receptor-positive invasive breast cancer and Oncotype DX recurrence score results in the SEER database. Breast Cancer Res Treat. 2017;163(2):303–10. https://doi.org/10.1007/s10549-017-4162-3.
Rath MG, Uhlmann L, Fiedler M, Heil J, Golatta M, Dinkic C, et al. Oncotype DX® in breast cancer patients: clinical experience, outcome and follow-up—a case–control study. Arch Gynecol Obstet. 2018;297(2):443–7. https://doi.org/10.1007/s00404-017-4618-z.
Carlson JJ, Roth JA. The impact of the Oncotype dx breast cancer assay in clinical practice: a systematic review and meta-analysis. Breast Cancer Res Treat. 2013. https://doi.org/10.1007/s10549-013-2666-z.
DeFrank JT, Salz T, Reeder-Hayes K, Brewer NT. Who gets genomic testing for breast cancer recurrence risk? Public Health Genomics. 2013;16(5):215–22. https://doi.org/10.1159/000353518.
Stanek EJ, Sanders CL, Taber KAJ, Khalid M, Patel A, Verbrugge RR, et al. Adoption of pharmacogenomic testing by US physicians: results of a nationwide survey. Clin Pharmacol Ther. 2012;91(3):450–8. https://doi.org/10.1038/clpt.2011.306.
Collin LJ, Yan M, Jiang R, Ward KC, Crawford B, Torres MA, et al. Oncotype DX recurrence score implications for disparities in chemotherapy and breast cancer mortality in Georgia. npj Breast Cancer. 2019;5(1). https://doi.org/10.1038/s41523-019-0129-3.
Dinan MA, Mi X, Reed SD, Lyman GH, Curtis LH. Association between use of the 21-gene recurrence score assay and receipt of chemotherapy among medicare beneficiaries with early-stage breast cancer, 2005-2009. JAMA Oncol. 2015;1(8):1098–109. https://doi.org/10.1001/jamaoncol.2015.2722.
Press DJ, Ibraheem A, Dolan ME, Goss KH, Conzen S, Huo D. Racial disparities in omission of oncotype DX but no racial disparities in chemotherapy receipt following completed oncotype DX test results. Breast Cancer Res Treat. 2018;168(1):207–20. https://doi.org/10.1007/s10549-017-4587-8.
Roberts MC, Weinberger M, Dusetzina SB, Dinan MA, Reeder-Hayes KE, Troester MA, et al. Racial variation in adjuvant chemotherapy initiation among breast cancer patients receiving oncotype DX testing. Breast Cancer Res Treat. 2015;153(1):191–200. https://doi.org/10.1007/s10549-015-3518-9.
McVeigh TP, Kerin MJ. Clinical use of the oncotype DX genomic test to guide treatment decisions for patients with invasive breast cancer. Breast Cancer. Dove Medical Press Ltd. 2017. https://doi.org/10.2147/BCTT.S109847.
Bombard Y, Rozmovits L, Trudeau M, Leighl NB, Deal K, Marshall DA. The value of personalizing medicine: medical oncologists’ views on gene expression profiling in breast Cancer treatment. Oncologist. 2015;20(4):351–6. https://doi.org/10.1634/theoncologist.2014-0268.
Leggett LE, Lorenzetti DL, Noseworthy T, Tiwana S, MacKean G, Clement F. Experiences and attitudes toward risk of recurrence testing in women with breast cancer: a systematic review. Breast Cancer Res Treat. 2014;144(3):457–65. https://doi.org/10.1007/s10549-014-2900-3.
Weldon CB, Trosman JR, Gradishar WJ, Benson AB, Schink JC. Barriers to the use of personalized medicine in breast Cancer. J Oncol Pract. 2012;8(4):e24–31. https://doi.org/10.1200/jop.2011.000448.
Rees JR, Zens MS, Gui J, Celaya MO, Riddle BL, Karagas MR. Non melanoma skin cancer and subsequent cancer risk. PLoS One. 2014;9(6). https://doi.org/10.1371/journal.pone.0099674.
North American Association of Central Cancer Registries. (n.d.). Certified Registries. Retrieved October 18, 2019, from http://www.naaccr.org/certified-registries/.
The National Bureau of Economic Research. (2019). NPI Data -- CMS’ National Plan and Provider Enumeration System (NPPES) Files in SAS, Stata, and CSV format. Retrieved January 1, 2019, from https://www.nber.org/data/npi.html.
Centers for Medicare and Medicaid Services. (2019). Physician Compare datasets. Retrieved May 10, 2019, from https://data.medicare.gov/data/physician-compare.
Shahinian VB, Kuo YF, Freeman JL, Goodwin JS. Determinants of androgen deprivation therapy use for prostate cancer: role of the urologist. J Natl Cancer Inst. 2006;98(12):839–45. https://doi.org/10.1093/jnci/djj230.
Snijders TAB, Bosker RJ. Multilevel analysis: an introduction to basic and advanced multilevel modeling. 2nd ed. London: SAGE Publications; 2003. https://doi.org/10.1080/10705511.2013.797841.
Lin HY, Bedrosian I, Babiera GV, Shaitelman SF, Kuerer HM, Woodward WA, et al. Using the National Cancer Data Base for quality evaluation to assess adherence to treatment guidelines for nonmetastatic inflammatory breast cancer. Cancer. 2017;123(14):2618–25. https://doi.org/10.1002/cncr.30660.
R development core team. R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2019. Retrieved from https://www.r-project.org/.
Tao JJ, Visvanathan K, Wolff AC. Long term side effects of adjuvant chemotherapy in patients with early breast cancer. Breast. 2015;24(2):S149–53. https://doi.org/10.1016/j.breast.2015.07.035.
Jasem J, Amini A, Rabinovitch R, Borges VF, Elias A, Fisher CM. 21-Gene recurrence score assay as a predictor of adjuvant chemotherapy administration for early-stage breast Cancer : an analysis of use, therapeutic implications, and disparity profile. J Clin Oncol. 2016;34(17):1995–2004. https://doi.org/10.1200/JCO.2015.65.0887.
Roberts MC, Bryson A, Weinberger M, Dusetzina SB, Dinan MA, Reeder-Hayes K, Wheeler SB. Oncologists’ barriers and facilitators for Oncotype DX use: qualitative study. Int J Technol Assess Health Care. 2016;32(5):355–61. https://doi.org/10.1017/S026646231600060X.
Roberts MC, Bryson A, Weinberger M, Dusetzina SB, Dinan MA, Reeder-Hayes KE, Wheeler SB. Patient-centered communication for discussing Oncotype DX testing. Cancer Investig. 2016;34(5):205–12. https://doi.org/10.3109/07357907.2016.1172637.
Trosman JR, Van Bebber SL, Phillips KA. Coverage policy development for personalized medicine: private payer perspectives on developing policy for the 21-gene assay. J Oncol Pract. 2010;6(5):238–42. https://doi.org/10.1200/jop.000075.
Dressler LG, Deal AM, Patel J, Markey J, Van Riper M, McLeod HL. Cancer pharmacogenomics, adoption by oncologists and patient benefit. Personalized Med. 2014;11(2):143–53. https://doi.org/10.1186/gm280.
Su KW, Hall J, Soulos PR, Abu-Khalaf MM, Evans SB, Mougalian SS, et al. Association of 21-gene recurrence score assay and adjuvant chemotherapy use in the medicare population, 2008–2011. Journal of Geriatric Oncology. 2016;7(1):15–23. https://doi.org/10.1016/j.jgo.2015.11.002.
Spellman E, Sulayman N, Eggly S, Peshkin BN, Schwartz MD, Neill SCO, Comprehensive L. Conveying genomic recurrence risk estimates to patients with early stage breast cancer : oncologist perspectives. Psychooncology. 2013;22(9):2110–6. https://doi.org/10.1002/pon.3264.
Ruhl, J., Groves, C., Schussler, N., & Handley, B. (2020). 202019 EOD, Summary Stage, and SSDI Reliability Study 2019 EOD, Summary Stage, and SSDI Reliability Study Surveillance, Epidemiology, and End Results ( SEER ) Program National Cancer Institute January 2020. Retrieved February 7, 2020, from https://seer.cancer.gov/qi/tools/results/2019/FinalReport-2019ReliabilityStudy.pdf.
American College of Surgeons. (2014). AJCC 8th 2017. AJCC Cancer Staging Manual. Retrieved February 10, 2019, from https://cancerstaging.org/references-tools/deskreferences/Documents/AJCCBreast CancerStagingSystem.pdf.
Acknowledgements
Not applicable.
Funding
This research is supported through an American Cancer Society Research Grant #IRG-16-191-33 awarded through the Norris Cotton Cancer Center, and NIH NIGMS P20GM104416. The New Hampshire State Cancer Registry is funded in part by the Centers for Disease Control and Prevention’s National Program of Cancer Registries, cooperative agreement 5 NU58DP006298–03-00 awarded to the New Hampshire Department of Health and Human Services, Division of Public Health Services, Bureau of Public Health Statistics and Informatics, Office of Health Statistics and Data Management. The paper’s contents are solely the responsibility of the authors and do not necessarily represent the official views of the Centers for Disease Control and Prevention or New Hampshire Department of Health and Human Services.
Author information
Authors and Affiliations
Contributions
TS, EM, and JR contributed to study design and conceptualization. Funding acquisition and supervision was performed by EM. JR and MC assisted with data acquisition and variable curation. Data analysis was performed by TS. TS, JR, RZ, AS, TO, and EM contributed to interpretation of data and results. The first draft of the manuscript was written by TS and all authors made significant contributions to subsequent versions of the manuscript. All authors read and approved the final manuscript and agree to be accountable for their own contributions.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of Dartmouth College (STUDY00031403) and the Institutional Review Board of Massachusetts Department of Public Health. The use of the data was approved by the State of New Hampshire and State of Massachusetts Departments of Health and Human Services. Below-threshold values have been censored. Analyses, conclusions, interpretations, and recommendations drawn from this research are solely those of the authors and not necessarily those of the New Hampshire Department of Health and Human Services.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Schwedhelm, T.M., Rees, J.R., Onega, T. et al. Patient and physician factors associated with Oncotype DX and adjuvant chemotherapy utilization for breast cancer patients in New Hampshire, 2010–2016. BMC Cancer 20, 847 (2020). https://doi.org/10.1186/s12885-020-07355-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-020-07355-6