Abstract
Background
Papua New Guinea (PNG) recorded 22 neonatal deaths out of every 1,000 livebirths in 2019. Some of these deaths are related to complications that arise shortly after childbirth; hence, postnatal care (PNC) utilisation could serve as a surviving strategy for neonates as recommended by the World Health Organisation. National level study on determinants of PNC uptake in PNG is limited. Utilising the Bronfenbrenner’s Ecological Model of Human Development, the study aimed at assessing determinants of PNC utilisation for babies by their mothers aged 15–49 in PNG.
Methods
The study used data from the women’s file of the 2016–18 PNG Demographic and Health Survey (2016–18 PNGDHS) and a sample of 4,908 women aged 15–49 who had complete information on the variables of interest to the study. Nineteen (19) explanatory variables were selected for the study whereas PNC for babies within first two months after being discharged after birth was the main outcome variable. At 95% confidence interval (95% CI), six multilevel logistic models were built. The Akaike Information Criterion (AIC) was used to assess models’ fit. All analyses were carried out using STATA version 14.0.
Results
Generally, 31% of the women utilised PNC for their babies. Women with primary education [aOR = 1.42, CI = 1.13–1.78], those belonging to the middle wealth quintile [aOR = 1.42, CI = 1.08–1.87], working class [aOR = 1.28, CI = 1.10–1.49], women who had the four or more ANC visits [aOR = 1.23, CI = 1.05–1.43], those with twins [aOR = 1.83, CI = 1.01–3.29], women who belonged to community of medium literate class [aOR = 1.75, CI = 1.34–2.27] and those of moderate socioeconomic status [aOR = 1.60, CI = 1.16–2.21] had higher odds of seeking PNC for their babies. The odds to seek PNC services for babies reduced among the cohabiting women [aOR = 0.79, CI = 0.64–0.96], those at parity four or more [aOR = 0.77, CI = 0.63–0.93], women who gave birth to small babies [aOR = 0.80, CI = 0.67–0.98] and residents in the Highlands region [aOR = 0.47, CI = 0.36–0.62].
Conclusions
Maternal education, wealth quintile, occupation, partner’s education, ANC visits, marital status, parity, child size at birth, twin status, community literacy and socioeconomic status as well as region of residence were associated with PNC uptake for babies in PNG. Variation in PNC uptake for babies existed from one community/cluster to the other. There is the need to strengthen public health education to increase awareness about the benefits of seeking PNC services for babies among women in PNG. Such programs should consider maternal and community/cluster characteristics in their design.
Similar content being viewed by others
Background
Globally, approximately 6,700 new-borns died every day in 2019 despite reduction in global neonatal deaths from 5.0 million in 1990 to 2.4 million in 2019. Neonatal deaths account for a larger share of under-five deaths due to a faster global decline in mortality among children aged 1–59 months compared to children below one month of life. In particular, in 2019, 47% of all under-five deaths occurred in the neonatal period, and this exceeds what was recorded in 1990 (i.e. 40%). Oceania has experienced remarkable decline of neonatal deaths from 15 deaths per 1,000 livebirths in 1990 to 10 deaths per 1,000 livebirths in 2019. A clear synthesis of Oceania’s neonatal deaths shows that Papua New Guinea is the highest contributor to the sub-region’s neonatal deaths. Typically, whilst Australia’s neonatal deaths reduced from 5 deaths per 1,000 livebirths to 2 deaths per 1,000 livebirths from 1990 to 2019, PNG witnessed a decline of neonatal deaths from 34 deaths per 1,000 livebirths to 22 deaths per 1000 livebirths from 1990 to 2019 [1].
Generally, postnatal period, a stage which marks the first six weeks after birth, is a crucial period in the life of the mother and her new-born [2]. PNC period demands urgent and focused attention in order to avoid preventable morbidity and mortality [3]. Thus, the period provides an avenue for healthcare providers to educate women about healthy breast-feeding practices, screen for postpartum depression, monitor the child’s development and entire health condition, treat delivery related complications, encourage nutrition and insecticide bed net use, and refer mothers and new-borns for dedicated care if required [4, 5]. The WHO, therefore, recommends that mothers and neonates seek early PNC within the first 24 h after delivery and not less than three additional PNC visits within 48–72 h, 7–14 days and 6 weeks after childbirth [6]. However, these guidelines were altered and refined to be context-specific.
As a result, the Government of PNG through its various ministries have implemented a number of strategies/interventions to control maternal and child deaths. Such initiatives include midwifery education, improving access to contraception, emergency obstetric training [7] as well as family and community health care (FCC) through Village Health Volunteers (VHV) and aims at improving maternal, new-born and child health [8]. Again, health policies like the National Health Plan 2011–2020, National Health Service Standards, National Health Sector Gender Policy and National Sexual Reproductive Health policy were also set out to improve maternal and child health service delivery in PNG [9]. Regardless of these political commitments, PNC service utilisation is the most deserted health service in PNG [10]. The 2016–18 PNG DHS indicated that 46% of women reported having received a PNC check-up in the first 2 days after birth whereas only 24% had a postnatal check less than 4 h after childbirth. A substantial fraction of them (51%) did not receive postnatal check at all [10].
Studies have established that, financial constraints, mothers’ attitudes, accessibility of health care facility, interpersonal factors such as husband’s support, parity and pregnancy experiences, mother’s age, place of residence and marital status predict maternal health decision making and healthcare utilisation [11,12,13]. Plethora of studies have been done on maternal healthcare utilisation in PNG [14, 15]. Davis and colleagues, for instance, noted that factors supporting fathers’ participation in antenatal consultations included feelings of shared responsibility for the unborn child, concern for the mother’s or baby’s health, the child being a first child, friendly health workers, and male health workers [14]. A recent evidence also indicated that rich women, those working and women with secondary or higher education were more likely to utilise skilled attendants during delivery [15].
This is suggestive that, maternal, child, community-level and other factors are critical and play essential role in maternal healthcare utilisation for their babies. However, national level study on the determinants of PNC uptake for babies in PNG is limited. It is against this background that this study seeks to assess the determinants of PNC utilisation for babies in PNG. The study seeks to answer the question, “what factors determine PNC uptake for babies in PNG?” Findings from this study will be useful in designing maternal, child health interventions and campaigns especially those focusing on PNC utilisation for babies.
This study is guided by Bronfenbrenner’s Ecological Model of Human Development (Fig. 1) [16, 17]. Bronfenbrenner conceptualised ecology as a fit between the individual and his/her environment and as such, the fit between the individual and its environment must be even closer in order for an individual to develop and survive [17, 18]. Bronfenbrenner described the ecological environment as composed of systems at four different levels: microsystem, mesosystem, exosystem and macrosystem. The microsystem contains relations between the individual and the immediate environment surrounding the individual, such as the home, school and workplace whereas the mesosystem constitutes interrelations between major settings accommodating an individual, such as relations between home and school, home and peer groups [17, 19].
The exosystem embraces social structures of society including the world of work, the mass media and public agencies. According to Bronfenbrenner, the social structures do not themselves contain the developing person but impinge upon the immediate settings in which that person is found, and as such influence what is going on in these settings [17, 19]. Finally, the macrosystem consists of the blueprints of a particular society such as laws and regulations as well as unprinted rules and norms [17, 20]. Analysing the composition of these ecological systems as well as interactions between and within these systems and individual factors were regarded as crucial in order to understand and explain a developmental outcome [17]. In the context of this study, it is anticipated that maternal and child-level factors and surrounding community-level factors may affect the uptake of PNC. The theory provided a robust means of assessing the determinants of PNC from a wider scope. Figure 1 is the diagrammatical illustration of the framework for the study.
Methods
Design and extraction of data for the study
The study adopted a cross sectional survey design and made use of women’s file of the 2016–18 Papua New Guinea Demographic and Health Survey (2016–18 PNGDHS). The 2016–18 PNGDHS is the third in the series of the DHS surveys conducted in the country. The survey was implemented by the National Statistical Office (NSO) of PNG. The survey started data gathering from October 2016 to December 2018. All necessary technical and advisory support were provided by the NSO. The ICF International provided technical assistance through the DHS Program, which offers support and technical assistance for the implementation of population and health surveys.
The survey covered areas such as fertility, family planning, breastfeeding practices, nutritional status of children, maternal and child health, childhood immunisation, adult and childhood mortality, women’s empowerment, domestic violence, malaria, awareness and behaviour concerning HIV/AIDS and other sexually transmitted infections (STIs). The survey applied a stratified sampling technique and in all, a total of 18,175 women aged 15–49 were identified for individual interviews. However, 15,198 women were completely interviewed which yielded a response rate of 84%. Details of the sampling procedures, pretesting of instrument, fieldwork, data processing and analysis can be obtained from the 2016–2018 PNGDHS report [10]. Meanwhile, the present study focused on 4,908 women aged 15–49 who had complete information about the variables of the study.
Description of study variables
Outcome variable
During the 2016–18 PNGDHS, all women who had birth(s) in the 5 years preceding the survey were asked if they had postnatal check-up for their children after exiting the health facilities where they delivered. This was posed as “Did any health care provider or a traditional birth attendant check on (NAME)’s health in the two months after you left?” accompanied by “yes”, “no” and “don’t know” responses. Therefore, the outcome variable for this study was ‘‘postnatal care for babies within first two months after exiting the facility where baby was born’’, defined as having received a postnatal check-up for the baby within first two months after exiting place baby was delivered. Those who affirmed “Yes” were recoded as “1” and “No” recoded as “0”. For precision in responses, “don’t know” responses were excluded from the analysis. Also, the outcome variable excludes pre-discharge checks for babies within facility where births took place to aid assess babies that actually received PNC services after discharge.
Explanatory variables
Nineteen (19) explanatory variables were selected for the study [21,22,23]. These are: age, education, wealth quintile, marital status, occupation, parity, health decision making, partners’ education (maternal factors/microsystem), sex of child, twin status and size of child at birth (child factors/microsystem); community literacy level, community socioeconomic status, residence and region (mesosystem); access to mass media, place of delivery and antenatal care (ANC) visits (exosystem); and covered by health insurance (macrosystem). For clarity of presentation, educational status was recoded into “no education”, “primary”, “secondary/higher”. Occupation recoded into “not working” and “working”; and partner’s education was recoded into “no education”, “primary” and secondary/higher”. Considering the current fertility rate of PNG which is 4.2 children per woman [10], total children ever born was recoded into “one birth”, “two births”, “three births” and “four or more births”. Access to mass media was determined from three principal variables: frequency of reading newspaper/magazine; frequency of listening to the radio; and frequency of watching television which were asked during the 2016–18 PNGDHS. Each of these variables had three responses: ‘not at all’, ‘less than once a week’, and ‘at least once a week’. A composite variable was created whereby all ‘less than once a week’ and ‘at least once a week’ responses were categorised as having access to mass media whilst ‘not at all’ was considered as not having access to mass media. Also, ANC visits were recoded into “less than four visits” and “four or more visits”. For child-level factors, twin status was recoded as “single birth” and “twins” and finally, child’s size at birth recoded as “large”, “average” and “small”. Health decision making was recoded as “alone”, “respondent/partner”, and “others”; place of delivery recoded into “home”, “health facility” and “others”; community literacy level (proportion of women who can read and write at all) was recoded into “low”, “medium” and “high”; and community socioeconomic status was recoded into “low”, “moderate” and “high”. Community literacy level was computed from the women who could read and write at all [24]. Also, community socioeconomic status was measured as the percentage of households in the poorest quintile of Papua New Guinea’s household wealth index [25]. Missing variables were low (3.4%) and were omitted.
Statistical analysis
The present study assessed determinants of PNC uptake for babies in PNG. Based on the focus of the study, the following steps were involved in analysing the data. The weighting factor inherent in the dataset (v005/100000) and the “svy command” were applied to cater for over and under sampling biases and to account for the complex survey design and generalizability of the findings respectively. Next, computation of women who received PNC for their babies after two months of exiting place baby was born was done (data not shown) and further analysed providers of PNC. Thereafter, a univariate computation of independent variables was done to describe the sample whereas a bivariate analysis was done for the independent variables across PNC utilisation with their chi square test of independence reported. The chi square test of independence helped to gauge independent variables which were not associated with the outcome variable, hence, excluding such variables from the inferential analyses. Also, the “VIF” command was applied to assess collinearity among the explanatory variables and the results indicated no evidence of multicollinearity existing between the explanatory variables (Maximum VIF = 2.55, Minimum VIF = 1.02, Mean VIF = 1.46) (Appendix 1).
Subsequently, at 95% confidence intervals (95% CIs), six (6) multilevel logistic models were built. The first was a null model (Model 0) to account for variability in PNC which can be attributed to the clustering of the primary sampling units (PSUs) without the effect of micro, meso, exo and macro-system. Further, Model I and Model II considered micro and mesosystem-level factors respectively. Model III and IV were fitted to cater for exosystem-level factors and macro system-level factors. Finally, a complete model containing all the factors (Model 0, I, II, III and IV) were constructed (Model V). The results for the fixed effects were presented in adjusted odds ratio (aOR) and any odds less than one was interpreted as reduced likelihood of PNC whilst an odds higher than 1 meant otherwise. Since the models were nested, the Akaike Information Criterion (AIC) was used to measure the model fit [26]. The random effects which are measures of variation of PNC utilisation across communities or clusters, were expressed using Intra-Class Correlation (ICC) and PSUs variance [26, 27]. These were calculated to gauge the variation of PNC utilisation across clusters and the proportion of variance explained by successive models. The entire analyses were done with the aid of STATA version 14.0.
Ethical considerations
The present study dwelt on an already existing data and since the authors were not involved in the data gathering, no ethical clearance was sought. However, the authors sought for access to use the data from Measure DHS and after obtaining permission, the data was downloaded. The dataset is freely available to the public at https://dhsprogram.com/data/dataset/Papua-New-Guinea_Standard-DHS_2017.cfm?flag=1. However, Measure DHS report has documented details of ethical issues considered in gathering the 2016–18 PNGDHS data [10].
Results
Descriptive results for the study
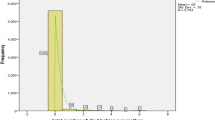
Generally, it was revealed that about two-thirds of women aged 15–49 (3,367; 69%) did not receive postnatal services, with only a small fraction of them (1,541; 31%) availing themselves for postnatal check-ups (data not shown). From Fig. 2, most of the women received postnatal check-ups from a nurse (77%).
Table 1 demonstrates descriptive results for the study. It was evident that 35% of women aged 20–24 sought PNC service for their babies. Forty percent of women with secondary or higher education had PNC for their babies. PNC for babies peaked among the richest (43%), the married (34%) and the working class (37%). Women whose partners completed secondary/higher education (38%) topped PNC utilisation for their babies. It was found that women at parity one (36%) and three (36%), those who had access to mass media (40%) and are covered by health insurance (48%) were the highest to seek PNC services for their babies. Women that had four or more ANC visits utilise PNC often (38%) for their babies. PNC utilisation for babies was same among women that gave birth to male (33%) or female (33%) child, just as among women that gave to single or twin babies (33%).
Utilisation of PNC was highest among women that gave birth to large babies (35%). PNC uptake for babies peaked among urban residents (44%), inhabitants of Southern region (43%), women that made health decision alone (35%) and delivered in a health facility (37%). It was found that utilization for babies by women belonging to higher community literacy (40%) topped PNC. Utilisation of PNC for babies peaked among women belonging to moderate (41%) and high (41%) community socioeconomic class. Finally, with the exception of maternal age [X2 = 4.6448, p = 0.590], sex of the child [X2 = 0.0888, p = 0.766] and health decision making capacity [X2 = 5.5252, p = 0.063], the rest of the theoretically selected covariates had significant association with PNC (Table 1).
Fixed effect results
The Module V is the fixed effect results for study (Table 2). It was evident that, women with Primary education had higher odds to seek PNC for their babies compared with their counterparts without education [aOR = 1.42, CI = 1.13–1.78]. Women in the middle wealth quintile had higher odds to seek PNC for their babies compared with those in the poorest wealth quintile [aOR = 1.42, CI = 1.08–1.87]. It was also revealed that those cohabiting had lower odds to seek PNC for their babies compared with the married [aOR = 0.79, CI = 0.64–0.96]. Comparatively, the results indicated that the working class had higher odds to seek PNC for their babies compared with those who were not working [aOR = 1.28, CI = 1.10–1.49], just as among women whose partners had completed secondary/higher education compared with those whose partners had no education [aOR = 1.32, CI = 1.01–1.72]. Women at parity four or more had lower odds to utilise PNC for their babies compared with those at parity one [aOR = 0.77, CI = 0.63–0.93]. Those that had four or more ANC visits had higher odds to PNC uptake for their babies compared with women who failed to meet the recommended ANC visits [aOR = 1.23, CI = 1.05–1.43]. Women who gave birth to twins had higher odds to seek PNC for their babies compared with those that had single births [aOR = 1.83, CI = 1.01–3.29]. Comparatively, women that gave birth to small babies had lower odds to seek PNC for their babies compared with those that gave birth to large babies [aOR = 0.80, CI = 0.67–0.98]. Residents in the Highlands region lower odds to seek PNC for their babies compared with their counterparts in the Southern region [aOR = 0.47, CI = 0.36–0.62]. Women belonging to community of medium literate class had higher odds to seek PNC for their babies compared with those in the low literate class [aOR = 1.75, CI = 1.34–2.27]. Similarly, women belonging to community of moderate socioeconomic status had higher odds to seek PNC for their babies as compared to those from community of low socioeconomic class [aOR = 1.60, CI = 1.16–2.21].
Random effect results
From Table 2, the random effect results indicated that there was variation in PNC utilisation for babies [σ2 = 1.09, CI = 0.87–1.37]. In particular, almost 25% variance for babies in PNC is attributable to variation in the intra class correlation (ICC) (ICC = 0.25). The ICC values reduced in Model II (ICC = 0.18) and Model V (ICC = 0.18). This implies that the variability to utilise PNC for babies is attributable to the variability in the primary sampling units (PSUs).
There were substantial improvement in the desirability of the models specifically in model V (AIC = 5749.148). Therefore, model V is well specified relative to the other models.
Discussion
The present study aimed at investigating PNC uptake for babies in PNG utilising the Bronfenbrenner’s Ecological Model of Human Development (Fig. 1). The major factors which were associated with PNC uptake were education, wealth quintile, marital status, occupation, partner’s education, parity, twin status, child size at birth (which are found within the microsystem), ANC visits (found within the exosystem) and region, community literacy and socioeconomic status (mesosystem factors). The subsequent section discussed the direction of these key findings.
Consistent with earlier studies [28, 29], the present study noted that women with primary education or belonging to community of medium literate class had higher odds to seek PNC for their babies. This is in line with our framework for the study which indicted that individual level factors also influence their propensity to use health services. Ndugga et al. [21] explained that education enlighten women to be informed and aware of basic health services and health risks which improve their health-seeking behaviour. The authors further argued that higher education empower women to voice their opinions in decisions concerning their own health. Moreover, education exposes mothers to maternal complications and their implications, thereby motivating them to seek timely PNC [30]. This has been corroborated by Yaya et al. [31] who indicated that education affect utilization of all PNC services positively. Congruent with our framework for the study, the study observed that those whose partners had no formal education had lesser odds to seek PNC for their babies. In their meta-analysis, Chaka et al. [32] found that women with husbands who have completed secondary education or above were more likely to use PNC service than those whose husbands had informal or no education in Ethiopia. It is argued that educated husbands are knowledgeable about the benefits of PNC uptake and hence less restrictive towards their wives’ uptake of PNC services [32, 33].
In agreement to previous study [32], the present study found that neonates born by those in the middle wealth quintile or belonging to community of moderate socioeconomic status had higher odds to seek PNC. Maternal wealth status has the potential to influence their PNC utilisation since mothers with enough funds can afford user fees associated with PNC services as highlighted by the framework of the study. Chaka and colleagues [32] found that women with middle household monthly income were more likely to use PNC service than those with lower monthly income in Ethiopia. A plausible reason given in the literature is that wealthier women belong to households that can afford medical and non-medical cost of PNC [32,33,34]. Practically, reproductive healthcare services are provided across aid posts, health sub centres, health centres, district hospitals and provincial public hospitals, in ascending order of size and resources in PNG which are either publicly or privately owned [35, 36]. Despite the availability of these services, there is low uptake of healthcare services among infants and children by their caregivers in PNG, with significant income-related inequalities in use [37]. Also, most caregivers in PNG tend to rely on healthcare services for their infants and children provided by non-hospital public facilities such as health centres and government aid posts, public hospitals and church health facilities. This is because, some care givers especially the poor, are unable to afford user-fees associated with utilization of essential healthcare services particularly, those provided by private-owned facility [37]. Therefore, our observation is not surprising.
In relation to the above, residents in the Highlands region had lower odds to seek PNC for their babies compared with their counterparts in the Southern region. Region of residence, considered in our study as a mesosystem factor (Fig. 1), plausibly influence PNC uptake in the sense that mothers, especially those distant from a health facility, have to walk for longer distance before reaching a facility to assess PNC services for their babies. In particular, PNG, considered as one of the most rural countries in the world, is also characterised by isolated populations with four out of five people living in rugged or coastal terrain without access to roads and public transportation [38]. Bauze et al. [39] added that restricted or poor access to roads and public services in rural areas is a major obstacle to accessing health care in PNG especially among women and children in rural areas [39]. Izudi et al. [40] further argued that long distances limit the willingness and ability of postpartum women to seek PNC due to the physical difficulties of travel and high costs of motorized transport. Probably, women in the Highland areas have to travel over a longer distance in accessing health facility for PNC services.
The present study noted that the cohabiting had lower odds to seek PNC for their babies compared with the married which supports the framework used for the study (Fig. 1). Plausibly, partner or husbands’ support including financial assistance rendered to their spouse could enrich the married and enable them afford user fees associated with PNC utilisation [17, 19]. It is increasingly known that unemployed women are more likely to be economically dependent and consequently unable to access and use maternal health services [41, 42]. Therefore, observing that the working class have higher odds to utilise PNC for their babies in PNG in the present study is not surprising as such women are economically independent and can afford user fees associated with PNC utilisation. In Nigeria, Adigun and Adigun [43] found that women belonging to the working class used high quality PNC services than non-working class. Ndugga et al. [21] also found that unemployed women had lower odds of PNC within 2 days after childbirth compared with women employed in the agricultural sector in Uganda.
Women at parity four or more had lower odds to utilise PNC for their babies compared with those at parity one. Probable reason could be that women of higher parity might depend on their experience acquired from previous PNC visits. On the other hand, it is held that multiple demands including caring for new-borns and older children often prohibit women from seeking PNC particularly where proximity to a health facility is perceived to be a challenge [21]. Any of these explanations could accounts for our observation in the present study. Additionally, those that had four or more ANC visits had higher odds to PNC uptake for their babies compared with women who had less than four visits. The exosystem which embraces social structures of society including health facilities where mothers receive ANC services (Fig. 1), could exposed mothers to useful health information such as the benefits of using PNC services for their babies; hence, influence their PNC uptake for their babies. The results are in line with a study by Fekadu and colleagues [44] who found that mothers who received more ANC components had higher odds of also receiving PNC in Ethiopia. Fekadu and co explained that receiving more components of ANC implies that the mother is more likely to be informed about complications that may occur after delivery which encourages them to seek timely postnatal care [44]. Similar reason could explain our phenomenon.
Women who gave birth to twins had higher odds to seek PNC compared with those that had single births. PNC service utilisation is essential since such services give health staff platform to detect and manage maternal and new-born diseases. As such, women need to avail themselves for such services devoid of type of birth. This confirms our framework used for the study (Fig. 1). Perhaps, perception held about giving birth to twins encourages women to seek PNC for twin births, however, further studies on giving birth to twins and PNC uptake is needed to understand the phenomenon better. Finally, the present study catered for the hierarchical structures embedded in the sampling design of PNG DHS and realised that variation in community characteristics accounted for variation in PNC uptake in PNG. As a result, interventions targeted at increasing PNC uptake for babies in PNG must take into consideration the inequalities that exist among communities which influence PNC utilisation.
Strengths and weaknesses
The main strength of this study is that the data originated from a current nationwide survey that drew respondents using probabilistic methods. In addition to larger sample size, the study employed a rigorous analytical procedure and also accounted for community/cluster influence on PNC utilization which improved the robustness of results. Also, sampling errors were controlled using the weighting factor inherent in the data (v005/100000). However, the results of the present study should be interpreted with caution. Firstly, causality cannot be established since the study depended on data derived from cross-sectional survey design. Secondly, the study is not free from social desirability and recall biases. Additionally, the study design limited the effort to unravel reasons to explain some of the observed findings. Additional limitations could include validity of survey questions. Also, this study relied on the framework which shows that there are ecological factors associated with PNC utilisation; yet, structural changes in the availability, affordability and accessibility of PNC are crucial. Although these factors are not the focus of the paper.
Conclusions
In conclusion, maternal education, wealth quintile, occupation, partners’ education, marital status, parity, child size at birth, twin status (microsystem), community literacy, socioeconomic status, region of residence (mesosystem factors) as well as ANC visits (exosystem), are positively associated with PNC uptake for babies in PNG. Additionally, variation in PNC uptake exist across communities/clusters. These significant findings have policy implications and as such, the following recommendations are needful. Firstly, female education should be a priority in PNG whereas barriers to education faced by females should be addressed by the Government of PNG through its education ministry. Secondly, there is an urgent need for public health education to increase awareness about the benefits of seeking PNC services for babies among women in PNG. Such programs should consider maternal and community characteristics in its program design.
Availability of data and materials
The datasets generated and/or analysed during the current study are available in the Measure DHS repository, http://www.measuredhs.com.
Abbreviations
- ANC:
-
Antenatal Care
- AIC:
-
Akaike Information Criterion
- AOR:
-
Adjusted Odds Ratio
- FCC:
-
Family and Community Health care
- GOPNG:
-
Government of Papua New Guinea
- ICC:
-
Intra-Class Correlation
- ICF:
-
Inner-City Fund
- MMR:
-
Maternal Mortality Ratio
- NSO:
-
National Statistical Office
- PNG:
-
Papua New Guinea
- PNC:
-
Postnatal Care
- PNGDHS:
-
Papua New Guinea Demographic and Health Survey
- PSU:
-
Primary Sampling Units
- STIs:
-
Sexually Transmitted Infections
- DFAT:
-
The Australian Government Department of Foreign Affairs and Trade
- UNFPA:
-
The United Nations Population Fund
- UNICEF:
-
The United Nations Children’s Fund
- VHV:
-
Village Health Volunteers
References
United Nations Inter-agency Group for Child Mortality Estimation (UN IGME). Levels & Trends in Child Mortality: Report 2020, Estimates developed by the United Nations Inter-agency Group for Child Mortality Estimation. New York: United Nations Children’s Fund; 2019. (https://www.unicef.org/reports/levels-and-trends-child-mortality-report-2020).
WHO. WHO technical consultation on postpartum and postnatal care (no.WHO/MPS/10.03). Geneva: WHO; 2010.
Dhakal S, Chapman GN, Simkhad PP, van Teijlingen ER, Stephens J, Raja AE. Utilisation of postnatal care among rural women in Nepal. BMC Pregnancy Childbirth. 2007;7(1):19.
Hordofa MA, Almaw SS, Berhanu MG, Lemiso HB. Postnatal care service utilization and associated factors among women in Dembecha District, Northwest Ethiopia. Science Journal of Public Health. 2015;3(5):686–92.
Sisay MM, Geremew TT, Demlie YW, Alem AT, Beyene DK, Melak MF, et al. Spatial patterns and determinants of postnatal care use in Ethiopia: findings from the 2016 demographic and health survey. BMJ Open. 2019;9(6):e025066.
WHO. WHO recommendations on postnatal care of the mother and newborn. World Health Organization. WHO; 2014. https://apps.who.int/iris/handle/10665/97603
Robbers G, Vogel JP, Mola G, Bolgna J, Homer CS. Maternal and newborn health indicators in Papua New Guinea–2008–2018. Sexual and Reproductive Health Matters. 2019;27(1):52–68.
Byrne A, Morgan A. How the integration of traditional birth attendants with formal health systems can increase skilled birth attendance. Int J Gynecol Obstet. 2011;115(2):127–34.
WHO. WHO country cooperation strategy: Papua New Guinea 2010–2015. Manila: WHO Regional Office for the Western Pacific; 2016. (https://www.aidsdatahub.org/sites/default/files/resource/papua-new-guinea-who-country-cooperation-strategy-2016-2020.pdf).
National Statistical Office (NSO) [Papua New Guinea], ICF. Papua New Guinea Demographic and Health Survey 2016–18. Port Moresby, Papua New Guinea, and Rockville, Maryland, USA: NSO and ICF; 2019. (https://www.dhsprogram.com/pubs/pdf/FR364/FR364.pdf).
Andrew EV, Pell C, Angwin A, Auwun A, Daniels J, Mueller I, et al. Factors affecting attendance at and timing of formal antenatal care: results from a qualitative study in Madang, Papua New Guinea. PloS One. 2014;9(5):e93025.
Kulumbu E. Health Service Delivery in Papua New Guinea and Determinants Influencing Health Outcomes: The Case of Women and Health. 2018. https://doi.org/10.25911/5d7631bfd4875 (http://hdl.handle.net/1885/165911Accessed 02 April 2021).
Maraga S, Namosha E, Gouda H, Vallely L, Rare L, Phuanukoonnon S. Sociodemographic factors associated with maternal health care utilization in Wosera, East Sepik Province, Papua New Guinea. P N G Med J. 2011;54(3–4):154–63 (PMID: 24494512).
Davis J, Vaughan C, Nankinga J, Davidson L, Kigodi H, Alalo E, et al. Expectant fathers’ participation in antenatal care services in Papua New Guinea: a qualitative inquiry. BMC Pregnancy Childbirth. 2018;18(1):1–13.
Seidu AA, Ahinkorah BO, Agbaglo E, Oduro JK, Amoah A, Yaya S. Int Health. 2021;0:1–10. https://doi.org/10.1093/inthealth/ihab007.
Rosa EM, Tudge J. Urie Bronfenbrenner’s theory of human development: Its evolution from ecology to bioecology. J Fam Theory Rev. 2013;5(4):243–58.
Eriksson M, Ghazinour M, Hammarstro¨m A. Different uses of Bronfenbrenner’s ecological theory in public mental health research: what is their value for guiding public mental health policy and practice? Soc Theory Health. 2018;16:414–33. https://doi.org/10.1057/s41285-018-0065-6.
Bronfenbrenner U. Reality and research in the ecology of human development. Proc Am Philos Soc. 1975;119(6):439–69.
Bronfenbrenner U. Toward an experimental ecology of human development. Am Psychol. 1977;32(7):513–31.
Bronfenbrenner U. The social role of the child in ecological perspective. Zeitschrift fu¨r Soziologie. 1978;7(1):4–20.
Ndugga P, Namiyonga NK, Sebuwufu D. Determinants of early postnatal care attendance: analysis of the 2016 Uganda demographic and health survey. BMC Pregnancy Childbirth. 2020;20:163. https://doi.org/10.1186/s12884-020-02866-3.
Ameyaw EK, Kofinti RE, Appiah F. National health insurance subscription and maternal healthcare utilisation across mothers’ wealth status in Ghana. Heal Econ Rev. 2017;7(16):2–15. https://doi.org/10.1186/s13561-017-0152-8.
Appiah F, Salihu T, Fenteng JOD, Darteh AO, Kannor P, Ayerakwah PA, Ameyaw EK. Postnatal care utilisation among women in rural Ghana: analysis of 2014 Ghana demographic and health survey. BMC Pregnancy and Childbirth. 2021;21:2–9. https://doi.org/10.1186/s12884-020-03497-4.
Zegeye B, Olorunsaiye CZ, Ahinkorah BO, Ameyaw EK, Budu E, Seidu AA, Yaya S. Individual/Household and Community-Level Factors Associated with Child Marriage in Mali: Evidence from Demographic and Health Survey. BioMed Research International, 2021, 5529375.
Janevic T, Sarah PW, Leyla I, Elizabeth BH. Individual and community level socioeconomic inequalities in contraceptive use in 10 Newly Independent States: a multilevel cross-sectional analysis. International Journal for Equity in Health. 2012;11(1):1–13.
Ahinkorah BO. Individual and contextual factors associated with mistimed and unwanted pregnancies among adolescent girls and young women in selected high fertility countries in sub-Saharan Africa: A multilevel mixed effects analysis. PLoS ONE. 2020;15(10):e0241050. https://doi.org/10.1371/journal.pone.0241050.
Solanke BL, Oyinlola FF, Oyeleye OJ, Ilesanmi BB. Maternal and community factors associated with unmet contraceptive need among childbearing women in Northern Nigeria. Contraception and Reproductive Medicine. 2019;4(1):11.
Wanyenze RK, Tumwesigye NM, Kindyomunda R, Beyeza-Kashesya J, Atuyambe L, Kansiime A, et al. Uptake of family planning methods and unplanned pregnancies among HIV-infected individuals: a cross-sectional survey among clients at HIV clinics in Uganda. J Int AIDS Soc. 2011;14(1):35.
Mekonnen W, Worku A. Determinants of low family planning use and high unmet need in Butajira District, South Central Ethiopia. Reprod Health. 2011;8(1):37.
Limenih MA, Endale ZM, Dachew BA. Postnatal care service utilization and associated factors among women who gave birth in the last 12 months prior to the study in Debre Markos town, northwestern Ethiopia: a community-based cross-sectional study. International Journal of Reproductive Medicine. 2016;2016:7095352.
Yaya S, Bishwajit G, Shah V. Wealth, education and urban–rural inequality and maternal healthcare service usage in Malawi. BMJ Global Health, 2016; 1(2).
Chaka EE, Abdurahman AA, Nedjat S, Majdzadeh R. Utilization and Determinants of Postnatal Care Services in Ethiopia: A Systematic Review and Meta-Analysis. Ethiop J Health Sci. 2018;29(1):929. https://doi.org/10.4314/ejhs.v29i1.16.
Gabrysch S, Campbell OMR. Still too far to walk: Literature review of the determinants of delivery service use. BMC Pregnancy Childbirth. 2009;9:34.
Say L, Raine R. A systematic review of inequalities in the use of maternal health care in developing countries: examining the scale of the problem and the importance of context. Bull World Health Organ. 2007;85(10):812.
Davy C, Business UoSAIGSo. Primary Health Care: Knowledge Development and Application in Papua New Guinea: University of South Australia; 2009.
Andrew EVW, Pell C, Angwin A, Auwun A, Daniels J, et al. Factors Affecting Attendance at and Timing of Formal Antenatal Care: Results from a Qualitative Study in Madang, Papua New Guinea. PLoS ONE. 2014;9(5):e93025. https://doi.org/10.1371/journal.pone.0093025.
J Jayanthan W Irava C Anuranga RP Rannan-Eliya 2012 The Impact of Out-of-Pocket Expenditures on Families and Barriers to Use of Maternal and Child Health Services in Papua New Guinea: Evidence from the Papua New Guinea Household Survey 1996 and Household Income and Expenditure Survey 2009–2010 - RETA6515 Country Brief Asian Development Bank Manila
World Bank. Transport in Papua New Guinea. Washington DC: World Bank; 2013. (http://web.worldbank.org/wbsite/external/countries/eastasiapacificext/exteapregtoptransport/0,,contentMDK:20768397~menuPK:2069483~pagePK:34004173~piPK:34003707~theSitePK:574066,00.html).
Bauze A, Tran L, Nguyen KH, Firth S, Jimenez-Soto E, Dwyer-Lindgren L, et al. Equity and geography: The case of child mortality in Papua New Guinea. PloS One. 2012;7(5):e37861.
Izudi J, Akwang GD, Amongin D. Early Postnatal Care Use by Postpartum Mothers in Mundri East County, South Sudan. BMC Health Services Research. 2017;17:442. https://doi.org/10.1186/s12913-017-2402-1.
Chakraborty N, Islam MA, Chowdhury RI, Bari W. Utilisation of postnatal care in Bangladesh: evidence from a longitudinal study. Health Soc Care Commun. 2002;10(6):492–502.
Izudi J, Amongin D. Use of early postnatal care among postpartum women in eastern Uganda. Int J Gynecol Obstet. 2015;129(2):161–4.
Adigun AO, Adigun KA. An Analysis of Utilization of Postnatal Care Services Among Mothers in Nigeria. International Journal of Contemporary Research and Review. 2019;10(01):MS 20691-20699. https://doi.org/10.15520/ijcrr.v10i01.651.
GA Fekadu FA Getahun A Seblewongiel SA Kidanie 2018 Facility Delivery andPostnatal Care Services Use among Mothers Who Attended Four or More Antenatal Care Visits in Ethiopia:Further Analysis of the 2016 Demographic and Health Survey. DHS Working Paper No. 137. Rockville, Maryland, USA: ICF;.
Acknowledgements
We thank Measure DHS for making data available and accessible for the study.
Funding
Not applicable
Author information
Authors and Affiliations
Contributions
FA and EKA conceived the study and FA conducted the formal analysis. FA and EKA interpreted the results. FA, JODF, FD, TS, AOD, MT, PAA and EKA drafted the manuscript. The authors proof read and approved the final manuscript for important intellectual content.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The present study utilised an already existing data and since the authors were not involved in the data gathering, no ethical clearance was sought. However, the authors sought for access to use the data from Measure DHS and after obtaining permission, the data was downloaded. The dataset is freely available to the public at https://dhsprogram.com/data/dataset/Papua-New-Guinea_Standard-DHS_2017.cfm?flag=1. Measure DHS anonymised the dataset before making it available to the public. All methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Appiah, F., Fenteng, J.O.D., Dare, F. et al. Understanding the determinants of postnatal care uptake for babies: A mixed effects multilevel modelling of 2016–18 Papua New Guinea Demographic and Health Survey. BMC Pregnancy Childbirth 21, 841 (2021). https://doi.org/10.1186/s12884-021-04318-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-021-04318-y