Abstract
Background
As disease-modifying therapies (DMTs) for Alzheimer's disease (AD) are becoming a reality, there is an urgent need to select cost-effective tools that can accurately identify patients in the earliest stages of the disease. Subjective Cognitive Decline (SCD) is a condition in which individuals complain of cognitive decline with normal performances on neuropsychological evaluation. Many studies demonstrated a higher prevalence of Alzheimer’s pathology in patients diagnosed with SCD as compared to the general population. Consequently, SCD was suggested as an early symptomatic phase of AD. We will describe the study protocol of a prospective cohort study (PREVIEW) that aim to identify features derived from easily accessible, cost-effective and non-invasive assessment to accurately detect SCD patients who will progress to AD dementia.
Methods
We will include patients who self-referred to our memory clinic and are diagnosed with SCD. Participants will undergo: clinical, neurologic and neuropsychological examination, estimation of cognitive reserve and depression, evaluation of personality traits, APOE and BDNF genotyping, electroencephalography and event-related potential recording, lumbar puncture for measurement of Aβ42, t-tau, and p-tau concentration and Aβ42/Aβ40 ratio. Recruited patients will have follow-up neuropsychological examinations every two years. Collected data will be used to train a machine learning algorithm to define the risk of being carriers of AD and progress to dementia in patients with SCD.
Discussion
This is the first study to investigate the application of machine learning to predict AD in patients with SCD. Since all the features we will consider can be derived from non-invasive and easily accessible assessments, our expected results may provide evidence for defining cost-effective and globally scalable tools to estimate the risk of AD and address the needs of patients with memory complaints. In the era of DMTs, this will have crucial implications for the early identification of patients suitable for treatment in the initial stages of AD.
Trial registration number (TRN)
NCT05569083.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Research and clinical practice on Alzheimer's disease (AD) are at a turning point. The AD drug development pipeline is leading to new therapies [1], with aducanumab and lecanemab being the first disease-modifying therapies (DMTs) approved for AD [2, 3]. It is widely accepted that DMTs should be administered in the early stages of the disease to halt the pathological process before neurodegeneration begins [4]. Consequently, international research is now focusing on the prodromal and preclinical phases of AD. Subjective cognitive decline (SCD) refers to a self-experienced persistent decline in cognitive capacity compared to the previously normal state. During this decline, individuals exhibit normal age-, sex-, and education-adjusted performance on standardized cognitive tests [5].
SCD has been associated with neuroradiological features suggestive of AD, amyloid deposition [6, 7], and a higher risk of progression to Mild Cognitive Impairment (MCI) or dementia compared to individuals without SCD [8]. Recognizing these associations, the National Institute of Aging-Alzheimer's Association (NIA-AA) has included SCD as the first manifestation of symptomatic AD stages, preceding MCI [9]. Consequently, individuals with SCD may represent a target population for DMT to preserve cognitive function and psychological well-being [10].
However, SCD encompasses a heterogeneous group with various possible trajectories [11] and numerous potential underlying causes, including normal ageing, personality traits, psychiatric, neurological or medical disorders, substance use disorder, and medications [12]. Therefore, it is crucial to identify features and tools that accurately detect prodromal AD among patients with SCD.
In recent years, the Regional Reference Centre for Alzheimer's Disease and Cognitive Disorders of Careggi Hospital in Florence, Italy, has analysed a large dataset of neuropsychological, personality, and lifestyle data collected over approximately 25 years from patients with SCD. This analysis identified demographic [13, 14], cognitive [15, 16], personality [15], and genetic [15] and genetic [13, 17,18,19,20,21,22,23] features that increase the risk of progression from SCD to MCI or AD.
This paper describes the protocol of the PREVIEW (PRedicting the EVolution of SubjectIvE Cognitive Decline to Alzheimer's Disease With machine learning) study, which will prospectively investigate baseline predictors and biomarkers of Alzheimer's pathology and progression to MCI and dementia in a large cohort of patients with SCD. In this study, we will integrate our previous findings with data from non-invasive techniques, such as electroencephalography (EEG) and event-related potentials (ERP) recording. These techniques reliably measure neural circuits associated with cognitive processes and may provide sensitive metrics for early diagnosis of cognitive impairment [24]. Additionally, we will employ machine learning approaches, an emerging and promising tool that has demonstrated great potential in diagnosing and classifying neurodegenerative diseases and other medical conditions [25,26,27].
Specifically, our aims are as follows:
-
i)
Integrate a multimodal set of data from SCD patients, including clinical data, neuropsychological assessments, personality traits, cognitive reserve, genetic factors, and features from EEG and ERP recordings.
-
ii)
Train and test a machine learning model based on these features to predict biological AD pathology (defined according to CSF biomarkers) and conversion from SCD to MCI and AD dementia through machine learning tools.
-
iii)
Define a management protocol for SCD to be applied in memory clinic settings.
The PREVIEW study was registered on ClinicalTrials.gov (registration number: NCT05569083).
Methods and analysis
Study design and participants
This is a longitudinal observational cohort study. We will include consecutive patients who self-referred to the Centre for AD and Adult Cognitive Disorders of Careggi Hospital in Florence and are classified as SCD based on SCD-I criteria [5].
We will recruit patients who meet the following criteria:
-
I
age between 45 and 90 years;
-
II
complaining of cognitive decline with a duration of ≥ 6 months;
-
III
Mini Mental State Examination (MMSE) score greater than 24, corrected for age and education;
-
IV
normal functioning on the Activities of Daily Living (ADL) and the Instrumental Activities of Daily Living (IADL) scales [28];
- V
Exclusion criteria are history of head injury, current neurological and/or systemic disease, symptoms of psychosis, major depression, or substance use disorder (as defined by the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition [DSM-5] [30]).
The evaluation of exclusion criteria will be conducted through a thorough neurological examination of the patients. The presence of exclusion criteria will be assessed by two independent neurologists. In the event of a disagreement, a third neurologist will be consulted to reach a consensus.
All recruited patients will undergo the following assessments at baseline (T0):
-
I
comprehensive evaluation of familial and clinical history;
-
II
extensive neuropsychological assessment, including estimation of premorbid intelligence, evaluation of depression, personality assessment, and assessment of leisure activities;
-
III
blood collection for measurement of vitamin B12, folic acid, thyroid hormones, as well as APOE and BDNF genotype analysis;
-
IV
EEG and ERP recording.
Patients who provide additional informed consent for lumbar puncture will undergo CSF collection to measure Aβ42, Aβ42/Aβ40 ratio, total tau (t-tau), and phosphorylated tau (p-tau).
Patients will undergo neuropsychological evaluations every two years until progression to AD or other dementias. Based on the results of previous meta-analysis [8], we estimate that a period of six years will be required to reach the desired sample size (see Sect. 2.2). Progression to MCI and AD dementia will be determined based on the criteria established by the NIA-AA [29, 31]. Patients who progress to dementia will be referred to our centre for diagnostic and therapeutic assessments.
A summary of the study design is shown in Fig. 1.
For the purpose of cross-sectional comparison with the SCD group at baseline, two samples consisting of age-matched healthy controls (without cognitive concerns) and MCI patients will undergo EEG and ERP recording.
Sample size calculation
We estimated the sample size needed for this study using the statistical power of a hypothesis test using the Python module statsmodels [32]. We considered the following parameters:
-
Level of significance (α) = 0.05
-
Statistical power (1-β) = 0.8
-
Effect size (Cohen's d) = 0.6
The required number of patients was 45 per group. Therefore, considering that we aim to compare patients who will show a progression to objective cognitive decline and patients who will not, the total estimated sample size should be 90 individuals.
With an expected conservative drop-out rate of 10%, the number of participants to be included was estimated to be 99 patients.
Neuropsychological evaluation, assessment of depression and estimation of premorbid intelligence
Extensive neuropsychological examination includes: global measurements (MMSE) [33], tasks exploring verbal and spatial short-term and long-term memory (Digit and Visuo-spatial Span forward and backward [34], Rey Auditory Verbal Learning Test [35], Short Story Immediate and Delayed Recall [36], Rey-Osterrieth complex figure recall [37]), attention (Trail Making Test A [38], attentional matrices [39], Multiple Features Targets Cancellation [40]), language (Category Fluency Task [41], Phonemic Fluency Task [35] and Italian language battery: Screening for Aphasia NeuroDegeneration [42]), constructional praxis (Copying drawings [35], Rey-Osterrieth complex figure copy [37], Clock test [43]) and executive function (Trail Making Test B [38], Stroop Test [44], Frontal Assessment Battery [45]). The subjective perception of memory impairment will be investigated using the Memory Assessment Clinics-Questionnaire (MAC-Q) [46]. Premorbid intelligence will be estimated using the Short intelligence test (TIB) [47], that has been constructed as the Italian equivalent of the National Adult Reading Test [48]. The presence and severity of depressive symptoms will be evaluated by means of the 22-item Hamilton Depression Rating Scale (HDRS) [49]. Katz Index of Independence in Activities of Daily Living (ADL) [50] scale will be used to assess functional capacities at baseline and at follow-up (Table 1).
Personality traits and leisure activities
We will use the Big Five Factors Questionnaire (BFFQ) [51] to assess personality traits. Participants will be asked to fill out a questionnaire that measures the five factors of: 1) emotional stability, 2) energy, 3) conscientiousness, 4) agreeableness, and 5) openness to culture and experience. The inventory follows a widely accepted five-traits personality model [51, 52]. For the 24 items of each factor, subjects will rate their level of agreement on a five-point scale ranging from strongly agree to strongly disagree. Item scores will be computed for each factor to yield a summary measure of the trait with higher values representing a greater degree of the explored dimension.
At baseline, subjects will be interviewed regarding participation, when they were 30–40 years old, in nine Intellectual Activities, seven Social Activities and seven Physical Activities (modified from Yarnold PR et al. [53]). The frequency of participation will be reported for each activity on a Likert scale ranging from 0 to 5, where 0 refers to never, 1 to occasionally, 2 to monthly, 3 to once a week, 4 to several days per week and 5 to daily.
EEG and ERP recording
Resting-state EEG data will be collected at the Neurophysiological Laboratory of IRCCS Don Gnocchi (Florence, Italy) using the 64-channel Galileo-NT system (E.B. Neuro S.p.A.). The EEG will be recorded continuously from 64 electrodes using an EEG Prewired Headcaps. Electrodes were positioned according to the 10–10 international system (AF7, AF3, Fp1, Fp2, Af4, Af8, F7, F5, F3, F1, F2, F4, F6, F8, FT7, FC5, FC3, FC1,FC2, FC4, FC6, FT8, T3, C5, C3, C1, C2, C4, C6, T4 TP7, CP5, CP3, CP1, CP2, CP4, CP6, TP8, T5, P5, P3, P1, P2, P4, P6, T6, Fpz, PO7, PO3, O1, O2, PO4, PO8, Oz, AFz, Fz, FCz, Cz, CPz, Pz, and POz). The ground electrode will be placed in front of Fz. Horizontal eye movements will be detected by electrooculogram (EOG). Data will be digitized at a sampling rate of 512 Hz and analogue–digital precision will be 16 bits. The recording will be referenced to the common average of all electrodes, excluding Fp1 and Fp2. Re-referencing will be done prior to the EEG artifact detection and analysis. Electrode–skin impedance will be set below 5 kΩs. Subjects will be seated in a reclined chair in a comfortable position. Resting EEG recording begins with a 10-min eyes-closed registration followed by an alternance of 3 min eyes-open and 3 min eyes closed, repeated twice. Only the eyes-closed portions of the signal will be used for subsequent analyses.
ERP acquisition will be performed with the same EEG system used for EEG data acquisition. The participants will be administered an ERP test battery with concurrently recorded EEG consisting of a 3-choice vigilance task (3CVT) and standard image recognition task (SIR).
In order to remove electrophysiological and non-electrophysiological artifacts from the raw signals, we will apply a custom preprocessing pipeline written in MATLAB with the use of the EEGLAB toolbox functions [54]. The pipeline consists of two main steps: the PREP pipeline [55], followed by independent component analysis (ICA) to remove artefactual components [56]. Moreover, to generate the ERP epochs, time windows from -300 ms to + 1000 ms will be created for each EEG recording channel, with the stimulus presentation centred at 0 ms and the average of the trials from each epoch will be calculated.
Blood sample collection and analysis of APOE and BDNF genes
Blood samples will be collected by venipuncture into standard polypropylene EDTA test tubes (Sarstedt, Nümbrecht, Germany) at the Neurology Unit of Careggi University Hospital. They will be centrifuged within two hours at 1300 rcf at room temperature for 10 min, and plasma will be isolated and stored at -80 °C until tested at the Laboratory of Neurogenetics at Careggi University Hospital.
APOE genotypes will be investigated by HRMA. The samples with known APOE genotypes, which had been validated by DNA sequencing, will be used as standard references.
Analysis of BDNF rs6265 polymorphism will be performed using HRMA and the genotypes will be identified through Sanger sequencing (SeqStudio Genetic Analyzer, ThermoFisher).
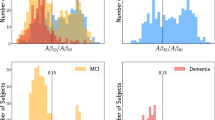
CSF collection and AD biomarker measurement
CSF samples will be collected at 8:00 a.m. by lumbar puncture at the Neurology Unit of Careggi University Hospital. Samples will be immediately centrifuged and stored at -80 °C until performing the analysis at the Laboratory of Neurogenetics of Careggi University Hospital. Aβ42, Aβ40, t-tau, and p-tau will be measured using a chemiluminescent enzyme immunoassay (CLEIA) analyser LUMIPULSE G600 (Fujirebio, Tokyo, Japan). Cut-off values for CSF biomarkers will be determined following Fujirebio guidelines (diagnostic sensitivity and specificity using clinical diagnosis and the follow-up golden standard as of November 19th, 2018).
Data collection and management
Data collection will be carried out anonymously on REDCap, an online-based software for the design of databases. Data will be collected in a pseudo-anonymized way, attributing a record ID to each patient on the electronic database and saving the correspondence between names and identification codes on a separate document.
EEG pre-processing
The EEG preprocessing will be conducted following the methodology outlined in Lassi et al., 2023 [57]. Firstly, the PREP pipeline will be applied, which involves high-pass filtering the signals at 1 Hz, removing line noise using the CleanLine routine, and identifying noisy channels through a combination of methods. Following the interpolation of noisy channels, the data will be re-referenced to the median. Subsequently, Independent Component Analysis (ICA) [58] will be performed on the re-referenced signals to eliminate artifacts while preserving neural components. To classify the components as neural or artefactual, a semi-automated process will be employed, utilizing both the ICLabel [59] toolbox and visual inspection. After completing these two processing steps, a final visual inspection will be conducted to identify and remove any remaining artifacts, if present.
EEG Statistical analysis
Firstly, we will calculate the power spectral density (PSD) of the signal recorded in each channel using the Welch's method. The PSD will be computed on continuous windows of EEG signals, applying Hanning windows with no overlap. The spectrum will be divided into four canonical frequency bands: delta (1–4 Hz), theta (4–8 Hz), alpha (8–13 Hz), and beta (13–30 Hz). The scalp will be divided into six regions of interest (ROIs): frontal right (Fp2, AF4, AF8, F2, F4, F6, F8), frontal left (Fp1, AF3, AF7, F1, F3, F5, F7), central right (FC2, FC4, FC6, FT8, C2, C4, C6, T4, CP2, CP4, CP6), central left (FC1, FC3, FC5, FT7, C1, C3, C5, T3, CP1, CP3, CP5), occipital right (P2, P4, P6, T6, PO8, PO4, O2), and occipital left (P1, P3, P5, T5, PO7, PO3, O1). ROI power will be computed as the average relative power from channels belonging to each ROI.
Next, we will analyse the connectivity between pairs of ROIs using LORETA source-reconstructed signals and extract several network metrics from the weighted undirected adjacency matrices. These metrics will include the average strength of connectivity among pairs of ROIs (mean weight of non-zero connections), the weighted clustering coefficient (C) and the weighted characteristic path length (L) [60]. Finally, we will compute the small-world coefficient [57]:
where L and C are the previously computed weighted clustering coefficient and weighted characteristic path length, whereas Lr is the weighted characteristic path length of an equivalent random network and Cl is the weighted clustering coefficient of an equivalent lattice network.
The final statistical analysis will involve extracting microstate maps [61] for each subject individually. Initially, a set of common microstates will be extracted from all subjects, regardless of conditions, using the modified k-means algorithm [62]. Then, individual microstate maps will be generated, and the template maps will be matched with the previously obtained grand-averages. The EEG signals of each subject will be reconstructed as a sequence of microstates by assigning each topography to the most similar microstate average map. From the reconstructed microstate sequence, various metrics such as duration, transition probability, and complexity of the sequence will be used as features. Spectral features, network metrics, and microstate features will be compared across conditions, providing the foundation for the machine learning analysis.
Regarding the ERP data, both spectral features (like the EEG processing) and voltage-level signals (amplitude, latency, integral of the signal) from different phases of the ERP will be used as input features.
Descriptive statistical analysis
Descriptive statistical analyses will be conducted using IBM SPSS Statistics Software Version 25 (SPSS Inc., Chicago, USA) and the computing environment R4.2.3 (R Foundation for Statistical Computing, Vienna, 2013). The distributions of variables will be assessed using the Shapiro–Wilk test. Patient groups will be characterized using means and standard deviations, medians and interquartile ranges (IQR), frequencies or percentages, and 95% confidence intervals (95% C.I.) for variables with continuous distribution, continuous non-normally distributed variables, and categorical variables, respectively. Depending on the distribution of the data, we will employ ANOVA or non-parametric Kruskal–Wallis tests for between-group comparisons, and Pearson's or Spearman's correlation coefficient to assess correlations between numeric measures of the groups. Chi-square tests will be used to compare categorical data. Effect sizes will be computed using Cohen's d for normally distributed numeric measures, η2 for the Mann–Whitney-U Test, and Cramer's V for categorical data.
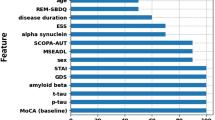
Machine learning classification of patient conditions
Demographic, clinical, cognitive, neurophysiological, and genetic data will be used as candidate input features without any further processing for training a machine learning model. During the training process, a feature selection algorithm will be applied to select the most informative features based on their performance on the validation set.
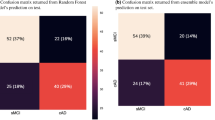
The machine learning problem will initially be treated as a multi-class classification task. The model will classify patients who are SCD at the time of the measurements into one of the following three classes: stable SCD, progressed to MCI, or progressed to AD dementia. For the subgroup of patients undergoing CSF biomarker analysis, a classification will be performed based on the results of the analysis. Specifically, patients will be classified as carriers or non-carriers of AD pathology, according to the NIA-AA framework [9].
For feature selection, we will test the efficacy of several algorithms including the ANOVA F-test statistic, ReliefF, mutual information, and minimum redundancy maximum relevance (MRMR). The number of retained features for each algorithm will be optimized in the validation loop.
Regarding the classifier models, a set of different machine learning models will be tested, including support vector machine (SVM) with linear, quadratic, cubic, and radial basis function kernels; random forest (RF); gradient boosted trees (xgboost); linear and quadratic discriminant analysis (LDA and QDA); and an artificial neural network (ANN). The hyperparameters of each algorithm will be optimized to determine the model with the best performance in the classification task.
In the SVM, the parameters C (misclassification penalty) and gamma (influence of single training points) will be optimized. For the RF, the number of trees (estimators), maximum depth of each tree, and minimum number of data points allowed in a leaf node will be optimized. The same hyperparameters will be tuned for xgboost, along with the learning rate of the algorithm. In LDA and QDA, the type of solver used by the algorithm and the shrinkage term will be adjusted. For the ANN, the number of layers and neurons per layer will be optimized. We have chosen to compare feature selection methods from classical statistics (such as ANOVA F-test) with data-driven methods (ReliefF and MI) that do not assume the distribution of the data. Additionally, the MRMR algorithm will be tested to consider possible redundancies among features.
In the machine learning models, both linear (linear SVM and LDA) and non-linear (polynomial and radial basis function [RBF]-SVM and QDA) algorithms that define separating hyperplanes will be tested, along with tree-based methods like RF and xgboost. The ANN will serve as a non-linear, black-box model to assess the discrimination performance and potential overfitting of more complex models. Furthermore, standard dimensionality reduction techniques will be applied to extract the most salient features. The procedure described above will be repeated to evaluate whether similar results can be achieved with a subset of the features. Once the cross-sectional classification is performed, longitudinal data will be utilized to develop an algorithm capable of predicting the future progression of cognitive impairment.
Out of the entire dataset, 30% of the data will be reserved as a testing set, while the remaining 70% will be used for training and validation of the model. A fivefold cross-validation approach will be employed to train and optimize the hyperparameters of the models. The best performing model, determined by the prediction F1-score and the set of optimized hyperparameters, will be tested on the testing set to obtain an unbiased estimate of the model's performance.
A visual summary of the data collection and analysis process is shown in Fig. 2.
Visual summary of data collection and analysis. A Data collection and feature extraction. Multi-modal data is collected from the recruited patients: clinical-neuropsychological evaluations, genetic and biological data, EEG at rest and during memory and attention tasks (ERP). From the EEG signals, features are extracted by using several analyses, such as connectivity (top left), microstates (top right), spectral and ERP time course analyses. B The extracted features, candidate biomarkers of progression to AD, are submitted to the cross-validated machine learning framework. First, only informative features are selected (green squares), while the non-informative ones are discarded. The selected features are used as inputs to train a set of machine learning classifiers (e.g., an ANN is displayed) to determine whether: i) the subject is carrier of biological AD pathology; ii) will remain SCD or will progress towards MCI or AD dementia. Abbreviations: CSF = cerebrospinal fluid; EEG = electroencephalogram; ERP = event related potentials; 3 CVT = 3-choice vigilance task; SIR = standard image recognition task; SCD = subjective cognitive decline; MCI = mild cognitive impairment; AD = Alzheimer’s disease; BDNF = brain-derived neurotrophic factor; APOE = apolipoprotein E
Discussion
On June 7, 2021, the FDA provisionally approved aducanumab, the first anti-amyloid monoclonal antibody for treating patients with MCI due to AD and mild AD dementia [63]. This approval marks a significant milestone as it is the first disease-modifying therapy for AD. Furthermore, additional AD treatments may become available in the near future [1]. As a consequence, clinicians, researchers, and health services will face increasing demands for diagnostic assessments of patients with cognitive disorders. However, these treatments are not without risks, and the most common adverse effect is amyloid-related imaging abnormality (ARIA) [64].
In this context, there is an urgent need to select cost-effective and easily accessible tools for identifying patients in the early stages of the disease, while minimizing the inclusion of patients who will not progress to AD dementia. The currently recognized AD biomarkers, such as PET neuroimaging [65,66,67] or CSF biomarkers [68, 69], are expensive, invasive, and not suitable for large-scale application. Our study aims to address these limitations by considering features that can be collected through clinical and neuropsychological examinations, as well as non-invasive assessments like EEG and blood collection.
Moreover, it is crucial to consider the target population for screening purposes. Conducting a general population screening may lead to an unacceptable number of false positive results and subsequent costs. Therefore, we focus our attention on patients SCD, who are individuals referred to memory clinics. There is increasing evidence that patients with SCD have a higher risk of carrying Alzheimer's pathology and progressing to dementia [6,7,8], compared to individuals without SCD [8]. Thus, patients with SCD represent an optimal population for screening prodromal AD.
The PREVIEW study will collect demographic, personality, cognitive, genetic, EEG, and ERP data to train a machine learning algorithm. Previous studies have successfully employed this approach to predict dementia in non-demented populations [70, 71], as well as positive AD biomarkers in patients with MCI [72, 73], indicating the great potential of this approach. However, only a few studies have focused on predicting the progression of cognitive decline [74,75,76,77], and to our knowledge, no studies have applied machine learning to predict progression from SCD to dementia.
This approach offers several advantages over classical statistics. Firstly, it allows us to consider all the collected variables simultaneously. Secondly, the machine learning procedure helps identify the most informative features for screening, enabling the development of a protocol that reduces the burden on patients and healthcare costs associated with cognitive assessments.
Furthermore, this approach will provide additional evidence to clarify the role of certain variables that still have controversial associations with SCD. For example, numerous studies have shown that individuals with SCD have lower scores on neuropsychological tests compared to those without SCD [78,79,80]. However, only a few longitudinal studies have assessed the prognostic value of baseline neuropsychological assessments, often yielding conflicting results [81,82,83,84].
Several studies have focused on the relationship between SCD and cognitive reserve [85,86,87,88,89]. Engaging in intellectual activities during earlier decades and having higher premorbid intelligence have been identified as protective factors, reducing the risk of progression from SCD to MCI [15, 16]. However, cognitive reserve seems to have a dual effect, as individuals with higher cognitive reserve exhibit faster disease progression once it begins [16, 90]. The interaction between SCD and mood disorders is also controversial. Recent community-based studies on large populations have shown that depressive symptoms increase the risk of progression to objective cognitive decline and dementia in SCD patients [91, 92]. However, a meta-analysis by Huang et al. found that depression was significantly higher in individuals with SCD compared to normal individuals, but there was no difference between SCD and MCI, or between SCD converters and non-converters [93]. Studies on personality traits have yielded conflicting results regarding their association with SCD. Most studies agree that high conscientiousness and low neuroticism are associated with a reduced risk of incident AD [94, 95]. However, a previous study found that emotional stability was significantly higher in SCD patients who progressed to MCI or AD dementia [96].
In the past decades, EEG has been extensively evaluated as a diagnostic tool for dementia [97,98,99]. However, previous studies have mostly focused on identifying quantitative EEG markers of AD compared to healthy controls. These markers can be classified into four main categories: i) spectral markers, ii) connectivity and network metrics, iii) complexity measures, and iv) microstates [100]. Regarding spectral markers, AD and MCI groups have shown slowing in oscillations of EEG activity, characterized by a decrease in higher frequency activity or an increase in low-frequency power, compared to healthy controls [101,102,103]. Other studies have demonstrated a reduction in the complexity of the EEG signal throughout the development of dementia [104,105,106]. Connectivity studies have investigated covariation patterns in EEG sensor or source signals, revealing a decrease in connectivity between brain areas, particularly in higher frequency bands, as cognitive impairment progresses [107,108,109,110]. More recently, event-related potentials (ERPs) have been suggested as potential sensitive and robust biomarkers for tracking disease progression and evaluating response to therapy [111, 112]. To the best of our knowledge, only a few studies have described quantitative EEG changes in patients with SCD [113,114,115], and ERP has not been investigated in this population thus far.
Our project has some limitations: i) CSF will not be available for all the patients; ii) neuroimaging techniques will be used only for basal assessment of patients and will not be considered for machine learning analysis; iii) healthy controls will undergo only EEG and ERP recording.
The PREVIEW study also has several strengths that deserve emphasis. As mentioned earlier, the use of machine learning is a significant strength and the primary innovative outcome of our project. Another strength is the collection of AD CSF biomarkers, which serves two main purposes: i) given that previous studies have reported an average ten-year period for SCD patients to develop dementia [8, 96], a long follow-up will be necessary to obtain an adequate sample size of patients who progress to AD. By using CSF biomarkers, we can identify patients at a higher risk of AD dementia (according to the ATN system [9]) and classify them as prodromal AD. This classification can be considered as a surrogate target for preliminary cross-sectional analyses; ii) as mentioned earlier, SCD can also be the first clinical manifestation of medical conditions other than AD. CSF biomarkers will enable us to differentiate SCD with Alzheimer's pathology from SCD due to other causes. It should be noted that our study includes patients who self-refer to our memory clinic, as recommended by previous studies, to reduce sample heterogeneity and increase the chances of identifying subjects with preclinical AD compared to community-based studies [116]. Finally, we would like to emphasize that all the features considered as potential predictors will be derived from non-invasive, relatively inexpensive, and easily accessible techniques.
Conclusions
The advent of DMTs will bring about a significant shift in the management of patients with cognitive decline caused by AD. Since the efficacy of these drugs is closely tied to the disease stage, it is crucial for clinicians to be able to identify individuals at risk of AD before neurodegeneration sets in. A suitable target population for this purpose is individuals who present with cognitive complaints but lack objective evidence of impairment. The PREVIEW study aims to extensively characterize patients with SCD through clinical, neuropsychological, neurophysiological, and genetic assessments. Utilizing a machine learning approach, we aim to assess potential biomarkers and develop a robust predictive model to evaluate the risk of progression to AD. This approach will provide relevant evidence regarding the most significant features to be assessed as the initial step in the diagnostic pathway for patients with SCD, before confirming the presence of AD pathology through more invasive and expensive tests.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- 3CVT:
-
3-Choise vigilance task
- AD:
-
Alzheimer's disease
- ADL:
-
Activities of Daily Living
- ANN:
-
Artificial neural network
- APOE :
-
Apolipoprotein E
- BDNF :
-
Brain-derived neurotrophic factor
- BFFQ:
-
Big Five Factors Questionnaire
- CLEIA:
-
Chemiluminescent enzyme immunoassay
- CSF:
-
Cerebrospinal fluid
- DMTs:
-
Disease-modifying therapies
- EEG:
-
Electroencephalography
- ERP:
-
Event-related potentials
- HDRS:
-
Hamilton Depression Rating Scale
- HRMA:
-
High-resolution melting analysis
- IADL:
-
Instrumental Activities of Daily Living
- IQR:
-
Interquartile range
- LDA:
-
Linear discriminant analysis
- MAC-Q:
-
Memory Assessment Clinics-Questionnaire
- MCI:
-
Mild Cognitive Impairment
- MMSE:
-
Minimental state examination
- NIA-AA:
-
National Institute of Aging-Alzheimer's Association
- p-tau:
-
Phosphorylated tau
- PREVIEW:
-
PRedicting the EVolution of SubjectIvE Cognitive Decline to Alzheimer's Disease With machine learning
- PSD:
-
Power spectral density
- QDA:
-
Quadratic discriminant analysis
- REDCap:
-
Research Electronic Data Capture
- RF:
-
Random forest
- ROIs:
-
Regions of interest
- RBF:
-
Radial basis function
- SCD:
-
Subjective cognitive decline
- SIR:
-
Standard image recognition
- SVM:
-
Support vector machine
- TIB:
-
Test di intelligenza breve
- t-tau:
-
Total tau
References
Cummings J, Zhou Y, Lee G, Zhong K, Fonseca J, Cheng F. Alzheimer’s disease drug development pipeline: 2023. Alzheimer Dement. 2023;9:e12385.
van Dyck CH, Swanson CJ, Aisen P, Bateman RJ, Chen C, Gee M, et al. Lecanemab in Early Alzheimer’s Disease. N Engl J Med. 2023;388:9–21.
Budd Haeberlein S, Aisen PS, Barkhof F, Chalkias S, Chen T, Cohen S, et al. Two Randomized Phase 3 Studies of Aducanumab in Early Alzheimer’s Disease. J Prev Alzheimers Dis. 2022;9:197–210.
Guest FL, Rahmoune H, Guest PC. Early Diagnosis and Targeted Treatment Strategy for Improved Therapeutic Outcomes in Alzheimer’s Disease. In: Guest PC, editor. Reviews on New Drug Targets in Age-Related Disorders. Cham: Springer International Publishing; 2020. p. 175–91.
Jessen F, Amariglio RE, van Boxtel M, Breteler M, Ceccaldi M, Chételat G, et al. A conceptual framework for research on subjective cognitive decline in preclinical Alzheimer’s disease. Alzheimers Dement. 2014;10:844–52.
Amariglio RE, Becker JA, Carmasin J, Wadsworth LP, Lorius N, Sullivan C, et al. Subjective cognitive complaints and amyloid burden in cognitively normal older individuals. Neuropsychologia. 2012;50:2880–6.
Wen C, Bi Y-L, Hu H, Huang S-Y, Ma Y-H, Hu H-Y, et al. Association of Subjective Cognitive Decline with Cerebrospinal Fluid Biomarkers of Alzheimer’s Disease Pathology in Cognitively Intact Older Adults: The CABLE Study. J Alzheimers Dis. 2022;85:1143–51.
Mitchell AJ, Beaumont H, Ferguson D, Yadegarfar M, Stubbs B. Risk of dementia and mild cognitive impairment in older people with subjective memory complaints: meta-analysis. Acta Psychiatr Scand. 2014;130:439–51.
Jack CR, Bennett DA, Blennow K, Carrillo MC, Dunn B, Haeberlein SB, et al. NIA-AA Research Framework: Toward a biological definition of Alzheimer’s disease. Alzheimers Dement. 2018;14:535–62.
Bhome R, Berry AJ, Huntley JD, Howard RJ. Interventions for subjective cognitive decline: systematic review and meta-analysis. BMJ Open. 2018;8:e021610.
Jessen F, Amariglio RE, Buckley RF, van der Flier WM, Han Y, Molinuevo JL, et al. The characterisation of subjective cognitive decline. Lancet Neurol. 2020;19:271–8.
Margolis SA, Kelly DA, Daiello LA, Davis J, Tremont G, Pillemer S, et al. Anticholinergic/Sedative Drug Burden and Subjective Cognitive Decline in Older Adults at Risk of Alzheimer’s Disease. J Gerontol Series A. 2020. https://doi.org/10.1093/gerona/glaa222.
Mazzeo S, Padiglioni S, Bagnoli S, Carraro M, Piaceri I, Bracco L, et al. Assessing the effectiveness of subjective cognitive decline plus criteria in predicting the progression to Alzheimer’s disease: an 11-year follow-up study. Eur J Neurol. 2020;27:894–9.
Giacomucci G, Mazzeo S, Padiglioni S, Bagnoli S, Belloni L, Ferrari C, et al. Gender differences in cognitive reserve: implication for subjective cognitive decline in women. Neurol Sci. 2021. https://doi.org/10.1007/s10072-021-05644-x.
Bessi V, Mazzeo S, Padiglioni S, Piccini C, Nacmias B, Sorbi S, et al. From Subjective Cognitive Decline to Alzheimer’s Disease: The Predictive Role of Neuropsychological Assessment, Personality Traits, and Cognitive Reserve. A 7-Year Follow-Up Study. J Alzheimers Dis. 2018. https://doi.org/10.3233/JAD-171180.
Mazzeo S, Padiglioni S, Bagnoli S, Bracco L, Nacmias B, Sorbi S, et al. The dual role of cognitive reserve in subjective cognitive decline and mild cognitive impairment: a 7-year follow-up study. J Neurol. 2019;266:487–97.
Mazzeo S, Bessi V, Padiglioni S, Bagnoli S, Bracco L, Sorbi S, et al. KIBRA T allele influences memory performance and progression of cognitive decline: a 7-year follow-up study in subjective cognitive decline and mild cognitive impairment. Neurol Sci. 2019. https://doi.org/10.1007/s10072-019-03866-8.
Mazzeo S, Bessi V, Bagnoli S, Giacomucci G, Balestrini J, Padiglioni S, et al. Dual Effect of PER2 C111G Polymorphism on Cognitive Functions across Progression from Subjective Cognitive Decline to Mild Cognitive Impairment. Diagnostics (Basel). 2021;11:718.
Bessi V, Mazzeo S, Bagnoli S, Padiglioni S, Carraro M, Piaceri I, et al. The implication of BDNF Val66Met polymorphism in progression from subjective cognitive decline to mild cognitive impairment and Alzheimer’s disease: a 9-year follow-up study. Eur Arch Psychiatry Clin Neurosci. 2020;270:471–82.
Ingannato A, Bagnoli S, Bessi V, Ferrari C, Mazzeo S, Sorbi S, et al. Intermediate alleles of HTT: A new pathway in longevity. J Neurol Sci. 2022;438:120274.
Bessi V, Giacomucci G, Mazzeo S, Bagnoli S, Padiglioni S, Balestrini J, et al. PER2 C111G polymorphism, cognitive reserve and cognition in subjective cognitive decline and mild cognitive impairment. A 10-year follow-up study. Eur J Neurol. 2020. https://doi.org/10.1111/ene.14518.
Mazzeo S, Emiliani F, Bagnoli S, Padiglioni S, Conti V, Ingannato A, et al. Huntingtin gene intermediate alleles influence the progression from subjective cognitive decline to mild cognitive impairment: A 14-year follow-up study. Eur J Neurol. 2022;29:1600–9.
Bessi V, Balestrini J, Bagnoli S, Mazzeo S, Giacomucci G, Padiglioni S, et al. Influence of ApoE Genotype and Clock T3111C Interaction with Cardiovascular Risk Factors on the Progression to Alzheimer’s Disease in Subjective Cognitive Decline and Mild Cognitive Impairment Patients. J Pers Med. 2020;10:45.
Ferreira D, Jelic V, Cavallin L, Oeksengaard A-R, Snaedal J, Høgh P, et al. Electroencephalography Is a Good Complement to Currently Established Dementia Biomarkers. DEM. 2016;42:80–92.
Samper-González J, Burgos N, Bottani S, Fontanella S, Lu P, Marcoux A, et al. Reproducible evaluation of classification methods in Alzheimer’s disease: Framework and application to MRI and PET data. Neuroimage. 2018;183:504–21.
Bansal A, Padappayil RP, Garg C, Singal A, Gupta M, Klein A. Utility of Artificial Intelligence Amidst the COVID 19 Pandemic: A Review. J Med Syst. 2020;44:156.
Pellegrini E, Ballerini L, Hernandez MDCV, Chappell FM, González-Castro V, Anblagan D, et al. Machine learning of neuroimaging for assisted diagnosis of cognitive impairment and dementia: A systematic review. Alzheimers Dement (Amst). 2018;10:519–35.
Lawton MP, Brody EM. Assessment of Older People: Self-Maintaining and Instrumental Activities of Daily Living. The Gerontologist. 1969;9:9 3 Part 1-86.
Albert MS, DeKosky ST, Dickson D, Dubois B, Feldman HH, Fox NC, et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:270–9.
Diagnostic and Statistical Manual of Mental Disorders. DSM Library. https://dsm.psychiatryonline.org/doi/book/https://doi.org/10.1176/appi.books.9780890425596. Accessed 19 Mar 2023.
McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR, Kawas CH, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:263–9.
Seabold S, Perktold J. Statsmodels: Econometric and Statistical Modeling with Python. Austin, Texas; 2010. p. 92–6.
Magni E, Binetti G, Bianchetti A, Rozzini R, Trabucchi M. Mini-Mental State Examination: a normative study in Italian elderly population. Eur J Neurol. 1996;3:198–202.
Monaco M, Costa A, Caltagirone C, Carlesimo GA. Forward and backward span for verbal and visuo-spatial data: standardization and normative data from an Italian adult population. Neurol Sci. 2013;34:749–54.
Carlesimo GA, Caltagirone C, Gainotti G. The Mental Deterioration Battery: normative data, diagnostic reliability and qualitative analyses of cognitive impairment. The Group for the Standardization of the Mental Deterioration Battery. Eur Neurol. 1996;36:378–84.
De Renzi E, Faglioni P, Ruggerini C. Prove di memoria verbale di impiego clinico per la diagnosi di amnesia. 1977.
Caffarra P, Vezzadini G, Dieci F, Zonato F, Venneri A. Rey-Osterrieth complex figure: normative values in an Italian population sample. Neurol Sci. 2002;22:443–7.
Giovagnoli AR, Del Pesce M, Mascheroni S, Simoncelli M, Laiacona M, Capitani E. Trail making test: normative values from 287 normal adult controls. Ital J Neurol Sci. 1996;17:305–9.
Della Sala S, Laiacona M, Spinnler H, Ubezio C. A cancellation test: its reliability in assessing attentional deficits in Alzheimer’s disease. Psychol Med. 1992;22:885–901.
Marra C, Gainotti G, Scaricamazza E, Piccininni C, Ferraccioli M, Quaranta D. The Multiple Features Target Cancellation (MFTC): an attentional visual conjunction search test. Normative values for the Italian population. Neurol Sci. 2013;34:173–80.
Novelli G, Papagno C, Capitani E, Laiacona M. Tre test clinici di ricerca e produzione lessicale. Taratura su sogetti normali. / Three clinical tests to research and rate the lexical performance of normal subjects. Archivio di Psicologia, Neurologia e Psichiatria. 1970;:477–506.
Catricalà E, Gobbi E, Battista P, Miozzo A, Polito C, Boschi V, et al. SAND: a Screening for Aphasia in NeuroDegeneration. Development and normative data. Neurol Sci. 2017;38:1469–83.
Shulman KI, Pushkar Gold D, Cohen CA, Zucchero CA. Clock-drawing and dementia in the community: A longitudinal study. Int J Geriatr Psychiatry. 1993;8:487–96.
Caffarra P, Vezzadini G, Dieci F, Zonato F, Venneri A. Una versione abbreviata del test di Stroop: Dati normativi nella popolazione Italiana. Riv Neurol. 2002;12:111–5.
Appollonio I, Leone M, Isella V, Piamarta F, Consoli T, Villa ML, et al. The Frontal Assessment Battery (FAB): normative values in an Italian population sample. Neurol Sci. 2005;26:108–16.
Crook TH, Feher EP, Larrabee GJ. Assessment of memory complaint in age-associated memory impairment: the MAC-Q. Int Psychogeriatr. 1992;4:165–76.
Colombo L, Brivio C, Benaglio I, Siri S, Capp SF. Alzheimer patients’ ability to read words with irregular stress. Cortex. 2000;36:703–14.
Bright P, Hale E, Gooch VJ, Myhill T, van der Linde I. The National Adult Reading Test: restandardisation against the Wechsler Adult Intelligence Scale-Fourth edition. Neuropsychol Rehabil. 2018;28:1019–27.
Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatr. 1960;23:56–62.
Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of Illness in the Aged: The Index of ADL: A Standardized Measure of Biological and Psychosocial Function. JAMA. 1963;185:914–9.
Goldberg LR. The development of markers for the Big-Five factor structure. Psychol Assess. 1992;4:26–42.
Costa PT, McCrae RR. The NEO personality inventory: Manual, form S and form R. Psychological Assessment Resources; 1985.
Yarnold PR, Stille FC, Martin GJ. Cross-sectional psychometric assessment of the Functional Status Questionnaire: use with geriatric versus nongeriatric ambulatory medical patients. Int J Psychiatry Med. 1995;25:305–17.
Delorme A, Makeig S. EEGLAB: an open source toolbox for analysis of single-trial EEG dynamics including independent component analysis. J Neurosci Methods. 2004;134:9–21.
Bigdely-Shamlo N, Mullen T, Kothe C, Su K-M, Robbins KA. The PREP pipeline: standardized preprocessing for large-scale EEG analysis. Frontiers in Neuroinformatics. 2015;9 JUNE:1–19.
Delorme A, Sejnowski T, Makeig S. Enhanced detection of artifacts in EEG data using higher-order statistics and independent component analysis. Neuroimage. 2007;34:1443–9.
Lassi M, Fabbiani C, Mazzeo S, Burali R, Vergani AA, Giacomucci G, et al. Degradation of EEG microstates patterns in subjective cognitive decline and mild cognitive impairment: Early biomarkers along the Alzheimer’s Disease continuum? NeuroImage. 2023;38:103407.
Bell AJ, Sejnowski TJ. An information-maximization approach to blind separation and blind deconvolution. Neural Comput. 1995;7:1129–59.
Pion-Tonachini L, Kreutz-Delgado K, Makeig S. ICLabel: An automated electroencephalographic independent component classifier, dataset, and website. Neuroimage. 2019;198:181–97.
Vecchio F, Miraglia F, Iberite F, Lacidogna G, Guglielmi V, Marra C, et al. Sustainable method for Alzheimer dementia prediction in mild cognitive impairment: Electroencephalographic connectivity and graph theory combined with apolipoprotein E. Ann Neurol. 2018;84:302–14.
Michel CM, Koenig T. EEG microstates as a tool for studying the temporal dynamics of whole-brain neuronal networks: A review. Neuroimage. 2018;180:577–93.
Pascual-Marqui RD, Michel CM, Lehmann D. Segmentation of Brain Electrical Activity into Microstates; Model Estimation and Validation. IEEE Trans Biomed Eng. 1995;42:658–65.
Rabinovici GD. Controversy and Progress in Alzheimer’s Disease - FDA Approval of Aducanumab. N Engl J Med. 2021;385:771–4.
Withington CG, Turner RS. Amyloid-Related Imaging Abnormalities With Anti-amyloid Antibodies for the Treatment of Dementia Due to Alzheimer’s Disease. Front Neurol. 2022;13:862369.
Clark CM, Pontecorvo MJ, Beach TG, Bedell BJ, Coleman RE, Doraiswamy PM, et al. Cerebral PET with florbetapir compared with neuropathology at autopsy for detection of neuritic amyloid-β plaques: a prospective cohort study. Lancet Neurol. 2012;11:669–78.
Sabri O, Sabbagh MN, Seibyl J, Barthel H, Akatsu H, Ouchi Y, et al. Florbetaben PET imaging to detect amyloid beta plaques in Alzheimer’s disease: phase 3 study. Alzheimers Dement. 2015;11:964–74.
Mueller A, Bullich S, Barret O, Madonia J, Berndt M, Papin C, et al. Tau PET imaging with 18F-PI-2620 in Patients with Alzheimer Disease and Healthy Controls: A First-in-Humans Study. J Nucl Med. 2020;61:911–9.
Lewczuk P, Esselmann H, Otto M, Maler JM, Henkel AW, Henkel MK, et al. Neurochemical diagnosis of Alzheimer’s dementia by CSF Abeta42, Abeta42/Abeta40 ratio and total tau. Neurobiol Aging. 2004;25:273–81.
Buerger K, Ewers M, Pirttilä T, Zinkowski R, Alafuzoff I, Teipel SJ, et al. CSF phosphorylated tau protein correlates with neocortical neurofibrillary pathology in Alzheimer’s disease. Brain. 2006;129(Pt 11):3035–41.
Park JH, Cho HE, Kim JH, Wall MM, Stern Y, Lim H, et al. Machine learning prediction of incidence of Alzheimer’s disease using large-scale administrative health data. npj Digit Med. 2020;3:1–7.
James C, Ranson JM, Everson R, Llewellyn DJ. Performance of Machine Learning Algorithms for Predicting Progression to Dementia in Memory Clinic Patients. JAMA Netw Open. 2021;4:e2136553.
Ezzati A, Harvey DJ, Habeck C, Golzar A, Qureshi IA, Zammit AR, et al. Predicting Amyloid-β Levels in Amnestic Mild Cognitive Impairment Using Machine Learning Techniques. J Alzheimers Dis. 2020;73:1211–9.
Kang SH, Cheon BK, Kim J-S, Jang H, Kim HJ, Park KW, et al. Machine Learning for the Prediction of Amyloid Positivity in Amnestic Mild Cognitive Impairment. J Alzheimers Dis. 2021;80:143–57.
Grueso S, Viejo-Sobera R. Machine learning methods for predicting progression from mild cognitive impairment to Alzheimer’s disease dementia: a systematic review. Alzheimer Res Ther. 2021;13:162.
Costafreda SG, Dinov ID, Tu Z, Shi Y, Liu C-Y, Kloszewska I, et al. Automated hippocampal shape analysis predicts the onset of dementia in Mild Cognitive Impairment. Neuroimage. 2011;56:212–9.
Wee C, Yap P, Shen D. Prediction of Alzheimer’s disease and mild cognitive impairment using cortical morphological patterns. Hum Brain Mapp. 2012;34:3411–25.
Young J, Modat M, Cardoso MJ, Mendelson A, Cash D, Ourselin S. Accurate multimodal probabilistic prediction of conversion to Alzheimer’s disease in patients with mild cognitive impairment. Neuroimage Clin. 2013;2:735–45.
Hao L, Sun Y, Li Y, Wang J, Wang Z, Zhang Z, et al. Demographic characteristics and neuropsychological assessments of subjective cognitive decline (SCD) (plus). Ann Clin Transl Neurol. 2020;7:1002–12.
Wolfsgruber S, Polcher A, Koppara A, Kleineidam L, Frölich L, Peters O, et al. Cerebrospinal Fluid Biomarkers and Clinical Progression in Patients with Subjective Cognitive Decline and Mild Cognitive Impairment. J Alzheimers Dis. 2017;58:939–50.
Poptsi E, Moraitou D, Tsardoulias E, Symeonidisd AL, Tsolaki M. Is the Discrimination of Subjective Cognitive Decline from Cognitively Healthy Adulthood and Mild Cognitive Impairment Possible? A Pilot Study Utilizing the R4Alz Battery. J Alzheimers Dis. 2020;77:715–32.
Kurt P, Yener G, Oguz M. Impaired digit span can predict further cognitive decline in older people with subjective memory complaint: a preliminary result. Aging Ment Health. 2011;15:364–9.
Silva D, Guerreiro M, Maroco J, Santana I, Rodrigues A, Bravo Marques J, et al. Comparison of four verbal memory tests for the diagnosis and predictive value of mild cognitive impairment. Dement Geriatr Cogn Dis Extra. 2012;2:120–31.
Balota DA, Tse C-S, Hutchison KA, Spieler DH, Duchek JM, Morris JC. Predicting Conversion to Dementia of the Alzheimer Type in a Healthy Control Sample: The Power of Errors in Stroop Color Naming. Psychol Aging. 2010;25:208–18.
Van Mierlo LD, Wouters H, Sikkes SAM, Van der Flier WM, Prins ND, Bremer JAE, et al. Screening for Mild Cognitive Impairment and Dementia with Automated, Anonymous Online and Telephone Cognitive Self-Tests. J Alzheimers Dis. 56:249–59.
Lojo-Seoane C, Facal D, Guàrdia-Olmos J, Juncos-Rabadán O. Structural Model for Estimating the Influence of Cognitive Reserve on Cognitive Performance in Adults with Subjective Memory Complaints. Arch Clin Neuropsychol. 2014;29:245–55.
Perquin M, Diederich N, Pastore J, Lair M-L, Stranges S, Vaillant M, et al. Prevalence of Dementia and Cognitive Complaints in the Context of High Cognitive Reserve: A Population-Based Study. PLoS One. 2015;10:e0138818.
João AA, Maroco J, Ginó S, Mendes T, de Mendonça A, Martins IP. Education modifies the type of subjective memory complaints in older people. Int J Geriatr Psychiatry. 2015;31:153–60.
Aghjayan SL, Buckley RF, Vannini P, Rentz DM, Jackson JD, Sperling RA, et al. The influence of demographic factors on subjective cognitive concerns and beta-amyloid. Int Psychogeriatr. 2017;29:645–52.
Lojo-Seoane C, Facal D, Guàrdia-Olmos J, Pereiro AX, Juncos-Rabadán O. Effects of Cognitive Reserve on Cognitive Performance in a Follow-Up Study in Older Adults With Subjective Cognitive Complaints. The Role of Working Memory. Front Aging Neurosci. 2018;10:189.
van Loenhoud AC, van der Flier WM, Wink AM, Dicks E, Groot C, Twisk J, et al. Cognitive reserve and clinical progression in Alzheimer disease. Neurology. 2019;93:e334–46.
Lee YC, Kang JM, Lee H, Kim K, Kim S, Yu TY, et al. Subjective cognitive decline and subsequent dementia: a nationwide cohort study of 579,710 people aged 66 years in South Korea. Alzheimers Res Ther. 2020;12:52.
Liew TM. Subjective cognitive decline, anxiety symptoms, and the risk of mild cognitive impairment and dementia. Alzheimer Res Ther. 2020;12:107.
Huang Y, Xue J, Li C, Chen X, Fu H, Fei T, et al. Depression and APOEε4 Status in Individuals with Subjective Cognitive Decline: A Meta-Analysis. Psychiatry Investig. 2020;17:858–64.
Terracciano A, Sutin AR, An Y, O’Brien RJ, Ferrucci L, Zonderman AB, et al. Personality and risk of Alzheimer’s disease: new data and meta-analysis. Alzheimers Dement. 2014;10:179–86.
Luchetti M, Terracciano A, Stephan Y, Sutin AR. Personality and Cognitive Decline in Older Adults: Data From a Longitudinal Sample and Meta-Analysis. J Gerontol B Psychol Sci Soc Sci. 2016;71:591–601.
Bessi V, Mazzeo S, Padiglioni S, Piccini C, Nacmias B, Sorbi S, et al. From Subjective Cognitive Decline to Alzheimer’s Disease: The Predictive Role of Neuropsychological Assessment, Personality Traits, and Cognitive Reserve. A 7-Year Follow-Up Study. J Alzheimers dis. 2018;63:1523–35.
Alberdi A, Aztiria A, Basarab A. On the early diagnosis of Alzheimer’s Disease from multimodal signals: A survey. Artif Intell Med. 2016;71:1–29.
Malek N, Baker MR, Mann C, Greene J. Electroencephalographic markers in dementia. Acta Neurol Scand. 2017;135:388–93.
Gouw AA, Alsema AM, Tijms BM, Borta A, Scheltens P, Stam CJ, et al. EEG spectral analysis as a putative early prognostic biomarker in nondemented, amyloid positive subjects. Neurobiol Aging. 2017;57:133–42.
Maestú F, Cuesta P, Hasan O, Fernandéz A, Funke M, Schulz PE. The Importance of the Validation of M/EEG With Current Biomarkers in Alzheimer’s Disease. Front Hum Neurosci. 2019;13:17.
Fonseca LC, Tedrus GMAS, Prandi LR, de Andrade ACA. Quantitative electroencephalography power and coherence measurements in the diagnosis of mild and moderate Alzheimer’s disease. Arq Neuropsiquiatr. 2011;69:297–303.
Jelic V, Shigeta M, Julin P, Almkvist O, Winblad B, Wahlund LO. Quantitative electroencephalography power and coherence in Alzheimer’s disease and mild cognitive impairment. Dementia. 1996;7:314–23.
Kim J-S, Lee S-H, Park G, Kim S, Bae S-M, Kim D-W, et al. Clinical Implications of Quantitative Electroencephalography and Current Source Density in Patients with Alzheimer’s Disease. Brain Topogr. 2012;25:461–74.
Kulkarni NileshN, Parhad SaurabhV, Shaikh YasminP. Use of Non-linear and Complexity Features for EEG Based Dementia & Alzheimer Disease Diagnosis. In: 2017 International Conference on Computing, Communication, Control and Automation (ICCUBEA). 2017. p. 1–3.
Shumbayawonda E, López-Sanz D, Bruña R, Serrano N, Fernández A, Maestú F, et al. Complexity changes in preclinical Alzheimer’s disease: An MEG study of subjective cognitive decline and mild cognitive impairment. Clin Neurophysiol. 2020;131:437–45.
Tait L, Tamagnini F, Stothart G, Barvas E, Monaldini C, Frusciante R, et al. EEG microstate complexity for aiding early diagnosis of Alzheimer’s disease. Scientific Reports. 2020;10.
Babiloni C, Del Percio C, Lizio R, Noce G, Lopez S, Soricelli A, et al. Functional cortical source connectivity of resting state electroencephalographic alpha rhythms shows similar abnormalities in patients with mild cognitive impairment due to Alzheimer’s and Parkinson’s diseases. Clin Neurophysiol. 2018;129:766–82.
Besthorn C, Förstl H, Geiger-Kabisch C, Sattel H, Gasser T, Schreiter-Gasser U. EEG coherence in Alzheimer disease. Electroencephalogr Clin Neurophysiol. 1994;90:242–5.
Meghdadi AH, Karić MS, McConnell M, Rupp G, Richard C, Hamilton J, et al. Resting state EEG biomarkers of cognitive decline associated with Alzheimer’s disease and mild cognitive impairment. PLoS One. 2021;16:e0244180.
Smailovic U, Koenig T, Savitcheva I, Chiotis K, Nordberg A, Blennow K, et al. Regional Disconnection in Alzheimer Dementia and Amyloid-Positive Mild Cognitive Impairment: Association Between EEG Functional Connectivity and Brain Glucose Metabolism. Brain Connect. 2020;10:555–65.
Waninger S, Berka C, Meghdadi A, Karic MS, Stevens K, Aguero C, et al. Event-related potentials during sustained attention and memory tasks: Utility as biomarkers for mild cognitive impairment. Alzheimers Dement. 2018;10:452–60.
Olichney JM, Taylor JR, Gatherwright J, Salmon DP, Bressler AJ, Kutas M, et al. Patients with MCI and N400 or P600 abnormalities are at very high risk for conversion to dementia. Neurology. 2008;70(19 Pt 2):1763–70.
Alexander DM, Arns MW, Paul RH, Rowe DL, Cooper N, Esser AH, et al. Eeg markers for cognitive decline in elderly subjects with subjective memory complaints. J Integr Neurosci. 2006;05:49–74.
Babiloni C, Visser PJ, Frisoni G, De Deyn PP, Bresciani L, Jelic V, et al. Cortical sources of resting EEG rhythms in mild cognitive impairment and subjective memory complaint. Neurobiol Aging. 2010;31:1787–98.
Jeong HT, Youn YC, Sung H-H, Kim SY. Power Spectral Changes of Quantitative EEG in the Subjective Cognitive Decline: Comparison of Community Normal Control Groups. Neuropsychiatr Dis Treat. 2021;17:2783–90.
Abdelnour C, Rodríguez-Gómez O, Alegret M, Valero S, Moreno-Grau S, Sanabria Á, et al. Impact of Recruitment Methods in Subjective Cognitive Decline. J Alzheimers Dis. 2017;57:625–32.
Acknowledgements
Not applicable.
Funding
This project underwent peer reviewed and is funded by Tuscany Region—PRedicting the EVolution of SubjectIvE Cognitive Decline to Alzheimer’s Disease With machine learning—PREVIEW—CUP. D18D20001300002.
Author information
Authors and Affiliations
Contributions
SM, SP, SS, SM, AG and VB contributed to conception and design of the study. SM, ML, SP, VM, GGa, CF, organized data collection. SM, SP, VM, GGi, MS, CM, RB, FE, SB, AI, BN, SS, AG, VB will contribute to data acquisition. SM, ML, AAV and LGA will perform the statistical analysis. SM wrote the first draft of this manuscript. ML, SP, AM, AG, AAV wrote sections of the manuscript. SM and ML prepared the figures. All authors contributed to manuscript revision, read, and approved the submitted version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All subjects will be recruited in accordance with the Declaration of Helsinki and with the ethical standards of the Committee on Human Experimentation of Careggi University Hospital (Florence, Italy). The study was approved by the local Institutional Review Board (“Comitato Etico di Area Vasta Centro” reference 15691oss). All participants in this study will sign an informed consent, agreeing to participate and to share the results deriving from their data.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mazzeo, S., Lassi, M., Padiglioni, S. et al. PRedicting the EVolution of SubjectIvE Cognitive Decline to Alzheimer’s Disease With machine learning: the PREVIEW study protocol. BMC Neurol 23, 300 (2023). https://doi.org/10.1186/s12883-023-03347-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-023-03347-8