Abstract
Background
Polyradiculoneuropathy following infection with varicella zoster virus (VZV) is rare and most of the time, happens in the context of reactivation of latent VZV. We report a case of acute polyradiculoneuropathy following primary infection with VZV marked by atypical clinical features raising the hypothesis of a para-infectious disease.
Case presentation
We describe a 43-years-old male who developed ataxia, dysphagia, dysphonia, and oculomotor disorders (vertical binocular diplopia and bilateral ptosis) followed by quadriplegia with areflexia which occurred 4 days later. The patient had a history of varicella that occurred 10 days before the onset of these symptoms. Nerve conduction study revealed features consistent with an acute motor-sensory axonal neuropathy (AMSAN). Anti-ganglioside antibodies were negative.
Based on clinical presentation and ancillary examination, we retain the Miller Fisher/Guillain-Barré overlap syndrome diagnosis.
The patient was treated with high doses of methylprednisolone but the evolution of the disease was nevertheless marked by a complete recovery six weeks after onset of symptoms.
Conclusion
GBS following varicella is a rare but severe disease occurring most often in adults and marked by greater involvement of the cranial nerves. Its clinical features suggest that it is a para-infectious disease. Antiviral therapy has no effect on the course of the disease but its administration within the first 24 h after the onset of chickenpox in adults can prevent its occurrence.
Similar content being viewed by others
Background
Guillain-Barré Syndrome (GBS) is an acute autoimmune inflammatory demyelinating polyradiculoneuropathy, clinically characterized by progressive motor weakness, areflexia with albuminocytologic dissociation on cerebrospinal fluid (CSF) study [1].
In most cases, GBS is a post-infectious disease, and the most reported pathogens are Campylobacter Jejuni, Cytomegalovirus, Epstein-Barr Virus, Measles Virus, Influenza A Virus, Mycoplasma Pneumonia, Enterovirus D68, and Zika Virus [1, 2]. The type of preceding infection may influence the clinical phenotype, course and outcome of the disease [3].
In the literature, Varicella zoster virus (VZV) is rarely cited as a trigger for GBS and it is most of the time in the context of reactivation disease from latent VZV [4]. Clinically, GBS following VZV infection is characterized by sensory-motor impairment with a greater involvement of cranial nerves [3].
The following is a report of a 43-year-old man hospitalized in April 2022 in the neurology department of Bogodogo University Hospital (Burkina-Faso) for a polyradiculoneuropathy following primary infection with VZV marked by atypical clinical features. Through this clinical case and a review of the literature we discuss the pathophysiology underlying this particular presentation, and the possible therapeutic implications.
Case presentation
It was a 43-year-old male working at a gas station as an attendant. He had a history of chickenpox which occurred on 06 April 2022, and was treated with paracetamol (1 g three times daily in case of fever) and skin antiseptic (Chlorhexidine gluconate). He was admitted to Bogodogo University Hospital's Neurology Department (Burkina-Faso) on 20 April 2022, for weakness of all four limbs, associated with dysphagia, dysphonia, and oculomotor disorders.
The onset of symptoms on 16 April 2022, was characterized by balance and gait disorders associated with a sensation of dizziness upon awakening. Two days later, the evolution was marked by swallowing disorders, a change in the timbre of the voice, and binocular diplopia. On the 5th day, the patient noted a weakness in the four limbs with tingling in the hands and feet.
At the admission, our examination found a normal consciousness, a proximal–distal weakness of the four limbs (2/5 proximally and distally according to MRC scale), a diffuse osteotendinous areflexia, involvement of the cranial nerves III, IX, and X, marked by vertical ophthalmoparesis (more noticeable on the left) and bilateral ptosis (III), dysphonia and abolition of nauseated reflex (IX) and dysphagia (X) without the respiratory disorder. The examination of gait, balance, and coordination was impossible due to the limb's weakness. No sphincter disturbance was noted. A dermatological analysis revealed chickenpox scar lesions that predominated on the face and the thorax. The patient had no history of chickenpox in childhood and was not vaccinated against chickenpox.
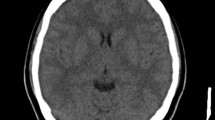
At this stage, GBS, Miller-fisher syndrome (MFS) and acute rhombencephalitis were considered. The usual biological assessment (blood count, C-reactive protein, complete blood ionogram, renal and hepatic function) came back normal. CSF analysis performed seven days after the onset of symptoms found normal proteinorachia and glycorrhachia without cells and germ. The search for anti-ganglioside antibodies (GM1, GM2, GM3, GM4, GD1a, GD1b, GD2 GD3, GT1a, GT1b, GQ1b) was negative for both IgM and IgG. VZV serology was positive for IgM and IgG, VZV testing in the CSF was not done (no technical facilities). The electroneuromyography (ENMG) performed 15 days after the onset of symptoms found increased latencies, reduced Compound Muscle Action Potentials (CMAP) amplitude, and reduced motor conduction velocities in all four limbs. Sensory nerves conduction study noted a reduction of Sensory Nerve Action Potentials (SNAP) amplitude more marked in lower limbs, with normal sensory conduction velocities (Tables 1 and 2). The Brain MRI was normal (Fig. 1A, B, C).
Based on the normality of the Brain MRI with gadolinium, we eliminate the hypothesis of rhombencephalitis. However, concerning GBS and MFS, the clinical presentation and ancillary exams, did not allow us to eliminate any of them. Thus, we retained the Miller Fisher/Guillain-Barré overlap syndrome diagnosis.
The patient received corticosteroid therapy at a dose of 500 mg/day of methylprednisolone for five days.
The evolution was positive with the total regression of dysphagia, dysphonia, and ophthalmoplegia with an improvement in motricity two weeks after the onset of symptoms (3/5 proximally and 4/5 distally according to MRC scale). We then transferred the patient to the rehabilitation unit. The patient, seen four weeks after admission to the rehabilitation unit, had recovered his motricity entirely, the examination of the cranial nerves was normal, and he was no longer presenting any complaints.
Discussion and conclusion
The patient presented clinically and electrophysiologically with an overlapping MFS and GBS syndrome. In the literature, several overlapping syndromes between GBS and MFS have been described [2, 5], and cranial nerves involvement seems to be the common point between these forms [5, 6].
Our patient had chickenpox a few days before his episode. Although rarely cited as a trigger for GBS spectrum diseases, studies have clearly shown a link between VZV infection and the occurrence of these diseases [7, 8]. Islam et al. [3] found in their literature review that cases of GBS occurring after chicken pox are mainly characterized by sensory-motor impairment, with cranial nerves involvement in 62% of cases could be. This is consistent with the clinical presentation of our study patient.
This greater involvement of the cranial nerves could find its explanation in the fact that VZV directly infects the spinal and geniculate ganglia a few weeks after the primary infection, where it remains latent for the rest of life [9]. Indeed, several arguments suggest that post-varicella polyradiculoneuropathy could be a para-infectious disease secondary to either the infectious process itself by direct attack by the virus [10], or an excessive and aberrant inflammatory immune response to the presence of the virus as described for SARS-CoV-2 [11]. Among these arguments, first, we have the short latency (less than 14 days) between the rash and the onset of neurological symptoms noted by most of the authors [3, 4, 12, 13]. Then, it was shown that VZV, which is known to infect T lymphocytes, remodels them. This could cause direct damage to the infected tissues, in particular the peripheral nerves [14, 15]. Moreover, the anti-ganglioside antibodies usually found in classic (post-infectious) cases of GBS are most often absent [3, 4, 12].
The absence of the virus in the CSF in most of the cases published and the ineffectiveness of antiviral therapy administered in some cases [12], seem to be more in favor of the excessive inflammatory immune reaction than a direct aggression by the virus. This virulence of the inflammatory immune reaction during the primary infection with VZV occurs particularly in adult and immunocompromised subjects [16]. Indeed, the majority of cases described in the literature were adult subjects. These patients had either not received antiviral treatment, or had received it several days after the onset of the rash. Unlike children, in whom it is a mild disease generally requiring only symptomatic treatment, in adults, chickenpox can be serious and an antiviral must be administered as quickly as possible to reduce viremia and serum antibodies to VZV [16]. The administration of acyclovir is recommended in the 24 h following the onset of the rash at a dose of 20 mg/kg (maximum dose of 800 mg) 4 times a day for 5 days [16].
The vaccination of adults who escaped chickenpox in childhood is also an effective way to prevent the occurrence of these severe forms. Although it is very rarely offered in several countries as chickenpox is perceived as a mild disease.
The indicated treatment in post-varicella GBS is either intravenous immunoglobulins (IVIg) or plasma exchange [3, 12]. Our patient received high doses of methylprednisolone due to the unavailability of plasma exchanges in the country and the very high cost of immunoglobulins, making them inaccessible without health insurance. Despite this unsuitable treatment [17, 18], and the fact that the disease is described as having a poor prognosis [13], the evolution was nevertheless marked in our case by a complete recovery of the patient 4 weeks after the onset of symptoms. A possible explanation would be the good prognosis of the MFS variant of GBS [19, 20].
In conclusion, GBS following varicella is a rare but severe disease occurring most often in adults and marked by greater involvement of the cranial nerves. The very short latency between the appearance of the rash and the occurrence of the polyradiculoneuropathy suggests that it is a para-infectious disease. Antiviral therapy has no effect on the course of the disease but its administration within the first 24 h after the onset of chickenpox in adults can prevent its occurrence.
Availability of data and materials
The data generated for this study are accessible upon request to the first author, Bademain Jean Fabrice Ido (idojfabrice@yahoo.fr).
Abbreviations
- GBS:
-
Guillain-Barré syndrome
- MFS:
-
Miller-Fisher syndrome
- VZV:
-
Varicella Zoster Virus
- CSF:
-
Cerebrospinal fluid
- ENMG:
-
Electroneuromyography
- CAMP:
-
Compound Muscle Action Potentials
- SNAP:
-
Sensory Nerve Action Potentials
References
Wachira VK, Peixoto HM, de Oliveira MRF. Systematic review of factors associated with the development of Guillain-Barré syndrome 2007–2017: What has changed? Trop Med Int Health. 2019;24:132–42.
Esposito S, Longo MR. Guillain-Barré syndrome Autoimmune Rev. 2017;16:96–101.
Islam B, Islam Z, Geurtsvankessel CH, Jahan I, Endtz HP, Mohammad QD, et al. Guillain-Barré syndrome following varicella-zoster virus infection. Eur J Clin Microbiol Infect Dis. 2018;37:511–8.
Cresswell F, Eadie J, Longley N, Macallan D. Severe Guillain-Barré syndrome following primary infection with varicella zoster virus in an adult. Int J Infect Dis. 2010;14(2):e161–3.
Lompo LD, Maitrot A, Aubertin A, Khatib M, Decombes R, Billaud B. Miller Fisher syndrome on the borders of Guillain-Barre syndrome: about one case and review of literature. Clin Med Rep. 2018;1(1):1–5.
Lo YL. Clinical and immunological spectrum of the Miller Fisher syndrome. Muscle Nerve. 2007;36(5):615–27.
Kang JH, Sheu JJ, Lin HC. Increased Risk of Guillain-Barré syndrome following recent herpes zoster: a population-based study across Taiwan. Clin Infect Dis. 2010;51:525–30.
Anderson TC, Leung JW, Harpaz R, Dooling KL. Risk of Guillain-Barré syndrome following herpes zoster, United States, 2010–2018. Hum Vaccin Immunother. 2021;17(12):5304–10.
Fillet AM. Histoire naturelle de l’infection à VZV : physiopathologie, mécanisme d’action et critères virologiques d’évaluation des antiviraux. Méd Mal Infect. 1998;28(spécial):767–74.
Cortese A, Tavazzi E, Delbue S, Alfonsi E, Pichiecchio A, Ceroni M, Ferrante P, Marchioni E. Varicella zoster virus-associated polyradiculoneuritis. Neurology. 2009;73(16):1334–5.
Najjar S, Najjar A, Chong DJ, Pramanik DK, Kirsch C, Kuzniecky RI, Pacia SV, Azhar S. Central nervous system complications associated with SARS-CoV-2 infection: integrative concepts of pathophysiology and case reports. J Neuroinflammation. 2020;17:231.
Tatarelli P, Garnero M, Del Bono V, Camera M, Schenone A, Grandis M, Benedetti L, Viscoli C. Guillain-Barré syndrome following chickenpox: a case series. Int J Neurosci. 2016;126:478–9.
Jasti AK, Selmi C, Sarmiento-Monroy JC, Vega DA, Anaya JM, Gershwin ME. Guillain-Barré syndrome: causes, immunopathogenic mechanisms and treatment. Expert Rev Clin Immunol. 2016;12:1175–89.
Zerboni L, Sen N, Oliver SL, Arvin AM. Molecular mechanisms of the tropism of varicella-zoster virus pathogenesis. Nat Rev Microbiol. 2014;12(3):197–210.
Sen N, Arvin AM. Dissecting the molecular mechanisms of the tropism of varicella-zoster virus for human T cells. J Virol. 2016;90(7):3284–7.
Mustafa MB, Arduino PG, Porter SR. Varicella zoster virus: review of its management. J Oral Pathol Med. 2009;38:673–88.
Guillain-Barré syndrome steroid trial group. Double-blind trial of intravenous methylprednisolone in Guillain-Barré syndrome. Lancet. 1993;341:586–90.
Hugues RAC, Newsom-David JM, Perkin GD, Pierce JM. Controlled trial prednisolone in acute polyneuropathy. Lancet. 1978;2:750–3.
Mori M, Kuwabara S. Fisher syndrome. Curr Treat Options Neurol. 2011;13:71–8.
Mori M, Kuwabara S, Fukutake T, Yuki N, Hattori T. Clinical features and prognosis of Miller Fisher syndrome. Neurology. 2001;56:1104–6.
Acknowledgements
We would like to express our gratitude to the participant for taking part in this study.
Funding
The authors fully funded this study.
Author information
Authors and Affiliations
Contributions
All authors have read and approved the manuscript. BJFI, SMG and EAC were responsible for data processing, investigations and manuscript preparation. AAD and CN were responsible for corrections and supervision.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the ethical committee of Bogodogo University Hospital. The authors acquired the patient’s consent for the involvement in and publishing of this case report.
Consent for publication
The authors acquired the patient’s written consent for the involvement in and publishing of this case report.
Competing interests
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ido, B.J.F., Guebre, S.M., Carama, E.A. et al. Is Guillain–Barre syndrome following chickenpox a parainfectious disease? A case report and literature review. BMC Neurol 23, 133 (2023). https://doi.org/10.1186/s12883-023-03185-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-023-03185-8