Abstract
Background
Mixed pathology, particularly Alzheimer’s disease with cerebrovascular lesions, is reported as the second most common cause of dementia. Research on mixed dementia typically includes people with a primary AD diagnosis and hence, little is known about the effects of co-existing amyloid pathology in people with vascular cognitive impairment (VCI). The purpose of this study was to understand whether individual differences in amyloid pathology might explain variations in cognitive impairment among individuals with clinical subcortical VCI (SVCI).
Methods
Twenty-two participants with SVCI completed an 11C Pittsburgh compound B (PIB) position emission tomography (PET) scan to quantify global amyloid deposition. Cognitive function was measured using: 1) MOCA; 2) ADAS-Cog; 3) EXIT-25; and 4) specific executive processes including a) Digits Forward and Backwards Test, b) Stroop-Colour Word Test, and c) Trail Making Test. To assess the effect of amyloid deposition on cognitive function we conducted Pearson bivariate correlations to determine which cognitive measures to include in our regression models. Cognitive variables that were significantly correlated with PIB retention values were entered in a hierarchical multiple linear regression analysis to determine the unique effect of amyloid on cognitive function. We controlled for age, education, and ApoE ε4 status.
Results
Bivariate correlation results showed that PIB binding was significantly correlated with ADAS-Cog (p < 0.01) and MOCA (p < 0.01); increased PIB binding was associated with worse cognitive function on both cognitive measures. PIB binding was not significantly correlated with the EXIT-25 or with specific executive processes (p > 0.05).
Regression analyses controlling for age, education, and ApoE ε4 status indicated an independent association between PIB retention and the ADAS-Cog (adjusted R-square change of 15.0 %, Sig F Change = 0.03). PIB retention was also independently associated with MOCA scores (adjusted R-Square Change of 27.0 %, Sig F Change = 0.02).
Conclusion
We found that increased global amyloid deposition was significantly associated with greater memory and executive dysfunctions as measured by the ADAS-Cog and MOCA. Our findings point to the important role of co-existing amyloid deposition for cognitive function in those with a primary SVCI diagnosis. As such, therapeutic approaches targeting SVCI must consider the potential role of amyloid for the optimal care of those with mixed dementia.
Trial registration
Similar content being viewed by others
Background
The world’s population is rapidly aging and the total number of people living with dementia is projected to increase globally from 24.3 million in 2001 to 81.1 million in 2040 [1]. Alzheimer’s disease (AD) and vascular cognitive impairment (VCI) are the two most common causes of cognitive dysfunction [2]. AD is a neurodegenerative disease characterized by amyloid-beta (Aβ) plaques and neurofibrillary tangles (NFT) [3]. Individuals with AD often present with impaired episodic memory, defined as the conscious retrieval of autobiographical events [3, 4]. Vascular cognitive impairment can be associated with both large vessel disease and small vessel disease [5]; this study will focus on those with subcortical VCI (SVCI) as this group is suggested to be a more homogenous group of patients that are expected to show greater predictability in their clinical picture, natural history, outcome, and treatment response [6]. SVCI is caused by small vessel damage that is typically associated with chronic and diffuse hypoperfusion causing cerebral white matter lesions (WML) and lacunes [7]. People with SVCI display relatively intact episodic memory, but show impairments on measures of executive functions, defined as higher-order cognitive processes underpinning goal directed behaviors [8].
AD and SVCI are often reported as two distinct diseases in epidemiological studies; however, evidence from neuropathological studies indicate a high rate of mixed AD-vascular pathology, generally referred to as “mixed dementia”. Mixed pathology is present in approximately half of all clinically diagnosed AD cases [9–13], including participants of AD clinical trials who were extensively screened for pure AD [14]. An autopsy study reported AD with cerebrovascular lesions to be the second most common pathology after AD [15]; thus, mixed pathology may often be the rule rather than the exception in clinical diagnosis. Recently, efforts were made in understanding the manifestation of AD with cerebrovascular disease [16]. For example, at the early AD pathology stage of entorhinal cortical involvement–which is generally clinically asymptomatic–the presence of cerebrovascular lesions is associated with cognitive impairment. This suggests that cerebrovascular lesions may lower the threshold for dementia [17]. In addition, among those with AD, the presence of ischemic lesions is associated with a greater degree of cognitive deficits compared with pure AD pathology. Overall, it is hypothesized that vascular lesions may magnify the effect of mild AD pathology, result in more severe cognitive impairment, and accelerate disease progression [18]. Currently, much of our knowledge on mixed dementia stems from the perspective of a primary AD diagnosis and hence, little is known on the effects of secondary AD pathology in a primary SVCI diagnosis. Specifically, it is unclear how co-existing amyloid pathology may affect cognitive function in people with a primary clinical SVCI diagnosis.
To investigate cognitive function in mixed pathology it is important to include cognitive domains associated with both SVCI and AD to understand the full spectrum of cognitive impairment. There is consensus that cognitive measures such as the Alzheimer’s Disease Assessment Scale-cognitive subscale (ADAS-Cog) [19], the Executive Interview Test (EXIT-25) [20], and the Montreal Cognitive Assessment (MOCA) [21] should be included for an optimal assessment battery in AD and VCI trials [22]. The ADAS-Cog is sensitive to a wide range of disease severity specific to the central dysfunctions experienced in AD including memory, praxis, and language; it is regarded as the standard instrument for use in clinical trials as a primary index of cognitive change in AD [23]. The EXIT-25 and the MOCA provide a standardized clinical assessment of executive control functions relevant to SVCI [20, 21]. Though it is important to use clinically relevant measures, these generalized tests may not capture specific processes that may be impaired in mixed dementia. As such, additional tests of specific executive functions–i.e. working memory (Digits Forward and Backward Test), attention and response inhibition (Stroop Test), and set shifting (Trail Making Test)–may be more sensitive to subtle change [24].
The neurocognitive profile of SVCI with co-existing amyloid pathology remains to be elucidated. A better understanding of the cognitive dysfunctions associated with amyloid pathology in SVCI may be a useful adjunct in the clinical assessment of mixed SVCI-AD dementia. Thus, the purpose of this study was to understand whether individual differences in amyloid pathology might explain variations in cognitive impairment among individuals with clinical SVCI, using a clinically relevant neuropsychological test battery that is sensitive to both pathologies.
Methods
Study design and participants
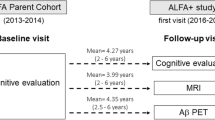
We conducted a cross-sectional analysis of baseline data acquired from a proof-of-concept randomized controlled trial of aerobic exercise (i.e., NCT01027858) [25].
This study consisted of adults with a clinical diagnosis of mild SVCI. We recruited from the University of British Columbia Hospital Clinic for AD and Related Disorders, the Vancouver General Hospital Stroke Prevention Clinic, and specialized geriatric clinics in Metro Vancouver, BC. Clinical diagnosis of SVCI was made by neurologists and geriatricians based on the presence of both small vessel ischemic disease and cognitive syndrome. Small vessel ischemic disease was defined as evidence of relevant cerebrovascular disease on MRI brain imaging that included: 1) Periventricular and deep WML: patchy areas of low attenuation or diffuse symmetrical areas of low attenuation with ill defined margins extending to the centrum semiovale, and at least one lacune; 2) Absence of cortical and or cortico-subcortical non-lacunar territorial infarcts and watershed infarcts, hemorrhages indicating large vessel disease, signs of normal pressure hydrocephalus, or other specific causes of WML (i.e. multiple sclerosis, leukodystrophies, sarcoidosis, and brain irradiation). Cognitive syndrome was defined as a MOCA score < 26/30 at baseline–the MOCA is a brief screening tool for mild cognitive impairment with high sensitivity and specificity [26]. Furthermore, study participants exhibited progressive cognitive decline (compared with previous level of cognitive function) as confirmed through medical records or caregiver/family member interviews. Overall, participants were generally functioning independently and living in the community with minimal assistance by family or caregiver. All participants underwent a physician assessment to confirm current health status and eligibility for the study. Ethical approval was obtained from the Vancouver Coastal Health Research Institute (V07-01160) and the University of British Columbia’s Clinical Research Ethics Board (H07-01160). All participants provided written informed consent.
Individuals were eligible for study entry if they met the following criteria: 1) aged 55 years or older; 2) MOCA score < 26/30 at screening [26]; 3) Mini-Mental State Examination score ≥ 20 at screening [27]; 4) lived in Metro Vancouver, Canada and was able to read, write, and speak English; 5) if participants are on cognitive medications (i.e. donepezil, galantamine, rivastigmine, memantine, etc.) they must be on a fixed dose for the duration of the trial; 6) must be in sufficient health to participate in the study’s aerobic-based exercise training program; and 7) provide informed consent. Exclusion criteria included: 1) absence of small vessel ischemic lesions such as WML or lacunes on brain CT or MRI; 2) diagnosed with another type of dementia (e.g. AD, dementia with lewy bodies, or frontal-temporal dementia) or other neurological conditions (e.g. multiple sclerosis or Parkinson’s disease); 3) taking medications that may negatively affect cognitive function (e.g. anticholinergics); and 4) people who planned to participate in a clinical drug trial concurrent to this study. This analysis included a sub-set of 22 participants who met the overall study eligibility criteria and volunteered to complete a positron emission tomography (PET) scan.
Descriptive variables
Demographic variables
Information regarding age, sex, education level, body mass index (BMI), and waist-hip ratio (WHR) was collected at study entry.
WML quantification
Scanning protocol
Structural MRI data was acquired on a Philips 3 T Achieva MRI scanner (Philips Medical Systems, Best, The Netherlands) at the UBC MRI Research Centre. A T2-weighted scan and a Proton-Density-weighted (PD-weighted) scan were acquired. The repetition time (TR) and echo time (TE) for the T2-weighted images were TR = 5431 and TE = 90 ms and for the PD-weighted images were TR = 2000 ms and TE = 8 ms. Dimensions for the T2-and PD-weighted scans were 256 × 256 × 60 voxels with a voxel size of 0.937 × 0.937 × 3.000 mm.
Image analysis
Prior to lesion identification and segmentation, each MR image was preprocessed using standard and publicly available neuroimaging tools that included: 1) MR intensity inhomogeneity correction using a multiscale version of the nonparametric non-uniform intensity normalization method (N3) [28]; 2) a structure-preserving noise-removal filter (SUSAN) was applied [29]; and 3) all non-brain tissues were removed using the brain extraction tool (BET) [30].
WML were identified and digitally marked by a single radiologist with extensive experience in WML identification. The radiologist used the following guidelines in the seeding procedure, which was designed to be simple while enabling subsequent automated processing:
-
1.
Mark all distinct WML regardless of size.
-
2.
Place more than one point on a lesion if the additional points would help define the extent of the lesion.
-
3.
Place at least one point near the center of each lesion.
WML were then segmented by a method that automatically computed the extent of each marked lesion [31]. This segmentation method has been extensively validated in large data sets with a large range of lesion loads, and was found to be highly accurate compared to radiologist segmentations and also robust to variations in the placement of the seed points [31]. Full details on the point placement procedure and subsequent automatic segmentation are described in previous work [31], but briefly, the seed points were processed by a customized Parzen windows classifier [32] to estimate the intensity distribution of the lesions. The algorithm included heuristics to optimize the accuracy of the estimated distributions by dynamically adjusting the position and the number of seed points used for the Parzen window computation, as well as a spatial method that approximated visual shape partitioning to identify areas that were likely to be false positives. The lesion masks were then used to quantify WML volumes in mm3.
Dependent variables
Global cognitive function
MOCA
This is a cognitive screening tool that includes an assessment of set shifting, visuospatial abilities, short-term and working memory, attention, concentration, language, abstraction, and orientation to time and place–generally, it places emphasis on executive functions [33]. The MOCA computes a score out of 30 with lower scores indicating greater cognitive impairment. The MOCA is a sensitive tool for detecting both mild cognitive impairment [26] and VCI, including SVCI [34].
ADAS-Cog
This scale assesses memory, language, and praxis. There are 11 tests and scores range from 0 to 70 with higher scores indicating greater cognitive dysfunction. The inter-rater reliability of the ADAS-Cog is 0.989 and its test-retest reliability is 0.915 [35].
Executive functions
EXIT-2
This is a standardized clinical assessment of global executive functions [20, 36] and is designed to detect frontal systems pathology [37]. This test contains 25 items and scores range from 0 to 50 with higher scores indicating greater global executive dysfunctions. This measure can accurately separate non-demented subjects from those with cortical or subcortical dementias [38]. Its inter-rater reliability is 0.90 [39].
Specific executive processes
Three specific executive processes were measured: 1) Working memory was assessed with the Verbal Digits Forward and Backward Tests [40]. Participants repeated progressively longer random number sequences in the same order as presented (forward) and in the reversed order (backward). The difference in score between the two tests was calculated, with smaller differences indicating better performance; 2) Selective attention and conflict resolution was assessed by the Stroop test [41], which involved three different conditions (80 trials each). First, participants read out words printed in black ink; second, they named the display colour of coloured-X’s; and third, they were shown a page with colour-words printed in incongruent coloured inks (e.g., the word “BLUE” printed in red ink). Participants were asked to name the ink colour in which the words were printed (while ignoring the word itself). We recorded the time participants took to read the items in each condition and calculated the time difference between the third condition and the second condition. Smaller time differences indicate better selective attention and conflict resolution; 3) Set shifting was assessed by the Trail Making Test (Part A and B) [42]. First, participants drew lines connecting encircled numbers sequentially (Part A) then they were asked to alternate between numbers and letters (Part B). The difference in time to complete Part B and Part A was calculated, smaller difference scores indicated better performance.
Independent variables
Amyloid imaging
Scanning protocol
PET scans were performed using 11C-PIB produced at UBC TRIUMF. Scans were performed in 3-D mode using the GE Advance tomograph (General Electric, Canada/USA). Prior to injection, a 10-minute transmission scan with a 68Ge rod was collected for attenuation correction. After the transmission scan, 555 to 560 MBq of 11C-PIB was injected as a bolus into the antecubital vein and flushed with saline. A 90-minute dynamic acquisition started at tracer injection and data were framed into an 18×300 sec imaging sequence.
Image analysis
Parametric images of the non-displaceable binding potential (BPND) [43] were generated using tissue input Logan graphical analysis [44, 45] with the cerebellum as the reference region. This method has been validated as reliable for quantification of amyloid deposition [46, 47]. A mean PIB-PET image, i.e. radiotracer concentration averaged over the entire scan duration was also formed for image co-registration and ROI definition purposes. Using SPM 8 (Wellcome Department of Cognitive Neurology, Institute of Neurology, University College London) each subject’s MRI image was co-registered to the corresponding mean PIB-PET image. Each subject’s MRI image was then normalized to the SPM MNI305 template and the corresponding transformation parameters were applied to the subject’s PET images (mean and parametric images). For those without MRI scans (5 subjects did not scan due to MR contraindications), the subject’s mean PIB-PET image was normalized to a mean PIB-PET image template in MNI space. This PIB-PET image template was created by averaging 6 healthy control PIB-PET scans that had all been warped with their own MRI to the SPM MNI305 template.
Regions of interest analysis
A custom set of regions of interest (ROIs) was defined on the coronal view of the MNI305 template [48]. These ROIs were transposed to each subject’s warped MRI and mean-PET images (in MNI space). ROIs were adjusted as necessary using both the MRI and mean PIB-PET image for guidance (1–2 pixels maximum). The modified set of ROIs was then applied to the parametric PIB-PET image and the average BPND within each ROI was extracted. Global PIB binding was determined by averaging values in bilateral frontal (combined orbitofrontal and medial prefrontal cortex), parietal (combined angular gyrus, superior parietal, precuneus, and supramarginal gyrus), temporal (combined lateral temporal and middle temporal gyrus), and occipital cortices, and anterior and posterior cingulate gyrus [49].
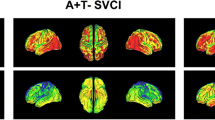
PIB-positive vs PIB-negative categorization
To determine PIB-positive/negative categorization we used standardized uptake values (SUV–tracer concentration/(injected dose/body weight)) normalized to the cerebellar cortex SUV, referred to as SUV ratio (SUVR–global SUV/cerebellar cortex SUV). An SUVR threshold of 1.50 was implemented–this PIB threshold was based on studies in a large group of cognitively normal subjects studied at the University of Pittsburgh [50] and is used by ADNI [51]. Participants with global SUVR above 1.50 were categorized as PIB-positive; participants with global SUVR below 1.50 were categorized as PIB-negative.
Amyloid and cognitive function
To determine the effect of amyloid on cognitive function we used Logan graphical analysis [44, 45] as it is more accurate when compared with SUVR [52].
Covariates
APOE ε4 genotype
ApoE genotype was determined using TaqMan assay systems for the single nucleotide polymorphisms–219G/T. DNA was extracted from whole blood using an automated DNA extraction machine (AutogenflexStar, Autogen Inc, Hollisten, MA). Because the ApoE ε4 genotype is relatively rare, the ApoE ε4 genotype odds ratios was collapsed into 2 main categories: those with at least 1 ε4 allele and those with no ε4 allele [53].
Statistical analysis
All statistical analyses were performed using Statistical Package for the Social Sciences 22.0. Initial data inspection determined that the distributions were normal (all skew values were less than the absolute value of 1). We first conducted Pearson bivariate correlations to determine which cognitive measures to include in our regression models–cognitive variables that were significantly correlated with PIB BPND values (p ≤ .05) were then entered in a hierarchical multiple linear regression analysis to determine the unique effect of amyloid on cognitive function. In the regression age, education, and ApoE ε4 status were entered in the first step as covariates, and PIB BPND was entered in the second step to determine the unique contribution of amyloid of cognitive function. However, due to our small sample size we conducted a regression analysis without covariates and a regression with covariates to ensure the robustness of our results. Also, we report adjusted R2 values, which penalizes the explained variance for each additional covariate. For each hierarchical regression model, we computed collinearity statistics (tolerance and variance inflation factor), histograms of the residuals, and scatterplots of the predicted versus residual values to ensure that the assumptions of linear regression were met. In all models, mutlicollinearity was not an issue among predictor variables, and the residuals were normally distributed and homoscedastic. These analyses also confirmed a linear association between the predictors and outcome variables for a hierarchical multiple linear regression.
Results
Descriptive variables
Twenty-two participants (8 females, 14 males) completed PIB-PET imaging. The mean age was 72.95 ± 7.76 years with an average MOCA score of 23.54 ± 2.34. Five out of 22 participants did not complete an MRI scan due to MR contraindications (e.g. presence of coronary stent or artificial optic lens). One scan was discarded from WML quantification analysis due to severe motion artifacts–with a subset of 16 participants, WML volume ranged from 23.49-3093.39 mm3 with an average of 616.41 ± 849.13 mm3. Of 22 participants, six were PIB-positive and 16 were PIB-negative. The global PIB BPND was 0.07 ± 0.23. Detailed demographic characteristics, neuropsychological test results, WML volume, and PIB BPND values are presented in Table 1. Compared with the total participants in the randomized controlled trial, this subset was not different in age (mean difference = 2.42, p > 0.05), but displayed higher MOCA scores (mean difference = 3.07, p < 0.01).
Bivariate correlations
PIB binding was significantly correlated with ADAS-Cog (r = 0.58, p < 0.01) and MOCA (r = −0.55, p < 0.01)–specifically, increased PIB BPND was associated with worse cognitive performance on the ADAS-Cog and the MOCA (Table 2). PIB BPND was not significantly correlated with the EXIT-25 or with any of the specific executive processes (p > 0.05).
Linear regression
To determine the independent association between PIB BPND and ADAS-Cog and MOCA scores we conducted a hierarchical multiple linear regression.
ADAS-Cog
Without covariates in the model, PIB rentention accounted for 31.0 % (adjusted R-square) of the variance in ADAS-Cog scores (F [1, 20] = 10.27, p = 0.00–Table 3). When controlled for age, education, and APOE ε4, this accounted for 27.0 % of the variance in ADAS-Cog scores. Adding PIB BPND to the model resulted in a significant adjusted R-square change of 15.0 % (F Change [1, 17] = 5.78, Sig F Change = 0.03–Table 3). The total adjusted variance accounted by the final model was 42.0 %.
MOCA
Without covariates in the model, PIB retention accounted for 27.0 % (adjusted R-square) of the variance in MOCA scores (F [1, 20] = 8.66, p = 0.01–Table 4). When controlled for age, education, and APOE ε4 this accounted for–7.0 % of the variance in MOCA scores, which suggests that the penalty for adding these covariates outweighed their explained variance in MOCA scores. Adding PIB BPND to the model resulted in a significant adjusted R-square change of 27.0 % (F Change [1, 17] = 6.98, Sig F Change = 0.02–Table 4). The total adjusted variance accounted by the final model was 20.0 %.
Discussion
To date, few studies have focused on the role of co-existing amyloid pathology in a primary SVCI diagnosis. Our study found that six out of twenty-two participants with clinical SVCI were PIB-positive. In assessing the effect of amyloid on cognitive function, we found that increased global amyloid deposition–suggestive of co-existing Alzheimer pathology–was significantly associated with worse cognitive function as indicated by the ADAS-Cog and MOCA. Our findings concur with and extend the results of previous literature assessing the role of amyloid on cognitive function in people with mild cognitive impairments (MCI) and healthy older adults.
The ADAS-Cog primarily assesses episodic memory and has been linked to amyloid deposition [54]. This association is present in both healthy older adults and people with MCI. Longitudinal studies in healthy older adults found that increased PIB binding was associated with greater memory decline over time [55, 56] and may be indicative of preclinical AD [56]. A similar association is found in people with MCI. Several studies have found increased PIB binding to be strongly correlated with episodic memory impairments in amnestic MCI subtypes [57, 58]; furthermore, PIB-positive amnestic MCI patients are more likely to progress to AD [59, 60]. Together, these previous studies have established the association between amyloid and memory impairments within an AD context. The current study extends previous knowledge of amyloid deposition by showing that greater amyloid deposition on PIB-PET screening is associated with greater memory impairment in a SVCI cohort.
Our study also found increased amyloid to be associated with lower MOCA scores, which assesses a mix of cognitive functions with an emphasis on executive functions. Though AD is typically associated with memory impairments, people in the early stages of AD display executive dysfunctions [61, 62]; thus, it is plausible that amyloid deposition would also be associated with executive dysfunctions. However, we note that we did not find a significant association with specific executive measures (i.e., Digit Span Test, Stroop test, and Trail Making Test) and the EXIT-25 test. No other studies have reported data on the EXIT-25 and few studies have examined the effect of amyloid deposition on specific executive processes. One reason for these non-significant results may lie in the minimal power of these tests to detect an effect. A complex statistical study conducted by ADNI found a composite score (ADNI-EF included: Category Fluency, Clock Drawing, WAIS-R Digit Symbol, Digit Span Backwards, and the Trail Making Test including Trails A, Trails B, and Trails B minus Trails A) to be superior to any independent measure of executive functioning. Specifically, ADNI-EF was sensitive to capturing changes in cognitive function over time and was the strongest baseline predictor of conversion to AD [63]. Although the MOCA does include a memory subtest, it places greater emphasis on tasks of executive function and has similar components to ADNI-EF (includes Clock Drawing, Digit Span Backwards, and Trail Making and additionally includes a phonemic fluency task, a two-item verbal abstraction task, a sustained attention task, and a concentration task). Thus, the MOCA–as a global composite measure–may be more sensitive compared with specific executive processes.
Overall, we found that amyloid was associated with impairments in multiple domains of cognitive function including memory and executive dysfunctions in people with clinical SVCI. A similar study conducted by Lee and colleagues [64] found that PIB retention in people with small vessel MCI was associated with impairments in multiple domains of cognitive function including language, visuospatial, memory, and executive functions. Furthermore, these results concur with a study published by Nordlund and colleagues [65] who found that people with cognitive impairments in multiple domains (i.e. memory and executive dysfunctions) were more likely to convert to mixed dementia and vascular dementia compared with people who exhibited either memory or executive dysfunction alone.
However, our conclusions are not without limitations. First, this is an exploratory study, and thus, is limited by its small sample size; therefore, we are limited in our ability to detect smaller effects and future studies are required to confirm and extend our current results. We also did not account for the effect of NFT on cognitive function. This is of particular importance as neocortical NFT is more consistently correlated with dementia severity, and it is suggested that NFT may mediate the association of amyloid on cognitive function [66]. In addition, we were not able to acquire MRI scans in all participants and did not have the sample size to include WML as a covariate. As a result, it is not clear how WML may have uniquely contributed to performance on the ADAS-Cog and MOCA. This is particularly important as declines in memory and executive functions have been linked to increased subcortical white matter disease [67–69]. However, a study published by Park and colleagues [49] investigating the relationship between cerebrovascular disease, amyloid, and cognitive function in SVCI suggested that amyloid burden and SVCI pathology were largely unrelated and that the effects of amyloid on cognition is independent of markers of SVCI pathology. The unique impact of amyloid on cognitive function is further supported by evidence in cerebrospinal fluid (CSF). A study assessing the role of amyloid beta (the 42-amino-acid form–Aβ1–42) and neurofilament light (NF-L)–elevated concentration of NF-L in CSF are associated with WML and small vessel disease—in CSF found that only Aβ1–42 was associated with worse cognitive outcomes in people with cerebral vascular disease [70]. Overall, the results of our study and previous studies [64, 70, 71] suggest that increased amyloid is independently associated with worse cognitive outcomes in people with vascular disease.
Conclusion
It is reported that approximately 33 % of those with SVCI exhibit amyloid pathology [71]. Yet, few studies have investigated the effect of amyloid deposition in people with SVCI and fewer studies have assessed PIB rentention as a continuous variable. Categorical diagnostic classifications of AD, SVCI, and mixed AD/SVCI in clinical practice fail to take into account the reality of a gradient of brain amyloid deposition across these disease states. Our findings point to the important role of amyloid deposition for cognitive function even among those with a primary SVCI diagnosis. As such, therapeutic approaches targeting SVCI must consider the potential role of amyloid for the optimal care of those with mixed dementia.
References
Ferri CP, Prince M, Brayne C, Brodaty H, Fratiglioni L, Ganguli M, et al. Global prevalence of dementia: a Delphi consensus study. Lancet. 2005;366(9503):2112–7. doi:10.1016/S0140-6736(05)67889-0.
Dementia: a public health priority. World Health Organization. 2012.
Mattson MP. Pathways towards and away from Alzheimer’s disease. Nature. 2004;430(7000):631–9. doi:10.1038/nature02621.
Tulving E. Episodic memory: from mind to brain. Annu Rev Psychol. 2002;53:1–25. doi:10.1146/annurev.psych.53.100901.135114.
Moorhouse P, Rockwood K. Vascular cognitive impairment: current concepts and clinical developments. Lancet Neurol. 2008;7(3):246–55. doi:10.1016/S1474-4422(08)70040-1.
Erkinjuntti T. Subcortical ischemic vascular disease and dementia. Int Psychogeriatr. 2003;15 Suppl 1:23–6. doi:10.1017/S1041610203008925.
Gorelick PB, Scuteri A, Black SE, Decarli C, Greenberg SM, Iadecola C, et al. Vascular contributions to cognitive impairment and dementia: a statement for healthcare professionals from the american heart association/american stroke association. Stroke. 2011;42(9):2672–713. doi:10.1161/STR.0b013e3182299496.
Breteler MM, van Swieten JC, Bots ML, Grobbee DE, Claus JJ, van den Hout JH, et al. Cerebral white matter lesions, vascular risk factors, and cognitive function in a population-based study: the Rotterdam Study. Neurology. 1994;44(7):1246–52.
Jellinger KA, Attems J. Neuropathological evaluation of mixed dementia. J Neurol Sci. 2007;257(1–2):80–7. doi:10.1016/j.jns.2007.01.045.
Kalaria RN. The role of cerebral ischemia in Alzheimer’s disease. Neurobiol Aging. 2000;21(2):321–30.
Rockwood K, Macknight C, Wentzel C, Black S, Bouchard R, Gauthier S, et al. The diagnosis of “mixed” dementia in the Consortium for the Investigation of Vascular Impairment of Cognition (CIVIC). Ann N Y Acad Sci. 2000;903:522–8.
Schneider JA, Arvanitakis Z, Bang W, Bennett DA. Mixed brain pathologies account for most dementia cases in community-dwelling older persons. Neurology. 2007;69(24):2197–204. doi:10.1212/01.wnl.0000271090.28148.24.
Zekry D, Hauw JJ, Gold G. Mixed dementia: epidemiology, diagnosis, and treatment. J Am Geriatr Soc. 2002;50(8):1431–8.
Wang BW, Lu E, Mackenzie IR, Assaly M, Jacova C, Lee PE, et al. Multiple pathologies are common in Alzheimer patients in clinical trials. Can J Neurol Sci. 2012;39(5):592–9.
Jellinger KA, Attems J. Prevalence of dementia disorders in the oldest-old: an autopsy study. Acta Neuropathol. 2010;119(4):421–33. doi:10.1007/s00401-010-0654-5.
Dubois B, Feldman HH, Jacova C, Cummings JL, Dekosky ST, Barberger-Gateau P, et al. Revising the definition of Alzheimer’s disease: a new lexicon. Lancet Neurol. 2010;9(11):1118–27. doi:10.1016/S1474-4422(10)70223-4.
Esiri MM, Nagy Z, Smith MZ, Barnetson L, Smith AD. Cerebrovascular disease and threshold for dementia in the early stages of Alzheimer’s disease. Lancet. 1999;354(9182):919–20. doi:10.1016/S0140-6736(99)02355-7.
Nagy Z, Esiri MM, Jobst KA, Morris JH, King EM, McDonald B, et al. The effects of additional pathology on the cognitive deficit in Alzheimer disease. J Neuropathol Exp Neurol. 1997;56(2):165–70.
Rosen WG, Mohs RC, Davis KL. A new rating scale for Alzheimer’s disease. Am J Psychiatry. 1984;141(11):1356–64.
Royall DR, Mahurin RK, Gray KF. Bedside assessment of executive cognitive impairment: the executive interview. J Am Geriatr Soc. 1992;40(12):1221–6.
Koski L. Validity and applications of the Montreal cognitive assessment for the assessment of vascular cognitive impairment. Cerebrovasc Dis. 2013;36(1):6–18. doi:10.1159/000352051.
O’Brien J, Lilienfeld S. Relevant clinical outcomes in probable vascular dementia and Alzheimer’s disease with cerebrovascular disease. J Neurol Sci. 2002;203–204:41–8.
Mohs RC, Kawas C, Carrillo MC. Optimal design of clinical trials for drugs designed to slow the course of Alzheimer’s disease. Alzheimers Dement. 2006;2(3):131–9. doi:10.1016/j.jalz.2006.04.003.
Hachinski V, Iadecola C, Petersen RC, Breteler MM, Nyenhuis DL, Black SE, et al. National Institute of Neurological Disorders and Stroke-Canadian Stroke Network vascular cognitive impairment harmonization standards. Stroke. 2006;37(9):2220–41. doi:10.1161/01.STR.0000237236.88823.47.
Liu-Ambrose T, Eng JJ, Boyd LA, Jacova C, Davis JC, Bryan S, et al. Promotion of the mind through exercise (PROMoTE): a proof-of-concept randomized controlled trial of aerobic exercise training in older adults with vascular cognitive impairment. BMC Neurol. 2010;10:14. doi:10.1186/1471-2377-10-14.
Nasreddine ZS, Phillips NA, Bedirian V, Charbonneau S, Whitehead V, Collin I, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695–9. doi:10.1111/j.1532-5415.2005.53221.x.
Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–98.
Sled JG, Zijdenbos AP, Evans AC. A nonparametric method for automatic correction of intensity nonuniformity in MRI data. IEEE Trans Med Imaging. 1998;17(1):87–97. doi:10.1109/42.668698.
Smith SMB JM. SUSAN-a new approach to low level image processing. Int J Comput Vis. 1997;23:1.
Smith SM. Fast robust automated brain extraction. Hum Brain Mapp. 2002;17(3):143–55. doi:10.1002/hbm.10062.
McAusland J, Tam R, Wong E, Riddehough A, Li D. Optimizing the Use of Radiologist Seed Points for Improved Multiple Sclerosis Lesion Segmentation. IEEE Trans Biomed Eng. 2010. doi:10.1109/TBME.2010.2055865.
Parzen E. On estimation of a probability density function and mode. Ann Math Stat. 1962;33:1065–76.
Lam B, Middleton LE, Masellis M, Stuss DT, Harry RD, Kiss A, et al. Criterion and convergent validity of the Montreal cognitive assessment with screening and standardized neuropsychological testing. J Am Geriatr Soc. 2013;61(12):2181–5. doi:10.1111/jgs.12541.
Dong Y, Sharma VK, Chan BP, Venketasubramanian N, Teoh HL, Seet RC, et al. The Montreal Cognitive Assessment (MoCA) is superior to the Mini-Mental State Examination (MMSE) for the detection of vascular cognitive impairment after acute stroke. J Neurol Sci. 2010;299(1–2):15–8. doi:10.1016/j.jns.2010.08.051.
Kirk A. Target symptoms and outcome measures: cognition. Can J Neurol Sci. 2007;34 Suppl 1:S42–6.
Stokholm J, Vogel A, Gade A, Waldemar G. The executive interview as a screening test for executive dysfunction in patients with mild dementia. J Am Geriatr Soc. 2005;53(9):1577–81. doi:10.1111/j.1532-5415.2005.53470.x.
Royall DR, Rauch R, Roman GC, Cordes JA, Polk MJ. Frontal MRI findings associated with impairment on the Executive Interview (EXIT25). Exp Aging Res. 2001;27(4):293–308. doi:10.1080/03610730109342350.
Roman GC, Royall DR. Executive control function: a rational basis for the diagnosis of vascular dementia. Alzheimer Dis Assoc Disord. 1999;13 Suppl 3:S69–80.
Royall DR, Chiodo LK, Polk MJ. Executive dyscontrol in normal aging: normative data, factor structure, and clinical correlates. Curr Neurol Neurosci Rep. 2003;3(6):487–93.
Wechsler D. Wechsler adult intelligence scale. 4edth ed. New York: NCS Pearson; 2008.
Trenerry M. Stroop neuropsychological screening test manual. Odessa, FL: Psychological Assessment Resources; 1989.
Allen DN, Haderlie MM. Trail-making test. The Corsini Encyclopedia of Psychology: Wiley; 2010.
Innis RB, Cunningham VJ, Delforge J, Fujita M, Gjedde A, Gunn RN, et al. Consensus nomenclature for in vivo imaging of reversibly binding radioligands. J Cereb Blood Flow Metab. 2007;27(9):1533–9. doi:10.1038/sj.jcbfm.9600493.
Logan J, Fowler JS, Volkow ND, Wang GJ, Ding YS, Alexoff DL. Distribution volume ratios without blood sampling from graphical analysis of PET data. J Cereb Blood Flow Metab. 1996;16(5):834–40. doi:10.1097/00004647-199609000-00008.
Logan J, Fowler JS, Volkow ND, Wolf AP, Dewey SL, Schlyer DJ, et al. Graphical analysis of reversible radioligand binding from time-activity measurements applied to [N-11C-methyl]-(−)-cocaine PET studies in human subjects. J Cereb Blood Flow Metab. 1990;10(5):740–7. doi:10.1038/jcbfm.1990.127.
Lopresti BJ, Klunk WE, Mathis CA, Hoge JA, Ziolko SK, Lu X, et al. Simplified quantification of Pittsburgh Compound B amyloid imaging PET studies: a comparative analysis. J Nucl Med. 2005;46(12):1959–72.
Price JC, Klunk WE, Lopresti BJ, Lu X, Hoge JA, Ziolko SK, et al. Kinetic modeling of amyloid binding in humans using PET imaging and Pittsburgh Compound-B. J Cereb Blood Flow Metab. 2005;25(11):1528–47. doi:10.1038/sj.jcbfm.9600146.
Collins DL, Neelin P, Peters TM, Evans AC. Automatic 3D intersubject registration of MR volumetric data in standardized Talairach space. J Comput Assist Tomogr. 1994;18(2):192–205.
Park JH, Seo SW, Kim C, Kim SH, Kim GH, Kim ST, et al. Effects of cerebrovascular disease and amyloid beta burden on cognition in subjects with subcortical vascular cognitive impairment. Neurobiol Aging. 2014;35(1):254–60. doi:10.1016/j.neurobiolaging.2013.06.026.
Aizenstein HJ, Nebes RD, Saxton JA, Price JC, Mathis CA, Tsopelas ND, et al. Frequent amyloid deposition without significant cognitive impairment among the elderly. Arch Neurol. 2008;65(11):1509–17. doi:10.1001/archneur.65.11.1509.
Jagust WJ, Bandy D, Chen K, Foster NL, Landau SM, Mathis CA, et al. The Alzheimer’s Disease Neuroimaging Initiative positron emission tomography core. Alzheimers Dement. 2010;6(3):221–9. doi:10.1016/j.jalz.2010.03.003.
Yaqub M, Tolboom N, Boellaard R, van Berckel BN, van Tilburg EW, Luurtsema G, et al. Simplified parametric methods for [11C] PIB studies. NeuroImage. 2008;42(1):76–86. doi:10.1016/j.neuroimage.2008.04.251.
Hsiung GY, Sadovnick AD, Feldman H. Apolipoprotein E epsilon4 genotype as a risk factor for cognitive decline and dementia: data from the Canadian Study of Health and Aging. CMAJ. 2004;171(8):863–7. doi:10.1503/cmaj.1031789.
Doraiswamy PM, Sperling RA, Johnson K, Reiman EM, Wong TZ, Sabbagh MN, et al. Florbetapir F 18 amyloid PET and 36-month cognitive decline: a prospective multicenter study. Mol Psychiatry. 2014;19(9):1044–51. doi:10.1038/mp.2014.9.
Resnick SM, Sojkova J, Zhou Y, An Y, Ye W, Holt DP, et al. Longitudinal cognitive decline is associated with fibrillar amyloid-beta measured by [11C] PiB. Neurology. 2010;74(10):807–15. doi:10.1212/WNL.0b013e3181d3e3e9.
Villemagne VL, Pike KE, Darby D, Maruff P, Savage G, Ng S, et al. Abeta deposits in older non-demented individuals with cognitive decline are indicative of preclinical Alzheimer’s disease. Neuropsychologia. 2008;46(6):1688–97. doi:10.1016/j.neuropsychologia.2008.02.008.
Forsberg A, Engler H, Almkvist O, Blomquist G, Hagman G, Wall A, et al. PET imaging of amyloid deposition in patients with mild cognitive impairment. Neurobiol Aging. 2008;29(10):1456–65. doi:10.1016/j.neurobiolaging.2007.03.029.
Pike KE, Savage G, Villemagne VL, Ng S, Moss SA, Maruff P, et al. Beta-amyloid imaging and memory in non-demented individuals: evidence for preclinical Alzheimer’s disease. Brain. 2007;130(Pt 11):2837–44. doi:10.1093/brain/awm238.
Okello A, Koivunen J, Edison P, Archer HA, Turkheimer FE, Nagren K, et al. Conversion of amyloid positive and negative MCI to AD over 3 years: an 11C-PIB PET study. Neurology. 2009;73(10):754–60. doi:10.1212/WNL.0b013e3181b23564.
Wolk DA, Price JC, Saxton JA, Snitz BE, James JA, Lopez OL, et al. Amyloid imaging in mild cognitive impairment subtypes. Ann Neurol. 2009;65(5):557–68. doi:10.1002/ana.21598.
Collette F, Van der Linden M, Salmon E. Executive dysfunction in Alzheimer’s disease. Cortex. 1999;35(1):57–72.
Sgaramella TM, Borgo F, Mondini S, Pasini M, Toso V, Semenza C. Executive deficits appearing in the initial stage of Alzheimer’s disease. Brain Cogn. 2001;46(1–2):264–8.
Gibbons LE, Carle AC, Mackin RS, Harvey D, Mukherjee S, Insel P, et al. A composite score for executive functioning, validated in Alzheimer’s Disease Neuroimaging Initiative (ADNI) participants with baseline mild cognitive impairment. Brain Imaging Behav. 2012;6(4):517–27. doi:10.1007/s11682-012-9176-1.
Lee MJ, Seo SW, Na DL, Kim C, Park JH, Kim GH, et al. Synergistic effects of ischemia and beta-amyloid burden on cognitive decline in patients with subcortical vascular mild cognitive impairment. JAME Psychiatry. 2014;71(4):412–22. doi:10.1001/jamapsychiatry.2013.4506.
Nordlund A, Rolstad S, Klang O, Edman A, Hansen S, Wallin A. Two-year outcome of MCI subtypes and aetiologies in the Goteborg MCI study. J Neurol Neurosurg Psychiatry. 2010;81(5):541–6. doi:10.1136/jnnp.2008.171066.
Bennett DA, Schneider JA, Wilson RS, Bienias JL, Arnold SE. Neurofibrillary tangles mediate the association of amyloid load with clinical Alzheimer disease and level of cognitive function. Arch Neurol. 2004;61(3):378–84. doi:10.1001/archneur.61.3.378.
Carmichael O, Schwarz C, Drucker D, Fletcher E, Harvey D, Beckett L, et al. Longitudinal changes in white matter disease and cognition in the first year of the Alzheimer disease neuroimaging initiative. Arch Neurol. 2010;67(11):1370–8. doi:10.1001/archneurol.2010.284.
Pasi M, Salvadori E, Poggesi A, Ciolli L, Del Bene A, Marini S, et al. White matter microstructural damage in small vessel disease is associated with Montreal Cognitive Assessment but not with mini mental state examination performances: Vascular Mild Cognitive Impairment Tuscany study. Stroke. 2015;46(1):262–4. doi:10.1161/STROKEAHA.114.007553.
Van Petten C, Plante E, Davidson PS, Kuo TY, Bajuscak L, Glisky EL. Memory and executive function in older adults: relationships with temporal and prefrontal gray matter volumes and white matter hyperintensities. Neuropsychologia. 2004;42(10):1313–35. doi:10.1016/j.neuropsychologia.2004.02.009.
Rolstad S, Berg AI, Eckerstrom C, Johansson B, Wallin A. Differential Impact of Neurofilament Light Subunit on Cognition and Functional Outcome in Memory Clinic Patients with and without Vascular Burden. J Alzheimers Dis. 2015;45(3):873–81. doi:10.3233/JAD-142694.
Lee JH, Kim SH, Kim GH, Seo SW, Park HK, Oh SJ, et al. Identification of pure subcortical vascular dementia using 11C-Pittsburgh compound B. Neurology. 2011;77(1):18–25. doi:10.1212/WNL.0b013e318221acee.
Acknowledgements
This study was jointly funded by the Canadian Stroke Network and the Heart and Stroke Foundation of Canada. Teresa Liu-Ambrose is a Canada Research Chair in Physical Activity, Mobility, and Cognitive Neuroscience, a Michael Smith Foundation for Health Research (MSFHR) Scholar, a Canadian Institutes of Health Research (CIHR) New Investigator, and a Heart and Stroke Foundation of Canada’s Henry J.M. Barnett Scholarship recipient. John Best is CIHR and Michael Smith Foundation for Health Research Post-Doctoral Fellow. Elizabeth Dao is a CIHR Doctoral Trainee. TRIUMF is gratefully acknowledged for PET tracer production.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
ED, G-YR H, VS, CJ, RT, KD, JRB, TLA contributed to study design, statistical analyses, data interpretation, and manuscript preparation. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Dao, E., Hsiung, GY.R., Sossi, V. et al. Exploring the effects of coexisting amyloid in subcortical vascular cognitive impairment. BMC Neurol 15, 197 (2015). https://doi.org/10.1186/s12883-015-0459-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-015-0459-1