Abstract
Background
Left ventricular mass (LVM) is an independent risk factor for the prediction of cardiac events. Its assessment is a clinically important diagnostic procedure in cardiology and may be performed by Computed Tomography (CT). The aim of this study was to assess the correlation between the cardiac left ventricular shell volume (LVShV) determined by postmortem Computed Tomography (PMCT) and the anatomic LVM obtained at autopsy and to calculate the myocardial tissue density.
Methods
A total of 109 deceased individuals were examined with a 64-slice CT scanner and LVShV was determined. At autopsy, the left ventricle was dissected and weighted. The correlation between LVShV and the anatomic LVM was analysed. Asymmetric left ventricular (LV) hypertrophy was recorded. Inter-observer variability was evaluated, and a density value for myocardial tissue was calculated.
Results
The mean age of the deceased was 55 ± 16 years, and 58% was men. We found 30 cases of asymmetric LV hypertrophy. A highly positive correlation existed between LVShV and anatomic LVM (r = 0.857; p < 0.0001), regardless of hypertrophy, asymmetric hypertrophy and gender. The mean difference in the inter-observer variability for LVShV assessment was - 4.4 ml (95% CI: -26.4; 17.6). A linear regression analysis was performed, resulting in a value of 1.265 g/ml for myocardial tissue density. Applying the hitherto used myocardial tissue density of 1.055 g/ml underestimated the anatomic LVM by 18.1% (p < 0.0001).
Conclusion
PMCT is a helpful tool for the assessment of LVM, and LVShV is highly correlated with LVM as assessed by subsequent autopsy. The correlation between the two was independent of gender, hypertrophy and LV asymmetric hypertrophy. We found a higher myocardial tissue density of 1.265 g/ml compared to previous studies. We show that PMCT combined with autopsy may contribute not only to anatomical but also clinical knowledge.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Left ventricular mass (LVM) is a prognostic factor in cardiac disease [1], and thus, assessment of LVM is used in the diagnosis and risk stratification of patients in clinical practice [2]. In addition, abnormal patterns of left ventricular (LV) size and shape have been found to have prognostic relevance [3,4,5]. Hypertrophy may occur in a specific region of the LV, asymmetric hypertrophy, regardless of the overall heart size [6, 7]. The most widespread tool for non-invasive measurements of the LVM is echocardiography [4, 7]. LVM determination by different imaging modalities is based on the LV shell volume (LVShV), which is the difference between the epicardial and endocardial volumes [4, 8]. The LVShV is subsequently converted to mass by multiplying it with the density of myocardial tissue [8, 9]. The clinically accepted value of myocardial tissue density is 1.055 g/ml [9,10,11,12,13,14]; however, there are different published values [6, 8, 15,16,17,18,19,20,21,22], cf. Table 1. LVM has been calculated based on Computed Tomography (CT)-angiography [10], magnetic resonance imaging (MRI) [23] and echocardiography [24], but the myocardial density has not been validated. The aim of this study was to assess the association between the LVShV determined by postmortem Computed Tomography (PMCT) and the anatomic LVM obtained at autopsy, and to calculate the myocardial tissue density.
Methods
Study population and design
The study population is part of a prospective nationwide autopsy-based Danish forensic study, SURVIVE-let the dead help the living, which focuses on deceased with mental illness [25]. The deceased were autopsied at the Section of Forensic Pathology at the Institute of Forensic Medicine, University of Copenhagen over an eleven-month period, from January 2014 to November 2014. The study group comprised 116 deceased that fulfilled the following inclusion criteria: individuals with a known or a suspected mental illness, and the intake of antipsychotic, antidepressive or anti-anxiety medication or a suspicion thereof. The exclusion criteria were putrefaction, suspicion of a criminal act, inadequate CT image quality for the analysis and failure to scan due to severe obesity. This led to the exclusion of seven individuals. After a medical inquest, the deceased underwent a whole-body PMCT. The scans occurred within 24 h prior to autopsy. At the autopsy (see details below), the sex, age, weight and height of the deceased were recorded, as were the size, shape and macroscopic changes of the heart. The project was approved by the Danish National Committee on Health Research Ethics (1377517).
Post mortem CT imaging protocol
Non-contrast PMCT imaging was performed using a 64-slice Multi Detector Computed Tomography scanner (MDCT) (Siemens Somatom definition syngo 2010A; Siemens medical solutions, Forchheim, Germany). The following scanning parameters were used: tube current time: 300 mAs, tube voltage: 120 kV, slice collimation: 32 × 0.6 mm and slice acquisition: 64 × 0.6 mm. The iterative reconstructed slice thickness was 1.5 mm using a soft tissue convolution kernel. All images were acquired with the deceased wrapped in an artefact-free body bag in a supine position with elevated arms (except for one due to a BMI of 50). The bodies were placed in the CT gantry and scanned from head to toe. After reconstruction of the raw data, the images were transferred to the local PACS server.
Imaging analysis
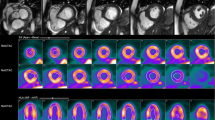
Assessment of the myocardial tissue was performed with commercial software (Vitrea 6.3, Vital Images, Inc., MN, USA). Imaging analysis was performed by individuals who were blinded to the autopsy results. The non-contrast PMCT data were reviewed in multiplanar reconstructions after adjusting the planes to a long-axis view of the heart. The LV myocardial tissue was segmented by manually tracing the endocardial and epicardial border for each long-axis slice and adding up the corresponding volumes from each slice (Fig. 1). We used normal cardiac window settings with a level = 200 Hounsfield Units (HUs) and width = 1000. Voxels corresponding to myocardial tissue were identified using mean threshold attenuation values of 50 ± 10 HUs to distinguish it from the LV blood pool (Fig. 1). The region of interest (ROI) for the segmentation of both LV myocardial tissue and the LV blood pool was defined at the height of the septum and the LV outlet by HUs. The ROI was set at a minimum of 1 cm2. Depending on the heart size, the number of manually traced slices varied from 70 to 100 in each case. Finally, based on the segmentation, the LVShV was calculated in millilitres and converted to mass, by multiplying it with 1.055 g/ml. Inter-observer variability was assessed in 25 randomly chosen individuals. Fifteen randomly chosen LV myocardial tissues were re-analysed using a different cardiac setting with level = 45 HU and width = 50 HU.
LV autopsy procedure
The autopsies were performed in accordance with the extended autopsy protocol of the SURVIVE study and the departments guidelines and were accredited by the Danish accreditation fund (DANAK). The length of the corpses were measured in the supine position from the top of the head (vertex) to the heel using an inelastic measuring tape. The heart was removed during the autopsy by preserving an adequate extension of the base and pulmonary vessels and dissected according to international standards detailed by Basso et al. [26]. After the removal of clotted blood, the whole heart was weighed. Dissection of the left ventricle was performed according to the method described by Bove et al. [27] with modifications; an incision was made in the posterior part of the left atrium following the atrioventricular groove to remove the atria from the ventricles. The ventricles were cut into transverse slices (short-axis direction). The right ventricle was separated from the septum and the left ventricle. The trabeculae encrusted in the septum and papillary muscles were preserved, and the hearts valves were removed. The epicardial fat was resected. The LV slices were blotted dry and separately weighed using an electronic scale (Mettler Toledo, ICS425, Glostrup, Denmark) with a 1-g precision.
The heart was recorded as being hypertrophic according to international forensic pathology standards and charts [28]. Anterior, lateral, posterior and septal wall thicknesses were measured at the level of the midventricular transversal slice. Papillary muscles were excluded from this measurement. Asymmetric LV hypertrophy was defined as biggest heart wall (millimetres) > 1.3*thinnest heart wall (millimetres) [7].
Statistical analyses
Data analysis was performed using the SPSS statistical software package (IBM Corp. IBM SPSS Statistics for Windows, Version 24, USA). Data was presented as the mean ± standard deviation, and a p-value of < 0.05 was considered statistically significant. Data distribution was tested with the Ancova/ linear regression test. Bland-Altman analysis was used to assess the re-analysis of LVShV and the degree of inter-observer variability. Scatterplots were used to illustrate the level of agreement and linearity between the CT obtained LVShV and the anatomic LVM as well as asymmetric LV hypertrophy. The degree of correlation was determined by Pearson’s correlation coefficient. The association between the CT-obtained LVShV and the anatomic LVM, with and without adjustment for gender, was assessed by linear regression analysis. A density factor was calculated by linear regression analyses, forcing the slope through origo (as done in comparable studies) [7, 8].
Results
Data were collected from a total study population of 109 deceased, comprising 46 females (42%) and 63 males (58%). The age and body weight distributions are detailed in Table 2. The deceased were autopsied at a mean time (± 1 SD) of 44 ± 16 h (range 29–150 h) after the declaration of death.
Left ventricular mass and LVShV
The results for anatomic LVM, LV wall thickness and LVShV are given in Table 2. There were 36 hypertrophic hearts, (25 men and 11 women) based on total heart weight. Thirty cases had asymmetric LV hypertrophy (19 men and 11 women) of which thirteen had hypertrophic hearts (total weight).
Overall, the CT-determined LVShV was highly correlated with the anatomic LVM (Pearson r = 0.857, p < 0.0001), also allowing us to assume linearity. Significant correlation was also found when the cohort was stratified by the presence of asymmetric LV hypertrophy (Fig. 2, Table 3) and by gender (Table 3). The inter-observer mean difference in LVShV assessment by CT was - 4.4 ml (95% CI: -26.4; 17.6). The mean HUs value of the ROI was 47 ± 7 in the segmentation of myocardial tissue and 68 ± 13 in the LV blood pool. A linear regression equation was calculated for each gender (Table 4) and for the genders combined (Fig. 3, Table 4). Linear regression analyses were also performed by forcing the line of regression through the origo for each gender (Table 4) and for the genders combined (Fig. 3, Table 4). The differences between the models based on gender were negligible. Forcing the line of regression through the origo resulted in the following estimated model: LVM = LVShV*1.265 g/ml, with 1.265 g/ml as the myocardial tissue density. The R2 values and residual standard error are presented in Table 4. Hypertrophic hearts based on total heart weight did not alter the myocardial tissue density compared to non-hypertrophic hearts (data not shown). Using the hitherto clinically accepted myocardial tissue density of 1.055 g/ml, the anatomic LVM was underestimated by 18.1% (95% CI = 29.9–40.0 g), p < 0.0001, (Fig. 3, Table 5). The mean difference in LVShV assessment by CT with the different settings in 15 randomly chosen LV myocardial tissues was - 19.4 ml (95% CI: -65.3; 25.5), p > 0.5.
Regression equations lines for LVM by LVShV. The lines are for genders combined (with the constant of 42.36). CT_vol represents the CT determined LVShV and the autopsy mass represents the anatomic LVM. The plot also shows the underestimation of the anatomic LVM when applying the clinically used myocardial tissue density of 1.055g/ml
Discussion
As expected, our data showed a highly positive correlation between the CT-determined LVShV and the anatomic LVM; also when stratifying by gender and when focusing on cases with hypertrophy and asymmetric LV hypertrophy. We then performed linear regression analyses with LVShV as the explanatory variable and LVM as the dependent variable. Stratification by gender showed no differences. Potentially, the resultant regression equation (genders combined) could thus be used for calculating LVM when LVShV has been determined. Traditionally, clinical volume-to-mass calculations use only a density factor, i.e. the volume is simply multiplied by a density factor [8, 9]. This is in line with a theoretical approach to a density factor: zero volume equals zero mass. Earlier attempts at establishing a myocardial density factor have therefore, more or less explicitly, assumed that a volume-to-mass regression must go through origo [7, 12, 24], hence resulting in a simple factor, and not in a regression equation with both a factor and a constant. We therefore performed new linear regression analyses, but this time forcing the line of regression through the origo. Again, differences by gender were negligible, thus allowing us to propose the resultant slope for the combined genders, 1.265 g/ml, as the myocardial tissue density. This density value is based on CT-determined LVShV and the actual weight of the anatomic LVM obtained at autopsy. When we compared this new myocardial tissue density value with the hitherto used value in the clinical setting of 1.055 g/ml (6–15), we found that the latter value significantly underestimated the anatomic LVM.
Indeed, the assumed density of myocardial tissue has varied over time, e.g., 1.029, 1.03, 1.04 and 1.055 g/ml, not least because of differing techniques in determining the density, e.g., by immersing cardiac muscle tissue or hearts in water (Archimedes principle) [14, 20, 21], different image modalities and different animal species [12, 17, 29,30,31,32] (cf. Table 1).
Echocardiography is the most widespread tool used for the quantification of LVM [7, 8], CT- angiography is often used for LVM calculations [10] and cardiac MRI is often considered the gold standard for LVM assessment [23, 33]. Although not often used, non-contrast CT can also be used for information in LV size in the clinical setting [34]. In this large study of recently deceased individuals, we showed that the use of non-contrast PMCT for the determination of LVShV is a useful tool and has a satisfactory repeatability due to the fact that a clear distinction between the HUs of myocardial tissue and LV blood pool without active circulation could be made. However, these CT settings were optimized for contrast-based studies. Changing the CT settings in 15 randomly chosen cases showed an overall, but negligible and non-significant (p > 0.5), decrease in LVShV (mean difference − 19.4 ml). We did find that the image quality improved in some cases using these different settings (n = 7/15), as a more clear-cut distinction between the blood-pool and the myocardium was achieved. However, in other cases a lot of noise was introduced, so we find that the majority of the scans were in fact better analysed with the original settings.
Several studies have presented normal reference values for LVM based on CT-angiography [10, 11, 15], echocardiography [8, 24] and MRI [23, 33] and thus it is reasonable to develop modality-specific reference values. However, regardless of the imaging modality used to obtain the LVShV, all shell volumes are converted to mass by multiplying it with the myocardial tissue density [8], with 1.055 g/ml being the most commonly used density. To our knowledge, this study is the first to calculate the human myocardial density factor using non-contrast CT based LVShV and LVM obtained at autopsy. This may explain why our value differs from other proposed values. Since our value is higher, this means that a given LVShV will result in a higher LVM, and will be most pronounced for higher and potentially pathological LVShV, which may be of interest for clinicians and warrants further studies.
Although it is currently not fully accepted clinically to use the LVM as a regular test for patients [3], the exact CT measurements and accurate values for myocardial tissue density can lead to important therapeutic opportunities concerning diagnosis, treatment and prognostics. If the hitherto used density value is substituted with our value, this could have implications for the reference values as it will move some patients to higher LVMs indicating abnormal LVM. If one continues with the hitherto used density value, there will be no problem in using the reference intervals, but to the best of our knowledge, this would mean that the recorded LVM is not the real LVM.
Study limitations
The following study limitations need to be addressed. This study included 73 non-hypertrophic hearts, but in order to develop LVM reference values based on the density, a bigger study population would be preferable. We did not take into consideration the status of ischaemic heart disease, fat infiltration or LV fibrosis and how this potentially could affect the size and shape of the left ventricle. The papillary muscles were included in the LVShV measurements. However, the impact of the inclusion or exclusion of papillary muscles on the assessment of LV function is negligible [15]. The scans were non-contrast scans, which in a clinical setting makes the differentiation between the LV blood pool and the LV myocardium difficult. However, non-contrast scans are possible in deceased individuals (cf. Fig. 1). We chose to perform the present study without contrast to avoid extravasation of contrast media in the examined deceased individuals and thereby omit a possible weight effect on the myocardium.
A study by Bai R et al. [20] has suggested a tendency of lower myocardial tissue density associated with pathological changes as oedema, none of our included cases had underwent putrefaction, as these were excluded. Therefore, we do assume that post mortal changes did not have any impact on the myocardial tissue density calculation. In vivo, the myocardium consist of intra-myocardial blood-volume. Postmortem, this volume may change, e.g., postmortem extravasation or, conversely, fluid accumulation from leaking and decomposing endocardial structures. Such changes are small and usually only become pronounced with extended postmortem intervals [35]. The deceased individuals in this study were kept at reduced temperature and autopsied rather quickly after declaration of death. Morphological observations as well as quantitative results suggest that elements of the blood are resistant to autolytic effects [36]. Overall, this leads us to assume that no significant organ volumetric changes took place. Water displacement was not performed in this study. There are several factors to take into consideration when performing water displacement measurements/techniques on cadaver hearts. Although it works accurately with solid objects, biological tissue is by its nature permeable and may be compressed or distended, and it may be fixed or unfixed. Given that we wanted to investigate CT-derived volume measures, as this is what is used clinically, we hence chose to base our volumes on this method. Boundaries are sensitive to threshold and windowing. We used a HU threshold for myocardial tissue of 50 ± 10, and 1 mm slice thickness for CT evaluations. The CT settings used for this study are optimized for contrast-based studies, and a different cardiac window settings could result in different myocardial volume. Also, different thresholds may apply for epicardial and endocardial borders and partial volume effects may be important. Due to the relatively close HU values of the blood pool and the myocardium, the myocardium may have been overestimated in some cases and underestimated in other cases.
Finally, our calculation of a new value for myocardial density is made performing a linear regression on the LVM and LVShV values of our study population. Thus, theoretically, we cannot be sure that very small hearts or LV masses below 96 g will conform to the linear model. This can probably only be investigated by also applying our method to a subadult study population. However, we note that all other analyses on myocardial tissue density were also constrained or even more limited. We would also note that when comparing with the hitherto-used value for myocardial density the differences are most pronounced for bigger hearts, so even if our new value has not been tested on very small hearts, any differences might be assumed minor.
Conclusion
The unique access to both PMCT scans and autopsy measurements allowed us to assess the correlation between LVShV and the anatomic LVM; the analysis was also possible based on gender and LV asymmetric hypertrophy. Our regression models determined only very small differences when stratified by gender and negligible differences when forcing the regression through the origo, which allowed us to determine a myocardial density at 1.265 g/ml. Applying the hitherto used myocardial tissue density value (1.055 g/ml) significantly underestimated the LVM. Our proposed new value is the result of post-mortem CT for volume determination, followed by post-mortem dissection for obtaining LV weight. We argue that this allows for a more precise determination of these two basic parameters, but obviously, we are aware that post-mortem anatomy may not be directly translational to clinical studies. Several LVM reference value tables have been produced using myocardial tissue density value of 1.055 g/ml, thus continuing to use this value when converting from LVShV to LVM will not have immediate clinical implications. However, we do think that our study calls for critical evaluation of especially high LVMs and how this value is obtained.
Abbreviations
- CT:
-
Computed Tomography
- DANAK:
-
Danish Accreditation fund
- HUs:
-
Hounsfield Units
- LV:
-
Left Ventricular
- LVM:
-
Left Ventricular Mass
- LVShV:
-
Left ventricular shell volume
- MDCT:
-
Multi Detector Computer Tomography
- MRI:
-
Magnetic Resonance Imaging
- PMCT:
-
Post Mortem Computed Tomography
- ROI:
-
Region of Interest
References
Hoang K, Zhao Y, Gardin JM, Carnethon M, Mukamal K, Yanez D, et al. LV mass as a predictor of CVD events in older adults with and without metabolic syndrome and diabetes. JACC Cardiovasc Imaging. 2015;8:1007–15. https://doi.org/10.1016/j.jcmg.2015.04.019.
Armstrong AC, Gidding S, Gjesdal O, Wu C, Bluemke DA, Lima JAC. LV mass assessed by echocardiography and CMR, cardiovascular outcomes, and medical practice. JACC Cardiovasc Imaging. 2012;5:837–48. https://doi.org/10.1016/j.jcmg.2012.06.003.
Litwin SE. Cardiac “Morphomics.”. JACC Cardiovasc Imaging. 2015;8:1016–8. https://doi.org/10.1016/j.jcmg.2015.06.008.
Celebi AS, Yalcin H, Yalcin F. Current cardiac imaging techniques for detection of left ventricular mass. Cardiovasc Ultrasound. 2010;8:19.
Udelson JE. Left ventricular shape. JACC: Heart Failure. 2017;5:179–81. https://doi.org/10.1016/j.jchf.2017.01.005.
Emanuel R, Marcomichelakis J, Withers R, O’Brien K. Asymmetric septal hypertrophy and hypertrophic cardiomyopathy. Br Heart J. 1983;49:309.
Losi M-A, Nistri S, Galderisi M, Betocchi S, Cecchi F, Olivotto I, et al. Echocardiography in patients with hypertrophic cardiomyopathy: usefulness of old and new techniques in the diagnosis and pathophysiological assessment. Cardiovasc Ultrasound. 2010;8:7.
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography’s guidelines and standards committee and the chamber quantification writing group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18:1440–63. https://doi.org/10.1016/j.echo.2005.10.005.
Fuchs A, Kühl JT, Lønborg J, Engstrøm T, Vejlstrup N, Køber L, et al. Automated assessment of heart chamber volumes and function in patients with previous myocardial infarction using multidetector computed tomography. Journal of Cardiovascular Computed Tomography. 2012;6:325–34. https://doi.org/10.1016/j.jcct.2012.01.006.
Fuchs A, Mejdahl MR, Kühl JT, Stisen ZR, Nilsson EJP, Køber LV, et al. Normal values of left ventricular mass and cardiac chamber volumes assessed by 320-detector computed tomography angiography in the Copenhagen general population study. Eur Heart J Cardiovasc Imaging. 2016;17:1009–17. https://doi.org/10.1093/ehjci/jev337.
Hindsø L, Fuchs A, Kühl JT, Nilsson EJP, Sigvardsen PE, Køber L, et al. Normal values of regional left ventricular myocardial thickness, mass and distribution-assessed by 320-detector computed tomography angiography in the Copenhagen general population study. Int J Card Imaging. 2017;33:421–9. https://doi.org/10.1007/s10554-016-1015-9.
Devereux RB, Alonso DR, Lutas EM, Gottlieb GJ, Campo E, Sachs I, et al. Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol. 1986;57:450–8.
Jackowski C, Schweitzer W, Thali M, Yen K, Aghayev E, Sonnenschein M, et al. Virtopsy: postmortem imaging of the human heart in situ using MSCT and MRI. Forensic Sci Int. 2005;149:11–23. https://doi.org/10.1016/j.forsciint.2004.05.019.
Masshoff W, Scheidt D, Reimers HF. Quantitative Bestimmung des Fett-und Myokardgewebes im Leichenherzen. Virchows Arch. 1967;342:184–9.
Stolzmann P, Scheffel H, Leschka S, Schertler T, Frauenfelder T, Kaufmann PA, et al. Reference values for quantitative left ventricular and left atrial measurements in cardiac computed tomography. Eur Radiol. 2008;18:1625–34. https://doi.org/10.1007/s00330-008-0939-4.
Lakatta EG, Mitchell JH, Pomerance A, Rowe GG. Human aging: changes in structure and function. J Am Coll Cardiol. 1987;10:42A–7A.
Reichek N, Devereux RB. Left ventricular hypertrophy: relationship of anatomic, echocardiographic and electrocardiographic findings. Circulation. 1981;63:1391–8. https://doi.org/10.1161/01.CIR.63.6.1391.
Snyder WS, Cook MJ, Nasset ES, Karhausen LR, Howells GP. Tipton IH. Report of the Task Group on Reference Man. n.d.:112–7.
Bardeen CR. Determination of the size of the heart by means of the x-rays. Dev Dyn. 1918;23:423–87.
Bai R, Yu X, Wang D, Lv J, Xu G, Lai X. The densities of visceral organs and the extent of pathologic changes. Am J Forensic Med Pathol. 2009;30:148–51. https://doi.org/10.1097/PAF.0b013e3181875ab2.
Friedman CE. Heart volume, myocardial volume and total capacity of the heart cavities in certain chronic heart diseases; a clinic, roentgenologic and patho-anatomic investigation of the problem of cardiac hypertrophy and dilatation and amount of residual blood of the heart. Acta Medica Scand Suppl. 1951;257:1–100.
de la Grandmaison GL, Clairand I, Durigon M. Organ weight in 684 adult autopsies: new tables for a Caucasoid population. Forensic Sci Int. 2001;119:149–54.
Gandy SJ, Waugh SA, Nicholas RS, Simpson HJ, Milne W, Houston JG. Comparison of the reproducibility of quantitative cardiac left ventricular assessments in healthy volunteers using different MRI scanners: a multicenter simulation. J Magn Reson Imaging. 2008;28:359–65. https://doi.org/10.1002/jmri.21401.
Takeuchi M, Nishikage T, Mor-Avi V, Sugeng L, Weinert L, Nakai H, et al. Measurement of left ventricular mass by real-time three-dimensional echocardiography: validation against magnetic resonance and comparison with two-dimensional and m-mode measurements. J Am Soc Echocardiogr. 2008;21:1001–5. https://doi.org/10.1016/j.echo.2008.07.008.
Banner J. SURVIVE: let the dead help the living—an autopsy-based cohort study for mapping risk markers of death among those with severe mental illnesses. Scandinavian journal of forensic science n.d.; 24/2018:7–17. https://doi.org/10.2478/sjfs-2018-0002.
Basso C, Burke M, Fornes P, Gallagher PJ, De Gouveia RH, Sheppard M, et al. Guidelines for autopsy investigation of sudden cardiac death. Pathologica. 2010;102:391–404.
Bove KE, Rowlands DT, Scott RC. Observations on the assessment of cardiac hypertrophy utilizing a chamber partition technique. Circulation. 1966;33:558–68.
Lucena J, Garcia-Pavia P, Pulpon LA. Clinico-pathological atlas of cardiovascular diseases. vol. 2015. Springer International Publishing, Switzerland. 362 pages. page 210-215. ISBN 13:978-3319111452.
Schiller NB, Skiôldebrand CG, Schiller EJ, Mavroudis CC, Silverman NH, Rahimtoola SH, et al. Canine left ventricular mass estimation by two-dimensional echocardiography. Circulation. 1983;68:210–6.
Manning WJ, Wei JY, Fossel ET, Burstein D. Measurement of left ventricular mass in rats using electrocardiogram-gated magnetic resonance imaging. Am J Phys Heart Circ Phys. 1990;258:H1181–6.
Wyatt HL, Heng MK, Meerbaum S, Hestenes JD, Cobo JM, Davidson RM, et al. Cross-sectional echocardiography. I. Analysis of mathematic models for quantifying mass of the left ventricle in dogs. Circulation. 1979;60:1104–13.
Ward SR, Lieber RL. Density and hydration of fresh and fixed human skeletal muscle. J Biomech. 2005;38:2317–20. https://doi.org/10.1016/j.jbiomech.2004.10.001.
Juergens KU, Fischbach R. Left ventricular function studied with MDCT. Eur Radiol. 2006;16:342–57. https://doi.org/10.1007/s00330-005-2888-5.
Dykun I, Mahabadi AA, Lehmann N, Bauer M, Moebus S, Jöckel K-H, et al. Left ventricle size quantification using non-contrast-enhanced cardiac computed tomography--association with cardiovascular risk factors and coronary artery calcium score in the general population: the Heinz Nixdorf recall study. Acta Radiol. 2015;56:933–42. https://doi.org/10.1177/0284185114542996.
Zilg B, Thelander G, Giebe B, Druid H. Postmortem blood sampling-comparison of drug concentrations at different sample sites. Forensic Sci Int. 2017;278:296–303. https://doi.org/10.1016/j.forsciint.2017.07.006.
Penttilä A, Laiho K. Autolytic changes in blood cells of human cadavers. II. Morphological studies. Forensic Sci Int. 1981;17:121–32.
Acknowledgments
The authors thank the physicians, morgue technicians, laboratory assistants and medical students for their assistance in the SURVIVE project as well as statistician Kyle Raymond for his statistical knowledge and assistance.
Funding
This project was sponsored by the Department of Forensic Medicine, University of Copenhagen (Unit number 361100).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
AGG, AF, CJ KFK, NL and JB contributed to the design of the study. AGG contributed to the literature search and the image analysis. AF contributed to literature search, the inter-observer imaging analysis and as Vitrea advisor. AGG and CJ contributed to the CT-scan protocol. AF, KFK and RM contributed as cardiology advisors. JB and CJ contributed as forensic pathology advisors. NL contributed as statistical advisor. AGG conducted the LVM excision at autopsy. AGG contributed to the manuscript writing and all drafts. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The next of kin gave informed written or verbal consents that was approved by the National Committee on Danish Health Research Ethics who also approved (20-01-2014) the research protocol (version 2.0 number 1377517).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Gheorghe, A.G., Fuchs, A., Jacobsen, C. et al. Cardiac left ventricular myocardial tissue density, evaluated by computed tomography and autopsy. BMC Med Imaging 19, 29 (2019). https://doi.org/10.1186/s12880-019-0326-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12880-019-0326-4