Abstract
Background
Human orthopneumovirus (HOPV) or respiratory syncytial virus (RSV) is one of the important causes of acute respiratory infections (ARIs) during the cold months of the year worldwide. Many countries have reported an absence of ARIs due to HOPV during the winter of 2020–2021 associated with preventive measures to reduce the spread of SARS-CoV2. However, with the reduction of COVID-19 public health restrictions and the absence of immunity in the community due to the lack of exposure in the previous season, many countries had a delayed HOPV outbreak. Here we reported the impact of COVID-19 on the changing pattern of HOPV infection in Iran.
Methods
Throat and nasopharyngeal swab samples were collected from patients (children and adults) with ARIs and sent to the Iran National Influenza Center. After RNA extraction, Real time RT-PCR was performed for HOPV detection.
Results
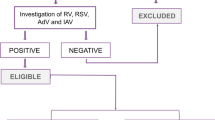
In 260 samples collected from patients with ARIs in three different groups, which included children in March 2021, pilgrims in July 2022, and outpatients during November and December 2022, no HOPV was detected in any group.
Conclusions
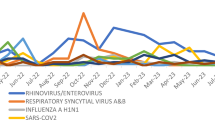
The lack of HOPV activity in Iran during the winter of 2020–2021 and then the resurgence in spring 2022 and again the absence of activity in summer and autumn 2022 was extraordinary in the HOPV epidemiology, and probably due to the implementation of public health non-pharmaceutical interventions to reduce the spread of SARS-CoV2. Although it is not possible to keep such restrictions, similar methods can be taken to control outbreaks caused by respiratory viruses.
Similar content being viewed by others
Introduction
Human orthopneumovirus (HOPV) or human respiratory syncytial virus (HRSV) belongs to the genus Orthopneumovirus within the family Pneumoviridae and is able to cause severe disease in different groups, including premature newborns, children, the elderly, and immunocompromised people [1]. The human orthopneumovirus genome consists of a 15.2 kb negative-sense single-stranded RNA containing 10 genes that encode 11 proteins. Based on the variations found in the G gene sequence its strains can be divided into two subtypes A and B [2]. Until 2019, HOPV had predicted seasonality patterns with annual epidemics in winter months, especially in the northern hemisphere [3]. In Iran, HOPV activity peaks during February and March every year.
The emergence of severe acute respiratory syndrome coronavirus 2 (SARS-CoV2) and the subsequent coronavirus disease 2019 (COVID-19) pandemic caused considerable changes in the circulation of respiratory viruses with a dramatic absence of HOPV and influenza activity [4].
Human orthopneumovirus is transmitted via respiratory droplets and indirect contact with contaminated surfaces like SARS-CoV2. During the COVID-19 pandemic, preventive measures were widely implemented to decrease the spread of SARS-CoV2, including physical distancing, facemasks, stay-at-home orders, work, schools, and border closures, and handwashing. All these measures have the potential to prevent the transmission of HOPV and influenza [5].
As public health non-pharmaceutical mitigation measures were reduced during the spring of 2021, an extraordinary resurgence of HOPV cases occurred worldwide [6]. The reasons for this unusual resurgence of RSV cases were uncertain, but it might be due to the lack of HOPV immunity because of the extended absence of virus circulation in the community [7]. During the COVID-19 pandemic, study about the effect of the pandemic on the changing pattern of other respiratory viruses and subsequent resurgence has increased worldwide.
Here, we studied HOPV circulation during the COVID-19 pandemic in different intervals and performed laboratory test for HPOV detection to show the impact of COVID-19 on the circulation pattern of HOPV in Iran.
Methods
Study population
Throat and nasopharyngeal swab samples were collected from different groups with acute respiratory infections (ARIs) for HOPV detection and the samples were sent to the Iranian National Influenza Center (NIC), Virology Department, School of Public Health, Tehran University of Medical Sciences. The groups were: children under 5 years of age who attended Children Medical Center, Tehran, Iran in March 2021, returning pilgrims from Mecca in July 2022, and outpatients from hospitals in different cities in autumn 2022. We obtained ethical clearance (including permission to study the children) from Tehran University of Medical Sciences Medical Ethics, ref no: IR.TUMS.REC.1399.306. Written informed consent was obtained from all patients as the samples were taken for influenza surveillance via the Ministry of Health and Education.
Nucleic acid extraction and real-time PCR
Ribonucleic acid (RNA) was extracted from all specimens by High Pure Viral Nucleic Acid kit (Roche, Germany) according to the manufacturer’s instructions. Detection of HOPV was performed using one-step real-time RT-PCR with the Biotech Rabbit kit (Japan). The nucleocapsid gene was selected for the amplification of HOPV RNA using RSV N forward primer: 5’-GCTAAAAGAAATGGGAGAGG-3’; RSV N reverse primer: 5’-TAATCACGGCTGTAAGAC C-3’ and RSV N probe: 5’-FAM AGCTCCAGAATACAGGCATGACTC-TAMRA-3’ [8]. RNA (5 µl) was added to a 20 µl PCR mixture containing 12.5 µl of mastermix, 1 µl of enzymemix, 1 µl of each primer (10 pmol), 0.5 µl probe (10 pmol) and, 4 µl ddH2O. The reaction consisted of 20 min at 50 °C and 2 min at 95 °C, followed by 40 cycles of amplification, including 30s at 95 °C and 30s at 54 °C.
Results
In total, 260 samples were taken from patients in all three groups but HOPV was not detected in any sample.
The first studied group was the children less than 5 years old hospitalized with ARIs at Children Medical Center in March 2021. Of 122 children, 69 (56.5%) were male, and 53 (43.5%) were female. We divided patients into two age groups: less than 1 year old and 1–5 years old. 37 (30.5%) children were younger than 1 year old and 85 (69.5%) were 1–5 years old. The most common clinical manifestations of patients were cough, nausea, diarrhea, and fever. Among 122 patients, no HOPV was detected.
The second studied group was the pilgrims who returned from Mecca after the pilgrimage, which was held after two years of closure because of the COVID-19 pandemic. All returning pilgrims to Tehran International Airport in July 2022, were screened for respiratory symptoms and signs, of whom 26 had at least cough, sore throat, and fever. The age range was 27–73 with a median of 53 years. The male to female ratio was 1. Human orthopneumovirus was not detected in these 26 pilgrims.
The third studied group was the adult outpatients with ARIs from different cities in Iran. Their samples were sent to NIC for screening of different respiratory viruses from November to December 2022. In all 112 samples, 62 (55.4%) were female and 50 (44.5%) were male. Human orthopneumovirus was not detected in these samples. It should be mentioned that public health interventions undertaken during the COVID-19 pandemic have led to a low circulation of HPOV cases.
Discussion
Before the COVID-19 pandemic, HOPV was an important cause of ARIs in children (under 5) and the elderly and was a significant burden on the public health system of Iran. Two systematic reviews about the prevalence of HOPV in Iran have been conducted; one covered from the 1996–2013 period and the other reviewed from 1996 to 2016. They showed the presence of HOPV 18.7% and 18% respectively during the cold months of the year (November-March) [9, 10]. Between January to March 2017, HOPV was detected in 2.75% of military trainees with ARIs in Tehran, Iran [11]. Another study in Tehran, Iran, between January and March 2018, and December 2018 to May 2019 among hospitalized or outpatient children younger than 2 years of age showed a prevalence of 35.92% HOPV with a peak in March followed by February [12].
The SARS-CoV2 pandemic has significantly changed the epidemiology of seasonal respiratory infections worldwide, for instance, HOPV epidemics during the cold months have disappeared during 2020 and 2021 [13]. In Iran, a study between March and May 2021 in children younger than 5 years old showed the absence of HOPV circulation during the COVID-19 pandemic which indicated the impact of a pandemic on HOPV circulation in Iran as shown in different studies worldwide [14]. In current study, HOPV was not detected in 122 hospitalized children in March 2021, 26 pilgrims in July 2022, and 112 outpatients in autumn 2022. Our findings were comparable with the reports from other countries that have reported decreased HOPV circulation in the first winter following the COVID-19 pandemic. For example, an analysis of HOPV activity in United States during 2020–2021, reported by the Centers for Disease Control and Prevention (CDC) revealed that circulation of HOPV decreased in early 2020 [15]. Similarly, in Australia, HOPV activity decreased 98% during the winter of 2020 [16]. Also findings were reported from Japan where the number of HOPV cases during January–December 2020 were reduced by almost 85% compared to 2014–2019 [17]. A study in Korea reported a 19% reduction in positive rates of HOPV during the COVID-19 pandemic [18]. A Chinese study showed the absence of HOPV circulation in 2020 [19]. A research study from Italy reported a significant reduction in HOPV circulation following the appearance of SARS-CoV2 in 2020–2021 [20, 21]. Another study from Finland reported that HOPV circulation had the pattern of previous years in the first 12 weeks of 2020 but then reduced, because of nationwide restrictions [15].
As mentioned above, more than one year after the COVID-19 pandemic, the circulation of HOPV was reduced in different countries. Potentially such reduction could cause a general increase in susceptibility to infections because of the possible reduction in immunity in society, which might lead to large epidemics of HOPV. Surveillance data from several countries have reported delayed HOPV outbreaks resulting from easing the restrictions and restarting social activities [22]. In Australia, the inter-seasonal resurgence of HOPV in children after the relaxation of COVID-19 restriction measures was reported [16]. A study in Israel showed a temporal move of the HOPV epidemic during 2021 among hospitalized children in Ashod, with a lack of HOPV circulation during the autumn/winter of 2020/21, and a delayed resurgence of cases from May to June 2021 [23]. Surveillance data from different countries including the Netherlands, France, Iceland, and Japan have shown a delay in the onset of the HOPV epidemic after easing the COVID-19 pandemic measures [22, 24]. In a study in Iran from December 2020 to March 2021 among 197 hospitalized patients suspected of COVID-19 with the age range of 45–68 years HOPV was detected in four (2.03%) patients [25]. In April 2022, another study in Iran, reported a delayed resurgence of HOPV in a small population of children in the southwest of Iran, after the lack of HOPV circulation from the beginning of the COVID-19 pandemic [6]. As shown here the change in HOPV seasonality reveals similar findings reported elsewhere. One of the limitations of our study is that the period and number of samples taken were not sufficient to provide more complete and precise epidemiological information on RSV during COVID-19 in Iran.
There have been limited data about the prevalence of HOPV in adults during the COVID-19 pandemic because most studies focused on children. As stated our study included a good number of adults to understand the impact of the COVID-19 pandemic on HOPV activity. As noted above HOPV was not detected in all three groups, emphasizing that the pandemic has impacted the circulation of HOPV in all populations. Our study confirms the change in HOPV seasonality indicated in other studies worldwide and we reiterate the significance of control measures, behavioral changes, and surveillance systems during a pandemic.
Data Availability
All data generated or analyzed during this study are included in this article.
Abbreviations
- RSV:
-
Respiratory syncytial virus
- SARS-CoV2:
-
Severe acute respiratory syndrome coronavirus 2
- COVID-19:
-
Coronavirus disease 2019
- NIC:
-
National Influenza Center
- ARIs:
-
Acute respiratory infections
- RNA:
-
Ribonucleic acid
- HOPV:
-
Human orthopneumovirus
References
Li Y, Wang X, Blau DM, Caballero MT, Feikin DR, Gill CJ, et al. Global, regional, and national disease burden estimates of acute lower respiratory infections due to respiratory syncytial virus in children younger than 5 years in 2019: a systematic analysis. Lancet. 2022;399(10340):2047–64. https://doi.org/10.1016/S0140-6736(22)00478-0.
Yu J-M, Fu Y-H, Peng X-L, Zheng Y-P, He J-SJSR. Genetic Divers Mol Evol Hum Respiratory Syncytial Virus B. 2021;11(1):12941.
Bardsley M, Morbey RA, Hughes HE, Beck CR, Watson CH, Zhao H, et al. Epidemiology of respiratory syncytial virus in children younger than 5 years in England during the COVID-19 pandemic, measured by laboratory, clinical, and syndromic surveillance: a retrospective observational study. Lancet Infect Dis. 2023;23(1):56–66. https://doi.org/10.1016/S1473-3099(22)00525-4.
Falsey AR, Cameron A, Branche AR, Walsh EE. Perturbations in respiratory Syncytial Virus Activity during the SARS-CoV-2 pandemic. J Infect Dis. 2022;227(1):83–6. https://doi.org/10.1093/infdis/jiac434.
Reicherz F, Xu RY, Abu-Raya B, Majdoubi A, Michalski C, Golding L, et al. Waning immunity against respiratory Syncytial Virus during the Coronavirus Disease 2019 Pandemic. J Infect Dis. 2022;226(12):2064–8. https://doi.org/10.1093/infdis/jiac192.
Mohebi L, Karami H, Mirsalehi N, Ardestani NH, Yavarian J, Mard-Soltani M, et al. A delayed resurgence of respiratory syncytial virus (RSV) during the COVID-19 pandemic: an unpredictable outbreak in a small proportion of children in the Southwest of Iran, April 2022. J Med Virol. 2022;94(12):5802–7. https://doi.org/10.1002/jmv.28065.
Hernández-Rivas L, Pedraz T, Calvo C, Juan IS, José Mellado M, Robustillo A. Respiratory syncytial virus outbreak during the covid-19 pandemic. How has it changed? [published online ahead of print, 2021 Dec 22]. Enferm Infecc Microbiol Clin. 2021. https://doi.org/10.1016/j.eimc.2021.12.003.
Malekshahi SS et al. Inhibition of respiratory syncytial virus replication by simultaneous targeting of mRNA and genomic RNA using dual-targeting siRNAs. 2016. 58: p. 767–75.
Salimi V, Tavakoli-Yaraki M, Yavarian J, Bont L, Mokhtari-Azad T. Prevalence of human respiratory syncytial virus circulating in Iran. J Infect Public Health. 2016;9(2):125–35. https://doi.org/10.1016/j.jiph.2015.05.005.
Faghihloo E, Yavarian J, Jandaghi NZ, Shadab A, Azad TM. Genotype circulation pattern of human respiratory syncytial virus in Iran. Infect Genet Evol. 2014;22:130–3. https://doi.org/10.1016/j.meegid.2014.01.009.
Niya MHK, Jeda AS, Tavakoli A, Sohani H, Tameshkel FS, Panahi M, et al. Molecular epidemiology of human respiratory syncytial virus (HRSV) in iranian military trainees with acute respiratory symptoms in 2017. Iran J Microbiol. 2020;12(5):495–502. https://doi.org/10.18502/ijm.v12i5.4612.
Tavakoli F, Izadi A, Yavarian J, Sharifi-Zarchi A, Salimi V, Mokhtari-Azad T. Determination of genetic characterization and circulation pattern of respiratory syncytial virus (RSV) in children with a respiratory infection, Tehran, Iran, during 2018–2019. Virus Res. 2021;305:198564. https://doi.org/10.1016/j.virusres.2021.198564.
Stera G, Pierantoni L, Masetti R, Leardini D, Biagi C, Buonsenso D, et al. Impact of SARS-CoV-2 pandemic on Bronchiolitis Hospitalizations: the experience of an italian Tertiary Center. Child (Basel). 2021;8(7):556. https://doi.org/10.3390/children8070556. Published 2021 Jun 28.
Letafati A, Aghamirmohammadali FS, Rahimi-Foroushani A, Hasani SA, Mokhtari-Azad T, Yavarian J. No human respiratory syncytial virus but SARS-CoV-2 found in children under 5 years old referred to Children Medical Center in 2021, Tehran, Iran. J Med Virol. 2022;94(7):3096–100. https://doi.org/10.1002/jmv.27685.
Kuitunen I, Artama M, Mäkelä L, Backman K, Heiskanen-Kosma T, Renko M. Effect of Social Distancing due to the COVID-19 pandemic on the incidence of viral respiratory tract infections in children in Finland during Early 2020. Pediatr Infect Dis J. 2020;39(12):e423–7. https://doi.org/10.1097/INF.0000000000002845.
Foley DA, Yeoh DK, Minney-Smith CA, Martin AC, Mace AO, Sikazwe CT, et al. The Interseasonal resurgence of respiratory Syncytial Virus in Australian Children following the reduction of Coronavirus Disease 2019-Related Public Health Measures. Clin Infect Dis. 2021;73(9):e2829–30. https://doi.org/10.1093/cid/ciaa1906.
Wagatsuma K, Koolhof IS, Shobugawa Y, Saito R. Decreased human respiratory syncytial virus activity during the COVID-19 pandemic in Japan: an ecological time-series analysis. BMC Infect Dis. 2021;21(1):734. https://doi.org/10.1186/s12879-021-06461-5. Published 2021 Aug 3.
Kim J-H, Roh YH, Ahn JG, Kim MY, Huh K, Jung J, et al. Respiratory syncytial virus and influenza epidemics disappearance in Korea during the 2020–2021 season of COVID-19. Int J Infect Dis. 2021;110:29–35. https://doi.org/10.1016/j.ijid.2021.07.005.
Yang Q, Xiao X, Gu X, Liang D, Cao T, Mou J, et al. Surveillance of common respiratory infections during the COVID-19 pandemic demonstrates the preventive efficacy of non-pharmaceutical interventions. Int J Infect Dis. 2021;105:442–7.
Calderaro A, De Conto F, Buttrini M, Piccolo G, Montecchini S, Maccari C, et al. Human respiratory viruses, including SARS-CoV-2, circulating in the winter season 2019–2020 in Parma, Northern Italy. Int J Infect Dis. 2021;102:79–84. https://doi.org/10.1016/j.ijid.2020.09.1473.
Curatola A, Lazzareschi I, Bersani G, Covino M, Gatto A, Chiaretti A. Impact of COVID-19 outbreak in acute bronchiolitis: lesson from a tertiary italian Emergency Department. Pediatr Pulmonol. 2021;56(8):2484–8. https://doi.org/10.1002/ppul.25442.
Garg I, Shekhar R, Sheikh AB, Pal S. Impact of COVID-19 on the changing patterns of respiratory Syncytial Virus Infections. Infect Dis Rep. 2022;14(4):558–68. https://doi.org/10.3390/idr14040059. Published 2022 Jul 24.
Weinberger Opek M, Yeshayahu Y, Glatman-Freedman A, Kaufman Z, Sorek N, Brosh-Nissimov T. Delayed respiratory syncytial virus epidemic in children after relaxation of COVID-19 physical distancing measures, Ashdod, Israel, 2021. Euro Surveill. 2021;26(29):2100706. https://doi.org/10.2807/1560-7917.ES.2021.26.29.2100706.
Ujiie M, Tsuzuki S, Nakamoto T, Iwamoto N. Resurgence of respiratory Syncytial Virus Infections during COVID-19 pandemic, Tokyo, Japan. Emerg Infect Dis. 2021;27(11):2969–70. https://doi.org/10.3201/eid2711.211565.
Veisi P, Shatizadeh Malekshahi S, Choobin H, Jabbari MR, Mohammadi Torbati P. Simultaneous detection of multiple respiratory viruses among SARS-CoV-2-Positive and negative patients by Multiplex TaqMan one-step real-time PCR. Jundishapur J Microbiol. 2022;15:1:e122090. https://doi.org/10.5812/jjm.122090.
Acknowledgements
We should say many thanks to the staff of the NIC located at the Virology Department, School of Public Health, Tehran University of Medical Sciences. We also should express our special thanks to the Ministry of Health of Iran for their support.
Funding
This study was supported by the School of Public Health, Tehran University of Medical Sciences under Grant No.1400-1‐99‐52190.
Author information
Authors and Affiliations
Contributions
Jila Yavarian: Writing the manuscript. Marziyeh Faraji-Zonouz: Methodology. Shirin Kalantari: Methodology. Sevrin Zadheidar: Investigation. Sara Saghafi: Methodology. Faezeh Tarpour: Data collection. Arash Letafati: Data collection. Nazanin-Zahra Shafiei-Jandaghi & Somayeh Shatizadeh Malekshahi: Data curation. Akram sadat Ahmadi: Editing. Talat Mokhtari-Azad: Supervision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
We obtained ethical clearance (including permission to study the children) from Tehran University of Medical Sciences Medical Ethics, ref no: IR.TUMS.REC.1399.306. Written informed consent was obtained from all patients as the samples were taken for influenza surveillance via the Ministry of Health and Education. All methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yavarian, J., Shatizadeh Malekshahi, S., Faraji-Zonouz, M. et al. Impact of COVID-19 on the changing pattern of human orthopneumovirus (respiratory syncytial virus) infection in Iran. BMC Infect Dis 23, 591 (2023). https://doi.org/10.1186/s12879-023-08588-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-023-08588-z