Abstract
Introduction
Respiratory tract infections (RTIs) stand out as the most frequent causes leading to visits to the emergency department and hospitalizations. This study aims to assess the types and prevalence of respiratory infections across two years following the end of the COVID-19 pandemic.
Methods
Patients presenting with an influenza-like illness (ILI) were tested using multiplex RT-PCR (QIAstat-Dx, Qiagen). The multiplexed RT- PCR test detects 21 respiratory viruses and bacteria.
Results
During the study period, PCR test was done on a total of 1,790 samples were tested, and 712 (40%) were positive for a total of 796 pathogens. The mean age (± SD) of the participants was 20.1 ± 28.4 years in 2022 and 21.9 ± 27.6 years in 2023. Among the detected pathogens, the most prevalent were Rhinovirus/Enterovirus 222 (12.4%), followed by RSV A&B (103 cases, 5.7%), and H1N1 Influenza (77 cases, 4.3%). Additionally, Influenza A/B constituted 172 (9.6%) while parainfluenza constituted (58, 3.2%). SARS-CoV-2 was identified in 3.97% of the samples. Over the two-year period, the monthly pattern of the identified pathogens exhibited fluctuations in the prevalence. Furthermore, variations were observed in the detected pathogens across different age groups.
Conclusion
In addition to adding significant knowledge to the field of respiratory viral infections, this study emphasizes the necessity of ongoing research and surveillance for the detection and characterization of respiratory viruses, particularly those with the potential for emergence. Such studies would also require setting up a strategy for genotyping and/or sequencing of viruses.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Respiratory tract infections (RTIs) are among the most prevalent illnesses that cause a high number of visits and hospital stays, and they have a significant morbidity and mortality rate, particularly in younger children and the elderly [1]. Rhinovirus type A and C, as well as respiratory syncytial virus (RSV), have been linked to chronic lung illnesses such asthma [2,3,4]. The prevalence of various RTIs tends to follow distinct seasonal trends [5, 6]. Seasons with the highest prevalence of viral infections are typically the fall and winter because temperature and humidity, for example, have an effect on the stability and rates of transmission of respiratory viruses as well as the host’s immune responses to RTIs [7, 8]. However, a key element in the propagation of viruses is the patterns of human behavior, which affects the frequency of interaction between susceptible hosts and infected persons. The COVID-19 pandemic significantly reduced contact rates due to social interactions, mask wearing, and hand hygiene [9, 10]. During the pandemic, these non-pharmaceutical interventions (NPIs) greatly reduced the transmission of viruses, such as SARS-CoV-2, RSV, and influenza A/B [9, 10].
Following the easing of pandemic-related limitations and decreased adherence to NPIs, a growing and persistent wave of non-COVID-19 RTIs in children has been seen since June 2021 [11,12,13,14]. Variations in the respiratory virus population in communities have been associated with viral interference and virus-virus interactions [15]. Variation in adherence to NPIs at different levels such as the community, regional, and national levels, varied especially after lifting the COVID-19 restrictions. These differences may have affected how respiratory pathogens disseminate within any given community. Although several European countries reported an increase in RTIs in 2022, it is unclear if coinfection frequency and clinical significance changed from the pre-pandemic period [2]. There are limited data from Saudi Arabia about the pattern of RTIs and causative agents in the post-COVID-19 era [16]. In Saudi Arabia, the COVID-19 pandemic had caused 837,569 cases including 9,646 (1%) deaths. The country had four main waves: the first wave peaked in June 2020, the second wave peaked in June 2021, the third peaked in January 2022, and the fourth peaked in June 2022. There were differences in these waves in relation to the number of cases as well as the death rates [17,18,19]. The third wave coincided with the Omicron variant and had caused a large number of cases but a lower mortality [19, 20]. One study from Saudi Arabia showed a significantly lower number of RSV cases admitted in 2022 compared to 2019, and this was attributed to the application of non-pharmacologic interventions to reduce COVID-19 cases [16]. In the Middle East and North Africa (MENA) region, a systematic review showed higher number of RSV during the winter months from November to February [21]. The full picture of the pattern of the circulating pathogens causing RTIs in Saudi Arabia is sparse [22]. Most of the studies had specifically addressed the pattern among Pilgrims and the Middle East respiratory Syndrome Coronavirus (MERS-CoV). Other studies had addressed specific pathogens such as RSV and human respiratory syncytial virus. Thus, to enhance our understanding of the epidemiology of RTIs post-COVID-19, this study intends to look into the patterns of pathogens of RTIs from 2022 to 2023 in a hospital in Saudi Arbia.
2 Materials and methods
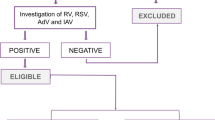
We conducted a retrospective cohort study in a hospital in Saudi Arabia, between January 2022 and November 2023. Patients presenting with an influenza-like illness (ILI) were tested using multiplex RT-PCR (QIAstat-Dx, Qiagen). The test was performed on swab samples from the upper respiratory tract (nasopharyngeal). The QIAstat-Dx Analyzer is a fully automatic diagnostic device and performs a multiplexed RT- PCR test for the detection of 21 respiratory viruses and bacteria. These pathogens are Mycoplasma pneumoniae, Chlamydophila pneumoniae, Bordetella pertussis, Influenza A, Influenza A subtype H1N1/2009, Influenza A subtype H1, Influenza A subtype H3, Influenza B, Parainfluenza virus 1, Parainfluenza virus 2, Parainfluenza virus 3, Parainfluenza virus 4, SARS-CoV-2, Coronavirus 229 E, Coronavirus HKU1, Coronavirus NL63, Coronavirus OC43, Adenovirus, RSV A/B, Human Metapneumovirus A/B, and Rhinovirus/Enterovirus, as described previously [23, 24]. The study included any patient who presented with ILI and was tested for the presence of respiratory pathogens. Confirmed cases were those who tested positive using real-time PCR. The study received approval from the institutional board (IRB).
Statistical Analysis: We classified participants with a positive PCR test into different age groups: infants and toddlers (< 2 years), early childhood (2–5 years), middle childhood (6–11 years), early adolescence (12–18 years), young adulthood (19–44 years), middle adulthood (45–64 years), and older adulthood (65 years and older) [25]. We examined the rate of occurrence of different pathogens in each group to allow for a comprehensive understanding of the impact of respiratory pathogens across the lifespan. We summarized the characteristics of continuous and categorical data as numbers and percentages. Statistical analysis was performed using the JASP [Computer software] (Version 0.18.1). A P value of ≤ 0.05 was considered as statistically significance.
3 Results
During the study period, a total of 1790 patients with ILI were tested and 712 (40%) were positive, yielding a total of 796 pathogens. The overall mean age (± SD) was 20.1 ± 28.4 years (Table 1) with a male to female ratio of 1.1:1. The analysis of the samples collected over a two-year period revealed a diverse range of respiratory pathogens. Among these, the most prevalent pathogen was Rhinovirus/Enterovirus detected in 222 samples (12.4%). This was followed by RSV A&B found in 103 samples (5.7%), and Influenza A H1N1 detected in 77 samples (4.3%) (Table 2). Influenza A/B constituted 172 (9.6%) and parainfluenza accounted for 58 samples (3.2%). Notably, SARS-CoV-2 was identified as the fourth leading pathogen present in 71 (4%) during this period. Several other respiratory agents were detected at relatively low frequencies, including Mycoplasma pneumoniae, and Legionella pneumophila.
The monthly pattern of the top 8 identified pathogens exhibited variations in the number of cases throughout the study period (Fig. 1). For instance, the detection levels of Rhinovirus/Enterovirus varied, with higher counts in September and December 2022. RSV A&B reached its peak in October 2022 and November 2023. SARS-CoV-2 cases were notably higher in June and December 2022 as well as in March and May 2023. Influenza A H3 exhibited an increase in June 2022 and November 2023, while, Influenza H1N1 had its peak in June 2022 and November 2023.
This study aimed to assess the prevalence of respiratory viruses across different age groups (Table 3). The top three pathogens showed variation across the different age ranges. For infants and toddlers (0–2 years), the most prevalent pathogens were RSV with 40 cases (27.6%), followed by influenza B with 12 cases (7.5%), and Rhinovirus with 34 cases (23.4%). In early childhood (3–5 years), RSV was still prominent with 20 cases (12.5%), followed by influenza A with 5 cases (3.1%) and Rhinovirus with 37 cases (23.1%). Among middle childhood (6–12 years), Rhinovirus was the most common with 19 cases (27.9%), followed by RSV with 6 cases (8.8%), and Influenza H1N1 with 10 cases (14.7%). Regarding early adolescence (13-17 years), Rhinovirus was the predominant pathogen, accounting for 15 cases (38.5%). Influenza A and H1N1 followed closely with 5 cases each, representing 12.8% of the cases for both pathogens. In young adulthood (18–25 years), Rhinovirus remained prevalent with 26 cases (23.4%), followed by SARS-CoV-2 with 19 cases (16.8%), and Influenza H1N1 with 20 cases (18.0%). In middle adulthood (26–64 years), Rhinovirus still ranked first with 16 cases (21.1%), while SARS-CoV-2 had 7 cases (4.8%), and H1N1 had 9 cases (11.8%). Lastly, among older adults (65 + years), Rhinovirus was the most common with 30 cases (26.5%), followed by RSV with 9 cases (8.0%), and Influenza H1N1 with 16 cases (14.2%). The mean age group across the different pathogens was significantly different (P < 0.001, in ANOVA analysis) (Table 3). When comparing the mean age of patients in 2022 and 2023 , there was no statistical difference. The mean age inn 2022 was 21.9 ± 27.6, while in 2023, it was 25.7 ± 28.5 (Fig. 2).
4 Discussion
In this study, we investigated the detection of various respiratory pathogens over a two-year period following the lifting of restrictions and the declaration that COVID-19 is no longer a global public health emergency. The study offers several important insights from an epidemiological standpoint. The diversity of respiratory pathogens detected is notable. Rhinovirus/Enterovirus, RSV A&B, and Influenza A viruses were the most commonly identified pathogens, which aligns with global respiratory infection trends. However, the continued presence of SARS-CoV-2 underscores the evolving nature of respiratory infections and the need for ongoing surveillance and indicates that this virus will reach an adaptation within the human beings [26].
The monthly breakdown reveals distinct patterns in pathogen occurrences. This aligns with established knowledge in epidemiology that respiratory viruses often display seasonal peaks, typically during colder months [8, 27]. Understanding these temporal trends is crucial for preparedness and targeted interventions during high-transmission periods.
In this study, we used a multiplex PCR to assess multiple respiratory pathogens over a two-year period. The simultaneous evaluation of various pathogens and their temporal dynamics provides a holistic view of respiratory illness epidemiology within the studied population. Additionally, the detection of less common viruses (e.g., bocavirus, coronaviruses) showcases the breadth of the pathogen spectrum and highlights their low occurrence yet relevant presence. The study showed different respiratory pathogens detected among 1790 samples over two years. The prevalence of Rhinovirus/Enterovirus, RSV A&B, and Influenza A stands out as the most prominent pathogens. Influenza A/B constituted 172 (9.6%) and parainfluenza constituted (58, 3.2%). The Kingdom of Saudi Arabia established the Integrated Influenza Sentinel Surveillance System (IISS), its most sophisticated surveillance system to date, in 2022, in response to the COVID-19 pandemic and the effective execution of the National Influenza Surveillance Development Plan. There are 100 sites in the IISS (30 hospitals and 70 primary care clinics). It combines quick COVID-19 testing, training for healthcare providers, and on-site molecular testing for influenza and respiratory syncytial virus. For subtyping, genetic sequencing, and sharing, all test results are forwarded to the Public Health Laboratory at the Public Health Authority [28]. Various studies indicated that the detection of influenza among patients with ILI ranged from 3 to 12% in Saudi Arabia [29].
Bocavirus infection predominantly affected toddlers, while Adenovirus infection was more common in early childhood. In a previous study from Saudi Arabia, Bocavirus was seen in 1.6% of patients and most of them were diagnosed in the winter [30] and another study showed a prevalence of 11.2% in pediatric patients [31]. However, this virus was not detected among pilgrims [32]. The most common detected pathogen in this study was Rhinovirus/Enterovirus. Few studies in Saudi Arabia showed that Rhinovirus/Enterovirus affects children < 5 years of age and those less than two years [33, 34]. Of particular interest is the occurrence of RSV and Enterovirus/Rhinovirus in 2022–2023. The COVID-19 pandemic had a significant impact on RSV cases, leading to a decrease in the number of RSV cases and hospital admissions [16]. This decrease can be attributed to the implementation of infection control measures, similar to the decline observed in influenza cases in certain regions [16]. The impact on RSV activity during the pandemic has exhibited geographical variability, with certain countries reporting low transmission levels. The impact of the pandemic on RSV activity has varied across different geographical areas. While some countries experienced low transmission during the pandemic, there has been an increase in RSV cases in subsequent years. The absence of seasonal exposure to RSV during the pandemic may lead to a decline in population immunity, potentially increasing the risk of severe RSV infection. In a study from Egypt, a total of 530 patients under the age of 16 with ILI symptoms were enrolled and 49.1% of them tested positive for one or more of the three tested viruses, including 25.3% for influenza, 20.9% for RSV, and 2.6% for RSV-influenza coinfection [35].
The results of this study shed light on the prevalence of respiratory viruses in various age groups. The fact that rhinovirus is consistently ranked among the most detected pathogens in a variety of age groups indicates the important role that this pathogen plays. Rhinoviruses can cause a sore throat, cough, and nasal congestion, among other respiratory symptoms, and as a major cause of the common cold [36]. Previous studies support the high prevalence of RSV in infants and toddlers. RSV can cause severe respiratory illness, especially in infants, and is a leading cause of lower respiratory tract infections in young children. The results highlight the necessity of focused preventive initiatives, like immunization and better hygiene practices, within this vulnerable age group to reduce the burden of RSV infections [37]. The presence of influenza viruses across multiple age groups underscores the ongoing significance of influenza as a respiratory pathogen. Influenza infections can cause seasonal outbreaks and have the potential for severe complications, particularly among older adults and individuals with underlying health conditions. Vaccination remains a key strategy for reducing the impact of influenza, and efforts should be made to enhance vaccination coverage, especially in high-risk populations [38, 39]. The detection of SARS-CoV-2 in various age groups reflects the ongoing global pandemic and its impact on respiratory health. The higher prevalence of SARS-CoV-2 in young adulthood and middle adulthood highlights the susceptibility of these age groups to infection. It emphasizes the importance of continued adherence to preventive measures, such as vaccination, mask-wearing, and physical distancing, to mitigate the spread of COVID-19 and its potential long-term consequences [40].
The monthly occurrences of respiratory pathogens over the study period mirrors well-established seasonal patterns observed in respiratory virus activity. For instance, peaks in Rhinovirus/Enterovirus and RSV A&B detections in the colder months, particularly during late fall and winter. Similar findings were found in earlier Saudi Arabian research, which showed that most RSV infections happened in the winter [31, 41, 42]. These results were corroborated by a systematic review that concentrated on the Middle East and North Africa (MENA) region and showed that RSV was more common in the winter, specifically from November to February [21]. The observed variations in pathogen detections month-to-month underscore the complex interplay of factors such as climate, population immunity, behavior, and viral transmissibility.
The findings of this study hold implications for public health interventions. Understanding seasonal trends helps in optimizing vaccination strategies, preparing healthcare systems for potential surges, and implementing targeted preventive measures during high-risk periods. Moreover, the emergence of novel viruses like SARS-CoV-2 underscores the necessity for adaptable surveillance systems and rapid response strategies. In addition, study offers a valuable resource for further epidemiological studies. Longitudinal data on multiple respiratory pathogens can facilitate predictive modeling, epidemiological forecasting, and in-depth analyses of transmission dynamics, contributing to the advancement of public health strategies.
However, it is important to note few limitations of the study. Results might not be generally applicable because they are particular to the single center’s population and circumstances. The small sample size may impact the study’s statistical power and capacity to identify uncommon infections. Since the study was conducted over a two-year duration, seasonal variations in respiratory pathogen may not be fully captured. Certain cases or demographics that are more likely to seek treatment or surveillance at that specific center may be the focus of bias in the study. It is possible that some pathogens’ evolution, emergence, or shifts in prevalence during the study period were not fully recorded. External factors, like public health initiatives or community interventions, could have an impact on the study’s findings by influencing the spread of different pathogens.
In conclusion, the study showed continued emergence of RSV and Enterovirus/Rhinovirus as the predominant pathogens in 2022 and 2023. However, several other pathogens were detected at relatively low frequencies, including Influenza A, Mycoplasma pneumoniae, and Legionella pneumophila. The study emphasizes the importance of continuous surveillance, especially during seasonal shifts, to monitor the prevalence and circulation patterns of respiratory pathogens. The insights gleaned from such data can inform targeted public health strategies, including vaccination campaigns, infection control measures, and resource allocation, aimed at mitigating the burden of respiratory infections. Further studies are needed to be prospective and multi-centers and to have better studies concerning the detection and characterization of respiratory viruses, particularly those with the potential for emergence. Such studies would also require setting up a strategy for genotyping and/or sequencing of viruses with potential for emergence such as influenza and SARS-CoV-2.
Data Availability
Available upon a reasonable request.
References
De Conto F, Conversano F, Medici MC, Ferraglia F, Pinardi F, Arcangeletti MC, et al. Epidemiology of human respiratory viruses in children with acute respiratory tract infection in a 3-year hospital-based survey in Northern Italy. Diagn Microbiol Infect Dis. 2019;94:260–7. https://doi.org/10.1016/j.diagmicrobio.2019.01.008.
Raita Y, Camargo CA, Bochkov YA, Celedón JC, Gern JE, Mansbach JM, et al. Integrated-Omics endotyping of infants with rhinovirus bronchiolitis and risk of childhood asthma. J Allergy Clin Immunol. 2021;147:2108–17. https://doi.org/10.1016/j.jaci.2020.11.002.
Kotaniemi-Syrjänen A, Vainionpää R, Reijonen TM, Waris M, Korhonen K, Korppi M. Rhinovirus-induced wheezing in infancy - the first sign of childhood asthma? J Allergy Clin Immunol. 2003;111:66–71. https://doi.org/10.1067/mai.2003.33.
Bergroth E, Aakula M, Elenius V, Remes S, Piippo-Savolainen E, Korppi M, et al. Rhinovirus type in severe bronchiolitis and the development of Asthma. J Allergy Clin Immunol Pract. 2020;8:588–595e4. https://doi.org/10.1016/j.jaip.2019.08.043.
Wrotek A, Czajkowska M, Jackowska T. Seasonality of respiratory Syncytial Virus hospitalization. Adv Exp Med Biol. 2020;1279:93–100. https://doi.org/10.1007/5584_2020_503.
Chadha M, Hirve S, Bancej C, Barr I, Baumeister E, Caetano B, et al. Human respiratory syncytial virus and influenza seasonality patterns—early findings from the WHO global respiratory syncytial virus surveillance. Influenza Other Respi Viruses. 2020;14:638–46. https://doi.org/10.1111/irv.12726.
Zhu G, Xu D, Zhang Y, Wang T, Zhang L, Gu W, et al. Epidemiological characteristics of four common respiratory viral infections in children. Virol J. 2021;18. https://doi.org/10.1186/s12985-020-01475-y.
Moriyama M, Hugentobler WJ, Iwasaki A. Annual review of virology seasonality of respiratory viral infections. Annu Rev Virol. 2020;7:83–101. https://doi.org/10.1146/annurev-virology-012420-022445.
Haapanen M, Renko M, Artama M, Kuitunen I. The impact of the lockdown and the re-opening of schools and day cares on the epidemiology of SARS-CoV-2 and other respiratory infections in children – A nationwide register study in Finland. EClinicalMedicine. 2021;34. https://doi.org/10.1016/j.eclinm.2021.100807.
Terliesner N, Unterwalder N, Edelmann A, Corman V, Knaust A, Rosenfeld L, et al. Viral infections in hospitalized children in Germany during the COVID-19 pandemic: Association with non-pharmaceutical interventions. Front Pediatr. 2022;10. https://doi.org/10.3389/fped.2022.935483.
Hodjat P, Christensen PA, Subedi S, Bernard DW, Olsen RJ, Long SW. The reemergence of Seasonal Respiratory viruses in Houston, Texas, after relaxing COVID-19 restrictions. Microbiol Spectr. 2021;9. https://doi.org/10.1128/spectrum.00430-21.
Eden JS, Sikazwe C, Xie R, Deng YM, Sullivan SG, Michie A, et al. Off-season RSV epidemics in Australia after easing of COVID-19 restrictions. Nat Commun. 2022;13. https://doi.org/10.1038/s41467-022-30485-3.
Maison N, Peck A, Illi S, Meyer-Buehn M, von Mutius E, Hübner J, et al. The rising of old foes: impact of lockdown periods on non-SARS-CoV-2 viral respiratory and gastrointestinal infections. Infection. 2022;50:519–24. https://doi.org/10.1007/s15010-022-01756-4.
Delestrain C, Danis K, Hau I, Behillil S, Billard MN, Krajten L, et al. Impact of COVID-19 social distancing on viral infection in France: a delayed outbreak of RSV. Pediatr Pulmonol. 2021;56:3669–73. https://doi.org/10.1002/ppul.25644.
Piret J, Boivin G. Viral interference between respiratory viruses. Emerg Infect Dis. 2022;28:273–81. https://doi.org/10.3201/eid2802.211727.
AlBahrani S, Al otaibi TO, Alqahtani J, AlZahrani SJ, Sharbini DA, AlMuyidi FW, et al. The impact of non-pharmacologic interventions on respiratory Syncytial Virus hospitalization during the COVID-19 pandemic: a retrospective study from Saudi Arabia. J Infect Public Health. 2023;17. https://doi.org/10.1016/j.jiph.2023.11.010.
AlBahrani S, AlAhmadi N, Hamdan S, Elsheikh N, Osman A, Almuthen S, et al. Clinical presentation and outcome of hospitalized patients with COVID-19 in the first and second waves in Saudi Arabia. Int J Infect Dis. 2022;118:104–8. https://doi.org/10.1016/j.ijid.2022.02.048.
AlJishi JM, Alhajjaj AH, Alkhabbaz FL, AlAbduljabar TH, Alsaif A, Alsaif H, et al. Clinical characteristics of asymptomatic and symptomatic COVID-19 patients in the Eastern Province of Saudi Arabia. J Infect Public Health. 2021;14:6–11. https://doi.org/10.1016/j.jiph.2020.11.002.
AlBahrani S, AlBarrak A, Al-Musawi T, AlGubaisi NA, Almalki M, Hakami FH, et al. COVID-19 vaccine had a significant positive impact on patients with SARS-COV-2 during the third (Omicron) wave in Saudi Arabia. J Infect Public Health. 2022;15:1169–74. https://doi.org/10.1016/j.jiph.2022.09.005.
Aldawish S, Abusaris R, Almohammadi E, Althobiti F, Albarrag A. Effectiveness of COVID-19 vaccines against ICU admission during Omicron surge in Saudi Arabia: a nationwide retrospective cohort study. BMC Infect Dis. 2023;23. https://doi.org/10.1186/s12879-023-08686-y.
Yassine HM, Sohail MU, Younes N, Nasrallah GK. Systematic review of the respiratory syncytial virus (RSV) prevalence, genotype distribution, and seasonality in children from the Middle East and North Africa (MENA) region. Microorganisms. 2020;8. https://doi.org/10.3390/microorganisms8050713.
Farrag MA, Hamed ME, Amer HM, Almajhdi FN. Epidemiology of respiratory viruses in Saudi Arabia: toward a complete picture. Arch Virol. 2019;164:1981–96. https://doi.org/10.1007/s00705-019-04300-2.
Ishikane M, Unoki-Kubota H, Moriya A, Kutsuna S, Ando H, Kaburagi Y, et al. Evaluation of the QIAstat-Dx Respiratory SARS-CoV-2 panel, a rapid multiplex PCR method for the diagnosis of COVID-19. J Infect Chemother. 2022;28:729–34. https://doi.org/10.1016/j.jiac.2022.02.004.
Lebourgeois S, Storto A, Gout B, Le Hingrat Q, Ardila Tjader G, Cerdan M del. Performance evaluation of the QIAstat-Dx® respiratory SARS-CoV-2 panel. Int J Infect Dis. 2021;107:179–81. https://doi.org/10.1016/j.ijid.2021.04.066.
Lindemann EA, Chen ES, Wang Y, Skube SJ, Melton GB. Representation of Social History Factors Across Age Groups: A Topic Analysis of Free-Text Social Documentation. AMIA. Annu Symp Proceedings AMIA Symp. 2017;2017:1169–78.
Al-Tawfiq JA, Chu DT, Hoang VT, Memish ZA. From Pandemicity to endemicity: the Journey of SARS-CoV-2. J Epidemiol Glob Health. 2022;12:147–9. https://doi.org/10.1007/s44197-022-00046-4.
Neumann G, Kawaoka Y. Seasonality of influenza and other respiratory viruses. EMBO Mol Med. 2022;14. https://doi.org/10.15252/EMMM.202115352.
World Health Organization(WHO). A Saudi Arabian journey in influenza surveillance 2022. https://www.who.int/news/item/13-12-2022-a-saudi-arabian-journey-in-influenza-surveillance (accessed February 12, 2024).
Soudani S, Mafi A, Al Mayahi Z, Al Balushi S, Dbaibo G, Al Awaidy S, et al. A systematic review of Influenza Epidemiology and Surveillance in the Eastern Mediterranean and North African Region. Infect Dis Ther. 2022;11:15–52. https://doi.org/10.1007/s40121-021-00534-3.
Alkhalf H, Almutairi AR, Almutairi A, Almutairi RK, AlGhnam S, Aljohani S, et al. Prevalence and clinical characterization of Bocavirus Infection in a Specialized Children’s hospital in Saudi Arabia. Cureus. 2022;14. https://doi.org/10.7759/cureus.22127.
Eifan SA, Hanif A, Aljohani SM, Atif M. Respiratory Tract Viral Infections and Coinfections Identified by Anyplex™ II RV16 Detection Kit in Pediatric Patients at a Riyadh Tertiary Care Hospital. Biomed Res Int. 2017;2017. https://doi.org/10.1155/2017/1928795.
Alsayed SM, Alandijany TA, El-Kafrawy SA, Hassan AM, Bajrai LH, Faizo AA, et al. Pattern of respiratory viruses among pilgrims during 2019 Hajj season who sought healthcare due to severe respiratory symptoms. Pathogens. 2021;10. https://doi.org/10.3390/pathogens10030315.
Al-Ayed MS, Asaad AM, Qureshi MA, Ameen MS. Viral etiology of respiratory infections in children in southwestern Saudi Arabia using multiplex reverse-transcriptase polymerase chain reaction. Saudi Med J. 2014;35:1348–53.
Al-Shehri A, Saleh A, Khan MA, Dandachi I, Aljabr W. Prevalence of common respiratory viruses in children at a Tertiary Care Hospital in Saudi Arabia. Pediatr Infect Dis J. 2023;42:E312–5. https://doi.org/10.1097/INF.0000000000003943.
Kandeel A, Fahim M, Deghedy O, Roshdy WH, Khalifa MK, Shesheny R, El, et al. Resurgence of influenza and respiratory syncytial virus in Egypt following two years of decline during the COVID-19 pandemic: outpatient clinic survey of infants and children, October 2022. BMC Public Health. 2023;23. https://doi.org/10.1186/s12889-023-15880-9.
Jartti T, Gern E. Rhinovirus-Associated Wheeze during Infancy and Asthma Development. Curr Respir Med Rev. 2011;7:160–6. https://doi.org/10.2174/157339811795589423.
Borchers AT, Chang C, Gershwin ME, Gershwin LJ. Respiratory syncytial virus - A comprehensive review. Clin Rev Allergy Immunol. 2013;45:331–79. https://doi.org/10.1007/s12016-013-8368-9.
Paules CI, Marston HD, Fauci AS. Coronavirus infections-more than just the Common Cold. JAMA - J Am Med Assoc. 2020;323:707–8. https://doi.org/10.1001/jama.2020.0757.
Chung JR, Rolfes MA, Flannery B, Prasad P, O’Halloran A, Garg S, et al. Effects of Influenza Vaccination in the United States during the 2018–2019 influenza season. Clin Infect Dis. 2020;71:E368–76. https://doi.org/10.1093/cid/ciz1244.
Link-Gelles R, Ciesla AA, Mak J, Miller JD, Silk BJ, Lambrou AS, et al. Early estimates of updated 2023–2024 (Monovalent XBB.1.5) COVID-19 vaccine effectiveness against symptomatic SARS-CoV-2 infection attributable to co-circulating Omicron variants among Immunocompetent adults - increasing Community Access to Testing Program. MMWR Morb Mortal Wkly Rep. 2024;73:77–83. https://doi.org/10.15585/mmwr.mm7304a2.
Amer HM, Alshaman MS, Farrag MA, Hamad ME, Alsaadi MM, Almajhdi FN. Epidemiology of 11 respiratory RNA viruses in a cohort of hospitalized children in Riyadh, Saudi Arabia. J Med Virol. 2016;88:1086–91. https://doi.org/10.1002/jmv.24435.
Albogami SS, Alotaibi MR, Alsahli SA, Masuadi E, Alshaalan M. Seasonal variations of respiratory viruses detected from children with respiratory tract infections in Riyadh, Saudi Arabia. J Infect Public Health. 2018;11:183–6. https://doi.org/10.1016/j.jiph.2017.06.001.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
All authors contributed to data collection and finalizing the manuscript. J.A.A: concept design, formal analsyis and finalizing the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was appproved by the IRB of the Armed Forces Hospitals Eastern Province (AFHER-IRB-2023-015).
Consent for publication
Not applicable.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
AlBahrani, S., AlZahrani, S.J., Al-Maqati, T.N. et al. Dynamic Patterns and Predominance of Respiratory Pathogens Post-COVID-19: Insights from a Two-Year Analysis. J Epidemiol Glob Health 14, 311–318 (2024). https://doi.org/10.1007/s44197-024-00213-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s44197-024-00213-9