Abstract
Background
There is a four-fold risk for hepatitis B infection among healthcare workers compared to the general population. Due to limited access to diagnosis and treatment of hepatitis B in many resource-constrained settings, there is a real risk that only few healthcare workers with viral hepatitis may get screened or diagnosed and treated. Studies on hepatitis B vaccination among healthcare workers in developing countries are sparse and this bodes ill for intervention and support. The aim of the study was to estimate the prevalence and explored the associated factors that predicted the uptake of the required, full dosage of hepatitis B vaccination among healthcare workers (HCWs) in five developing countries using nationally representative data.
Methods
We used recent datasets from the Demographic and Health Surveys Program’s Service Provision Assessment Survey. Descriptive summary statistics and logistic regressions were used to produce the results. Statistical significance was pegged at p < 0.05.
Results
The proportion of HCWs who received the required doses of hepatitis B vaccine in Afghanistan, Haiti, Malawi, Nepal, and Senegal were 69.1%, 11.3%, 15.4%, 46.5%, and 17.6%, respectively. Gender, occupational qualification, and years of education were significant correlates of receiving the required doses of hepatitis B among HCWs.
Conclusions
Given the increased risk of hepatitis B infection among healthcare workers, policymakers in developing countries should intensify education campaigns among HCWs and, perhaps, must take it a step further by making hepatitis B vaccination compulsory and a key requirement for employment, especially among those workers who regularly encounter bodily fluids of patients.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Over the past three decades, significant global health efforts have been made to control viral hepatitis [1, 2], including initiatives on blood safety, healthcare injection safety, infection control, harm reduction for intravenous drug users, and vaccination [3, 4]. There have been global policies by the World Health Organization (WHO) such as the Global Hepatitis Programmes (2011 and 2014) to improve public awareness and drastically reduce hepatitis infections [4]. Also, there was the 2016–2021 Global Health Sector Strategy on viral hepatitis in 2016 which aims to eliminate viral hepatitis by 2030 by reducing new infections by 90% and mortality by 65% [4, 5]. Despite these significant efforts, hepatitis B virus (HBV) infection continues as a serious public health concern [6, 7]. Globally, an estimated 237 million people live with chronic HBV with about 900,000 deaths [8]. The majority of the disease burden is in WHO African and Western Pacific Regions, affecting 6.1% and 6.2% of the adult populations respectively [5, 9]. Although preventable, HBV is transmitted mostly through mother-to-child during birth and delivery (vertical transmission), percutaneously or mucosal exposure to infected bodily fluids such as sexual intercourse with an infected partner, injection-drug use, needle injuries, and occupation-risk healthcare workers [HCWs] [10, 11].
Worldwide, millions of healthcare professionals work in healthcare institutions [10]. Due to the nature of their work, HCWs are more prone to HBV infections. There is a four-fold risk for HBV infection among HCWs compared to the general population [12, 13]. Studies in sub-Saharan Africa indicate that more than half a million of HCWs are infected with HBV infections annually [10, 11]. With over 5% of healthcare-related injections being unsafe [4], there is about 30% risk of getting HBV infection from a single needlestick injury compared to hepatitis C virus (3%) and HIV (0.3%) [11, 14]. The most effective and feasible means of preventing HBV infection are by avoiding exposure to infected bodily fluids, screening, and vaccination [3, 14, 15]. Screening links people to interventions to reduce transmission through risk behaviour counselling and hepatitis B vaccination. However, limited access to hepatitis B diagnosis and treatment in resource-constrained settings is challenging [7].
In 1982, a safe and effective vaccine that offers 90–100% protection against the HBV was discovered [16, 17]. Following this, hepatitis B vaccination continues to be a part of the WHO Extended Programme for Immunization [18]. This underlines the need for HCWs who are exposed to the HBV infection on daily bases to be vaccinated against the disease. Complete vaccination against HBV is achieved by a three-dose regimen administration, with the second and third doses given at 1 and 6 months after the initial dose, following which a test for hepatitis B surface antibody should be carried out 6–8 weeks after the final dose [14, 16]. In the event of low antibody levels, a booster dose should be given immediately to improve response, followed by a blood test in 6–8 weeks to check the response to the booster dose [14, 19]. According to the Centers for Disease Control and Prevention (CDC), all HCWs should receive the 3-dose vaccine regimen with an approximate protection rate of 30–55% after the first dose, 75% after the second dose, and > 90% after the third dose in adults aged ≤ 40 years [3, 20]. However, adherence to vaccinations in general is said to be poor among HCWs, especially in developing countries [11, 13, 21]. The estimated hepatitis B vaccination rate among HCWs range from 18 to 39% in developing countries compared to 67–79% for their counterparts in developed countries [10, 11, 22]. Previous studies have reported the type of profession, years of education, years of working experience, and gender among others as predictors of low hepatitis B vaccination uptake among HCWs [3, 10, 11, 23, 24].
Despite the critical nature of HBV infections among HCWs, there is paucity of literature on the uptake of hepatitis B vaccinations among HCWs in endemic countries such as Afghanistan, Haiti, Malawi, Nepal, and Senegal. Although data on specific endemicity of HBV in these countries is limited, the available statistics show an overall prevalence rate of 6.15%, 6.54%, 1.53% and 1.76% among injecting drug users, female sex workers, obstetric patients and blood donors respectively in Afghanistan alone [25, 26]. Also, Haiti is reported to be the only country in the Antimicrobial Resistance (AMR) that is highly endemic in HBV with a reported HBsAg prevalence > 7% [27]. Systematic reviews have reported a pooled prevalence of 8.1% among adults in Malawi and chronic HBV prevalence of ≥ 11% for Senegal with an estimated 85% of the Senegalese population reported to have experienced HBV infection [28, 29]. Senegal is therefore described as a hyperendemic country with regards to HBV. In Nepal, although the overall prevalence rate is reported to be low, a high prevalence rate (≥ 8%) has been reported by various studies among sub-groups within the population especially in the mountain regions [30].
A combined hepatitis B vaccine given at 6, 10, and 14 weeks of age as part of National Immunization Schedule were introduced in Nepal, Senegal, Malawi, Afghanistan, and Haiti in 2002 [31, 32], 2002 [33], 2004 [34], 2006 [35], and 2012 [36, 37] respectively. However, the birth dose was introduced only in 2014 in Afghanistan [35], while Senegal introduced the monovalent birth-dose vaccine in 2016 [34]. Yet, the Senegalese government lacks vaccination programme for high risk population such as HCWs [31, 32]. Contrary to the WHO recommendations, a birth dose of hepatitis B vaccine is not included or implemented in the present vaccination schedule in Haiti [36] and Malawi [33]. Although immunization of HCWs before they come into contact with patients at all levels is recommended by the Malawian Ministry of Health, there is inconsistent adherence to and enforcement of such recommendations [38]. The existing data provides an overview of overall prevalence without providing insights into specific important sub-groups such as health worker groups. Therefore, this study estimated the prevalence and explored the associated factors that predicted the uptake of the required, full dosage of hepatitis B vaccination among HCWs in these five developing countries using nationally representative data.
Methods
Study design and data source
In all, there were 13 developing countries who participated in the Service Provision Assessment (SPA) surveys under the Demographic and Health Survey (DHS) program. Only formal facilities are included in the SPA survey hence pharmacies and individual doctors’ offices are often excluded from the SPA. For the purposes of our study, we selected countries with recently conducted SPA surveys from 2013 up till now and having questions on hepatitis B screening for HCWs. The countries that met the criteria were Afghanistan (2018–2019), Haiti (2017–2018), Malawi (2013–2014), Nepal (2015), and Senegal (2019), and these SPA surveys were conducted by the countries’ respective national agencies with technical support from the Demographic and Health Surveys (DHS). Besides the standard DHS, the Service Provision Assessment survey is undertaken to evaluate the health system readiness to provide quality care, amongst others. The surveys used generic questionnaires to assess the availability of essential services and assessed the presence of standard facilities and equipment required to provide these essential services. These services included child welfare clinics, and immediate newborn care, maternal and child health, antenatal services, birth control, treatment for sexuality transmitted diseases, tuberculosis, malaria, and non-communicable diseases amongst other essential health care services. These generic questionnaires included “facility inventory questionnaire”, “health provider interview questionnaire”, “observation protocols for antenatal care, family planning, services for sick children, and normal obstetric delivery and immediate newborn care” and “exit Interview questionnaires for antenatal care and family planning clients and for caretakers of sick children whose consultations were observed”. The survey also assessed health system readiness to ensure infection prevention in the health environment. The healthcare facilities included governmental, private, and quasi-governmental facilities in both rural and urban areas. Along with data on health system preparedness, data on vaccination history of health care providers were obtained. The unit of measurement included both the health facility and individual health care providers.
Data collection and sample size
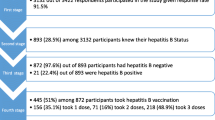
Computer-Assisted Personal Interviews (CAPI) were used to collect data from HCWs who were working in sampled healthcare facilities. For Afghanistan, the 1038 HCWs selected were all interviewed, representing 100% response rate [39]. For Haiti, 4461 HCWs were interviewed out of 4680; this represents 95.32% response rate [40]. For Malawi, the selected 2660.0 HCWs were all interviewed, representing 100% response rate [41]. For Nepal, 4057 HCWs were interviewed out of the selected sample of 4216; this represents 96.23% response rate [42]. For Senegal, 1353 HCWs were interviewed out of 1355; this represents 99.99% response rate [43]. The following demographic characteristics of the HCWs were collected: years of education, sex, and qualification. The following were the weighted analytic sample sizes for each of the countries included in the study: Afghanistan, N = 1038.0; Haiti, N = 4461.0; Malawi, N = 2660.0; Nepal, N = 4057.0; Senegal, N = 1353.0. There were no missing cases in the datasets.
Outcome and explanatory variables
The outcome variable is complete dosing of hepatitis B vaccination among healthcare providers. The HCWs were asked the following ‘Yes/No’ question to know their hepatitis B vaccination status: “Have you received any dose of Hepatitis B vaccine?” Those who answered “YES” were further asked the following to determine complete vaccination status: IF YES, how many doses have you received so far? The forgoing question has the following response scale: 1 dose, 2 doses, 3 or more doses. HCWs who had received at least 3 doses were classified as those who have received complete hepatitis B vaccination. Explanatory variables under investigation included gender, occupation, and years of training.
Data analysis
Data was analyzed using STATA version 14 software. Each of the selected countries was analyzed separately. Analysis was mainly in two stages. The first stage involved descriptive analysis during which weighted estimates of the outcome and associated 95% confidence intervals were provided. Weighting was done due to the unequal probability of inclusion of cases from certain subgroups in the DHS sample. All included health care facilities were selected from a sample frame of listed health care facilities stratified by facility type, regional location, and management type (i.e., public vs. private facilities). Hospital facilities are usually oversampled because of their relative numbers in each country. Sample weight is a function of the selection probability of health facility and the selection probability within the subgroup of the individual. Sample weights were normalized and estimated in six decimals but often presented in the DHS data without the decimals. Therefore, prior to applying the sample weights during analysis, the sample weight for each case was divided by 1,000,000. All weighting adjustments were done in STATA-14. Thus, sample weights were applied to adjust for representation and ensure accurate estimates of the outcome. Given that the outcome variable is binary, we used binary logistic regression to build the multivariable model showing estimates of the predictors of complete dosing of hepatitis B vaccination among healthcare providers. In the multivariable model, we reported odds ratios and its associated 95% confidence intervals.
Data availability
Data used for the present study is freely available after online request at https://dhsprogram.com/data/dataset_admin/index.cfm.
Ethical consideration
Ethical clearance to undertake the survey was granted by the respective national authorizing bodies. Informed consent was obtained from the health care providers prior to being interviewed. Owing to the use of secondary data, no further consents were sought.
Results
Demographic characteristics
The proportion of HCWs who received the required doses of hepatitis B vaccine in Afghanistan, Haiti, Malawi, Nepal, and Senegal were 69.1%, 11.3%, 15.4%, 46.5%, and 19.6%, respectively. There were more males than female HCWs in Afghanistan and Malawi. Haiti, Nepal, and Senegal datasets contained more females than male HCWs. In the Afghanistan sample, many of the HCWs were medical doctors. There were more nurses and midwives than other HCWs in Haiti and Senegal as shown in Table 1.
Correlates of the required doses of hepatitis B among healthcare workers
Among the five countries under observation, gender was significantly associated with the required doses of hepatitis B vaccination among HCWs in Haiti only (Table 2). Compared to male HCWs in Haiti, female HCWs in Haiti [AOR = 1.59, CI 1.23, 2.06] were more likely to receive the required doses of hepatitis B vaccination (Table 2). In all the five countries, the study observed that a unit increase in years of education was associated with a higher likelihood of receiving the required doses of hepatitis B vaccination (Table 2). Occupational qualification (the type of profession) was significantly associated with receiving the required doses of hepatitis B vaccine, but the category of the qualification that was protective varied from country to country. Compared to medical doctors, nurses and midwives [AOR = 5.95, CI 2.23, 15.88], and other professionals [AOR = 8.57, CI 2.92, 25.09] were more likely to receive the required doses of Hepatitis B vaccine in Afghanistan. In Haiti, nurses and midwives [AOR = 0.22, CI 0.16, 0.31], and other professionals [AOR = 0.19, CI 0.12, 0.29] were less likely to receive the required doses of Hepatitis B vaccine compared to medical doctors. Compared to medical doctors, other professionals [AOR = 0.30, CI 0.11, 0.76] were less likely to receive the required doses of hepatitis B vaccine in Malawi. Compared to medical doctors, nurses and midwives [AOR = 0.29, CI 0.20, 0.43] and other professionals [AOR = 0.22, CI 0.15, 0.31] were less likely to receive the required doses of hepatitis B vaccination in Nepal. In Senegal, nurses and midwives [AOR = 0.23, CI 0.12, 0.57] were less likely to receive the required doses of hepatitis B vaccination compared to medical doctors.
Discussion
This study found that the estimated national prevalence of required hepatitis B vaccination coverage among HCWs in Afghanistan, Haiti, Malawi, Nepal, and Senegal were 69.1%, 11.3%, 15.4%, 46.5%, and 19.6%, respectively. The study also found gender to be significantly associated with hepatitis B vaccination among HCWs in Haiti. Years of education was protective for hepatitis B vaccination among HCWs in all five countries. Similarly, occupational qualification (type of profession) was significantly associated with hepatitis B vaccination among HCWs, with the protective occupational qualification varying from country to country.
The differences in diagnostic techniques and immunization protocols in these countries may be contributing factors to the discrepancies in the uptake of hepatitis B vaccination among the HCWs [44]. The low coverage in some countries may be due to the cost and unavailability of vaccination [13, 15], while the high coverage in some countries such as Afghanistan is likely due to local and national policies that ensure the availability of free hepatitis B vaccine for the HCWs [3, 15, 23]. The study findings of low prevalence (11.3%) in Haiti was similar to results from Cameroon (11.4%) [45] and Burkina Faso (10.9%) [23]. Afghanistan’s relatively high coverage (69.1%) compares to that of China (60%) [15], United States of America (63.4%) [46], and Libya (62.1%) [23]. Haiti’s low coverage is not surprising because hepatitis B vaccine was only introduced into their national routine immunization schedule in 2012 [36, 37].
Afghanistan, for example, has a robust national hepatitis B immunization strategy which targets mandatory vaccination at birth, 6 weeks, 10 weeks and 14 weeks [47]. Nevertheless, this childhood hepatitis B vaccination strategy does not explain the high vaccination prevalence in adults. A recent cross-sectional survey among 502 health workers in Kabul, the Afghan Capital, found that only 77.45% had undergone screening for HBV, and 56.37% had received at least one dose of the hepatitis B vaccine [48]. Given that the forgoing results is from a study conducted in one locality, the result from our analysis is complementary and has an added advantage of the possibility of generalizability because of the nationwide representativeness of our study sample.
The study found significant association between hepatitis B vaccination status and gender, healthcare occupational qualification (type of profession) and years of education. While in general, female HCWs were more likely to receive the required doses of the hepatitis B vaccine, gender was not a statistically significant predictor in Afghanistan, Malawi, and Nepal. In Haiti and Senegal, the study found that females were more likely than male HCWs to have had a complete dose of the hepatitis B vaccine. This could be explained by the observation that, females have greater risk perception than males [10] and this could possibly be due to the high health-seeking behaviours among women in general [11]. Our result concurs with findings in similar studies conducted in Ethiopia [3, 10, 11]. Therefore, contextual gender-specific, friendly interventions can be devised to improve the uptake of hepatitis B vaccination among all HCWs.
In this study, there was significant association between occupational qualification (type of profession) and vaccination status. Except in Afghanistan and Malawi (nurses and midwives only), where other healthcare professionals and nurses were more likely than medical doctors to have received the required doses of hepatitis B vaccine, nurses and midwives and other professionals were less likely than doctors to have received the required dose of hepatitis B vaccine. This concurs with other studies that found medical doctors to have higher vaccination coverage in general than nurses and other professional groups [23, 24, 49]. This underlines the importance of targeted interventions towards all HCWs to be encouraged to vaccinate against hepatitis B especially among nurses and midwives and other HCWs. In addition, years of education were statistically significant to vaccination status across all the five countries. This concurs with previous studies that found significantly higher vaccination coverage among bachelor/first degree and master’s degree holders compared to their counterparts with associate degree/diploma and below [3, 49]. The study results are consistent with other studies conducted in the United States of America [46], Western Greece [50] and Nigeria [51]. This could be explained in terms of the key role played by education in promoting better awareness of the infectious disease and a higher acceptance of vaccination among highly educated HCWs [3, 52].
Based on the study findings, one would argue that policymakers in developing countries should mandatorily make hepatitis B vaccination and other important vaccinations key requirements for employment, especially among HCWs who regularly encounter bodily fluids of patients. This is practised elsewhere in countries such as France, where even students going into clinical practice require mandatory hepatitis B vaccination [53]. Nevertheless, in our knowledge, although global strategies highly encourage complete vaccination among health care providers with potential risk for exposure bodily fluids, these recommendations do not generally encourage discrimination of HCWs based on hepatitis B vaccination status [54]. In developing countries where health care providers may be inadequate, making vaccinations requisite for employment may be counterproductive. This calls for wholistic approach to improve vaccination rate in developing countries. Students being enrolled into healthcare-related programmes could be targeted to increase vaccination among future HCWs and help in protecting them during clinical training and their future healthcare practice [23]. In addition, various governments should commit financial resources towards free hepatitis B vaccination as part of incentives for frontline HCWs while incorporating it into national immunization programmes from birth for the entire population. With the varying, endemic incidence of hepatitis B in these countries, there should be key priorities in increasing screening uptakes to identify HCWs requiring vaccination and those with chronic infections who may find antiviral treatment rather beneficial [23, 55]. Lastly, with the resolution of the World Health Organization to drastically reduce hepatitis B infections, these countries should not hesitate to seek technical support and resources from the global union when the need arises.
Strengths and limitations of the study
The study relied on nationally representative health facilities datasets, which increases the validity of generalizing the estimated results. However, the study has certain limitations. First, the survey has limited variables on socioeconomic and demographic characteristics. As a result, the study relied on just a few variables to build the logistic regression models. Second, the associations between the outcome variable and the explanatory variables cannot be interpreted as causal given that the datasets are from population-based surveillance surveys. Lastly, the study periods of the surveys vary from one country to another. Given that national and global policy changes between survey times may affect vaccination rates, any observed inter-country variation should be interpreted in context of the differential time points for data collection.
Conclusion
The study findings provide better insights to policymakers in the five countries to understand the prevalence of hepatitis B vaccination among HCWs by unravelling the geo-clinicodemographic factors that predict its uptake. We found the uptake of complete hepatitis B vaccination among HCWs in Afghanistan, Haiti, Malawi, Nepal, and Senegal to be 69.1%, 11.3%, 15.4%, 46.5%, and 17.6%, respectively. Gender, occupational qualification, and years of education were significant correlates of receiving the required doses of hepatitis B among HCWs. Policymakers in these developing countries should intensify education campaigns, screening uptakes to identify HCWs requiring vaccination, consider making hepatitis B vaccination a compulsory and key requirement for employment following stakeholder consultations, and support the antiviral treatment of HCWs with chronic infections. Ultimately, this will reduce the infection rate among the general population.
Availability of data and materials
Data used for the present study is freely available after online request at https://dhsprogram.com/data/dataset_admin/index.cfm. The dataset supporting the conclusions of this article is included within the article.
Abbreviations
- AOR:
-
Adjusted odd ratio
- AMR:
-
Antimicrobial resistance
- HBV:
-
Hepatitis B virus
- CDC:
-
Centre for Disease Control and Prevention
- CI:
-
Confidence interval
- DHS:
-
Demographic and Health Survey
- HCW:
-
Health care worker
- SPA:
-
Service Provision Assessment
- WHO:
-
World Health Organization
References
Cox AL, El-Sayed MH, Kao J-H, Lazarus JV, Lemoine M, Lok AS, et al. Progress towards elimination goals for viral hepatitis. Nat Rev Gastroenterol Hepatol. 2020;17:533–42.
Stanaway JD, Flaxman AD, Naghavi M, Fitzmaurice C, Vos T, Abubakar I, et al. The global burden of viral hepatitis from 1990 to 2013: findings from the Global Burden of Disease Study 2013. Lancet. 2016;388:1081–8.
Awoke N, Mulgeta H, Lolaso T, Tekalign T, Samuel S, Obsa MS, et al. Full-dose hepatitis B virus vaccination coverage and associated factors among health care workers in Ethiopia: a systematic review and meta-analysis. PLoS ONE. 2020;15:e0241226.
World Health Organization. WHO | Global hepatitis report, 2017. WHO. 2017. http://www.who.int/hepatitis/publications/global-hepatitis-report2017/en/. Accessed 28 Jan 2021.
Spearman CW, Afihene M, Ally R, Apica B, Awuku Y, Cunha L, et al. Hepatitis B in sub-Saharan Africa: strategies to achieve the 2030 elimination targets. Lancet Gastroenterol Hepatol. 2017;2:900–9.
Abara WE, Qaseem A, Schillie S, McMahon BJ, Harris AM. Hepatitis B vaccination, screening, and linkage to care. Ann Intern Med. 2018;168:902–3.
Ssekamatte T, Mukama T, Kibira SPS, Ndejjo R, Bukenya JN, Kimoga ZPA, et al. Hepatitis B screening and vaccination status of healthcare providers in Wakiso district, Uganda. PLoS ONE. 2020;15:e0235470.
Lancet T. Carving a new path to a hepatitis B cure. Lancet. 2019;394:2202.
MacLachlan JH, Cowie BC. Hepatitis B virus epidemiology. Cold Spring Harb Perspect Med. 2015;5:a021410.
Abebaw T-A, Aderaw Z, Gebremichael B. Hepatitis B virus vaccination status and associated factors among health care workers in Shashemene Zonal Town, Shashemene, Ethiopia: a cross sectional study. BMC Res Notes. 2017;10:260.
Bante A, Debalkie M, Getie A, Biresaw A, Mersha A, Ahmed Y, et al. Hepatitis B vaccination and its associated factors among health care workers working in Wolayita Sodo Hospitals, Southern Ethiopia: a cross-sectional study. J Infect Dis Immunity. 2019;11:1–10.
World Health Organization. Hepatitis B vaccines: WHO position paper, July 2017—recommendations. Vaccine. 2019;37:223–5.
Abiye S, Yitayal M, Abere G, Adimasu A. Health professionals’ acceptance and willingness to pay for hepatitis B virus vaccination in Gondar City Administration governmental health institutions, Northwest Ethiopia. BMC Health Serv Res. 2019;19:796.
Kesieme EB, Uwakwe K, Irekpita E, Dongo A, Bwala KJ, Alegbeleye BJ. Knowledge of Hepatitis B vaccine among operating room personnel in Nigeria and their vaccination status. Hepat Res Treat. 2011. https://doi.org/10.1155/2011/157089.
Yuan Q, Wang F, Zheng H, Zhang G, Miao N, Sun X, et al. Hepatitis B vaccination coverage among health care workers in China. PLoS ONE. 2019;14:e0216598.
World Health Organization. Hepatitis B. 2020. https://www.who.int/news-room/fact-sheets/detail/hepatitis-b. Accessed 28 Jan 2021.
Dahlström E, Funegård Viberg E. Knowledge about hepatitis B virus infection and attitudes towards hepatitis B virus vaccination among Vietnamese university students in Ho Chi Minh City:—a quantitative study. 2013.
Ajuwon BI, Yujuico I, Roper K, Richardson A, Sheel M, Lidbury BA. Hepatitis B virus infection in Nigeria: a systematic review and meta-analysis of data published between 2010 and 2019. BMC Infect Dis. 2021;21:1120.
Leuridan E, Van Damme P. Hepatitis B and the need for a booster dose. Clin Infect Dis. 2011;53:68–75.
Advisory Committee on Immunization Practices, Centers for Disease Control and Prevention (CDC). Immunization of health-care personnel: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2011;60:1–45.
Ziglam H, El-Hattab M, Shingheer N, Zorgani A, Elahmer O. Hepatitis B vaccination status among healthcare workers in a tertiary care hospital in Tripoli, Libya. J Infect Public Health. 2013;6:246–51.
Ouédraogo HG, Kouanda S, Tiendrébeogo S, Konseimbo GA, Yetta CE, Tiendrébeogo E, et al. Statut vaccinal contre le virus de l’hépatite B et facteurs associés parmi le personnel de santé au Burkina Faso. Médecine et Santé Tropicales. 2013;23:72–7.
Auta A, Adewuyi EO, Kureh GT, Onoviran N, Adeloye D. Hepatitis B vaccination coverage among health-care workers in Africa: a systematic review and meta-analysis. Vaccine. 2018;36:4851–60.
Ogoina D, Pondei K, Adetunji B, Chima G, Isichei C, Gidado S. Prevalence of Hepatitis B vaccination among health care workers in Nigeria in 2011–12. Int J Occup Environ Med. 2014;5:51–6.
Attaullah S, Ur Rehman S, Khan S, Ali I, Ali S, Khan SN. Prevalence of Hepatitis B virus genotypes in HBsAg positive individuals of Afghanistan. Virol J. 2011;8:281.
Khan S, Attaullah S. Share of Afghanistan populace in hepatitis B and hepatitis C infection’s pool: is it worthwhile? Virol J. 2011;8:216.
Childs L, Adrien P, Minta AA, François J, Phaïmyr Jn Charles N, Blot V, et al. Prevalence of chronic Hepatitis B virus infection among children in Haiti, 2017. Am J Trop Med Hyg. 2019;101:214–9.
Coste M, De Sèze M, Diallo A, Carrieri MP, Marcellin F, Boyer S. Burden and impacts of chronic hepatitis B infection in rural Senegal: study protocol of a cross-sectional survey in the area of Niakhar (AmBASS ANRS 12356). BMJ Open. 2019;9:e030211.
Stockdale AJ, Mitambo C, Everett D, Geretti AM, Gordon MA. Epidemiology of hepatitis B, C and D in Malawi: systematic review. BMC Infect Dis. 2018;18:516.
Shedain PR, Devkota MD, Banjara MR, Ling H, Dhital S. Prevalence and risk factors of hepatitis B infection among mothers and children with hepatitis B infected mother in upper Dolpa, Nepal. BMC Infect Dis. 2017;17:667.
Bhattarai S, Smriti KC, Pradhan PM, Lama S, Rijal S. Hepatitis B vaccination status and Needle-stick and Sharps-related injuries among medical school students in Nepal: a cross-sectional study. BMC Res Notes. 2014;7:774.
Shrestha DB, Khadka M, Khadka M, Subedi P, Pokharel S, Thapa BB. Hepatitis B vaccination status and knowledge, attitude, and practice regarding Hepatitis B among preclinical medical students of a medical college in Nepal. PLoS ONE. 2020;15:e0242658.
Stockdale AJ, Meiring JE, Shawa IT, Thindwa D, Silungwe NM, Mbewe M, et al. Hepatitis B vaccination impact and the unmet need for antiviral treatment in Blantyre, Malawi. J Infect Dis. 2021. https://doi.org/10.1093/infdis/jiab562.
Périères L, Diallo A, Marcellin F, Nishimwe ML, Ba EH, Coste M, et al. Hepatitis B in Senegal: a successful infant vaccination program but urgent need to scale up screening and treatment (ANRS 12356 AmBASS survey). Hepatol Commun. 2022;6:1005–15.
Kumar GS, Pezzi C, Wien S, Mamo B, Scott K, Payton C, et al. Health of special immigrant visa holders from Iraq and Afghanistan after arrival into the United States using Domestic Medical Examination data, 2014–2016: a cross-sectional analysis. PLoS Med. 2020;17:e1003083.
Tohme RA, Andre-Alboth J, Tejada-Strop A, Shi R, Boncy J, François J, et al. Hepatitis B virus infection among pregnant women in Haiti: a cross-sectional serosurvey. J Clin Virol. 2016;76:66–71.
Ropero Álvarez AM, Pérez-Vilar S, Pacis-Tirso C, Contreras M, El Omeiri N, Ruiz-Matus C, et al. Progress in vaccination towards hepatitis B control and elimination in the Region of the Americas. BMC Public Health. 2017;17:325.
Chipetah F, Chirambo A, Billiat E, Shawa IT. Hepatitis B virus seroprevalence among Malawian medical students: a cross-sectional study. Malawi Med J. 2017;29:29–31.
Ministry of Public Health, Afghanistan, ICF. Afghanistan Service Provision Assessment 2018–19. Kabul: Ministry of Public Health, Afghanistan, and ICF; 2019.
Institut Haïtien de l’Enfance (IHE), ICF. Évaluation de la Prestation des Services de Soins de Santé, Haïti, 2017–2018. Rockville: IHE and ICF; 2019.
Ministry of Health (MoH) [Malawi], ICF International. Malawi Service Provision Assessment (MSPA) 2013–14. Lilongwe: MoH and ICF International; 2014.
Ministry of Health, Nepal, New ERA, Nepal, Nepal Health Sector Support Program (NHSSP), ICF. Nepal Health facility survey 2015. Kathmandu: Ministry of Health, Nepal; 2017.
Agence Nationale de la Statistique et de la Démographie ANSD/Sénégal, ICF. Senegal: Enquête Continue sur la Prestation des Services de Soins de Santé ECPSS 2019. Dakar: ANSD et ICF; 2020.
Akazong WE, Tume C, Njouom R, Ayong L, Fondoh V, Kuiate J-R. Knowledge, attitude and prevalence of hepatitis B virus among healthcare workers: a cross-sectional, hospital-based study in Bamenda Health District, NWR, Cameroon. BMJ Open. 2020;10:e031075.
Bilounga Ndongo C, Eteki L, Siedner M, Mbaye R, Chen J, Ntone R, et al. Prevalence and vaccination coverage of Hepatitis B among healthcare workers in Cameroon: a national seroprevalence survey. J Viral Hepat. 2018;25:1582–7.
Byrd KK, Lu P, Murphy TV. Hepatitis B vaccination coverage among health-care personnel in the United States. Public Health Rep. 2013;128:498–509.
World Health Organization. Vaccination schedule for Afghanistan. 2021. https://immunizationdata.who.int/pages/schedule-by-country/afg.html?DISEASECODE=&TARGETPOP_GENERAL=GENERAL. Accessed 31 Jan 2022.
Roien R, Mousavi SH, Ozaki A, Baqeri SA, Hosseini SMR, Ahmad S, et al. Assessment of knowledge, attitude, and practice of health-care workers towards hepatitis B Virus prevention in Kabul, Afghanistan. J Multidiscip Healthc. 2021;14:3177–86.
Biset Ayalew M, Adugna Horsa B. Hepatitis B vaccination status among health care workers in a Tertiary Hospital in Ethiopia. Hepatitis Res Treat. 2017;2017:e6470658. https://www.hindawi.com/journals/heprt/2017/6470658/. Accessed 22 Jan 2021.
Karaivazoglou K, Triantos C, Lagadinou M, Bikas C, Michailidou M, Kalafateli M, et al. Acceptance of hepatitis B vaccination among health care workers in Western Greece. Arch Environ Occup Health. 2014;69:107–11.
Omotowo IB, Meka IA, Ijoma UN, Okoli VE, Obienu O, Nwagha T, et al. Uptake of hepatitis B vaccination and its determinants among health care workers in a tertiary health facility in Enugu, South-East, Nigeria. BMC Infect Dis. 2018;18:288.
Hur K, Wong M, Lee J, Lee J, Juon H-S. Hepatitis B infection in the Asian and Latino communities of Alameda County, California. J Community Health. 2012;37:1119–26.
Loulergue P, Launay O. Vaccinations among medical and nursing students: coverage and opportunities. Vaccine. 2014;32:4855–9.
Centers for Disease Control and Prevention S. CDC guidance for evaluating health-care personnel for Hepatitis B virus protection and for administering postexposure management. Morb Mortal Wkly Rep. 2013.
Malewezi B, Omer SB, Mwagomba B, Araru T. Protecting health workers from nosocomial Hepatitis B infections: a review of strategies and challenges for implementation of Hepatitis B vaccination among health workers in Sub-Saharan Africa. J Epidemiol Glob Health. 2016;6:229–41.
Acknowledgements
The authors thank the Service Provision Assessment Survey DHS project for their support and for free access to the original data used in this study.
Funding
This research received no specific grant from any funding agency, commercial entity or not-for-profit organization.
Author information
Authors and Affiliations
Contributions
PAD was responsible for the conceptualization and design, interpretation of data, literature search and drafting, as well as review and editing of the manuscript for publication. ED was responsible for design and drafting, as well as review and editing of the manuscript for publication. PA was responsible for the conceptualization and design, data acquisition, formal analyses, interpretation of data, literature search and drafting, as well as review and editing of the manuscript for publication. HOD was responsible for the design, formal analyses, interpretation of data, literature search and drafting, as well as review and editing of the manuscript for publication. JJN was responsible for the conceptualization and design, interpretation of data, literature search and drafting, supervision, as well as review and editing of the manuscript for publication. PAD and PA are the guarantors of the paper. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This analysis was based on the Service Provision Assessment Survey DHS project from Afghanistan, Haiti, Malawi, Nepal, and Senegal. Ethical clearance to undertake the survey was granted by the respective national authorizing bodies. For Afghanistan, approval for the survey was granted by the General Directorate of Monitoring & Evaluation and Health.
Information Systems with the Ministry of Public Health, Afghanistan. For Haiti, approval for the survey was granted by le Comité d’Ethique National and was implemented by Institut Haïtien de l’Enfance, Haiti. For Malawi, approval for the survey was granted by the National Health Sciences Research Committee and was implemented by the Ministry of Health (MoH), Malawi. For Nepal, approval for the survey was granted by the Public Health Administration Monitoring and Evaluation Division of the Ministry of Health, Nepal. For Senegal, approval for the survey was granted by Agence Nationale de la Statistique et de la Démographie. Informed written consent was obtained from the health care providers prior to being interviewed. Owing to the use of secondary data, no further consents were sought. The study conducted a secondary analysis with no identifiable information on survey respondents.
Competing interests
The authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Duodu, P.A., Darkwah, E., Agbadi, P. et al. Prevalence and geo-clinicodemographic factors associated with hepatitis B vaccination among healthcare workers in five developing countries. BMC Infect Dis 22, 599 (2022). https://doi.org/10.1186/s12879-022-07556-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-022-07556-3