Abstract
Background
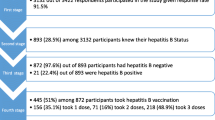
Hepatitis B vaccination for healthcare workers (HCWs) is a key component of the WHO Hepatitis B Elimination Strategy 2016–2021. Data on current hepatitis B vaccine coverage among health care workers in Sub-Saharan Africa are scarce, but these data are vital for effective programming. We assessed the proportion of HCWs vaccinated for hepatitis B and the factors associated with adequate vaccination coverage at a national hospital in Tanzania.
Methods
A descriptive cross-sectional study was conducted among consenting healthcare workers between 30th July and 30th September 2015. Vaccination histories were obtained through self-administered questionnaires. Means and proportions were used to summarize the data. Student’s t and chi-squared tests were used as appropriate. Logistic regression was used to determine the factors associated with vaccination.
Results
A total of 348 HCWs were interviewed, of whom 198 (56.9%) had received at least one dose of hepatitis B vaccination, while only 117 (33.6%) were fully vaccinated. About half of the 81 HCWs with partial vaccination (49.4%) had missed their subsequent vaccination appointments. Among unvaccinated HCWs, 14 (9.3%) had either HBV infection or antibodies against HBV infection upon pre-vaccination screening. However, the remaining participants were not vaccinated and did not know their immune status against HBV.
Nearly all respondents (347, 99.3%) had heard about the hepatitis B viral vaccine. The following reasons for non-vaccination were given: 98 (65.3%) reported that they had not been offered the vaccine; 70 (46.7%) observed standard precautions to ensure infection prevention and 60 (41.3%) blamed a low level of awareness regarding the availability of the hepatitis B vaccine.
Conclusion
The current vaccination coverage among practicing healthcare workers at Muhimbili National Hospital is low, despite a high level of awareness and the acceptance of the vaccine. Expedited and concerted efforts to scale vaccine uptake should include improved access to the vaccine, especially for newly recruited HCWs. The extension of the study to private healthcare settings and lower-level facilities would be useful.
Similar content being viewed by others
Background
Viral hepatitis infection was the seventh leading cause of global mortality and was responsible for 1.5 million deaths and 42 million disability-adjusted life years (DALYs) in 2013 [1]. Among the hepatitis viruses, Hepatitis B and C are responsible for more than 90% of the global burden of viral hepatitis [1]. It is estimated that about 240–257 million people have chronic HBV infections around the world [1]. The global prevalence of HBV infection is 1.3% and varies by geographical setting from as low as 0.2% in America to 3% in Africa [1]. More than two-thirds of hepatitis patients are in Sub-Saharan Africa and East Asia, where the prevalence is more than 8% [1,2,3]. The Hepatitis B vaccine has been available since 1981 and is considered a key strategy for preventing HBV infections.
HBV is endemic in East Africa, with an estimated HBsAg prevalence of 8% [1, 3]. In Tanzania, the HBV prevalence varies from one population to another, ranging between 8.8 and 11% among blood donors, [4,5,6] between 4 and 8% among pregnant women [7,8,9,10] and between 8 and 17% among HIV-infected individuals [11]. A study performed in Uganda showed that the sero-prevalence of HBV infection in the general population was 10% [12], and in Kenya, a recent national survey reported an HBV prevalence of 2.1%, with some regions recording a prevalence of 7.5% [13]. Earlier studies in Kenya reported an HBV prevalence between 8 and 10% [14, 15].
Healthcare workers (HCWs) are exposed to the constant risk of HBV infection due to their occupational contact with blood, blood products and other body fluids, as well as the risk of needle-stick injuries. In East Africa, the prevalence of HBV among HCWs is estimated to be between 7 and 8% [16, 17]. In developing countries, 40–65% of HBV infections among healthcare workers are attributable to percutaneous occupational exposure, whereas the corresponding risk in developed countries is as low as 10% [18]. A safe and effective HBV vaccine is available and recommended by the world Health Organization (WHO) for the primary prevention of HBV among all healthcare workers [19]. The introduction of the Hepatitis B vaccine, along with health education, reduced HBV prevalence from 10% to 1% among healthcare workers in India [19,20,21].
In Tanzania, the Hepatitis B vaccine is offered without charge to all public healthcare workers. However, only one in five healthcare workers were found to have protective immunity resulting from vaccination in a tertiary referral hospital in Tanzania [17]. In such a setting, it is important to assess the facilitators of and hurdles to HBV protection among healthcare workers. This study therefore seeks to determine the proportion of HCWs vaccinated against HBV, as well as to un-cover the factors associated with vaccination status. The findings of this study will guide policy and interventions in similar settings, particularly in Sub-Saharan Africa (SSA), as the global community works toward the elimination of HBV.
Methods
Design, patients and study procedures
A descriptive cross-sectional study was conducted at Muhimbili National Hospital (MNH), Dar es Salaam, from 30th July to 30th September 2015. The study included healthcare providers working in all departments, including trained nurses, medical attendants, and clinicians – both surgical and medical-related specialties and laboratory technicians. The investigator approached healthcare workers through the hospital administration and the heads of the departments. A self-administered questionnaire was used to obtain information from the participants. The questionnaires were collected from the healthcare workers upon completion by appointment with the participant. The sample size was calculated using the following formula for cross-sectional studies: N = {Z2P (1 – P)} /D2, where N = minimum sample size required; Z = standard normal deviation, which was set at 1.96; P = estimated proportion of healthcare workers vaccinated for HBV, which was unknown during the planning of this research and was estimated at 50%, and D = type 1 error, which we set at 0.05. The required sample size was 384.
Definition of terms
HBV vaccination schedule
HBV vaccination is provided in the form of an intramuscular injection in three doses. The first dose is the baseline dose, and the second and third doses are provided one and 6 months after the first dose, respectively.
Complete HBV vaccination
Healthcare workers who had received three HBV vaccine doses according to the HBV schedule were considered to have complete HBV vaccination.
Incomplete but on schedule HBV vaccination
Healthcare workers who had received one or two HBV vaccine doses according to the schedule but were not due for their next dose were considered to have a vaccination level that was incomplete but on schedule.
Incomplete HBV vaccination
Healthcare workers who had not received a full vaccination course but who were otherwise 1 month or more post-appointment for their scheduled dose were considered to have incomplete vaccination.
Ineligible for HBV vaccination
Healthcare workers with HBV infection or immunity to HBV upon their vaccination screening visit were considered ineligible for HBV vaccination.
Statistical analysis
The information requested via the questionnaire included vaccination status, knowledge about the transmission of and protection against HBV, and attitudes toward the Hepatitis B vaccine. The questionnaires were initially prepared in English, translated into Kiswahili and then back-translated in English to ensure that there was no loss of meaning. Both questionnaires were pre-tested for clarity and adjusted accordingly. The data were analyzed using Statistical Software for the Social Sciences (SPSS) Version 20. The categorical variables were summarized using proportions, while means were used to summarize the continuous variables. The variable of interest was complete or on-schedule vaccination as per the hepatitis B vaccination schedule. The differences between participants with complete/on-schedule vaccination and those with incomplete or no vaccination were tested using student’s t- and chi-squared tests as appropriate. Logistic regression was used to investigate the factors associated with complete and on-schedule vaccination. HCWs who were ineligible for HBV vaccination were removed from the comparative analyses.
Ethics, consent and permissions
Ethical clearance was sought from the Muhimbili University of Health and Allied Sciences (MUHAS) review board. Permission to conduct the study was sought from the MNH administration. Informed written consent was obtained from participants before recruitment into the study. Confidentiality and privacy were ensured, and the information provided was stored securely, with access being limited to the investigators. No individual information or data that could lead to identity disclosure are published in this manuscript.
Results
During the study, 348 healthcare workers (HCWs) were interviewed at the hospital, of whom 158 (45%) were males and 190 (54.5%) were females. Table 1 provides the demographic characteristics of the study participants. The mean age was 33 years, and half of the participants were 30 years old or younger. More than three-quarters of the participants had worked for 10 years or fewer. The nurse cadre was predominant in the study group, making up 124 (35.6%) of the participants. Specialist doctors were the least common, at 22 participants (6.3%). Details regarding these demographic characteristics are provided in Table 1.
Table 2 shows the vaccination status of the interviewed HCWs. Partial or full vaccination for the Hepatitis B virus was reported by 198 (56.9%) interviewees. However, only 117 (33.6%) were fully vaccinated, with three doses of the vaccine. Among HCWs with partial vaccination, 41 (50.6) were not yet due for their next dose according to the vaccination schedule. The remaining half, some 40 individuals (49.4%) with partial vaccination, had missed their scheduled vaccination visit for 1 month or more. Among unvaccinated HCWs, 14 (9.3%) had either HBV infection or antibodies against HBV infection upon pre-vaccination screening.
Table 3 provides an unadjusted comparison of vaccination coverage among the interviewed HCWs by department. Outpatient departments had the lowest proportion of vaccinated HCWs, at ten individuals (22.7%), while emergency departments, intensive care units (ICUs) and mortuary departments had the highest proportion of vaccinated individuals (76.6%) (Table 3). Healthcare workers (HCWs) who underwent partial or full-course vaccination had a mean employment duration 2.3 years, as compared to 2.5 years among those who were not vaccinated (p = 0.72).
Regarding knowledge of the transmission and prevention of HBV, the majority of the respondents, 342 individuals (98.3%), had heard about hepatitis B viral infection prior to the interview. A total of 337 (96.8%) HCWs correctly identified their work as increasing the risk of acquiring HBV infection.
Unvaccinated health workers provided the following reasons for non-vaccination: they had not been offered a chance for hepatitis B vaccination (98 individuals, 65.3%), or they were very careful and observed standard precautions while at work (70 individuals, 46.7%) (Table 4). Others reported that there was not enough awareness concerning access to hepatitis B vaccination (62 individuals, 41.3%) (Table 4).
Table 5 shows attitudes towards the hepatitis B vaccine. Among the respondents, 326 (93.7%) agreed that the Hepatitis B vaccine was effective in preventing HBV infection, while a few either disagreed (seven individuals, 2.0%) or were unsure about the effectiveness of the hepatitis B vaccine (15 individuals, 4.3%). Similarly, to a large extent, HCWs reported having trust in the vaccine (312 individuals, 89.7%), while a few (15 individuals, 4.3%) did not trust hepatitis B vaccine or had doubts about it (21 individuals, 6%). When we enquired into whether the hepatitis B vaccine should be compulsory among HCWs in Tanzania, 333 (96.8%) of the respondents agreed, while seven (2%) disagreed and four (1.1%) were undecided about mandatory hepatitis B vaccination for HCWs.
Based on the multivariate logistic regression analysis, medical attendants (PR 6.6; 95% CI 2.0–21.7) and laboratory technicians (PR = 5.7; 95% CI 1.4–22.6) were more like likely to have incomplete or no vaccination compared to interns. Similarly, newly recruited HCWs were more likely to be associated with incomplete or non-vaccination status as compared to HCWs who had been working for more than 10 years (Table 6). It is worth noting that HCWs working in the outpatient department were significantly less likely to be vaccinated as compared to HCWs from medical (internal medicine and pediatrics) departments (PR 7; 95% CI 2.0–21.7). The detailed multivariate analysis results are provided in Table 6.
Discussion
In this study, we have observed that only one in three HCWs at the national referral hospital had undergone full hepatitis B vaccination, despite high levels of awareness and the near complete acceptance of the vaccine. These rates are lower than those in Europe 50–90% [22,23,24,25,26,27,28,29] and North America 63.4% [30]. Hepatitis B vaccine coverage is even lower in the neighboring countries of Kenya (12%) [31] and Uganda (5%) [32]. These low vaccination rates are worrisome because accidental exposure to blood and body fluids is common among healthcare workers [32,33,34] and has been associated with occupational hepatitis B infections. Efforts must be made to increase coverage.
Addressing incomplete vaccination (81 individuals, 23%) is also important, particularly among those who have already missed their scheduled visit and are thus potential defaulters on the vaccination program (40 individuals, 11.4%). These HCWs are potentially at risk for infection should they be exposed to HBV. A full-course hepatitis B vaccine (three doses) is safe and tolerable and offers 95–100% protection for adults [35, 36]. The first and second HBV vaccine doses provide less protection, specifically up to 85% protection against HBV infection [35]. A significant proportion of the HCWs who received two doses and even more of those who received only one dose of the vaccine are at risk of contracting hepatitis B infection should they be exposed. This message must clearly delivered to HCWs because incomplete vaccination is largely attributed to carelessness or forgetfulness [31]. There should be no misconceptions regarding HCWs having full protection with less than three doses without demonstrated evidence of immunity through antibody level assessment.
Improving hepatitis B vaccination coverage among healthcare workers at MNH requires addressing various bottlenecks. Based on previous studies, as well as the findings from our study, hepatitis B knowledge [14, 23], access to hepatitis B vaccination [31] and a lack of publicity are the major stumbling blocks to increased coverage [31, 38, 39]. Our study revealed that 47% of unvaccinated HCWs thought that observing infection control precautions and being careful would be enough to prevent HBV infection at their workplace. Healthcare personnel who view their susceptibility to HBV infection as high are more likely to be vaccinated than their counterparts who view their susceptibility to infection as low [23]. In other studies, those who wore gloves all or most of the time when they cared for patients or instruments were more likely to be vaccinated [37]. Appropriate knowledge about the transmission and prevention of HBV infection is vital in this regard. Two out of the three unvaccinated HCWs who responded reported that they had not been offered hepatitis B vaccination. Increased publicity for the vaccine would empower HCWs to demand vaccine and know how to access the vaccine. Reports show that publicity campaigns regarding the vaccination of HCWs yielded nearly complete protection rates among HCWs [38, 39]. Given the high acceptance rates regarding the vaccine among the HCWs in our study (97%) and those in Uganda (98%) [32], publicity is important in improving vaccine coverage. Therefore, a vaccination program, when properly planned and guided with policies such as mandatory vaccination among HCWs, could be successful [29, 40]. In European countries, policies differ; some countries enforce the mandatory vaccination of HCWs [41].
Multivariate analysis demonstrated that, laboratory technicians and medical attendants were six and seven times more likely to be unvaccinated/incomplete vaccination as compared to intern doctors. This finding is worrisome because the risk of occupational injury and exposure to HBV is higher among nurses and intern doctors [22, 42,43,44]. In other places such as India, vaccination for HBV was highest among interns and lowest among nursing attendants [45]. Our data, suggest that the majority of HCWs who worked at the outpatient department, were less likely to be vaccinated. Previous reports have shown that higher vaccination coverage has been associated with surgical and laboratory departments, where the risk is high [44]. It is therefore important that these departments be sensitized to and educated about the risks and advantages of vaccination. The locations for vaccine administration, the conflicting schedules for vaccine administration vs. duty stations, and the varying workloads among departments should be considered when designing and implementing HCW vaccination programs at a given health facility. Similarly, there was an association between the probability of non−/incomplete vaccination and increased employment duration. Education must particularly target recent employed health personnel to reduce risk of new hepatitis infections.
This study has shown the level of awareness of HBV infection among HCWs. Through first-hand information gathered via self-administered questionnaires, we were able to assess HCWs’ acceptance of the hepatitis B vaccine and address bottlenecks regarding increased uptake. Notwithstanding this important contribution, our study has certain weaknesses. Vaccination status was assessed through self-provided information, which is prone to recall bias. Given the fact that the participants were healthcare workers and recent national efforts to vaccinate healthcare workers in the country, we believe this bias to be very low. Vaccination does not always translate into immunity. Therefore, the use of a hospital database and coupling this study with an assessment of anti-HBsAb titres would have helped to inform policy change. Secondly, HCWs from all departments were approached through the administration, regardless of cadre and duration of employment. Purposeful selection would probably have increased the number specialist doctors included in the study.
Conclusion
Hepatitis B vaccination coverage at this national hospital in Tanzania is currently low, despite good knowledge of and positive attitudes towards the vaccine. More effective programming, including publicity, as well as increasing access to the vaccination, could improve hepatitis B vaccine coverage. Feasibility studies regarding mandatory vaccination as a pre-requisite for employment should be conducted. Similar studies at private and lower-level health facilities are also warranted.
Abbreviations
- DALYs:
-
Disability-adjusted life years
- EMD:
-
Emergency medicine department
- HBsAb:
-
Hepatitis B surface antibody
- HBsAg:
-
Hepatitis B surface antigen
- HBV:
-
Hepatitis B virus
- HCW:
-
Health care worker
- ICU:
-
Intensive care unit
- IDU:
-
Injection drug use
- MNH:
-
Muhimbili National Hospital
- MUHAS:
-
Muhimbili University of Health and Allied Sciences
- OBGY:
-
Obstetrics and gynecology
- OPD:
-
Outpatient department
- PR:
-
Prevalence ratio
- SPSS:
-
Statistical software for the social sciences
- WHO:
-
World Health Organization
References
Stanaway JD, Flaxman AD, Naghavi M, Fitzmaurice C, Vos T, Abubakar I, et al. The global burden of viral hepatitis from 1990 to 2013: findings from the global burden of disease study 2013. Lancet. 2016;388(10049):1081–8.
Global Hepatitis Report 2017. Geneva: World Health Organization; 2017. Available at http://apps.who.int/iris/bitstream/10665/255016/1/9789241565455-eng.pdf?ua=1. Accessed 15 Dec 2017.
Schweitzer A, Horn J, Mikolajczyk RT, Krause G, Ott JJ. Estimations of worldwide prevalence of chronic hepatitis B virus infection: a systematic review of data published between 1965 and. Lancet. 2013;386:1546–55.
Hollinger FB, Liang TJ. Hepatitis B virus. In: Knipe DM, et al., editors. Field virology. 4th ed. Philadelphia: Lippincott Williams & Wilkins; 2001. p. 2971–3036.
Matee MI, Lyamuya EF, Mbena EC, et al. Prevalence of transfusion-associated viral infections and syphilis among blood donors in Muhimbili medical Centre in Dar es salaam, Tanzania. East Afr Med J. 1999;76:167–71.
Matee MN, Magesa PM, Lyamuya EF. Seroprevalence of human immunodeficiency virus, hepatitis B and C viruses and syphilis infections among blood donors at the Muhimbili National Hospital in Dar Es Salaam, Tanzania. BMC Public Health. 2006;6:21.
Rashid S, Kilewo C, Aboud S. Seroprevalence of hepatitis B virus infection among antenatal clinic attendees at a tertiary hospital in Dar es salaam, Tanzania. Tanzan J Health Res. 2014;16(1):9–15.
Menendez C, Sanchez-Tapias JM, Kahigwa E, Mshinda H, Costa J, Vidal J, Acosta C, Lopez-Labrador X, Olmedo E, Navia M, Tanner M, Rodes J, Alonso PL. Prevalence and mother-to-infant transmission of hepatitis viruses B, C, and E in southern Tanzania. J Med Virol. 1999;58(3):215–20.
Manyahi J, Msigwa Y, Mhimbira F, Majigo M. High sero-prevalence of hepatitis B virus and human immunodeficiency virus infections among pregnant women attending antenatal clinic at Temeke municipal health facilities, Dar es salaam, Tanzania: a cross sectional study. BMC Pregnancy Childbirth. 2017;17(1):109.
Pellizzer G, Ble C, Zamperetti N, Stroffolini T, Upunda G, Rapicetta M, Chione P, Villano U, Fabris P, de Lalla F. Serological survey of hepatitis B infection in Tanzania. Public Health. 1994;108(6):427–31.
Nagu TJ, Bakari M, Matee M. Hepatitis a, B and C viral co-infections among HIV-infected adults presenting for care and treatment at Muhimbili National Hospital in Dar es salaam, Tanzania. BMC Public Health. 2008 Dec 19;8:416.
Ministry of health (MoH) Uganda, ORC Marco: Uganda HIV/AIDs Sero-behavioural survey 2994–2005, Calverton Maryland USA: MoH and ORC Marco 2006.
Ly KN, Kim AA, Umuro M, Drobenuic J, Williamson JM, Montgomery JM, Fields BS, Teshale EH. Prevalence of hepatitis B virus infection in Kenya, 2007. Am J Trop Med Hyg. 2016;95(2):348–53.
Hyams KC, Morrill JC, Woody JN, Okoth FA, Tukei PM, Mugambi M, Johnson B, Gray GC. Epidemiology of hepatitis B in eastern Kenya. J Med Virol. 1989;28:106–9.
Kabanga JM, Julius K, Shiramba TL, Njenga MK, Kaiguri PM, Osidiana V. Prevalence of hepatitis B virus (HBV) surface antigen and HBV-associated hepatocellular carcinoma in Kenyans of various ages. Afr J Health Sci. 2011;18:53–61.
Ziraba AK, Bwogi J, Namale A, Wainaina CW, Mayanja-Kizza H. Sero-prevalence and risk factors for hepatitis B virus infection among health care workers in a tertiary hospital in Uganda. BMC Infect Dis. 2010;10:191.
Mueller A, Stoetter L, Kalluvya S, Stich A, Majinge C, Weissbrich B, Kasang C. Prevalence of hepatitis B virus infection among health care workers in a tertiary hospital in Tanzania. BMC Infect Dis. 2015;15:386.
Elavia AJ, Banker DD. Hepatitis B infection in hospital personnel. Natl Med India. 1992;5:265–8.
World Health Organization. Global Health sector strategy on viral hepatitis 2016–2021. WHO/HIV/2016.06 available at http://apps.who.int/iris/bitstream/10665/246177/1/WHO-HIV-2016.06-eng.pdf. Accessed 15 Dec 2017.
Kumar KA, Baghal PK, Shukla CB, Jain MK. Prevalence of hepatitis surface antigen (HBsAg) among health care workers. Indian J Comm Med. 2000;25:93–6.
Sukrit PNT, Sethi A, Angrawal K, Kumal GT. Low levels of awareness, vaccine coverage and the need for booster among health care workers in tertially care hospitals in India. J Gastro enterol Hepatol. 2008;23:1710–5.
Marković-Denić L, Branković M, Maksimović N, Jovanović B, Petrović I, Simić M, Lesić A. Occupational exposures to blood and body fluids among health care workers at university hospitals. Srp Arh Celok Lek. 2013;141(11–12):789–93.
Tafuri S, Martinelli D, Caputi G, Arbore A, Lopalco PL, Germinario C, Prato R. An audit of vaccination coverage among vaccination service workers in Puglia. Italy Am J Infect Control. 2009;37(5):414–6.
Karaivazoglou K, Triantos C, Lagadinou M, Bikas C, Michailidou M, Kalafateli M, Thomopoulos K, Assimakopoulos K, Nikolopoulou V, Jelastopulu E, Labropoulou-Karatza C. Acceptance of hepatitis B vaccination among health care workers in western Greece. Arch Environ Occup Health. 2014;69(2):107–11.
Faure E, Cortot C, Gosset D, Cordonnier A, Deruelle P, Guery B. Vaccinal status of healthcare students in Lille. Med Mal Infect. 2013;43(3):114–7.
Maltezou HC, Katerelos P, Poufta S, Pavli A, Maragos A, Theodoridou M. Attitudes toward mandatory occupational vaccinations and vaccination coverage against vaccine-preventable diseases of health care workers in primary health care centers. Am J Infect Control. 2013;41(1):66–70.
Maltezou HC, Gargalianos P, Nikolaidis P, Katerelos P, Tedoma N, Maltezos E, Lazanas M. Attitudes towards mandatory vaccination and vaccination coverage against vaccine-preventable diseases among health-care workers in tertiary-care hospitals. J Inf Secur. 2012;64(3):319–24.
Schenkel K, Radun D, Bremer V, Bocter N, Hamouda O.Viral hepatitis in Germany: poor vaccination coverage and little knowledge about transmission in target groups. BMC Public Health. 2008 23;8:132.
Vranckx R, Jacques P, De Schrijver A, Moens G. Hepatitis B vaccination coverage in Belgian health care workers. Infection. 2004;32(5):278–81.
Kathy K. Byrd, a Peng-jun Lu, and Trudy V. Murphy. Hepatitis B vaccination coverage among health-care personnel in the United States. Public Health Rep. 2013;128(6):498–509.
Suckling RM, Taegtmeyer M, Nguku PM, Al-Abri SS, Kibaru J, Chakaya JM, Tukei PM, Gilks CF. Of healthcare workers in Kenya to hepatitis B: new strategies for facilitating vaccination uptake. J Hosp Infect. 2006;64(3):271–7.
Braka F, Nanyunja M, Makumbi I, Mbabazi W, Kasasa S, Lewis RF. Hepatitis B infection among health workers in Uganda: evidence of the need for health worker protection. Vaccine. 2006;24(47–48):6930–7.
Goel V, Kumar D, Lingaiah R, Singh S. Occurrence of Needlestick and Injuries among Health-care Workers of a Tertiary Care Teaching Hospital in North India. J Lab Physicians. 2017;9(1):20–5.
Vardas E, Ross MH, Sharp G, McAnerney J, Sim J. Viral hepatitis in south African healthcare workers at increased risk of occupational exposure to blood-borne viruses. J Hosp Infect. 2002;50(1):6–12.
Assad S, Francis A. Over a decade of experience with a yeast recombinant hepatitis B vaccine. Vaccine. 1999;18(1–2):57–67.
Joukar F, Mansour-Ghanaei F, Naghipour M-R, Asgharnezhad M. Immune responses to single-dose versus double-dose hepatitis B vaccines in healthcare workers not responding to the primary vaccine series: a randomized clinical trial. Hepat Mon. 2016;16(2):e32799.
Rachiotis G, Goritsas C, Alikakou V, Ferti A, Roumeliotou A. Vaccination against hepatitis B virus in workers of a general hospital in Athens. Med Lav. 2005 Jan-Feb;96(1):80–6.
Stroffolini T, Guadagnino V, Rapicetta M, Menniti Ippolito F, Caroleo B, De Sarro G, Focà A, Liberto MC, Giancotti A, Barreca GS, Marascio N, Lombardo F. Staltari O; Sersale's study collaborating group. The impact of a vaccination campaign against hepatitis B on the further decrease of hepatitis B virus infection in a southern Italian town over 14 years. Eur J Intern Med. 2012;23(8):e190–2.
Dini G, Toletone A, Barberis I, Debarbieri N, Massa E, Paganino C, Bersi F, Montecucco A, Alicino C, Durando P. Persistence of protective anti-HBs antibody levels and anamnestic response to HBV booster vaccination: a cross-sectional study among healthcare students 20 years following the universal immunization campaign in Italy. Hum Vaccin Immunother. 2017;13(2):440–4.
Kondili LA, Ulqinaku D, Hajdini M, Basho M, Chionne P, Madonna E, Taliani G, Candido A, Dentico P, Bino S, Rapicetta M. Hepatitis B virus infection in health care workers in Albania: a country still highly endemic for HBV infection. Infection. 2007;35(2):94–7.
Maltezou HC, Wicker S, Borg M, Heininger U, Puro V, Theodoridou M, Poland GA. Vaccination policies for health-care workers in acute health-care facilities in Europe. Vaccine. 2011;29(51):9557–62.
Vos D, Götz HM, Richardus JH. Needlestick injury and accidental exposure to blood: the need for improving the hepatitis B vaccination grade among health care workers outside the hospital. Am J Infect Control. 2006;34(9):610–2.
Falagas ME, Karydis I, Kostogiannou I. Percutaneous exposure incidents of the health care personnel in a newly founded tertiary hospital: a prospective study. PLoS One. 2007 Feb 7;2(2):e194.
Marinho RT, Moura MC, Pedro M, Ramalho FJ, Velosa JF. Hepatitis B vaccination in hospital personnel and medical students. J Clin Gastroenterol. 1999;28(4):317–22.
Joshi SC, Joshi G, Singh Y, Khalil M, Joshi A, Jha SK. Hepatitis B vaccination status among healthcare workers in a tertiary care hospital in Haldwani City of Nainital, Uttarakhand, India. Ann Trop Med Public Health. 2014;7(2):96.
Acknowledgements
The authors are grateful to the following: the Government of Tanzania, which provided funds to support this study; the Muhimbili University of Health and Allied Sciences for assisting with logistical issues; Muhimbili National Hospital authority for allowing the study to be performed and all staff who participated in the study.
Funding
Funding for this research was provided by the Government of Tanzania through the Ministry of Education as part of research training for medical doctors. The funder had no role in the design, data acquisition, data management, data analysis or the presentation of the findings.
Availability of data and materials
The dataset generated and used during the current study is available and may be accessed from the corresponding author upon reasonable.
Author information
Authors and Affiliations
Contributions
The study was conceived and developed by DA and TJN. Data collection was performed by DA. Analysis and results interpretation was performed by DA, TJN, EK and JR. The manuscript was first drafted by TJN. All authors contributed to the draft, and finally, all authors approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical clearance was granted by the Muhimbili University of Health and Allied Sciences (MUHAS) ethics review board. All permissions were obtained before the commencement of the study. Informed written consent was obtained from the participants before recruitment. Confidentiality and privacy were ensured, and the information provided was securely stored and accessible only to the investigators.
Consent for publication
Not applicable. There are no personal identifiers in the data we are presenting in this manuscript.
Competing interests
All authors declare that they have no any competing interests with regard to this publication.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Aaron, D., Nagu, T.J., Rwegasha, J. et al. Hepatitis B vaccination coverage among healthcare workers at national hospital in Tanzania: how much, who and why?. BMC Infect Dis 17, 786 (2017). https://doi.org/10.1186/s12879-017-2893-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-017-2893-8