Abstract
Background
Colorectal cancer (CRC) is the 3rd most common cancer worldwide and the Czech Republic has the 6th highest incidence of CRC worldwide. Large intestinal microbiota play in its etiopathogenesis important role. Bacteriocins are proteins, produced by bacteria from the Enterobacteriaceae family. The aim of our prospective study was to assess the colonization of large intestinal mucosa by Escherichia coli strains and to investigate their bacteriocin production.
Methods
A total of 30 consecutive patients with colorectal adenoma, CRA (17 men, 13 women, aged 39–79, mean age 63 ± 9), 30 patients with CRC (23 men, 7 women, aged 38–86, mean age 67 ± 11) and 20 healthy controls (9 men, 11 women, age 23–84, mean age 55 ± 15) were enrolled into prospective study. Mucosal biopsies were taken in the caecum, transverse colon and rectum during pancolonoscopy. Microbiological culture, isolation and identification of bacteria followed. Bacteriocin production was assessed by growth inhibition of indicator strains E. coli K12-Row, E. coli C6 (phi), and Shigella sonnei 17. Identification of bacteriocin-encoding determinants and E. coli phylogroups was performed using PCR methods.
Results
A total of 622 strains were isolated and further investigated. A significantly higher frequency of simultaneous production of colicins and microcins was revealed in the group of patients with CRC, when compared to patients with CRA, p = 0.031. A significantly higher frequency of E. coli phylogroup D was found in patients with CRC, when compared to controls, p = 0.044. A significantly higher prevalence of bacteriocinogeny was confirmed in patients with advanced adenoma when compared to patients with non-advanced adenoma, p = 0.010. Increasing bacteriocinogeny was associated with an increasing stage of CRC (assessed according to TNM classification). Either E. coli phylogroup B2 or E. coli phylogroup D were isolated in biopsies of patients with right-sided CRC. A statistically higher incidence of E. coli phylogroup B2 was found in patients with right-sided CRC when compared to patients with left-sided CRC, p = 0.028.
Conclusions
Large intestinal mucosa of patients with more advanced colorectal neoplasia is colonized with more virulent strains of E. coli and higher production of bacteriocins is observed in these patients when compared to those with less advanced colorectal neoplasia.
Similar content being viewed by others
Background
Colorectal cancer (CRC) is the 3rd most common cancer having been diagnosed in nearly 1.4 million people worldwide in 2012. The Czech Republic had the 6th highest incidence of CRC worldwide and the age-standardized rate per 100 000 was 38.9 in 2012 [1]. Despite previous efforts, the etiopathogenesis of CRC has not been fully clarified yet and prevention does not exist. Large intestinal microbiota, undoubtedly, play an important role in the CRC pathogenesis [2],[3].
Even though a considerable effort was put into the development of new antineoplastic therapeutic strategies, severe side effects and resistance of colon cancer cells towards the therapy remain limiting hurdles [4],[5].
Bacteriocins possess antimicrobial [6], proapoptotic [7], and probiotic properties [8]. Although the exact role of bacteriocins is not known on both bacterial population level and at the level of their interaction with the eukaryotic host, several bacteriocins posess antineoplastic properties according to in vitro studies [9],[10]. Colicins, microcins, pyocins and pediocins belong to the bacteriocins with a reported antineoplastic activity [11].
Bacteriocins are produced by Escherichia coli strains and related bacteria from the Enterobacteriaceae family [12],[13].
The aim of our prospective study was to assess whether there are differences in E. coli colonization of the large intestinal mucosa between the groups tested and to investigate bacteriocin production in the patients with colorectal adenoma (CRA) and CRC.
Methods
A total of 30 consecutive patients with CRA (17 men, 13 women, aged 39–79, mean age 63 ± 9), 30 patients with CRC (23 men, 7 women, aged 38–86, mean age 67 ± 11) and 20 healthy controls (population with average risk for CRC with normal endoscopic findings and with negative history of CRA, CRC or inflammatory bowel disease; 9 men, 11 women, age 23–84, mean age 55 ± 15) were enrolled into the prospective study.
There were 6 patients with non-advanced (N-A) CRA and 24 patients with advanced (A) CRA. Advanced CRA is either an adenoma with low grade dysplasia larger than 10 mm and/or adenoma with high grade dysplasia of any size and/or adenoma with villous component found on histology. The group with CRC included 4 patients with right-sided CRC and 26 patients with left-sided CRC. The border between the “left” and the “right” colon was at the lineal flexure of the colon.
Individuals enrolled into the study were invited for the diagnostic and/or therapeutic pancolonoscopy. The usual bowel preparation was either polyethylene glycol or sodium phosphate solution. Pancolonoscopy was performed in a standard manner under conscious sedation in all the subjects. Video-colonoscopes Olympus 160 series (Olympus Corp., Tokyo, Japan) were used after previous high-level disinfection for each particular investigation (ETD2 and ETD3 disinfectors Olympus). Mucosal biopsies were taken from the caecum, transverse colon and the rectum during the procedure in all the patients/healthy controls (90 biopsies in patients with CRA, 90 biopsies in patients with CRC and 60 biopsies in the control group). Sterile biopsy forceps (Olympus) were used for every single biopsy. In our previous study we verified that the inner space of the forceps remained sterile despite the passage of the accessory through the working channel of the endoscope (data not shown). Each biopsy specimen of the colonic mucosa was immediately inserted into a transport liver-enriched broth. Standard primary cultures were inoculated on the blood and MacConkey agars (at 37°C for 24 hours); this was followed by a standard clone isolation. Up to 7 different colonies of the coliform bacteria were isolated from each sample (on the blood, MacConkey and deoxycholate agars). Particular bacteria were precisely identified by the Vitek2 system (BioMérieux, Marcy l’Etoile, France) and susceptibility of the strains to the antibiotics was assessed. Together, 622 isolates were identified: 221 in the group of patients with CRA, 151 in the healthy controls and 250 in the patients with CRC. All the bacterial strains were frozen in cryotube vials at −80°C appropriately.
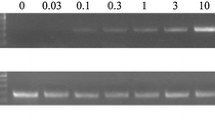
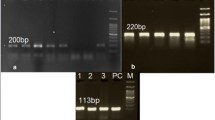
Bacteriocinogeny (bacteriocin production) of each strain, bacteriocinogenotypisation (determination of bacteriocin type) and E. coli phylogroups were further investigated. Frozen bacterial strains were streaked for single colonies and one single colony was used for inoculation of liquid TY medium containing tryptone (Hi-Media, Mumbai, India) 8 g/L, yeast extract (Hi-Media) 5 g/L, and sodium chloride 5 g/L. The agar plates (containing the 1.5% TY agar, w/v) were subsequently inoculated by needle stab with fresh broth cultures and the plates were incubated at 37°C for 48 hours. The bacteria were killed using chloroform vapours for 30 minutes. Each plate was overlaid with a thin layer of a soft agar (0.7% TY agar, w/v) containing 107 cells/mL of an indicator strain. The plates were then incubated at 37°C overnight. With the exception of TY agar plates, bacteriocin production was tested on a relatively unenriched agar containing a Difco™nutrient broth (Difco Laboratories, Sparks, MD) 8 g/L, sodium chloride 5 g/L, and 1.5% (w/v) agar. Indicator strains of E. coli K12-Row, E. coli C6 (phi) and Shigella sonnei 17 were used for the assessment of bacteriocin production (a zone of growth inhibition is present around the strain tested, if the indicator strain is susceptible to the bacteriocin produced by the strain tested). All these indicator strains were from our in-house collection of strains. Bacteriocin production was also confirmed by PCR methods. Bacteriocinogenotypisation and determination of E. coli phylogroups were investigated by PCR methods using specific primers for the detection of colicin, microcin genes (see Tables 1 and 2 for details) and genes specific for each E. coli phylogroup [14]. Altogether, 23 individual colicin types (colicins A, B, D, E1-E9, Ia, Ib, Js, K, L, M, N, S4, U, Y, 5/10) and 8 microcin types (mB17, mC7, mE492, mH47, mJ25, mL, mM, mV) were tested in this study [15]; see Additional file 1 for details.
Data obtained were treated statistically by means of descriptive statistics, non-paired t-test and Fisher’s exact test using Statistica software. The differences in bacteriocinogeny, colicinogeny and microcinogeny between the groups tested were assessed by non-paired t-test (as this was referred to the number of biopsies taken in each group: 90 vs 90 vs 60). Fisher t-test was used for investigation of differences in production of each bacteriocin between the groups tested (as this was reffered to the number of individuals in each group: 30 vs 30 vs 20 and the numbers were small).
All individuals enrolled into the study were adult persons. Participants were adequately informed and a written informed consent for participation in the study including agreement with the data and information to be published in an anonymous way was obtained from all the enrolled subjects. The project was approved by the Joint Ethical Committee (Charles University in Praha, Faculty of Medicine at Hradec Kralove & University Teaching Hospital Hradec Kralove). For all data obtained, all personal identification information was removed in compliance with the Czech laws for protection of confidentiality.
Results
Microbiological culture was performed on 240 mucosal biopsies taken from 60 patients (30 patients with CRC, 30 patients with CRA) and 20 healthy controls. Together 622 strains were isolated and futher investigated. There were no statistically significant differences in the frequency of strains belonging to the Enterobacteriaceae family between our groups investigated. A significantly higher frequency of Escherichia coli strains was found in the patients with CRC, when compared to the healthy controls, p < 0.001; see Table 3 for details.
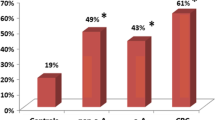
There was no difference in colicinogeny and microcinogeny between the groups tested. A significantly higher frequency of simultaneous production of colicins and microcins was revealed in the group of patients with CRC, when compared to patients with CRA, p = 0.031; see Table 3 for details. A trend towards higher co-production of colicins and microcins in the healthy controls, when compared to the patients with CRA, was revealed, p = 0.065; see Table 3 for details. A statistically significant difference in bacteriocinogeny was found between patients with non-advanced (N-A) and patients with advanced (A) CRA: N-A: 7/18 (39%), A: 51/71 (72%); p = 0.010.
Colicin Ia was the most commonly synthetised colicin in all the groups tested. It was followed by the colicin Ib in the patients with CRA and in the healthy controls. In the patients with CRC, the colicin M belongs to the 2nd most frequently synthetised colicin after the colicin Ia. Colicin M was produced by 4% of patients with CRA, 10% of healthy individuals and 21% of patients with CRC. There was a statistically significant difference in production of colicin M between the patients with CRA and CRC (p = 0.001) and a trend towards higher production of colicin M in the patients with CRC, when compared to the healthy controls, was identified; p = 0.070. Microcin mH47 was the most frequently produced microcin in all the groups tested. In the patients with CRA, it was followed by microcin mV. Synthesis of microcin mM was the second most common after microcin mH47 in the patients with CRC and in the healthy individuals.
The lowest incidence of E. coli phylogroup A and B1 were found in the group of the patients with CRC. A significantly higher frequency of E. coli phylogroup D was found in the group of patients with CRC, when compared to the healthy controls, p = 0.044. Similar frequency of E. coli phylogroup B2 was found in all the groups tested; see Table 3 for details. A trend towards lower frequency of E. coli phylogroup B2 was revealed in the group of patients with N-A CRA, when compared to the patients with A CRA: N-A: 4/17 (24%), A: 31/60 (52%); p = 0.054. Either E. coli phylogroup B2 or E. coli phylogroup D were isolated in all biopsies, which were taken in the patients with right-sided CRC. A statistically significant difference in the frequency of E. coli phylogroup B2 was revealed between patients with right-sided CRC and patients with left-sided CRC: right-sided: 9/12 (75%), left-sided: 32/78 (41%); p = 0.028.
Increasing bacteriocinogeny, colicinogeny, microcinogeny and colicinogeny & microcinogeny was associated with an increasing stage of CRC (assessed according to the TNM classification), see Table 4 for details. A statistically significant difference was found in microcinogeny between the stage 1 and stage 4: p = 0.038.
Discussion
Large intestinal microbiota, undoubtedly, play an important role in the pathogenesis of CRC [2],[3]. E. coli can be classified into 3 major groups: commensal strains, intestinal pathogenic strains and extraintestinal pathogenic strains [16],[17]. Phylogenetic diversity of E. coli exists within each subgroup [16]. Four phylogroups of E. coli are well-known. Commensal strains usually belong to the A or B1 phylogenetic group; pathogenic strains usually belong to B2 or D phylogroup of E. coli and they possess more virulence factors when compared to the commensal strains [16],[18],[19]. Among our groups tested, the lowest incidence of E. coli phylogroup A and B1 and the highest frequency of E. coli phylogroup D was revealed in the patients with CRC. This finding shows that the large intestinal mucosa of the patients with CRC is colonized with more virulent E. coli strains. We also confirmed in our study, that large intestinal mucosa of patients with CRC is inhabited with a significantly higher proportion of Escherichia coli strains when compared to the healthy controls.
E. coli strains of the B2 phylogenetic group harbour the “pks” genomic island, which encodes production of a non-ribosomally synthetised polyketide-peptide genotoxin, called colibactin [20]. A study carried out by Cuevas-Ramos et al. documented that even a single and short exposure of mammalian epithelial cells to “pks” positive E. coli strains at low infectious doses induced DNA-double strand breaks, signs of incomplete DNA repair during the cell division which finally lead to the chromosome aberrations [21]. Infection caused by “pks” positive E. coli strains affects the host immune response and is accompanied by the production of oxygen species, pro-inflammatory cytokines and protease secretion. These mediators are able to trigger DNA-double strand breaks [22],[23]. Nowrouzian et al. substantiated the contribution of “pks” island to long-term gut-colonization of E. coli B2 strains [20]. Association of colonic mucosa of patients with CRC and enterotoxigenic E. coli belonging to the B2 phylogroup, which produces toxins called cyclomodulins, has been also highlighted recently [24]. Despite all recent efforts, the precise etiopathogenesis of right-sided colorectal cancer has not yet been clarified [25]. The high occurrence of the mutagenic E. coli B2 phylogroup in our patients with right-sided colorectal cancer could elucidate the pathogenesis and difference in the pathways of cancer development when compared to the patients with left-sided colorectal cancer. These conclusions are in agreement with those of Cuevas-Ramos, who assumed that colon colonization with “pks” positive E. coli strains contributes to the development of sporadic CRC [21]. A study carried out by Arthur et al. also confirmed that the deletion of the “pks” genotoxic island from E. coli NC101 decreased intestinal tumor multiplicity and invasion in experimental mice, without altering intestinal inflammation [26]. A higher frequency of E. coli phylogroup B2 in the patients with advanced CRA when compared to the patients with non-advanced CRA in our study confirms the anticipated involvement of “pks” positive E. coli strains in the pathogenesis of CRC.
The antineoplastic effect of colicins has been described in in vitro studies: colicin E3 is able to inhibit proliferation of leukemic cells [27],[28] and shows antineoplastic effect towards HeLa cells, epithelial cells derived from the cervix [29]. The cytotoxic effect of colicins was also proven against breast cancer cells [30]. Farkas-Himsley substantiated in an experimental study, that the cells of colorectal adenocarcinoma were more sensitive to bacteriocins when compared to normal cells of large bowel mucosa [31]. Bures et al. studied colicin production in the patients with CRC and found a significantly higher colicinogeny in the healthy controls when compared to the patients with CRC [12]. This was not confirmed in another study performed by Smarda et al. [32]. Our current study is in agreement with that of Smarda et al. in that we have not found a difference in bacteriocinogeny between the patients with CRC and the healthy controls. However we found a significantly higher simultaneous production of colicins and microcins in the patients with CRC when compared to the patients with CRA. Patients with advanced CRA had also a statistically higher bacteriocinogeny when compared to those with non-advanced CRA. Increasing bacteriocinogeny associated with an increasing stage of CRC (when assessed according to the TNM classification) highlights the previous findings: there is an increasing bacteriocin production from non-advanced CRA to advanced CRA and from non-advanced CRC to advanced CRC. Large intestinal mucosa of the patients with more advanced colorectal neoplasia is also colonized with more virulent strains of Escherichia coli.
We presume that the intermicrobial competition (for nutrition, etc.) in the large bowel of healthy subjects can be conveyed as a high simultaneous production of microcins and colicins. We may hypothetize that if the production of antimicrobial, antiapoptotic and potentially antineoplastic bacteriocins decreases in the healthy individuals, this could co-iniciate the development of a non-advanced colorectal neoplasia. With the growth, development and progression of a non-advanced neoplasia into an advanced one, higher production of bacteriocins is again identified and also more virulent E. coli strains are present. We assume, that this situation could be beneficial for the host and might help the macroorganism in combating the colorectal cancer. Our hypothesis needs furher investigation especially in the field of potential antineoplastic properties of the bacteriocins and clarification of their interaction with the eukaryotic host.
Conclusions
Large intestinal mucosa of the patients with more advanced colorectal neoplasia is colonized with more virulent strains of Escherichia coli and a higher production of bacteriocins is observed in these patients when compared to those with less advanced colorectal neoplasia.
Availability of supporting data
The data sets supporting the results of this article are included within the article and its additional file.
Additional file
References
World Cancer Research Fund international. [http://www.wcrf.org/cancer_statistics/world_cancer_statistics.php]
Zackular JP, Baxter NT, Iverson KD, Sadler WD, Petrosino JF, Chen GY, Schloss PD: The gut microbiome modulates colon tumorigenesis. MBio. 2013, 4: e00692-13. 10.1128/mBio.00692-13.
Yang T, Owen JL, Lightfoot YL, Kladde MP, Mohamadzadeh M: Microbiota impact on the epigenetic regulation of colorectal cancer. Trends Mol Med. 2013, 19: 714-725. 10.1016/j.molmed.2013.08.005.
Di Francia R, Siesto RS, Valente D, Del Buono A, Pugliese S, Cecere S, Cavaliere C, Nasti G, Facchini G, Berretta M: Current strategies to minimize toxicity of oxaliplatin: selection of pharmacogenomic panel tests. Anticancer Drugs. 2013, 24: 1069-1078. 10.1097/CAD.0000000000000002.
Rahman AU, Salajegheh A, Smith RA, Lam AK: BRAF Inhibitor Therapy for Melanoma, Thyroid and Colorectal Cancers: Development of Resistance and Future Prospects. Curr Cancer Drug Targets, in press.,
Brown CL, Smith K, McCaughey L, Walker D: Colicin-like bacteriocins as novel therapeutic agents for the treatment of chronic biofilm-mediated infection. Biochem Soc Trans. 2012, 40: 1549-1552. 10.1042/BST20120241.
Chumchalová J, Smarda J: Human tumor cells are selectively inhibited by colicins. Folia Microbiol (Praha). 2003, 48: 111-115. 10.1007/BF02931286.
Messaoudi S, Manai M, Kergourlay G, Prévost H, Connil N, Chobert JM, Dousset X: Lactobacillus salivarius: bacteriocin and probiotic activity. Food Microbiol. 2013, 36: 296-304. 10.1016/j.fm.2013.05.010.
Farkas-Himsley H, Yu H: Purified colicin as cytotoxic agent of neoplasia: comparative study with crude colicin. Cytobios. 1985, 42: 193-207.
Musclow E, Farkas-Himsley H: Bacteriocin and flow cytometry in laboratory diagnosis of leukemic peripheral blood lymphocytes and bone marrow cells. Eur J Cancer Clin Oncol. 1983, 19: 163-171. 10.1016/0277-5379(83)90413-3.
Cornut G, Fortin C, Soulières D: Antineoplastic properties of bacteriocins: revisiting potential active agents. Am J Clin Oncol. 2008, 31: 399-404. 10.1097/COC.0b013e31815e456d.
Bures J, Horák V, Fixa B, Komárková O, Zaydlar K, Lonský V, Masurka V: Colicinogeny in colorectal cancer. Neoplasma. 1986, 33: 233-237.
Cascales E, Buchanan SK, Duché D, Kleanthous C, Lloubès R, Postle K, Riley M, Slatin S, Cavard D: Colicin biology. Microbiol Mol Biol Rev. 2007, 71: 158-229. 10.1128/MMBR.00036-06.
Bures J, Smajs D, Kvetina J, Forstl M, Smarda J, Kohoutova D, Kunes M, Cyrany J, Tacheci I, Rejchrt S, Lesna J, Vorisek V, Kopacova M: Bacteriocinogeny in experimental pigs treated with indomethacin and Escherichia coli Nissle. World J Gastroenterol. 2011, 17: 609-617. 10.3748/wjg.v17.i5.609.
Smajs D, Micenkova L, Smarda J, Vrba M, Sevcíkova A, Valisova Z, Woznicova V: Bacteriocin synthesis in uropathogenic and commensal Escherichia coli: colicin E1 is a potential virulence factor. BMC Microbiol. 2010, 10: 288-10.1186/1471-2180-10-288.
Russo TA, Johnson JR: Proposal for a new inclusive designation for extraintestinal pathogenic isolates of Escherichia coli: ExPEC. J Infect Dis. 2000, 181: 1753-1754. 10.1086/315418.
Bonnet M, Buc E, Sauvanet P, Darcha C, Dubois D, Pereira B, Déchelotte P, Bonnet R, Pezet D, Darfeuille-Michaud A: Colonization of the human gut by E. coli and colorectal cancer risk. Clin Cancer Res. 2014, 20: 859-867. 10.1158/1078-0432.CCR-13-1343.
Lee S, Yu JK, Park K, Oh EJ, Kim SY, Park YJ: Phylogenetic groups and virulence factors in pathogenic and commensal strains of Escherichia coli and their association with blaCTX-M. Ann Clin Lab Sci. 2010, 40: 361-367.
Sobieszczańska BA, Duda-Madej AB, Turniak MB, Franiczek R, Kasprzykowska U, Duda AK, Rzeszutko M, Iwańczak B: Invasive properties, adhesion patterns and phylogroup profiles among Escherichia coli strains isolated from children with inflammatory bowel disease. Adv Clin Exp Med. 2012, 21: 591-599.
Nowrouzian FL, Oswald E: Escherichia coli strains with the capacity for long-term persistence in the bowel microbiota carry the potentially genotoxic pks island. Microb Pathog. 2012, 53: 180-182. 10.1016/j.micpath.2012.05.011.
Cuevas-Ramos G, Petit CR, Marcq I, Boury M, Oswald E, Nougayrède JP: Escherichia coli induces DNA damage in vivo and triggers genomic instability in mammalian cells. Proc Natl Acad Sci U S A. 2010, 107: 11537-11542. 10.1073/pnas.1001261107.
Secher T, Samba-Louaka A, Oswald E, Nougayrède JP: Escherichia coli producing colibactin triggers premature and transmissible senescence in mammalian cells. PLoS One. 2013, 8: e77157-10.1371/journal.pone.0077157.
Cougnoux A, Gibold L, Robin F, Dubois D, Pradel N, Darfeuille-Michaud A, Dalmasso G, Delmas J, Bonnet R: Analysis of structure-function relationships in the colibactin-maturating enzyme ClbP. J Mol Biol. 2012, 424: 203-214. 10.1016/j.jmb.2012.09.017.
Buc E, Dubois D, Sauvanet P, Raisch J, Delmas J, Darfeuille-Michaud A, Pezet D, Bonnet R: High prevalence of mucosa-associated E. coli producing cyclomodulin and genotoxin in colon cancer. PLoS One. 2013, 8: e56964-10.1371/journal.pone.0056964.
Hansen IO, Jess P: Possible better long-term survival in left versus right-sided colon cancer - a systematic review. Dan Med J. 2012, 59: A4444-
Arthur JC, Perez-Chanona E, Mühlbauer M, Tomkovich S, Uronis JM, Fan TJ, Campbell BJ, Abujamel T, Dogan B, Rogers AB, Rhodes JM, Stintzi A, Simpson KW, Hansen JJ, Keku TO, Fodor AA, Jobin C: Intestinal inflammation targets cancer-inducing activity of the microbiota. Science. 2012, 338: 120-123. 10.1126/science.1224820.
Fuska J, Fusková A, Smarda J, Mach J: Effect of colicin E3 on leukemia cells P388 in vitro. Experientia. 1979, 35: 406-407. 10.1007/BF01964380.
Mittelman M, Farkas-Himsley H, Haran-Ghera N: Recognition of T-cell murine leukemia by bacteriocin (colicin); correlation with transplantation experiments. Leuk Res. 1987, 11: 215-222. 10.1016/0145-2126(87)90045-2.
Smarda J, Obdrzalek V: The lethal effect of colicin E3 on HeLa cells in tissue cultures. IRCS Med Sci. 1977, 5: 524-
Smarda J, Obdrzalek V, Taborsky I, Mach J: The cytotoxic and cytocidal effect of colicin E3 on mammalian tissue cells. Folia Microbiol (Praha). 1978, 23: 272-277. 10.1007/BF02876680.
Farkas-Himsley H, Cheung R, Tompkins WAF: Selective antitumor agents: bacteriocins from gram-negative bacteria. IRCS Med Sci. 1975, 3: 149-151.
Smarda J, Obdrzalek V: Incidence of colicinogenic strains among human Escherichia coli. J Basic Microbiol. 2001, 41: 367-374. 10.1002/1521-4028(200112)41:6<367::AID-JOBM367>3.0.CO;2-X.
Acknowledgements
The study was supported by research grant IGA NT/13413 (from the Czech Ministry of Health) and by research project PRVOUK P37-08 (from Charles University in Praha, Faculty of Medicine at Hradec Kralove, Czech Republic).
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
DK participated in the design of the study, was involved into obtaining samples and wrote the manuscript. DS investigated bacteriocin production and bacteriocinogenotypisation; he has been involved in drafting the manuscript. PM was involved into acquisition of data and obtaining samples. JC was involved into acquisition of data and obtaining samples. MM carried out microbiological culture and assessed the results from the culture. MF carried out microbiological culture and assessed the results from the culture. MC participated in the design of the study and performed the statistical analysis. SR was involved into acquisition of data and obtaining samples. JB has made substantial contributions to the conception of the study, to the interpretation of the data and has given final approval of the version to be published. All authors read and approved the final manuscript.
Electronic supplementary material
12879_2014_733_MOESM1_ESM.xls
Additional file 1: Sheet 1: information regarding patients with colorectal cancer (CRC). Sheet 2: information regarding patients with colorectal adenoma (CRA). Sheet 3: information regarding healthy controls (Controls). (XLS 60 KB)
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Kohoutova, D., Smajs, D., Moravkova, P. et al. Escherichia colistrains of phylogenetic group B2 and D and bacteriocin production are associated with advanced colorectal neoplasia. BMC Infect Dis 14, 733 (2014). https://doi.org/10.1186/s12879-014-0733-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-014-0733-7