Abstract
Background
There is no general agreement on a standard form of functional classification in older adults and is mainly assessed by Activities of Daily Living (ADL) and/or Instrument Activity of Daily Living. A refined classification based on evaluation the limitations of intrinsic capacity, environment and social interaction, could provide a basis to predict the future disability and identify individuals with increased risk of adverse outcomes.
Methods
A new functional classification among older adults aged 60 and over was conducted by latent class analysis and compared with the traditional classifications, based on the China Health and Retirement Longitudinal Study. To further investigate the scientific validity of this new classification, associations with 7-year mortality and ADLs impairments among categories were tested by using Survival curves and Cox proportional hazard models. This was followed by the confirmatory analysis related to the prospective data. Competing risk analysis was also performed to analysis the sensitivity to further support our conclusions.
Results
Five categories were identified among 5,992 older adults which gave the best fitting, yielding a significant Bootstrap Likelihood Ratio Test (p < 0.001) and Lo-Mendell-Rubin adjusted likelihood ratio test (p < 0.001), with an entropy over 0.80. The presence of five categories: “health” (34.0%), “sub-disorder status” (36.6%), “acute diseases” (10.3%), “somatic functional disorder” (7.7%), and “viability disorder” (11.4%), which matched well with the functional independence rates by the international classifications. Among them, those in “sub-disorder status” were considered as an intermediate status between disability and health. The findings also revealed that those who were in “acute disease”, “somatic functional disorders”, “health” and “sub-disorder status” had a significant lower risk of mortality and ADLs limitations than “viability disorder”. And the risks gradually increased towards the less functionally independent end of the classification. However, the distribution of characteristics among five categories were in a synchronous change, indicating a stable classification.
Conclusions
A new classification representing the functional heterogeneity of older adults could effectively stratify the risk of mortality and ADLs limitations. Identifying the clusters of functional decline might be useful in predicting subsequent ageing trends, designing personalized intervention, and delaying the progression of disability and preventing its occurrence.
Similar content being viewed by others
Background
According to the recent Decade of Healthy Ageing Baseline Report of the World Health Organization (WHO), functional ability includes individuals’ physical and mental abilities, the environment where people live, and the manner people interact within that [1]. Maintaining functional independence is essential for older adults to keep healthy and to delay or prevent the possible adverse outcomes in ageing process [2]. However, the WHO’s report highlighted the fact that in 2021, over 142 million of older people were unable to meet all of their basic daily needs, which accounts for 14% of all people aged 60 and above, all over the world [1]. As people age, their health needs tend to become increasingly chronic and complex. Therefore, it is urgent to assess the level of function in older adults, as well as valuable to develop responses to the problem of population ageing for health policy makers.
The diverse needs of older adults should be regarded as a continuum of functions, covering functional independence from highest to lowest [3]. The targeted interventions can be developed for different functional levels to maintain or improve functional independence and prevent adverse health outcomes [4, 5]. Functional capacity should be measured by using an instrument that assesses individuals’ intrinsic abilities, the environment where people live and their interactions within it [1, 6]. From a holistic life course perspective, intrinsic ability refers to the combination of all the physical and mental abilities of individuals that is also regarded as the physiological basis for healthy ageing [7]. Scholars usually assessed intrinsic abilities indirectly by measuring basic activities of daily living (BADL) and/or instrumental activities of daily living (IADL). BADL is important to sustain self-care (e.g., dressing, eating), while IADL are critical for independent living (e.g., shopping, preparing a meal). However, this approach is only used to identify people with severe loss of function, which approaches to disability status [8,9,10]. On this basis, a disability process model (VJ94) was proposed, and defined disability as the inability to perform normal activities in social and economic life [11]. Those activities are not limited to the ADLs, IADLs, etc. [12]. The VJ94 model is a major refinement over the medical model of disability that elucidates the role of the underlying physical, emotional, and social contexts in which pathology develops into functional decline (impairments of comprehensive functions), that is followed by disability [13]. The studies investigating levels of functioning in relation to survival or adverse outcomes have focused on the end of the continuum (intrinsic capacity impairment) or early stages (limitations of environment and social interaction), but few have comprehensively analyzed the full continuum from health to severe disability [12, 14, 15]. However, it is imperative to look into a wider range of functional continuum [16], because it is of great value and practically significant to take appropriate intervention measures for those who are at risk of adverse outcomes or functional decline before the disability state occurs.
The influence of environment and interactions within it on enabling ageing well should be taken into account while classifying groups on functional ability. The environment which is referred as a place where people live, that includes the home, community, society, and all the elements within them that contribute to shape the behavior and characteristics of older adults at certain levels of intrinsic competence. In agreement with a framework of Capability approach [17], there are factors that allow individuals to convert resources into capabilities. Those conversion factors could be internal and external. The internal conversion factors refer to physical conditions. The external conversion factors included environmental characteristics [18, 19]. An environment could provide a range of resources or barriers that are essential factors in enabling older adults to adapt or compensate for their losses of intrinsic abilities [20]. Thus, the development of a favorable and age-friendly environment is an effective way to optimize functional capacity and develop healthy ageing [21]. However, few studies to date have incorporated the environment in the assessment process of the functional continuum, which means that there may be a large number of older adults who are unable to meet their basic needs, but remained unidentified. In addition, these studies do not capture a person’s real-time functional ability in a dynamic way, taking into account a person’s intrinsic capacity and interaction with their environment, which including activities in public spaces, participation in educational and physical activity opportunities and ways to contribute to society [22,23,24]. Therefore, based on clarifying the optimized contents within each domain of functional ability, we include intrinsic capacity, environment, social interaction, and a pre-disability state in the functional continuum construct, to fill in the gap of small losses of functioning and standardize the evaluation and classification of function in population-based surveys. As well the use of the capability approach is rather an innovative way of assessing disabling situations.
The national guidelines maintain the information on the functional classification, but the classification has not been updated much in the past 10 years, and very few attempts have been made to explore the functional heterogeneity in terms of resources and society [25, 26]. We searched Web of Science and Google research up to Jan 1,2019, using the Medical Subject Heading terms “disability” “functional assessment”, and “classification”. We identified several calls from expert groups for revision of the classification, but few efforts have made to include intrinsic capacity, environment and social interaction, and implemented in the home-based community.
Existing Long-term care insurance is restricted by the fact they cover severe disability when it has developed, but there is no way to predict or care for which older population will become functional impairments and need intensified treatment or prevention measures [27]. Evidence suggests that early intervention is essential to prevent life-shortening complications caused by functional decline, as the ensuing severe disability appears to exacerbate the mechanism of apoptotic and is irreversible [28, 29].
A refined classification could provide a powerful tool to identify those functional decline and most likely to experience severely disabled at an early stage. It also could be a better predictor of adverse events in older adults, more predictive than multimorbidity or polypharmacy, and that it should be considered an assistance for clinicians to optimal treatment [30, 31]. To this end, latent class analysis (LCA) was used to classify functional ability. There are two main reasons for us to use it. First, LCA is a method of classifying heterogeneous samples by probability distribution, i.e., the presence of a latent category variable that can classify a heterogeneous whole into multiple subgroups and can be viewed as a special case of model-based clustering, for multivariate discrete data. LCA is applicable to our research, for these functional indicators are multivariate discrete data [32]. Second, LCA is increasingly used to study population heterogeneity in health and support decision-making. It has been applied to typify or cluster clinical patients with severe illness, depression, and medical conditions to support the development of treatments or prevention programs, with high application value and reliability [33, 34].
Therefore, an LCA was used to classify the older population combining intrinsic capacity, environment and society interaction in this study, to better capture the full stage of it. This new functional classification will be studied in relation to mortality and ADLs impairments, to see whether it is effective in stratifying the risk of them. The main objective was to investigate whether the new classification is validated and effective, and whether it is associated with mortality and ADLs impairments in older adults during 7-year follow up, using data from the China Health and Retirement Longitudinal Study (CHARLS), a population-based cohort study of China.
Methods
Theoretical framework
Based on the framework “capability approach” theory elaborated by Amartya Sen, functional ability is closely related to the accessibility of resources and society, as well as the individual impairment [35]. In agreement with WHO framework for healthy ageing, we have included intrinsic capacity, environment and social interaction in the functional continuum construct. To this end, this study classified functional ability according to the multidimensional indexes constructed in previous studies.
Study population
We used data from the first wave of the CHARLS (2011) and follow-up data on mortality over 7 years (2011–2018). The CHARLS is a population-based cohort study among adults aged 45 and older from 28 provinces and municipalities of China. Details on the methods and sampling have been published previously [36]. Within a total sample size of 17,708 in the 2011 baseline data, groups such as missing variables, incomplete information, and institutional pensions were excluded, and then a sample of 5992 older people aged 60 and above living at the home-based community were selected and included in the study. Of the 3859 people who had independent ADLs were also included in the current analysis. Based on data availability, relevant indicators and dimensions from systematic literature analysis, our conceptual framework of function of older people was defined in terms of three aspects of intrinsic capacity, environment and social interaction [37, 38]. And all the data information used in analysis mainly covers issues on sociodemographic characteristics, family, behavior, cognitive, psychological, environmental and biological factors that affect health and longevity. The present research protocol was approved by the Biomedical Ethics Review Committee of Peking University (IRB00001052–11,015). Ethics approval for the use of the CHARLS data was obtained from the University of Newcastle Human Research Ethics Committee (H-2015–0290). All methods were conducted in accordance with the principle of the Declaration of Helsinki, and all the participants or their legal representatives gave their written informed consent before any study procedures began.
-
(1)
Sociodemographic characteristics: age, sex, place of residence (urban and rural), educational level
-
(2)
Household factors: marital status, per capita annual household income
-
(3)
Biological factors: blood pressure, Body Mass Index (BMI)
-
(4)
Daily behavior: social activities, motor ability
-
(5)
Health behavior: sleep duration, self-rated health, life satisfaction, pain, formal (paid) and informal (unpaid) care
-
(6)
Multidimensional functional ability related variables
Exclusion for data analysis
After excluding the missing of functional indicators, losing information, and participants who did not meet our study criteria, a total of 5992 older adults were included in this analysis. To assess the association of the new functional classification with 7-year all-cause mortality and ADLs impairment, after excluding those data missing, there were 3859 participants in 2018 (Figs. 1 and 2).
Participants flow chart. Note. Participants who are suffering from ADLs impairments in baseline, and losing important information were excluded. A total of 3859 older adults were included to assess the association of the new functional classification with 7-year all-cause mortality and upcoming ADLs impairments
Variables
Participants were categorized into five groups representing the functional continuum, based on 29 multidimensional functional indexes. There were three aspects (intrinsic capacity, environment and social interaction) in terms of those indexes. Intrinsic capacity includes self-care, motor ability, ability of processing diseases, cognitive mental status and communication skills, and medical conditions. For example, self-care impairment was defined as the presence of at least one negative index, which indicated reducing ability to perform ADL, IADL [39] and frailty [40]. Motor ability included balance, falls, postural transition, arm stretching and mobility, while this capability impairment was evaluated by failing to complete one of them. Older people who seek medical treatment, exceptional treatment or use assistive device, without adopt self-treatment were regarded as a loss in the ability of processing disease. Cognitive mental status and communication skills were experience-dependent, and encompasses cognition, memory, vision, hearing, sadness and depression condition, as this ability impairment was defined to exist with at least one decline capability. The measurement of medical condition was derived from medical records where chronic diseases and physical disability are registered.
The assessment of functional capacity in environments includes both care resources and home setting for older adults. Care resources constituted of access of caregivers and living arrangement. Older people who lived alone and far away from their children or lacking of caregivers were defined as sources of care deficiency. Home settings as an environmental characteristic could be converted into capabilities, while limitation of it was defined as none of the elevator in a four-story apartment and accessibility.
Social interactions impairment results in activity limitations like restriction in interacting with friends, joining community club and community-related organization, and failure to help friends. A summary statistic of the variables applied for this study was presented in Table S1 in supplement.
Mortality
All deaths that occurred between the baseline measurement and the follow-up of CHARLS (2013–2018) were recorded. The occurrence of death was noted and checked with the death registration in the database (100% ascertainment for the current study sample).
Covariates
The study controlled for other functional ability attributes that affect mental and physical health. These included age, gender, marital status, place of residence(rural or urban), household per capita income, body mass index (BMI), educational level and numbers of children in the family. A summary statistic of the variables applied for this study was presented in supplementary Table S1.
Statistical analysis
Statistical data processing was performed using stata version 16.0. Based on the previously constructed dimensions and indexes, Latent class analysis (LCA) was performed to identify the latent classes of functional ability among older adults for the year 2011, 2013, 2015 in Mplus8.0. LCA models with 2–7 classes were performed to find the best fitting model. We reported the value of Akaike Information Criterion (AIC) and Bayesian information criterion (BIC) values for each model, where a lower score indicates a better fit and a higher entropy to evaluate the model fit [41]. If entropy is greater than 0.8, which means the accuracy of classification is more than 90%. Then, we used Bootstrap Likelihood Ratio Test (BLRT) and Lo-Mendell-Rubin adjusted (LMR-A) test to compare n-class model with n-1-class models, with smaller classes indicating more optimal. In addition to the model-fitting metrics, the simplicity and interpretability of the model were also considered. We also tested the measurement invariance of LCA p across sex, age and living region. The latent classes of functional ability for older adults were named according to the distinctive conditional probability of multidimensional indicators in each category [42].
Descriptive analysis was performed to present sociodemographic characteristics according to the five categories of the total samples. The univariate logistic regression model was used to examine the association between multidimensional functional indicators with mortality, and to further confirm the assigned values of 29 indicators (negative or positive). Bonferroni correction was used to determine significance for multiple tests.
To evaluate the association of the new functional classification with 7-year all-cause mortality and 7-year all-cause ADLs impairment, Cox proportional hazard models were fitted in R version 4.1.0. adjusted for age, sex, marital status, place of residence, household per capita income, BMI, educational level and numbers of children. Those who died or got ADLs impairment during follow-up were censored on the date of their death or impairment. Survivors were censored on the date of the last interview (approximately 7 years since the baseline). To demonstrate the differences in 7-year survival between the functional categories, survival curves were fitted in R version 4.1.0. Factor analysis was used to determine the percentage of mortality variability explained by the different variables of the study.
In addition, a competing risk analysis was performed by using the “cmprsk” R package to evaluate the risk of ADLs impairment from the year 2011 to 2013 for different functional categories, treating non-ADLs deaths, including, car accidents, accidents, natural disasters, poisonings, and injuries as competing events. This model was used as a sensitivity analysis to further support our conclusions.
Results
Classification of multi-dimensional functional ability and confirmatory analysis
Latent class analysis
A total of 5992 participants (49.97% men, 36.25% age over 70 years, 20.46% living in urban) were included in latent functional classes in 2011. The fitting indices of the different class models examined are shown in Table 1. The two-, three-, four- and five-class model yielded a significant LMR-A and BLRT result at p < 0.05. Both the six- and seven-class models yielded a significant LMR-A result at p < 0.05, but not a significant LMR-A result. The five-class model had both a significant of LMR-A and trustworthy BLRT result, with an entropy value higher than 0.8, and had the lowest AIC and BIC values among the five models considered. Thus, based on all of the fitting indices examined and on the interpretability of the symptom profiles of the classes (consistent with the study hypotheses), the five-class model was selected. In table S2, we compared the functional dependence rates measured by the internationally adopted classifications (ADL, IADL, and both ADL and IADL) with the results measured by the new classification in this study, and found that the new classification matched well with the functional decline rates. This indicates the new functional classification is reliable and accurate. The results also presented that the range of 58.39% to 76.22% of perfectly healthy or independent older adults measured by the traditional method is equivalent to the sum of the fourth and fifth categories of the new classification (70.65%), indicating that both the fourth and fifth categories belonged to the traditional health category. Together with the conditional probability distribution with reference to Table S3, we found that the fourth category had the best functional condition among all the categories, thus, the fourth category could be defined as “health”, which is similar to the WHO’s definition of health as “a state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity”.
In addition, an LCA for the 13- to 15-year follow-up period was applied to further verify the stability and scientific validity of this classification, as well observe the changes over time in the proportion of different categories of functional ability. As shown in Table 2, the 3-year LCA results showed that entropy is greater than 0.8, indicating that the accuracy of this classification is more than 90%. The values of AIC and BIC are small, indicating that the model fits well. Moreover, the BLRT test was passed in all three years. This illustrates that the number of categories set 5 was appropriate. Furthermore, it was found that the fifth category of older adults with functional limitation had the largest proportion of the population at each time point, although always in a dynamic process of change. The reason behind might be this group can be supplemented by transfers from other functional categories. Thus, the class 5 was considered to be an intermediate status between disability and health, which defined as “sub-disorder status”, with a very large scope for modulation and intervention, and provides important information and is of great relevance for delaying the progression of disability and preventing its occurrence.
A graphical depiction of conditional probability distribution of multidimensional functional indicators in each category was provided in Fig. 3, and stratified by gender, age and region (Supplementary Figs. S1, S2, S3, S4, S5, S6 and Tables S4, S5, S6). Based on comprehensive analysis of above results, we found that class 1 had a higher dysfunction rate in all items, except self-treatment, receiving medical services, exceptional treatment and hearing condition, as compared to class 2, "health", and "sub-disorder status". Moreover, an LCA for the 13- to 15-year follow-up period showed that both the proportion of older adults with the most severe functional decline in the first category and the best functional conditions in the fourth category decreased over time. The former possibly is due to an increase in mortality, while the latter might result from a transfer to other functional categories. Thus class 1 was named as "viability disorders". Likewise, class 3 had a poor function in all aspects and the severity, which is similar to that of class 1, especially in the medical treatment, the use of auxiliary devices, self-care, motor ability, medical condition, sources of care, home settings, social interactions, thus defined as "somatic functional disorders". Moreover, as these two categories are both in severe impairments in intrinsic capacity (e.g. ADL and IADL impairments), they are close to disability states. Class 2 had higher rates use of auxiliary devices, high probability of seeking medical treatment and special treatment conditions, while other aspects of function are in a good state, which is defined as "acute disease onset". However, the classes of "acute disease onset" and "somatic functional disorder" suggested that functional impairment in self-treatment, receiving medical services, exceptional treatment and hearing condition were both worse than the rest of three categories. The reason behind it might be the individuals in the "acute disease onset" more likely to get an acute injury to seek medical care and lose normal cognitive mental status in a sudden, and close to "viability disorder" for a short time period.
Characteristics of five categories
The description of sociodemographic characteristics and health behavior of 5 categories were shown in Table 3 and Fig. S7 in supplement, where “acute disease” class age 67.04 ± 5.98 years, BMI 22.91 ± 3.71 kg/m2, Systolic pressure 132.15 ± 24.93 mm/Hg, Diastolic pressure 74.01 ± 12.33 mm/Hg, hours of informal care 2.15 ± 19.17 h, hours of formal care 6.95 ± 48.15 h, Sleeping duration 6.07 ± 3.47 h), "somatic functional disorders" class (age 69.36 ± 7.25 years, BMI 22.74 ± 4.41 kg/m2, Systolic pressure 136.49 ± 23.85 mm/Hg, Diastolic pressure 75.39 ± 12.77 mm/Hg, hours of informal care 16.09 ± 52.7 h, hours of formal care 47.80 ± 95.17 h, Sleeping duration 5.33 ± 2.39 h), "viability disorders" (age 71.54 ± 7.63 years, BMI 22.60 ± 4.50 kg/m2, Systolic pressure 141.56.09 ± 30.50 mm/Hg, Diastolic pressure 76.73 ± 12.70 mm/Hg, hours of informal care 33.73 ± 92.07 h, hours of formal care 83.55 ± 143.61 h, Sleeping duration 5.60 ± 2.41 h), "sub-disorder status" (age 68.25 ± 6.64 years, BMI 22.84 ± 4.23 kg/m2, Systolic pressure 136.30 ± 25.04 mm/Hg, Diastolic pressure 75.00 ± 12.02 mm/Hg, hours of informal care 4.79 ± 29.99 h, hours of formal care 14.85 ± 59.44 h, Sleeping duration 6.09 ± 2.07 h), "health" (age 66.76 ± 5.88 years, BMI 23.04 ± 3.89 kg/m2, Systolic pressure 134.98 ± 24.78 mm/Hg, Diastolic pressure 75.25 ± 11.20 mm/Hg, hours of informal care 0.49 ± 8.17 h, hours of formal care 1.33 ± 14.18 h, Sleeping duration 6.63 ± 1.64 h).
Differences for trend across five categories over time
ANOVA and Chi-square analyses were performed to assess differences in sociodemographic characteristics, biological factors and health behavior across the classes identified in the LCA. The results of Table S7 in the supplement indicated that the five classes differed by age, gender, educational level, marital status, blood pressure, sleeping duration, life satisfaction, and self-rated health. In addition, Fig. S8 in supplement presented that the distribution of those major characteristics of the five categories changed synchronously with time, indicating that the classification results were relatively stable. The "somatic functional disorders" and "viability disorders" classes were in a higher proportion of females and older ages, higher blood pressure, shorter sleep duration, longer formal care duration, poorer life satisfaction, and higher rates of poor self-reported health status than other groups. In contrast, the proportion of men in the "health" class with the normal function was the highest. Notably, the proportion of illiteracy in the "viability disorders" was the highest, and the proportion of older adults with more than 5 children was the highest. It also can be seen from the supplementary Fig. S9 that the proportion of "somatic functional disorders", "viability disorders" and "sub-disorder status" among elderly female aged 70 and above who lived in the rural areas was relatively higher than males under 70 and living in cities and towns.
Development and validation of functional classification
The Multiple Cox regression analysis showed that after adjusting for the baseline characteristics, the effects of stratified variables on survival remained consistent with the primary analysis. The results of the univariate logistic analysis are presented in supplementary Table S8. On this model, with reports as hazard ratio (95% CI); male (HR 1.73, 95% CI 1.30–2.30; p < 0.001 vs female); with 1–3 children (0.64, 0.43–0.93; p = 0.028 vs with 6–7 children); inability to mobility(2.34, 1.58–3.46; p < 0.001 vs achievable mobility); use of assistive device(2.10, 1.50–2.93; p < 0.001 vs without use of assistive device); self-treatment (0.74, 0.56–0.97; p = 0.029 vs good cognition), chronic disease(1.71, 1.19–2.47;p = 0.004 vs without chronic disease), living in a same house with children (0.54, 0.33–0.88; p = 0.012 vs living in another province), living in a same dwelling or courtyard (0.57, 0.36–0.94; p = 0.028 vs living in another province), were independently associated with mortality (Fig. 4).
Survival analysis
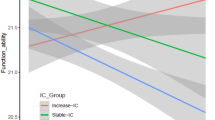
All variables used in this analysis were based on the 29 variables which used to construct a multi-dimensional functional indexes and the sociodemographic Characteristics. The results presented that the risk of mortality gradually increased toward the less functionally independent end of the classification. This indicates that the elucidation of a new functional classification composed of intrinsic capacity, environments, and social interaction indicators, is effective in stratifying the risk for mortality in older adults. The presence of impairment was associated with mortality (p < 0.001), in model adjusted for age, sex, marital status, place of residence, household per capita income, BMI, educational level and numbers of children (Fig. 5). To account for the differences in 7-year survival rates between the categories of the functional classification, survival curves were fitted. The overall mortality in 5992 older adults was 3.8%. Thirty-three of 685 older adults in the “viability disorder” class, 24 of 618 in “acute disease” class, 63 of 463 in “somatic functional disorder”, 44 of 2036 in “health”, 59 of 2190 in “sub-disorder status”, died within 7 years. The comparison of the survival differences between different categories suggested that the “health” and “sub-disorder status” survival was prolonged compared with “viability disorder” (P < 0.001), while there was no significant difference of “acute disease” and “somatic functional disorder” survival compared with “viability disorder” (Table S10 in supplement).
Survival progression according to the new functional classification during follow-up (Note. Cox proportional hazard model adjusted for baseline characteristics; class 1: viability disorders; class 2: acute disease; class 3: somatic functional disorders; class 4: health; class 5: sub-disorder status)
Analysis of ADLs impairments
The risk of 7-year ADLs impairments gradually increased toward the less functionally independent end of the classification, which is close to mortality patterns. The presence of functional decline among categories was associated with the presence of ADLs impairments, in models adjusted for baseline characteristics (Fig. S10 in supplement). To illustrate the differences in 7-year ADLs impairment rates among the functional categories, hazard curves were fitted. The overall ADLs impairment rate for 3971 older adults was 49.2%. Seventy of 82 older adults in “viability disorder”, 242 of 469 in “acute disease”, 93 of 123 in “somatic functional disorder”, 603 of 1695 in “health”, 896 of 1501 in “sub-disorder status”, got ADLs impairments within 7 years. The comparison of the differences in ADLs impairments of different categories suggested that the survival period of “sub-disorder status”, “health” and “acute disease” was prolonged compared with that of “viability disorder” (P < 0.001), but there was no significant difference of “somatic functional disorder” in ADLs impairments compared with “viability disorder” (Tables S9 and S10 in supplement).
Competitive risk modeling
The results of the competitive risk regression analysis showed that Log pseudolikelihood = -3012.434, Wald = 169.65, P < 0.001. There is a competing risk of accidental death with the ADLs outcome. Taking the category variables as an example, after controlling for sociodemographic variables such as age, gender, and marital status, the risk of ADLs impairments in class 2, class 4 and class 5 had 0.536, 0.268, and 0.514 times the risk of ADLs impairments than class 1, respectively, with a statistically significant difference (P < 0.05). This showed a consistency with the Cox risk regression, and it is a sensitivity analysis to further support our conclusions (Table S11 in supplement).
Discussion
Taken together, the results of this study showed that new classification of older adults with functional limitations was superior to the classic functional clusters because it initially identifies high-risk functional decline with limited intrinsic capacity, environments and social interaction, and provided information about underlying disability to guiding choice of intervention. Unlike previous attempts to dissect the functional heterogeneity of older adults [43], we applied comprehensive variables of key aspects of functional ability monitored in the older population. Therefore, this clustering can be easily applied to both existing functional independence cohorts (eg, from sports intervention), especially for older people in the home-cased community. An assessment tool for assigning the older people to specific clusters was being developed, provided that the appropriate variables have been measured.
A new functional classification effectively stratified the risk for mortality in older adults. Our classification composed of 8 dimensions and 29 indexes. As 5 exclusive categories representing the functional continuum, it can effectively stratify the risk for mortality in older adults, that is independent of age, sex, marital status, place of residence, household per capita income, BMI, educational level and numbers of children. These categories coming from a population-based study are not only an epidemiologic structure but may also help clinicians to implement diagnostic and therapeutic procedures, advanced care planning, and assign resources to older adult in the entire functional continuum, starting from normal function (category 4) to functional decline (categories 2 and 5), and then to disability (categories 1 and 3). Since disability is a common end-result of acute and chronic conditions in the older population [44, 45], the new classification could help solve the always difficult decision process around when to screen and take the subsequent interventions for osteoarthritis [46], depression [47], adverse events [48] and a major predictor to the years to survive, which now is age-determined. Other procedures that could benefit from the use of the new classification in the treatment decision-making process might be heart failure, chronic kidney disease, among others. Our work could be considered as a proof of concept, since the functional categories work across physical condition, care sources, different settings and social support, which was less taken into account previously.
The results presented that functional impairments in social support, home settings, sources of care, medical condition, movement, ability of processing diseases, cognition and communication, and self-care are health conditions independently associated with mortality. It is well known that the limitations of ADLs and IADLs are not the only two independent factors that identify the risk of other health-related adverse consequences for older adults, as well as institutionalization [49], hospitalization [49],quality of life [50], and health care costs [51]. Furthermore, in agreement with WHO healthy ageing framework we have described in previous work that the multidimensional functional index is the better predictor of adverse events in older adults, more predictive than ADLs or IADLs, and should be considered the cornerstone of geriatric medicine.
Other procedures could benefit from the use of the new classification in the decision-making of relevant policy implications, since health care and social service decisions may be adopted on the basis of validated stratification [52]. Our work could be considered as a proof of concept; In this category, the “health” category in the new classification is similar to the WHO’s definition of health as “a state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity” [53]; those in “sub-disorder status” is considered to be an intermediate status between disability and “health”, with a very large scope for modulation and intervention, and provides important information and is of great relevance for delaying the progression of disability and preventing its occurrence. However, “acute disease” class has a similar mortality risk as those that are “sub-disorder status”, and should be managed by primary care to take timely treatment and postoperative rehabilitation training to avoid the processing toward “viability disorder”, “somatic functional disorder” and “sub-disorder status”.
Thereafter, the high mortality and other risks of adverse outcomes of participants who got poor performances temporarily, but got better in other dimensions could make us include this category as a unique one “somatic functional disorder” coexists with the highest impairment on cognitive mental status and communication skills, and ability of processing diseases, but with lower self-care limitation than “viability disorder”. Older adults often relapse after treatment with a high disability rate [54]. The rehabilitation process after treatment should be a highlight to avoid permanently damaged in this group. "viability disorder" class was severely damaged in self-care, and it was unlikely to get better and move to other categories. The “somatic functional disorder” has more chronic diseases, such as arthritis, dementia and diabetes, indicating the need of more treatment [55, 56], while the "viability disorders" had more lethal diseases, including heart diseases and stroke, and demonstrating less period of hospitalization [57], which partly explains the longer but more morbid survival of “somatic functional disorder”. Therefore, the existing long-term care insurance should pay the most attention to those who lived longer, have complex but non-fatal health problems and need long-term intensified treatment, which consumes resources and lays a heavy burden on family and society.
Additionally, a subset of women, who had more children, with less education, higher blood pressure, longer sleep time, longer care time, and poorer life satisfaction are more likely to posted in “viability disorder” and “somatic functional disorder”. Special attention needs to be paid to these two categories of female elderly to improve their health literacy. For example, it is recommended that the government specifically set up community education activities, vital signs health monitoring facilities and public service activities for older adults with high risk of severe disability categories in order to shift to a better functional status and delay the progression of disability.
Nevertheless, there existed three limitations to this study that need to be addressed: the first important one is that it needs external validation in other countries and settings, although categories were created based on statistical analysis, latent class analysis and geriatric medicine knowledge and were thought to be a well-based proof of concept. The second is the hierarchical structure of these 5 categories of functional ability is itself controversial. However, we have adopted survival analysis and logistics regression analysis to explore the heterogeneity among the 5 categories to provide objective evidence, which may be more convincing. Furthermore, taking competing risks into account in the survival analysis of ADLs impairment, we applied compete risk model as a sensitivity analysis, to further support our conclusion. The third limitation is the exact overlap of weaker association signals and transition probability between categories needs to further explored. Nonetheless, an LCA for the 11- to 15-year follow-up period was added to observe the changes over time in the proportion of different functional categories. We consider to use empirical variables in larger cohorts to find out the possible relationships between categories in the future.
Conclusion
The combined multiple variables central to the development of functional independence is superior to measurement of only one or two aspects, ADL or IADL. The results showed that impaired self-care contributes to the highest mortality risk for older adults and should be regarded as the decisive factor in defining disability level. The “sub-disorder status” was considered to be an intermediate status between disability and health, with a very large scope for modulation and intervention, and provides important information and is of great relevance for delaying the progression of disability and preventing its occurrence. “Acute disease” should be given an urgent primary care to prevent the processing towards "viability disorders" or "somatic functional disorders" class. Close attention must be paid to the health and functioning of the "somatic functional disorders", so as to provide a sound and sustainable basis for planning health. Since the concept of functional decline is closely related to the deprivation of capabilities through restrictions on physical condition, environment and social interaction, based on capacity approach, this study provides a first step representing an important step towards a more precise and useful stratification for older adults in home-based community. Our classification also paves the way for analyzing the care needs and costs of different categories of older people and their future transferred probability among different clusters.
Availability of data and materials
CHARLS aims to set up a high quality, nationally representative and publicly available micro-database that provides a wide range of information about the households of the elderly and individual information on the older respondents and their spouses. CHARLS provides broad data that allows for analysis by multiple disciplines. All data stripped of private identifying information will be available for research use at no charge. National baseline data and a baseline national report are public on the CHARLS website and available from http://www.isss.pku.edu.cn/sjsj/charlsxm/index.htm.
Abbreviations
- ADL:
-
Activities of Daily Living
- IADL:
-
Instrument Activity of Daily Living
- BMI:
-
Body Mass Index
- LCA:
-
Latent class analysis
- CHARLS:
-
China Health and Retirement Longitudinal Study
- AIC:
-
Akaike Information Criterion
- BIC:
-
Bayesian information criterion
- BLRT:
-
Bootstrap Likelihood Ratio Test
- LMR-A:
-
Lo-Mendell-Rubin adjusted
References
WHO. Decade of healthy ageing: baseline report. 2021. (https://www.who.int/publications/i/item/9789240017900).
Beard JR, Officer A, de Carvalho IA, Sadana R, Pot AM, Michel J-P, et al. The World report on ageing and health: a policy framework for healthy ageing. Lancet. 2016;387(10033):2145–54.
Lowry KA, Vallejo AN, Studenski SA. Successful ageing as a continuum of functional independence: Lessons from physical disability models of ageing. Ageing dis. 2012;3(1):5–15.
Khan N, Hewson D, Randhawa G. Effectiveness of integrated chronic care interventions for older people with different frailty levels: a systematic review protocol. BMJ Open. 2020;10(9):e038437.
Fried LP, Guralnik JM. Disability in older adults: evidence regarding significance, etiology, and risk. J Am Geriatr Soc. 1997;45(1):92–100.
WHO. World report on ageing and health. Geneva: 2015 (https://apps.who.int/iris/handle/10665/186463 accessed 2 Sept 2020).
WHO. ICD-10: international statistical classifi cation of diseases and related health problems: tenth revision. 2nd ed. Geneva: World Health Organization; 2004. (https://apps.who.int/iris/handle/10665/42980 (accessed 1 Sept 2020).
Reynolds SL, Silverstein M. Observing the onset of disability in older adults. Soc Sci Med. 2003;57(10):1875–89.
Bleijenberg N, Zuithoff NPA, Smith AK, de Wit NJ, Schuurmans MJ. Disability in the Individual ADL, IADL, and Mobility among Older Adults: A Prospective Cohort Study. J Nutr Health Ageing. 2017;21(8):897–903.
Connolly D, Garvey J, McKee G. Factors associated with ADL/IADL disability in community dwelling older adults in the Irish longitudinal study on ageing (TILDA). Disabil Rehabil. 2017;39(8):809–16.
Verbrugge LM, Jette AM. The disablement process. Soc Sci Med (1982). 1994;38(1):1–14.
Hoogendijk EO, Romero L, Sánchez-Jurado PM, Flores Ruano T, Viña J, Rodríguez-Mañas L, et al. A New Functional Classification Based on Frailty and Disability Stratifies the Risk for Mortality Among Older Adults: The FRADEA Study. J Am Med Dir Assoc. 2019;20(9):1105–10.
Reynolds SL, Silverstein M. Observing the onset of disability in older adults. Sol sci med (1982). 2003;57(10):1875–89.
Marengoni A, von Strauss E, Rizzuto D, Winblad B, Fratiglioni L. The impact of chronic multimorbidity and disability on functional decline and survival in elderly persons. A community-based, longitudinal study. J Intern Med. 2009;265(2):288–95.
Stineman MG, Xie D, Pan Q, Kurichi JE, Zhang Z, Saliba D, et al. All-cause 1-, 5-, and 10-year mortality in elderly people according to activities of daily living stage. J Am Geriatr Soc. 2012;60(3):485–92.
Cosco TD, Stephan BCM, Brayne C. (Unsuccessful) binary modeling of successful ageing in the oldest-old adults: a call for continuum-based measures. J Am Geriatr Soc. 2014;62(8):1597–8.
Kuklys W. Amartya Sen’s Capability Approach. 2005.
Mitra S. The Capability Approach and Disability. J Disabil Policy Stud. 2006;16:236–47.
Burchardt T. Capabilities and disability: the capabilities framework and the social model of disability. Disabil Soc. 2004;19(07):735–51.
The national Prevention Agreement: a healthier Netherlands. The Hague: Netherlands Ministry of Health, Welfare and Sports; 2019. (https://www.government.nl/documents/reports/2019/06/30/the-national-prevention-agreement, accessed 4 Sept 2020).
WHO. International Classification of Functioning, Disability and Health (ICF). Geneva: World Health Organization; 2017. https://www.who.int/standards/classifications/international-classification-of-functioning-disability-andhealth.
Cerin E, Sit C, Zhang C, Barnett A, Cheung M, Lai P-C, et al. Neighbourhood environment, physical activity, quality of life and depressive symptoms in Hong Kong older adults: A protocol for an observational study. BMJ Open. 2016;6:e010384.
Cultural off er for seniors. [Kulturtilbud for seniorer]. Trondheim: Trondheim Kommue; 2019. https://www.trondheim.kommune.no/globalassets/10-bilder-og-filer/07-kultur-og-naring/kulturenheten/seniorkultur/kulturtilbud-for-seniorer-juli-desember-2019–2.pdf. Accessed 10 Sept 2020.
Sadana R, Banerjee A. WHO Consortium on Metrics and Evidence for Healthy Ageing. Metrics and evidence for healthy ageing. Bulletin of the World Health Organization. 2019;97(12):792–792A. https://doi.org/10.2471/BLT.19.246801.
Saito T, Izawa KP, Omori Y, Watanabe S. Functional Independence and Difficulty Scale: Instrument development and validity evaluation. Geriatr Gerontol Int. 2016;16(10):1127–37.
Kojima G. Frailty as a predictor of disabilities among community-dwelling older people: a systematic review and meta-analysis. Disabil Rehabil. 2017;39(19):1897–908.
Zhang L, et al. Prediction of the Number of and Care Costs for Disabled Elderly from 2020 to 2050: A Comparison between Urban and Rural Areas in China. Sustainability-Basel. 2020;12:2598.
de Castro-Cros M, Sebastian-Romagosa M, Rodríguez-Serrano J, Opisso E, Ochoa M, Ortner R, et al. Effects of Gamification in BCI Functional Rehabilitation. Front Neurosci. 2020;14:882.
Angulo J, El Assar M, Álvarez-Bustos A, Rodríguez-Mañas L. Physical activity and exercise: Strategies to manage frailty. Redox biol. 2020;35:101513.
Abizanda P, Romero L, Sánchez-Jurado PM, Martínez-Reig M, Alfonso-Silguero SA, Rodríguez-Mañas L. Age, frailty, disability, institutionalization, multimorbidity or comorbidity. Which are the main targets in older adults? J Nutr Health Ageing. 2014;18(6):622–7.
Abizanda P, Rodríguez-Mañas L. Function But Not Multimorbidity at The Cornerstone of Geriatric Medicine. J Am Geriatr Soc. 2017;65(10):2333–4.
Zhou M, Thayer WM, Bridges JFP. Using Latent Class Analysis to Model Preference Heterogeneity in Health: A Systematic Review. Pharmacoeconomics. 2018;36(2):175–87.
Vasquez CR, Gupta S, Miano TA, Roche M, Hsu J, Yang W, et al. Identification of Distinct Clinical Subphenotypes in Critically Ill Patients With COVID-19. Chest. 2021;160(3):929–43.
Garthus-Niegel S, Staudt A, Kinser P, Haga SM, Drozd F, Baumann S. Predictors and Changes in Paternal Perinatal Depression Profiles-Insights From the DREAM Study. Front psychiatry. 2020;11:563761.
Mitra S. The Capability Approach and Disability. J Disabil Policy Stud. 2006;16(4):236–47.
Zhao Y, Hu Y, Smith JP, Strauss J, Yang G. Cohort profile: the China Health and Retirement Longitudinal Study (CHARLS). Int J Epidemiol. 2014;43(1):61–8.
Chatterji S, Byles J, Cutler D, Seeman T, Verdes E. Health, functioning, and disability in older adults—present status and future implications. Lancet. 2015;385(9967):563–75.
Trani J-F, Bakhshi P, Brown D, Lopez D, Gall F. Disability as deprivation of capabilities: Estimation using a large-scale survey in Morocco and Tunisia and an instrumental variable approach. Soc Sci Med. 2018;211:48–60.
Lawton MP, Brody EM. Assessment of Older People: Self-Maintaining and Instrumental Activities of Daily Living1. Gerontologist. 1969;9(3_Part_1):179–86.
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in Older Adults: Evidence for a Phenotype. J Gerontol: Series A. 2001;56(3):M146–57.
Nylund KL, Asparouhov T, Muthén BO. Deciding on the Number of Classes in Latent Class Analysis and Growth Mixture Modeling: A Monte Carlo Simulation Study. Struct Equ Modeling. 2007;14(4):535–69.
Xiao J, Shi Z, Fang Y. Association Between Disability Trajectory and Health Care Service Utilization Among Older Adults in China. J Am Med Dir Assoc. 2021;22(10):2169-2176.e4.
Yang M, Ding X, Dong B. The Measurement of Disability in the Elderly: A Systematic Review of Self-Reported Questionnaires. J Am Med Dir Assoc. 2014;15(2):150.e1-9.
Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet (London, England). 2012;380(9859):2163–96.
Furukawa TA, Cipriani A, Cowen PJ, Leucht S, Egger M, Salanti G. Optimal Dose of Selective Serotonin Reuptake Inhibitors, Venlafaxine, and Mirtazapine in Major Depression: A Systematic Review and Dose-Response Meta-Analysis. Focus (Am Psychiatr Publ). 2020;18(2):211–9.
Butterfield NC, Curry KF, Steinberg J, Dewhurst H, Komla-Ebri D, Mannan NS, et al. Publisher Correction: Accelerating functional gene discovery in osteoarthritis. Nat Commun. 2021;12(1):3302.
Karnib N, El-Ghandour R, El Hayek L, Nasrallah P, Khalifeh M, Barmo N, et al. Lactate is an antidepressant that mediates resilience to stress by modulating the hippocampal levels and activity of histone deacetylases. Neuropsychopharmacology. 2019;44(6):1152–62.
Biscetti F, Nardella E, Bonadia N, Angelini F, Pitocco D, Santoliquido A, et al. Association between plasma omentin-1 levels in type 2 diabetic patients and peripheral artery disease. Cardiovasc Diabetol. 2019;18(1):74.
Kojima G. Frailty as a Predictor of Nursing Home Placement Among Community-Dwelling Older Adults: A Systematic Review and Meta-analysis. J geriatr phys ther (2001). 2018;41(1):42–8.
Kojima G, Iliffe S, Jivraj S, Walters K. Association between frailty and quality of life among community-dwelling older people: a systematic review and meta-analysis. J Epidemiol Community Health. 2016;70(7):716–21.
García-Nogueras I, Aranda-Reneo I, Peña-Longobardo LM, Oliva-Moreno J, Abizanda P. Use of Health Resources and Healthcare Costs associated with Frailty: The FRADEA Study. J Nutr Health Ageing. 2017;21(2):207–14.
Brown A, Barnes C, Byaruhanga J, McLaughlin M, Hodder RK, Booth D, et al. Effectiveness of Technology-Enabled Knowledge Translation Strategies in Improving the Use of Research in Public Health: Systematic Review. J Med Internet Res. 2020;22(7):e17274.
Grad FP. The Preamble of the Constitution of the World Health Organization. Bull World Health Organ. 2002;80(12):981–4.
Wang Z, Pan J, Wang L, Chen P. Clinical efficacy of comprehensive nursing in patients with cerebral hemorrhagic hemiplegia. Am J Transl Res. 2021;13(5):5526–32.
Hung WW, Ross JS, Boockvar KS, Siu AL. Recent trends in chronic disease, impairment and disability among older adults in the United States. BMC Geriatr. 2011;11(1):47.
Derby CA, Katz MJ, Lipton RB, Hall CB. Trends in Dementia Incidence in a Birth Cohort Analysis of the Einstein Ageing Study. JAMA Neurol. 2017;74(11):1345–51.
Enroth L, Raitanen J, Halonen P, Tiainen K, Jylhä M. Trends of Physical Functioning, Morbidity, and Disability-Free Life Expectancy Among the Oldest Old: Six Repeated Cross-Sectional Surveys Between 2001 and 2018 in the Vitality 90+ Study. J Gerontol: Series A. 2020;76(7):1227–33.
Acknowledgements
The authors would like to thank the National Bureau of statistics of the People's Republic of China, for its support with the data. We are also grateful to the National Natural Science Foundation and School of Public Health, Xiamen University, for their supporting to our study.
Disclaimers
Authors declare that they have no conflict of interests.
Funding
This study was supported by the National Natural Science Foundation of China (grant number 81973144) and the China Postdoctoral Science Foundation (grant number 2020M671949).
Author information
Authors and Affiliations
Contributions
Y H, LW Z and Y F worked together. Y H was in charge of the study design. Y H analyzed and interpreted the data, and drafted the manuscript. Y F and Y H participated in the statistical analysis and manuscript drafting. Y F and LW Z supervised and revised the manuscript. All authors have revised, read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The present study was approved by the Biomedical Ethics Review Committee of Peking University (IRB00001052–11015). Ethics approval for the use of the China Health and Retirement Longitudinal Study (CHARLS) data was obtained from the University of Newcastle Human Research Ethics Committee (H-2015–0290). All methods were conducted in accordance with the guidelines and regulations of the Declaration of Helsinki, and all the participants or their legal representatives gave their written informed consent before any study procedures began.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Han, Y., Zhang, L. & Fang, Y. Novel subgroups of functional ability in older adults and their associations with adverse outcomes. BMC Geriatr 22, 390 (2022). https://doi.org/10.1186/s12877-022-03081-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-022-03081-9