Abstract
Background
To enable delivery of high quality patient-centered care, as well as to allow primary care health systems to allocate appropriate resources that align with patients’ identified self-management problems (SM-Problems) and priorities (SM-Priorities), a practical, systematic method for assessing self-management needs and priorities is needed. In the current report, we present patient reported data generated from Connection to Health (CTH), to identify the frequency of patients’ reported SM-Problems and SM-Priorities; and examine the degree of alignment between patient SM-Priorities and the ultimate Patient-Healthcare team member selected Behavioral Goal.
Methods
CTH, an electronic self-management support system, was embedded into the flow of existing primary care visits in 25 primary care clinics and was used to assess patient-reported SM-Problems across 12 areas, patient identified SM-Priorities, and guide the selection of a Patient-Healthcare team member selected Behavioral Goal. SM-Problems included: BMI, diet (fruits and vegetables, salt, fat, sugar sweetened beverages), physical activity, missed medications, tobacco and alcohol use, health-related distress, general life stress, and depression symptoms. Descriptive analyses documented SM-Problems and SM-Priorities, and alignment between SM-Priorities and Goal Selection, followed by mixed models adjusting for clinic.
Results
446 participants with ≥ one chronic diseases (mean age 55.4 ± 12.6; 58.5% female) participated. On average, participants reported experiencing challenges in 7 out of the 12 SM-Problems areas; with the most frequent problems including: BMI, aspects of diet, and physical activity. Patient SM-Priorities were variable across the self-management areas. Patient- Healthcare team member Goal selection aligned well with patient SM-Priorities when patients prioritized weight loss or physical activity, but not in other self-management areas.
Conclusion
Participants reported experiencing multiple SM-Problems. While patients show great variability in their SM-Priorities, the resulting action plan goals that patients create with their healthcare team member show a lack of diversity, with a disproportionate focus on weight loss and physical activity with missed opportunities for using goal setting to create targeted patient-centered plans focused in other SM-Priority areas. Aggregated results can assist with the identification of high frequency patient SM-Problems and SM-Priority areas, and in turn inform resource allocation to meet patient needs.
Trial registration
ClinicalTrials.gov ID: NCT01945918.
Similar content being viewed by others
Background
Managing a chronic health condition, like type 2 diabetes, requires many ongoing patient activities occurring in parallel, e.g., eating a healthy diet, regular physical activity, and taking medications as directed [1, 2]. The sheer number of tasks can be overwhelming for individuals, with many of the required changes for many viewed as difficult to achieve [1, 3]. Given that almost all daily management decisions are made by patients outside of a healthcare setting with < 1% of an individuals’ time spent with their healthcare team [4], it is crucial to foster patient engagement and persistence in managing their chronic illness to achieve desired clinical goals [5, 6].
Self-Management Support (SMS) refers to the process of education and support provided to people with chronic health conditions and their families to help them understand their central role in managing their disease, to make informed decisions about care, and to engage in healthy behaviors [7,8,9]. While recognizing that patients often have several competing self-management needs (e.g., diet, exercise, stress, substance use, medication taking), in practice specific areas of patient self-management support are often siloed (e.g., nutrition or exercise), rather than prioritized in a meaningful way. Furthermore, clinicians and other members of the healthcare team often are unaware of patient priorities and resources, making it hard to align patient needs with clinician/healthcare team preferences [10, 11]. Related literature on shared decision-making points to the importance of considering patient priorities and collaboratively setting goals to enhance and sustain behavior change [12, 13]. However, only a small minority of patients are routinely asked about their self-management behaviors or preferences [9, 14, 15]. Furthermore, when screening of self-management behaviors does occur, it typically does not address the full range of required disease self-management behaviors and occurs with limited feedback to patients; which in turn constrains comprehensive collaborative care planning. For example, in Krist and colleagues’ review, they note that only 10–20% of smokers report being told to quit smoking by their clinician and less than 20% of obese patients report being told by their clinician that they are overweight [14, 15].
To enable delivery of high quality patient-centered care, as well as to allow primary care health systems to allocate appropriate resources that align with patients’ identified self-management problem areas and priorities, a practical, systematic method for assessing self-management needs and priorities is needed. Connection to Health (CTH) is an electronic SMS system for primary care that addresses these problems by recording patients’ self-management problems and challenges across a range of areas, assessing patient priorities, and facilitating structured action planning and follow-up through a process of shared goal setting (see www.conntectiontohealth.org to learn more). Thus, CTH provides a useful method for gathering information from patient cohorts about disease self-management in primary care. Such information can be useful for identifying high frequency self-management problems and patient priority areas, and in turn inform needs for adequate resources and care plans to address these needs and priorities.
In the current report, we utilize CTH data generated from patients with a chronic disease in 25 primary care clinics to further explore the following questions to enhance our understanding of SMS provision and gaps in primary care settings for patients with chronic disease: (1) Which areas of self-management do patients with chronic disease report the most difficulty?, (2) Which areas of self-management do patients tend to prioritize for behavior change? (3) Which areas of self-management do patients and Healthcare team members ultimately select as goals or targets of behavior change? (4) To what extent do these goals align with initial patient priorities?
Methods
Design
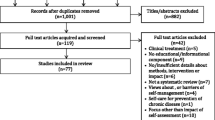
This report focuses exclusively on the patient-reported health assessment and priority-based goal setting data collected as part of a three-arm, cluster-randomized trial to evaluate strategies for implementing CTH in diverse primary care practices.
Practice sample
Twenty five primary care practices, 13 in Colorado and 12 in Northern California participating in the CTH study were randomized to the two study arms utilizing the electronic CTH program. Inclusion criteria for practices were family medicine or general internal medicine practices with a minimum of 80 patients with T2DM. A diverse set of practices of various sizes and organizational structures were recruited (i.e., private, system-owned, and safety net practices). Practices participated for 18 months, with participation encompassing December 2013 to March 2017 [16].
Procedure
The CTH program guides patients and members of the healthcare team through the following steps (Fig. 1): (1) patient assessment to identify self-reported management problems (SM-Problem), (2) identification of patient-reported management priorities (SM-Priorities), and (3) creation of an action plan and follow up process with a member of the healthcare team to select a self-management goal. In face to face meetings with a member of their healthcare team, patients were introduced to the program through an iPad logged into the CTH system. Patients were asked to complete a web-based, electronic assessment of their current self-management in twelve SMS areas. Based on national guidelines and validated scoring, automated algorithms flagged problem areas for patients and a member of the healthcare team, with recommendations for change. After patients reviewed a summary of their assessment results, the program prompted them to prioritize up to two areas they wished to discuss with a member of the healthcare team. Patients and a member of the healthcare team then met to review the assessment results, select a goal and develop a subsequent action plan to achieve the goal.
Given the overall aims of the larger study, clinics generally focused on working with patients with type 2 diabetes, although they were also encouraged to utilize CTH with patients diagnosed with other chronic illnesses. There were no patient eligibility criteria. As part of the study design, all practice members (clinicians and staff) participated in two hours of training including an introduction to SMS and an interactive tutorial on the CTH system including a practice dyad using the summary report and engaging in goal setting. Practices selected the subset of healthcare team members to use CTH in patient encounters. The majority (> 90%) of those team members identified as community health workers (CHWs), health educators, panel managers, chronic care managers, volunteers, or similar roles; while a small portion identified as a nurse or Certified Diabetes Educator (CDE) or primary care physician. The research protocol was approved by the University of Colorado at Denver and the University of California, San Francisco institutional review boards who waived any patient consent given the data presented were collected and used at the point of care and provided to the research team in de-identified form.
Measures
Congruent with policy recommendations from the Society of Behavioral Medicine [17], the CTH assessment utilized brief scales that are reliable, sensitive to change, and age appropriate to assess 12 areas of patient self-management [18]. Each area of self-management was automatically scored based on national guidelines with results for each presented in three categories: Green (no need for change), Yellow (moderate level/need for change), and Red (high level/need for change). Areas of SMS, items and cut-points for scoring appear in Table 1 for each of the twelve SMS areas including: BMI (based upon self-reported height and weight), diet (servings of fruits and vegetables, salt, fat, sugar sweetened beverages [19,20,21], physical activity (frequency and duration of weekly moderate to strenuous physical activity; [22], missed medications (number of days missed in past 7 days; [23,24,25] tobacco and alcohol use (frequency of use and binge drinking; [26,27,28,29], health-related distress (5 items based on the Diabetes Distress Scale, [30, 31] presence of a recent major life stressor) [32], and depression symptoms (assessed with the PHQ8); [33, 34]. Frequency of each of the 12 areas by category (green, yellow, red) along with priorities for discussion and ultimate self-management goal were recorded. Additional patient demographics (age group, gender, race, education level, and reported chronic diseases) were additional captured to describe the sample.
Data analysis
Descriptive statistics were computed to review item and scale distributions and frequencies by health area. Chi-square tests or t tests, as appropriate, tested for differences between completers of priority and goal setting versus non-completers and associations with patient characteristics. Frequencies of SM-Priorities were examined contingent upon the presence of a SM-Problem in that area. Goals selected during action planning were examined in cross-tabs to document frequency of agreement. Generalized Linear Mixed Models (GLMM) examined frequencies adjusting for clustering by clinic as well as patient characteristics associated with the outcomes of interest. Sensitivity analyses using mixed models examined select planned patient subgroups for select common chronic diseases with the same adjustment factors. Data were analyzed using SPSS v.19 software.
Results
The majority of the 25 participating clinics were Community Health Centers (n = 18; 72%), with remaining split between independent practices or practices that were part of an integrated healthcare system; and 16 (64%) had achieved NCQA PCMH recognition. Clinics employed on average 6.8 (+ 3.7) FTE clinicians and served 37% (+ 20%) patients on Medicaid.
A total of 446 patients across the 25 clinics completed the health assessment (n = 287 for Colorado and n = 159 for California clinics). Participants were on average 55.4 (+ 12.6) years of age, 58.5% were female, and 52.6% had an education level < a high school diploma (Table 2). The majority identified themselves as Hispanic (42.6%) or non-Hispanic white (40.1%). In line with expectations for primary care, the most common chronic illnesses reported included diabetes (67.5%), hypertension (58.5%), and hypercholesterolemia (55.8%). All patients identified themselves as having at least one chronic illness, with 78.5% identifying two or more co-morbid chronic illnesses. Three-quarters of the sample (n = 336) prioritized one (n = 85) or two (n = 251) areas of self-management to discuss with their healthcare team (SM-Priorities). Of these, 74.7% (n = 227) went on to select a self-management goal and to create an action plan for change. Key reasons reported by member of the healthcare team for patients not completing action plans were clinic-based – primarily insufficient time due to work flow. There were no significant differences between patients who did not prioritize health areas or did not create an action plan compared to those who did on the basis of any assessed patient characteristic, reported health condition, or type of self-management need.
Self-management problem areas (SM-problems)
The frequency of patient-identified SM-Problems for each of the 12 areas is summarized in Fig. 2, with the most frequent areas targeting weight loss (88.8%), eating more fruits or vegetables (75.8%), reducing dietary fat (72.6%), increasing physical activity (71.5%), and high levels of health-related distress (63.7%).
Of the 12 SM-Problem areas, on average patients reported 6.0 (+ 2.1) areas of need for change (red) and 1.2 (+ 1.0) areas of moderate need for change (yellow). No patients reported zero SM-Problem areas, and only 1.3% reported one SM-Problem area. Thus, the average number of reported problem areas per patient was quite high.
Patient-reported priorities for self-management (SM-priorities)
Frequencies of patient-selected SM-Priorities, among those endorsing a given a SM-Problem, are displayed in Fig. 3. The frequency of prioritized SMS problems was highly variable across the 12 areas: the most frequent were weight loss (36.7%), fat in diet (35.1%), and depression symptoms 37.2%; the least frequent were decreasing sugar-sweetened drinks (8.1%), salt (15.4%), alcohol (16.3%) and health-related distress (17.5%). Considering rates of needs and priorities in tandem, it is interesting to note that weight loss and lowering fat in diet were self-management areas that were frequently endorsed by patients as both a SM-Problem and SM-Priority. Notably, although health-related distress was reported as an SM-Problem by over two-thirds of the sample, it was only identified as an SM-Priority for 17.5% of those individuals. Likewise, while three-quarters of participants reported a need for additional fruits/vegetables in their diet, only 21.1% of these individuals prioritized this area.
Goal setting and alignment with patient-reported SM-priorities
Overall, 72.7% of the sample created an action plan with a member of the healthcare team that focused on a goal in line with one of the patient-selected SM-Priorities. However, the frequency of alignment between action plan goals and patient SM-Priority areas varied greatly depending on SM-Problem area (Fig. 4). Of the patients who created action plans with an SM-Priority of weight loss (n = 76), almost all (96%) went on to create an action plan goal specifically targeting their weight or a behavior intended to directly result in weight loss (physical activity, specific changes to diet). Patient SM-Priorities of physical activity (n = 51) were also frequently translated into action plans that focused on physical activity (56.7%). However, concordance between patient SM-Priorities and their ultimate action plan goals was considerably lower for the remaining SM-Problem areas (Fig. 4). Strikingly, of the patients who prioritized health-related distress and medication taking, virtually none developed an action plan with their HCP that targeted these areas (2.6 and 0% respectively). When action plan goals did not align with any patient SM-Priorities, goals were typically made around physical activity, weight loss or diet. Of the patients who prioritized health-related distress, 50% made a diet/weight loss goal and 26% made a physical activity goal; with similar results for those who prioritized medication taking (56% made a diet/weight goal and 19% made a physical activity goal).
Additional analyses
There was no consistent pattern of association between any of the recorded patient demographic factors (age, gender, race, education level) and the measures of interest including the frequency of SM-Problems and SM-Priorities or alignment between SM-Priorities and Goal selection with the exception of patient age. Compared to older adults (age 40–64, 65 or older), younger adults (19–39 years) were more likely to report SM-Problems including: missed medications (24.0 and 33.6% vs. 51.0% p = .004), high levels of alcohol use (10.4 and 7.3% vs. 33.3% p < .001), and tobacco use (18.4 and 6.3% vs. 27.5%, p = .002). In addition, stress was elevated for the 19–39 year old (58.8%) and 40–64 year old groups (56.2%) relative to the oldest age group (37.5%, p = .004). Adjusting for clustering by clinic and patient age, virtually identical results were found for the frequency of SM-Problems, SM-Priorities, and degree of alignment with Goals. Likewise, analyses limited to each of the three most common chronic illnesses (diabetes, hypertension, and hypercholesterolemia) yielded similar results.
Discussion
This study assessed patient reported SM-Problems, SM-Priorities, and Patient-Healthcare team member Goal Selection. The current findings suggest that patients with chronic disease in primary care experience multiple competing SM-Problems. On average, patients reported experiencing simultaneous challenges in 7 out of the 12 SM-Problems, with less than 2% of patients reporting only one single SM-Problem. In line with related literature, the frequency for several SM-Problems was elevated among relatively younger adults living with chronic disease (age 19–39 years) [35, 36]. Patient SM-Priorities were variable across the self-management areas with the most frequently prioritized areas being weight loss, decreased fat in diet, and depression symptoms. Ultimate Patient-Healthcare team member Goal selection were aligned well with patient SM-Priorities when patients prioritized weight loss or physical activity, but suggested potential misalignment in other self-management areas, such as stress/health-related distress, medication taking, and tobacco/substance use.
The current findings suggest that patients with chronic disease in primary care are able to report on their self-management behaviors and to prioritize them among their often competing self-management problems or areas of challenge. In aggregate, this type of data can assist with the identification of high frequency patient SM-Problems and SM-Priority areas, and in turn to inform resource allocation as well as opportunities to better understand why patients generally are not viewing specific SM-Problems as a priority. Second, findings comparing ultimate goal selection to SM-Priorities illustrate areas of alignment vs. potential misalignment and missed opportunities for using goal setting to create targeted patient-centered plans. The lopsided use of goal setting for the inter-related areas of weight loss, diet, and physical activity is not surprising given the roots of action planning that have traditionally focused on these behavioral lifestyle elements [37]. However, results suggest that even when presented with alternative patient SM-Priorities, members of the healthcare team by and large do not expand their use of goal setting or planning to these other areas of self-management, such as stress/health-related distress, medication taking, and substance use. Findings can inform opportunities and discussion for creating greater alignment with patient priorities in these self-management areas.
Viewing patients’ SM-Problems, SM-Priorities and ultimate goal selection together, several notable patterns emerge. Weight loss and physical activity emerged as the most common areas of patient SM-Problems, with high rates of patient SM-Prioritization and translation into action plan goals. This concordance, however, did not extend beyond these two areas: in contrast, health-related distress, conceptually distinct from depression and more closely tied with chronic disease health outcomes [38, 39], was one of the most common SM-Problems, but was chosen as a SM-Priority by relatively few patients and rarely emerged as a targeted goal. Finally, none of the 19% of patients who selected taking their medications more regularly as an SM-Priority, a key consideration in chronic disease management, ultimately created an action plan goal in this area. Thus, we note specific SM-Problems were not often being viewed as SM-Priorities, and even among those that did prioritize these areas, rarely were translated into Patient-Healthcare team member goals.
Patient-reported SM-Priorities were in general distributed across the self-management tasks, highlighting the diversity of patient needs. Patients’ selection of SM-Priorities among their SM-Problems might have been influenced by multiple factors related to: (1) individual preferences and/or, (2) perceptions of their healthcare team. Other potential explanations were offered by a recent patient advisory group from five participating primary care clinics. They suggested that patients may be more likely to prioritize a given SM-Problem if they view it as: relatively easy or realistic to tackle, important, particularly pressing, comfortable to discuss, and/or something they have been told or think they “should” work on. Additional contributing patient perceptions of healthcare teams factors may include: patient comfort with the healthcare team member, patient viewing the healthcare team member as competent or potentially positioned to assist given their role or experience, or an area the patient believes is a clinician/healthcare team priority.
Patient centered care and evidence in support of shared decision making emphasizes the importance of patients’ input and voice in care discussions [12, 13]. The lack of concordance between patient SM-Priorities and ultimate action plan goal selection for areas outside of weight loss, diet and exercise may reflect a lack of collaborative decision making driven by healthcare team member lack of knowledge or comfort working with patients around specific areas of self-management. Some healthcare team members may not feel amply trained to work with patients around certain issues, judge that they are best addressed by other members of the healthcare team, or best handled by a referral to a specialist, especially given the individuals selected by practices in the current study (majority in lay healthcare team roles). On the other hand, this lack of concordance could at times reflect healthcare team members’ asserting clinical judgement in concert with patients, in which an action plan veering away from a patient SM-priority could reflect a collaborative process by which the patient and HCP arrive at a new goal together through discussion. Future work that allows for observations of patient-healthcare team member interactions around goal setting in light of SM-Priorities could further contextualize the findings.
The current study has multiple strengths, including a diverse set of health care settings, a diverse group of patients, and a comprehensive yet pragmatic assessment of patient SM-Problems and SM-Priorities. Nonetheless, several limitations are noteworthy. First, patients within clinics were not randomly selected, such that there may have been some bias within clinics regarding patient selection. Second, all variables, including chronic disease status and BMI, were limited to self-report. Confirmation using laboratory and chart data deserve further attention. Third, data presented are limited to only the information entered into the non-EHR integrated CTH program. This did not allow access to clinical referrals or documentation of additional discussions or health plans made with other members of the care team.
Conclusion
Results of the current study add to our understanding of the multiple and co-occurring SM-Problems and SMS needs that patients along with their healthcare teams s struggle to tackle together. While patients showed great variability in their SM-Priorities regarding self-management tasks, the resulting action plan goals that patients created with their healthcare team member show a striking lack of diversity, with a lopsided focus on weight loss and physical activity at the cost of addressing a diversity of other important patient-reported SM-Problems. There are many reasons why patient SM-Priorities are not ultimately selected as the focus on action plans and further work is needed to understand the likely multifaceted reasons from both patients’ and healthcare team members’ perspectives.
Availability of data and materials
Data generated and analyzed for the current study will be available from the corresponding author on reasonable request.
Abbreviations
- CTH:
-
Connection to Health
- PCMH:
-
Patient-centered medical home
- SM-Priorities:
-
Self-management priorities
- SM-Problems:
-
Self-management problems
- SMS:
-
Self-management support
References
DiMatteo MR. Variations in patients' adherence to medical recommendations: a quantitative review of 50 years of research. Med Care. 2004;42:200–9.
Ruggiero L, Glasgow R, Dryfoos JM, Rossi JS, Prochaska JO, Orleans CT, Prokhorov AV, Rossi SR, Greene GW, Reed GR, Kelly K, Chobanian L, Johnson S. Diabetes self-management. Self-reported recommendations and patterns in a large population. Diabetes Care. 1997;20:568–76.
Fisher L, Hessler DM, Polonsky WH, Mullan J. When is diabetes distress clinically meaningful?: establishing cut points for the diabetes distress scale. Diabetes Care. 2012;35:259–64.
Chen L, Farwell WR, Jha AK. Primary care visit duration and quality. Arch Intern Med. 2009;169(20):1866–72.
Jordan JE, Briggs AM, Brand CA, Osborne RH. Enhancing patient engagement in chronic disease self-management support initiatives in Australia: the need for an integrated approach. Med J Aust. 2008;189:S9–S13.
Coulter A, Ellins J. Effectiveness of strategies for informing, educating, and involving patients. BMJ. 2007;335:24–7.
Taylor SJC, Pinnock H, Epiphaniou E, Pearce G, Parke HL, Schwappach A, Purushotham N, Jacob S, Criffiths CJ, Greenhalg T, Sheik A. A rapid synthesis of the evidence on interventions supporting self-management for people with long-term conditions: PRISMS – practical systematic review of self-management support for long-term conditions. Health Serv Deliv Res. 2014;2:53.
Powers MA, Bardsley J, Cypress M, Duker P, Funnell MM, Fischl AH, Maryniuk MD, Siminerio L, Vivian E. Diabetes self-management education and support in type 2 diabetes: a joint position statement of the American Diabetes Association, the American Association of Diabetes Educators, and the academy of nutrition and dietetics. Diabetes Educ. 2017;43(1):40–53.
Beck J, Greenwood DA, Blanton L, Bollinger ST, Butcher MK, Condon JE, Cypress M, Faulkner P, Fischl AH, Francis T, Kolb LE. 2017 national standards for diabetes self-management education and support. Diabetes Educ. 2018;44(1):35–50.
Krist AH, Tong ST, Aycock RA, Longo DR. Engaging patients in decision-making and behavior change to promote prevention. Stud Health Technol Inform. 2017;240:284–302.
Barry MJ, Edgman-Levitan S. Shared decision making — the pinnacle of patient-centered care. N Engl J Med. 2012;366:780–1.
Ludman E, Katon W, Bush T. Behavioural factors associated with symptom outcomes in a primary care-based depression prevention intervention trial. Psychol Med. 2003;33:1061–70.
Stacey D, Légaré F, Col NF, Bennett CL, Barry MJ, Eden KB, Holmes-Rovner M, Llewellyn-Thomas H, Lyddiatt A, Thomson R, Trevena L, Wu JHC. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2014(1):1–334.
Leverence RR, Williams RL, Sussman A, Crabtree BF, Clinicians RN. Obesity counseling and guidelines in primary care: a qualitative study. Am J Prev Med. 2007;32:334–9.
Rothemich SF, Woolf SH, Johnson RE, Burgett AE, Flores SK, Marsland DW, Ahluwalia JS. Effect on cessation counseling of documenting smoking status as a routine vital sign: an ACORN study. Ann Fam Med. 2008;6:60–8.
Dickinson WP, Dickinson LM, Jortberg BT, Hessler DH, Fernald DH, Fisher L. A protocol for a cluster randomized trial comparing strategies for translating self-management support into primary care practices. BMC Fam Pract. 2018;19:126.
Glasgow R, Emmons KM. The public health need for patient-reported measures and health behaviors in electronic health records: a policy statement of the Society of Behavioral Medicine. Transl Behav Med. 2011;1:108–9.
Paxton AE, Strycker LA, Toobert DJ, Ammerman AS, Glasgow RE. Starting the conversation performance of a brief dietary assessment and intervention tool for health professional. Am J Prev Med. 2011;40:67–71.
Jilcott SB, Keyserling TC, Samuel-Hodge CD, Johnston LF, Gross MD, Ammerman AS. Validation of a brief dietary assessment to guide counseling for cardiovascular disease risk reduction in an underserved population. J Am Diet Assoc. 2007;197:246–55.
Moshfegh A, Goldman J, Ahuja J, Rhodes D, LaComb R. What We Eat in America, NHANES 2005–2006: Usual nutrient intakes from food and water compared to 1997 Dietary Reference Intakes for Vitamin D, Calcium, Phosphorous, and Magnesium. U.S. Department of Agricuture. Agricultural Research Service. 2009. https://www.researchgate.net/publication/280319360_What_We_Eat_in_America_NHANES_2005-2006_Usual_Nutrient_Intakes_from_Food_and_Water_Compared_to_1997_Dietary_Reference_Intakes_for_Vitamin_D_Calcium_Phosphorus_and_Magnesium. Accessed 4 Dec 2018.
Toobert DJ, Hampson SE, Glasgow RE. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care. 2000;23:943–50.
Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, Pratt M, Ekelund U, Yngve A, Sallis JF, Oja P. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–95.
Bender BG, Bartlett SJ, Rand CS, Turner C, Wamboldt FS, Zhang L. Impact of interview mode on accuracy of child and parent report of adherence with asthma-controller medication. Pediatrics. 2007;120:e471–7.
Bender BG, Rankin A, Tran ZV, Wamboldt FS. Brief-interval telephone surveys of medication adherence and asthma symptoms in the childhood asthma management program continuation stud. Ann Allergy Asthma Immunol. 2008;101:382–6.
Horne R, Weinman J. Patients' beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. J Psychosom Res. 1999;47:555–67.
Dawson DA, Grant BF, Li TK. Quantifying the risks associated with exceeding recommended drinking limits. Alcohol Clin Exp Res. 2005;29:902–8.
Helping patients who drink too much: A clinician's guide, 5th Edition, US Department of Health and Human Services. 2005. https://pubs.niaaa.nih.gov/publications/practitioner/cliniciansguide2005/clinicians_guide.htm. Accessed 4 Dec 2018.
Ory MG, Jordan PJ, Bazzarre T. The behavior change consortium: setting the stage for a new century of health behavior-change research. Health Educ Res. 2002;17:500–11.
Behavioral Risk Factor Surveillance System State Questionnaire, Centers for Disease Control and Prevention. 2004. https://www.cdc.gov/brfss/questionnaires/index.htm. Accessed 4 Dec 2018.
Polonsky WH, Fisher L, Earles J, Dudl J, Lees J, Mullan J, Jackson RA. Assessing psychosocial distress in diabetes: development of the diabetes distress scale. Diabetes Care. 2005;28:626–31.
Fisher L, Glasgow RE, Mullan RT, Skaff MM, Polonsky WH. Development of a brief diabetes distress screening instrument. Ann Fam Med. 2008;6:246–52.
Pearlin LI, Lieberman MA, Menaghan EG, Mullan JT. The stress process. J Health Soc Behav. 1981;22:337–56.
Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. 2009;114:163–73.
Kroenke K, Spitzer RL, Williams JB. The patient health Questionnaire-2: validity of a two-item depression screene. Med Care. 2003;41:1284–92.
Hessler DM, Fisher L, Mullan JT, Glasgow RE, Mashrani U. Patient age: a neglected factor when considering disaear management in adults with type 2 diabtes. Patient Educ Couns. 2011;85:154–9.
Hesler DM, Fisher L, Naranjo D, Mashrani U. Young adult African American patients with type 2 diabetes: a high risk patient sub=group with few supports for good diabetes management. J Health Psychol. 2012;17:535–44.
Lorig K, Laurent D, Plant K, Krishnan E, Ritter PL. The components of action planning and their associations with behavior and health outcome. Chronic Illn. 2014;10:50–9.
Fisher L, Skaff MM, Mullan JT, Arean P, Mohr D, Masharani U, Glasgow R, Laurencin G. Clinical depression versus distress among patients with type 2 diabetes: not just a question of semantics. Diabetes Care. 2007;3:542–8.
Hessler D, Fisher L, Strycker LA, Arean PA, Bowyer V. Causal and bidirectional linkages over time between depression and diabetes regimen distress in adults with type 2 diabetes. Diabetes Res Clin Pract. 2015;108:360–6.
Acknowledgements
We wish to acknowledge the dedication and efforts of all participating clinics –including leadership and staff as well as participating patients, as well as the San Francisco Bay Area Collaborative Research Network (SF Bay CRN, sfbaycrn.org) and the State Networks of Colorado Ambulatory Practices & Partners (SNOCAP) PBRN for their support and assistance with clinical site recruitment and engagement.
Funding
Funding for this work was supported by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK Award Number 1R18DK096387). This funding source had no role in the design and execution of this study, and will not have any role during analyses, interpretation of the data, or decision to submit results.
Author information
Authors and Affiliations
Contributions
All authors contributed to the preparation of the grant proposal and read and approved the final manuscript. WPD, LF, LMD, and DMH conceived of the study. WPD, LMD, DMH, LF, BMJ, and DMH initiated the study design, and all authors were involved in the implementation of the study design. DMH, WPD, and LF were grant holders. DMH, VB, and LMD provided statistical expertise and conducted the primary statistical analysis. BK, MS, and DF reviewed and edited the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Reviewed and approved by the University of California, San Francisco Human Research Protection Program Institutional Review Board (IRB) #12–10010 and the Colorado Multiple Institutional Review Board, Protocol #12–0645, Final Protocol Version v9-7-2014. Waiver of documented consent was granted by these named IRBs for the portions of the study presented in the current manuscript. Verbal or written consent was obtained for other portions of the study protocol not presented in the current manuscript pertaining to data collection from clinical site staff and clinicians.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Hessler, D.M., Fisher, L., Bowyer, V. et al. Self-management support for chronic disease in primary care: frequency of patient self-management problems and patient reported priorities, and alignment with ultimate behavior goal selection. BMC Fam Pract 20, 120 (2019). https://doi.org/10.1186/s12875-019-1012-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12875-019-1012-x