Abstract
Background
Out-of-hospital Emergency Medical Services (OHEMS) require fast and accurate assessment of patients and efficient clinical judgment in the face of uncertainty and ambiguity. Guidelines and protocols can support staff in these situations, but there is significant variability in their use. Therefore, the aim of this study was to increase our understanding of physician decision-making in OHEMS, in particular, to characterize the types of decisions made and to explore potential facilitating and hindering factors.
Methods
Qualitative interview study of 21 physicians in a large, publicly-owned and operated OHEMS in Croatia. Data was subjected to an inductive content analysis.
Results
Physicians (mostly young, female, and early in their career), made three decisions (transport, treat, and if yes on either, how) after an initial patient assessment. Decisions were influenced by patient needs, but to a greater extent by factors related to themselves and patients (microsystem), their organization (mesosystem), and the larger health system (macrosystem). This generated a high variability in quality and outcomes. Participants desired support through further training, improved guidelines, formalized feedback, supportive management, and health system process redesign to better coordinate and align care across organizational boundaries.
Conclusions
The three decisions were made complex by contextual factors that largely lay outside physician control at the mesosystem level. However, physicians still took personal responsibility for concerns more suitably addressed at the organizational level. This negatively impacted care quality and staff well-being. If managers instead adopt a learning orientation, the path from novice to expert physician could be more ably supported through organizational demands and practices aligned with real-world practice. Questions remain on how managers can better support the learning needed to improve quality, safety, and physicians’ journey from novice to expert.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Emergency Medical Services (EMS) require fast and accurate on-site assessment of patients that present with varied and unique medical, personal, and environmental circumstances [1]. This necessitates resourcefulness and flexibility in clinical judgment regarding immediate patient care as well as multiple operational and resource-management decisions made under pressure and based on limited information [2]. The level of clinical judgment required is partly determined by the EMS model employed. Whereas the Anglo-American “scoop-and-run” pre-hospital EMS (PEMS) paramedic-based approach limits in-field treatment and intervention, the Franco-German out-of-hospital EMS (OHEMS) approach employs a “stay-and-stabilize” strategy that often requires emergency physician support [3].
Working in a context that is volatile, uncertain, complex, and ambiguous is inherently risky [4]. Incorrect decisions may lead to medical errors and adverse events, which present a threat to clinical outcomes and both patient and provider safety [5]. It is clear that professional training alone is not enough to mitigate the risks, which has led to the application of team-training and decision-support tools, e.g. checklists, guidelines, protocols, and standard operating procedures (SOPs) in health care [6, 7]. However, there is a high variation (7.8–95%) in their use [8] such that protocols with proven effectiveness are not applied, while practices proven to be less effective and even potentially harmful persist [9]. Guideline compliance in prehospital settings is influenced by multiple factors, including perceptions of their quality and value, practitioners’ age, experience, and willingness to take risks [10], unique patient and organizational circumstances [8], and poor strategies for creating and disseminating guidelines [9]. In light of these insights, there is a need for research that identifies risks associated with patient care decisions in OHEMS settings and what influences adherence to guidelines or implementation strategies that improve adherence [11, 12].
Research on decision-making in OHEMS settings has primarily focused on paramedics, nurses, or a combination of EMS professionals in the context of: resuscitation [13,14,15], conveyance [2, 16,17,18,19], triage [20, 21], ethical issues [22, 23], and clinical judgment [1, 24, 25]. While exploring decision-making from different angles, these studies consistently suggest that the complexity of such highly contextual and multifactorial work processes require a reassessment of education and training programs, guidelines, and feedback mechanisms to improve performance and patient safety. Moreover, the continuous growth in demand and complexity of patient conditions, which reflect the needs of an aging society and chronic and palliative patients, can lead to questions about the capability of paramedic-led teams and calls to explore alternative care pathways and reevaluate EMS design [17, 26, 27].
There is less research on physician decision-making in OHEMS, which has mainly studied resuscitation [28, 29], care of palliative patients [30, 31], duration of interventions [32], and the impact of cognitive and non-technical skills on care quality [33, 34]. As physicians receive a broader education and acquire a wider set of skills and competencies, there is a greater decision-making scope. In addition, given the responsibility they bear for their patients, it is important to better understand the types of decisions they make, the kind of support that they need beyond existing guidelines, and the implications for patient safety. Therefore, the aim of this study was to increase our understanding of physician decision-making in out-of-hospital emergency medical services, to characterize the types of decisions made, and to explore potential facilitating and hindering factors.
Methods
Study design
We chose a qualitative approach as it was deemed the most appropriate to gain in-depth insights into personal lived experiences, behaviors, and perspectives [35], in a context where shame-and-blame of individual physicians is a commonplace cultural norm [36]. We report in accordance with the Consolidated Criteria for Reporting Qualitative Studies (COREQ) checklist (Appendix 1) [37].
Study setting
We conducted the study at a large regional OHEMS organization in Croatia. In 2021, the organization served a population of 769,944, employed 241 ambulance staff, answered 150,000 phone calls, and conducted 75,714 field interventions, of which 83% were of low acuity.
Croatian OHEMS are offered as a publicly owned, financed, and operated regional public service, coordinated by the Croatian Institute for Emergency Medicine [38]. The Institute provides guidelines, algorithms, and procedural suggestions for medical conditions [39], most often not tailored to the specific context of operation (Appendix 2). OHEMS provide medical interventions and procedures 24/7 in out-of-hospital settings and during ambulance transport [39]. Ambulance teams are characterized as either “Team 1” (3 members: physician, nurse, and a driver) or the more recent “Team 2” (2 members: 2 nurses; one of them drives), which was introduced due to a physician shortage [38]. The choice of which team to dispatch is dependent on an assessment of which competencies are required. Physician area of responsibility includes a physical exam, diagnosis, treatment selection, certain procedures, and team coordination. Nurses assist with the physical exam and carry out diagnostic and treatment procedures. The driver is responsible for safe transport and can assist others when needed [39]. It is common for physicians at the start of their career to work in OHEMS [38]. After about 1 year of ambulance work, physicians usually work at a dispatch center a few shifts per month. Dispatch centers follow the Croatian adaptation of the Norwegian Index for Medical Emergency Assistance [39].
Study participants
We chose participants using purposive sampling to ensure the requisite experience (1-year was deemed sufficient for insight into work-as-done) as well as interest and ability to participate in the study [40]. We contacted physicians via email and strove to ensure that participants reflected the overall physician population in the organization in terms of gender, age, and work experience.
Data collection
We initially tested a semi-structured interview guide with three interviews. After analyzing the interview transcripts, which lacked a smooth flow, we opted to use an open interview approach with a single query statement: “I would like you to tell me about your compliance to guidelines in your decision-making around patients’ treatment.” The query statement was designed as a prompt to stimulate a discussion about physician decision-making. It was based on the assumption, grounded in the emergency medical practice experience of the research team, that guidelines are often the point of departure for decision-making, and that if this was not the case, it would regardless spur a discussion. In this context, the term “treatment” was used to refer to the entire patient pathway from receiving a call to the conclusion of the intervention. To ensure that we collected data that answered our research question and collected specific and concrete examples, we posed two follow-up questions when needed: “What were the consequences for your patient?” and “What additional support, if any, would you have liked to receive?”.
We piloted this revised approach twice. Since the flow of the interview transcripts improved, and no additional changes were made, these pilot interviews were included in the analysis. Individual interviews were conducted by EK (female with training in qualitative research) in Croatian, during February-March 2022 in a private area of participants’ choosing, often their workplace. Interviews lasted approximately one hour and were digitally recorded. Data collection continued until theoretical saturation, i.e. when further data collection was deemed superfluous as no fundamentally new information surfaced regarding common views held by participants [41]. EK transcribed the interviews verbatim.
Data analysis
We utilized an inductive content analysis, where categories were derived from the raw data, as it is a content-sensitive method applicable where there is little or no a priori understanding or knowledge about the phenomenon of interest due to the lack of published research [42]. EK (as the native Croatian speaker) read through the transcripts repeatedly to develop familiarity with the data and identified meaning units that captured key thoughts using NVivo qualitative data analysis software; QRS International Pty Ltd. Version 12, 2018. These were condensed into codes in English by EK and then grouped into general themes and categories using the Miro visual collaboration platform (www.miro.com). To improve trustworthiness, each category and its constituent codes were reviewed by three authors. Discrepancies were discussed until consensus was achieved. The findings section was shared with all participants. Seven chose to respond and validated the findings, i.e. they felt their experience was captured in a fair and correct manner.
Ethical considerations
Participants provided their informed consent prior to commencement of the interviews after receiving written and oral information about the study. We explained we would strive to pseudonymize the results, especially considering the delicate and confidential nature of the topic. The study was vetted and approved by the Ethical Board of the Institute of Emergency medicine of the City of Zagreb (nr. 892).
Results
Of the twenty-one physicians interviewed, the majority were young, female, with less than three years of experience, and no specialist training (Table 1). Four physicians who had agreed to interviews later declined because of scheduling issues.
We identified four themes related to the types of decisions made, influential factors, perceived implications on quality of work and patient care, as well as the desired support for decision-making (Table 2).
Theme 1. Types of decisions made
Participants described a highly variable work process that involved patient assessment (including measuring vital signs, preforming a physical examination, taking a medical history, evaluating patients’ symptoms, and developing an overall impression of patients’ environment) and decision-making, which revolved around three main questions:
-
Whether or not to transport patients to the hospital?
-
Whether or not to treat?
-
If yes to either, then how?
Participants explained that these decisions required weighing the perceived risks of each option for each patient.
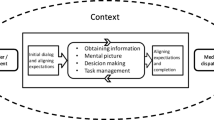
Theme 2. Factors that influenced decision-making
Participants described how each question often became complex and unclear due to physician-, patient-, organization-, and healthcare system-related factors, which influenced their decision-making process and guideline compliance.
Physician-related factors
Participants reflected on the learning journey physicians make from “novice” to “expert”: a seasoned physician accrues knowledge through first-hand experiences and by observing colleagues, whereas a novice lacks practical and applied knowledge. Guidelines were therefore especially valued by novices. However, guidelines presumed ideal working conditions and were therefore often not applicable. Many reported how they instead learned through “trial and error” and developed their own personal “guidelines”.
Participants described work as stressful, working conditions as poor, and expressed feeling undervalued and underpaid. They explained how feeling tired and overwhelmed had a negative impact on their relationship with and attitude towards patients, made them prone to conflicts or acquiescent to patients’ demands, and could lead to burnout. Some participants reflected upon co-workers’ suicides, which they thought might have been connected to high levels of stress and exhaustion and a lack of psychological support.
Patient-related factors
The severity of the patient’s condition was the paramount factor. “Real” emergencies were often easily identifiable due to training and guidelines, and it was easier to make decisions. Factors that increased complexity were patients’ socioeconomic situation, which influenced care quality at home. Participants also described that patients could lie or misrepresent their symptoms when calling emergency services. This could lead physicians to lose trust and empathy for their patients and consequently risk an underestimation of the severity of health issues. Physicians saw an increasing trend of verbal and physical aggression, complaints, and lawsuits, which they increasingly answered by practicing “defensive medicine”, e.g. “giving in” to patient demands to avoid conflict; even administering unnecessary therapies merely to satisfy patients.
Organizational factors
Organizational factors included training and feedback, diagnostic tools, guidelines, team dynamics, and physicians’ relationship with management.
Training and feedback
Participants’ views of their organization’s training courses differed widely. Some saw them as useful, while others felt they were too brief and irrelevant to real-world experiences, especially in terms of equipment and non-urgent situations. The consensus was that management was not investing enough in staff education.
Structured performance feedback was highly valued, but seldom received. Participants described how they sought information on patient outcomes from hospital staff, complaint logs, and occasionally managers. This was described as time-consuming, impractical, and more importantly – illegal – but nevertheless deemed necessary to improve decision-making.
Diagnostic and treatment tools
Participants expressed their frustration about daily problems related to the limited availability or malfunction of important diagnostic and treatment tools (e.g. defibrillator/ECG, glucometer, thermometer, paediatric pulse oximeter, infusion heaters, equipment for intubation, or lack of adult intraosseous device, Foley catheters, nasogastric tube, medication for rapid sequence intubation, insulin, etc.). In the absence of objectively measured patient parameters, decision-making depended on subjective assessments and improvisation. Aware of how this increased the risk for medical error, most participants preferred transporting patients to the hospital for a more thorough examination, especially pregnant women, children, and patients with chest pain.
Guidelines
Guidelines were seen as a useful tool for decision-making and to standardize care to improve patient outcomes and mitigate the risk for medical errors. However, despite access to multiple sources of guidelines, participants acknowledged compliance issues, including lack of organizational policies on which ones to use, where to find them, or how to apply them. Instead, there were “unwritten rules”, i.e. internal and unofficial instructions and expectations on how to act in certain situations. This knowledge was imparted by senior colleagues. The lack of clarity was faulted for mistakes.
Most participants believed it impossible to create situation-specific guidelines, as each patient has a unique set of symptoms and socioeconomic factors to be considered. Furthermore, when feeling like the patient’s or their own safety was compromised, they did not follow guidelines to the letter. This mostly included traffic accidents and interventions involving psychiatric or violent patients.
Some participants felt obliged to adhere to guidelines as it gave them a sense of legal protection should anything go wrong. Others felt the guidelines would not protect them in court, as they perceived them more as recommendations rather than legally binding. Lastly, all participants emphasized how insufficient and malfunctioning diagnostic and treatment tools prevented them from following the guidelines and providing the best patient care.
Most participants had attended the mandatory training for the OHEMS dispatch center. All admitted to not using the official dispatching guidelines (Croatian adaptation of the Norwegian Index), instead relying on personal judgment. This appeared to be encouraged by management, who had “unwritten rules” for triaging patients more suited to local needs.
Team dynamics
Close and friendly relationships and a positive atmosphere within the team were seen as important for guideline compliance and crucial for care quality. However, variation in experience levels combined with a lack of clear role descriptions led to confusion and poor coordination. Since most physicians were younger women and the drivers and nurses often older men, patients sometimes assumed the latter were physicians, which made establishing authority difficult. Some drivers and nurses interfered in decision-making and pressured younger doctors by telling them that “good doctors leave patients at home; bad doctors drive everyone to the hospital.” Worried about their image, some participants felt they had to balance patients’ interests with avoiding team tensions.
Relationship with management
Participants experienced a lack of support from management who they universally expressed “did not have my back”. Official reports on faulty equipment or vehicles seldom garnered a response. Management sometimes criticized physicians for following guidelines. Psychological and legal support, especially in the context of patient complaints, lawsuits, and acts of violence, was missing.
Healthcare system-related factors
Complexity of patient care conditions, ethical dilemmas, value judgments, and lack of patient trajectory planning on a healthcare system level resulted in “grey-zones” that had increased in frequency in recent years. These included palliative/terminally ill patients, or elderly patients often with multiple comorbidities, and often in nursing homes. There were also patients without life-threatening conditions, but which could become so if not recognized or treated in time. Without clear guidelines, it was challenging to decide on transport and treatment.
Grey-zone situations could start out seemingly simple, but become complex due to a lack of coordination across organizational boundaries, such as with law enforcement, social services, or other healthcare providers (e.g. primary care or hospital departments).
Emergency department overcrowding could induce physicians to avoid transporting patients due to the potentially greater risk incurred by long waiting times, e.g. for elderly patients during the Covid-19 pandemic. Already inadequate resources were further strained by numerous non-acute calls from citizens, who often could not differentiate between urgent and non-urgent conditions.
Additionally, there was a certain animosity between out-of-hospital and hospital-based physicians caused by overwhelming work conditions and differences in working principles and treatment preferences. This could lead to disputes during patient handovers, so participants sometimes preferred abdicating treatment choices to hospital-based physicians.
Theme 3. Perceived quality of work and patient care
Participants emphasized the importance their decision-making, and the factors that influenced it, had on the quality of their work and patient outcomes. They described a high variation in decision-making due to a lack of standardization in their work environment: malfunctioning equipment, absence of diagnostic and treatment tools, lack of clear guidelines and work protocols, and inadequate feedback and quality control mechanisms. High staff turnover rates led to a constant influx of new inexperienced doctors that hurt guideline compliance and team dynamics. Participants felt that these factors increased the risk for medical errors, including the loss of valuable time, which could make it difficult to provide care within the “golden hour”.
Theme 4. Decision-making support
Participants made numerous suggestions and recommendations about how to facilitate decision-making processes.
Organization-related recommendations
Training and formalized structured feedback were highlighted as areas for improvement. Participants desired annual and standardized training courses with modules on communication and case studies, an official mentorship program, and telemedicine connections between new physicians and experienced colleagues. A centralized information technology (IT) system could provide information on patients’ medical history to facilitate assessment and decision-making. Officially authorized feedback on patient outcomes and quality control mechanisms for continuous monitoring of work processes and outcomes were strategies suggested to identify areas for individual and organizational improvement. Team-building activities were desired as team relationships and a positive atmosphere were seen as crucial. A clear description of duties and responsibilities would ensure everyone had the requisite competencies and improve team coordination.
Participants asked for improved guidelines, ideally developed by managers, tailored to the work context (equipment, medications available, and specific challenges and changes within the local healthcare system), and encompassing the wider span of clinical and administrative tasks encountered in everyday work. Participants also wished for standardized and updated equipment as well as a response from managers on issues brought up in staff field reports, such as faulty equipment.
Participants emphasized the need for psychological support, such as professional psychological services, routines for after-action debriefing, or shortened shifts after especially taxing interventions (e.g. resuscitations). Due to the perceived high risk of lawsuits, participants saw a need for legal counselling and sharing liability with managers.
Healthcare system-related recommendations
Participants felt improved health literacy and health education for the public could lead to a decrease in the number of non-urgent calls and improve communication with patients. A separate phone line for medical advice in non-acute situations was also suggested, as well as improved coordination with law enforcement, social services, and other healthcare actors.
Discussion
We sought to understand physician decision-making in out-of-hospital emergency services. We found that physicians made three basic decisions. The first two were binary (whether or not to transport or to treat). The third was related to how – how to transport and how to treat. Typically, binary (yes/no) questions related to if are seen as simpler and questions related to how are more complex [43]. However, all three decisions were made more complex and perhaps unduly influenced by factors at the micro-, meso-, and macrosystem levels that forced physicians to make impromptu decisions on the fly and generated a high degree of variability that increased the risk for medical errors. Several of the factors that contributed to this complexity are corroborated in the literature: time pressure, patient condition, work environment, experience and competence level, team collaboration, and organizational support [2, 17, 44]. All these factors have been found to influence decision-making processes in different contexts. The educational backgrounds of ambulance staff, where lack of team and organizational support, adequate training and feedback, and ambiguous patient conditions and environment further increased the difficulty of making prompt and qualified decisions.
At the clinical micro-system level, where the patient and provider team meet, the findings suggest physician experience and competency level are fundamental. Most participants were women and at the start of their medical careers. This group may be more susceptible to internalizing failure with a subsequently higher rate of imposter phenomenon, depression, and suicide compared to other populations of academics [45, 46]. As gender roles in this setting were opposite the traditional stereotypes of men as doctors and women as nurses, female physicians often experienced an implicit bias from both patients and team members. Novice female physicians struggled to establish authority when coupled with older and more experienced male nurses and drivers, which sometimes complicated work. For the novice yet to develop “expert” tacit knowledge [47], a learning orientation supported by guidelines, checklists, SOPs, training, feedback, and mentors is essential to progress in expertise and develop the requisite competencies and capabilities [48, 49]. The organizational context can support this transition, for example high reliability organizations standardize routines and capture these in protocols and checklists [50].
Participants described meso-level constraints related to the availability of medication, equipment, vehicles, medical and legal competency levels, personal values and ethics, patient interaction, and work engagement levels which influenced guideline compliance, and created situations that required non-linear thought processes based on experience and instinct. To support guideline use, they need to be aligned with the natural decision-making process that allows for adaptation to changes in patient condition and surroundings [1, 20], or strategies explicated for how to address the needs of “grey zone” patients [10], which do not fit existing protocols. Indeed, while participants expressed a need for a more explicitly delineated structure, their adeptness to create and follow unwritten rules opens space for exploring an important concept in patient safety of facilitating flexibility of decision-making and embracing work complexity [51]. This provides additional support for not only teaching competencies, but also educating for capabilities [49].
Effective training for novices focuses on the development of practical, technical, and communication skills with observed benefits associated with performance in the field and confidence levels [17, 32]. Feedback is an effective quality improvement strategy that can improve clinical performance and patient outcomes [52]. Constructive, mutually respecting feedback from hospital staff can improve protocol compliance and decision-making on patient treatment in EMS [53]. Quantitative data analysis, e.g. statistical process control, integrated into governance systems can close feedback loops and lead to adjustments in practices that improve patient outcomes [54]. Feedback using IT-systems, such as real-time telemedicine support are useful – telemedicine consultations with emergency physicians by ambulance staff can improve efficiency and safety in assessment and transport of high-risk patients [55], stabilize life-threatening conditions [56], and decrease unnecessary transports of non-urgent cases [19]. And case studies, as raised by participants, support learning from concrete experiences [48, 57].
Sound meso-system leadership and management practices that support the development of and reinforce key learning practices are of vital importance in the volatile, uncertain, complex, and ambiguous context that characterizes OHEMS. Participants described how the work environment, with its lack of support for learning (guidelines, SOPs, training) and well-being (psychological and legal support, communication) created a feeling that the organization “did not have their back” and they were on their own. This negatively affected their feelings of psychological safety as they were afraid of reprisals and losing their license, which they felt stymied quality and safety improvement efforts, a pattern that has also been described in recent medical literature [2, 17]. The burden of responsibility participants carried and internalized was increased by the threat of legal repercussions, the lack of support structures, and continual exposure to questioning from patients, nurses, managers, and themselves. Participants’ descriptions of increased threats, violent behavior, and litigation create fear, lower job satisfaction and decrease motivation, which can negatively impact the provision of care [58, 59] and create space for medical errors, making them susceptible to developing a second victim phenomenon [60]. The coping strategy participants described – to practice defensive medicine and acquiesce to demands even though they violated guidelines or were without medical merit has, in hospital settings, led to decision-making that has not been in patients’ best interests [61, 62].
Medical settings that foster psychological safety and a positive learning environment, are better equipped to learn from mistakes and improve patient safety and employee well-being [63]. Team training, such as Crew Resource Management, can also contribute to a learning culture by improving team dynamics, communication, and a safe atmosphere [7, 64]. These techniques can also be paired with simulators to promote training under realistic conditions and help learners to deal with the aftermath and consequences of failed interventions [13]. More research is needed on strategies for how managers can lead to better support staff in OHEMS.
In the macrosystem, participants described issues related to coordination over organizational boundaries (e.g. contractual demands from law enforcement and process bottlenecks caused by emergency department overcrowding) and demographic changes in patient population. Campaigns to improve health literacy could reduce “overuse” of emergency services [65]. Reducing emergency overcrowding could reduce treatment delays, mortality, medical errors, and improve patient satisfaction [66]. Demographic changes have led to a shift towards older patients and more chronic conditions with an increase in low-acuity and non-urgent cases [2, 17, 26]. These are often more clinically complex to manage. Treatment outcomes could benefit from care-process redesign across organizational boundaries [67, 68] or innovative approaches to primary care [69].
Limitations/Methodological considerations
We found negative undertones in the data and analysis. The first author was previously employed at the study setting and had worked with several of the study participants, which we think contributed to a high level of trust, openness, and honesty during the interviews, vital when exploring a sensitive topic such as this one [70]. We did realize that our opening interview question could be an expression of our own bias of the importance of guidelines in emergency care. We made efforts to develop reflexivity by identifying and discussing any a priori bias, such as opinions on OHEMS and the employer in question, own experiences and difficult situations, views of the different professions, as well as more general prejudices or learned behaviors and perspectives that could bias data collection, analysis, and the reporting of the results [71]. We therefore feel confident in interpreting the results as another example of the importance of considering staff well-being and engagement as one of the four aims of health care [72].
We tried to improve transferability by providing a more detailed contextual description as a point of departure for the subsequent analysis and findings. Trustworthiness of the findings was increased due to the a priori understanding of the context, which was helpful in the analysis, and the rigor of the analysis process itself, which involved three additional researchers with backgrounds in public health, medicine, nursing, and research in medical management. Authenticity was enhanced through a participant group that reflected the gender, age, professional development, and work experience of physicians working in the setting.
Conclusion
Physician decision-making in out-of-hospital emergency medical services involves three deceptively simple decisions on transport, treatment, and how to carry out each. Physicians experienced these decisions as (unnecessarily) complex due to contextual factors at the micro, macro, and particularly meso system levels. We found that the burden of responsibility for answering these questions, and for the answers themselves, was borne by individual physicians, often at an early phase of their medical career. In itself, this could create quality and safety issues related to patient experience, patient outcomes, and staff well-being. However, factors outside traditional medical training curricula had a potentially undue influence on decision-making. Responsibility for the meso level is the province of managers. They have the means to create and support a safer learning environment by developing clear guidelines and standardized operating procedures aligned with real-world decision-making processes, strategies for when guidelines do not fit such as real-time tele-medicine support from older colleagues, reflective feedback, and psychological safety. These are ingredients not only important for organizational learning and safety, but also necessary to support physicians’ journey from novice to expert. There is a clear need for further research on how management and leadership strategies can better support staff as they make decisions-on-the-fly in out-of-hospital emergency medical services. With more effective support from employers and awareness of the contextual factors that influence decision-making beyond the patient themselves, staff will be able to feel better, learn better, and do better.
Data availability
The datasets generated during the analyses of the current study are available from the corresponding author on reasonable request.
Abbreviations
- COREQ:
-
Consolidated Criteria for Reporting Qualitative Studies
- ECG:
-
Electrocardiogram
- EMS:
-
Emergency Medical Services
- GP:
-
General Practitioner
- IT:
-
Information Technology
- OHEMS:
-
Out-of-hospital Emergency Medical Services
- PEMS:
-
Pre-hospital Emergency Medical Services
- SOP:
-
Standard Operating Procedure
References
Reay G, Rankin JA, Smith-Macdonald L, Lazarenko GC. Creative adapting in a fluid environment: an explanatory model of paramedic decision making in the pre-hospital setting. BMC Emerg Med. 2018;18.
Simpson P, Thomas R, Bendall J, Lord B, Lord S, Close J. ‘Popping nana back into bed’ - a qualitative exploration of paramedic decision making when caring for older people who have fallen. BMC Health Serv Res. 2017;17.
Tintinalli JE, Cameron P, Holliman J. EMS: a practical global guidebook. PMPH-USA; 2010.
Bennett N, Lemoine GJ. What a difference a word makes: understanding threats to performance in a VUCA world. Bus Horiz. 2014;57:311–7.
Atack L, Maher J. Emergency medical and health providers’ perceptions of key issues in prehospital patient safety. Prehosp Emerg Care. 2010;14:95–102.
Haynes AB, Weiser TG, Berry WR, Lipsitz SR, Breizat AH, Dellinger EP, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med. 2009;360:491–9.
Savage C, Gaffney FA, Hussain-Alkhateeb L, Olsson Ackheim P, Henricson G, Antoniadou I, et al. Safer paediatric surgical teams: a 5-year evaluation of crew resource management implementation and outcomes. Int J Qual Health Care. 2017;29:853–60.
Ebben RH, Vloet LC, Verhofstad MH, Meijer S, Groot JAM, van Achterberg T. Adherence to guidelines and protocols in the prehospital and emergency care setting: a systematic review. Scand J Trauma Resusc Emerg Med. 2013;21:9.
Brown KM, Macias CG, Dayan PS, Shah MI, Weik TS, Wright JL, et al. The development of evidence-based prehospital guidelines using a GRADE-based methodology. Prehospital Emerg Care Off J Natl Assoc EMS Physicians Natl Assoc State EMS Dir. 2014;18(Suppl 1):3–14.
Maria SJ. Paramedics’ Clinical Reasoning and Decision-Making in Using Clinical Protocols and Guidelines. 2021.
Ebben RHA, Siqeca F, Madsen UR, Vloet LCM, van Achterberg T. Effectiveness of implementation strategies for the improvement of guideline and protocol adherence in emergency care: a systematic review. BMJ Open. 2018;8:e017572.
Liang L, Bernhardsson S, Vernooij RWM, Armstrong MJ, Bussières A, Brouwers MC, et al. Use of theory to plan or evaluate guideline implementation among physicians: a scoping review. Implement Sci IS. 2017;12:26.
Anderson NE, Gott M, Slark J. Grey areas: New Zealand ambulance personnel’s experiences of challenging resuscitation decision-making. Int Emerg Nurs. 2018;39:62–7.
Anderson NE, Slark J, Gott M. Prehospital resuscitation decision making: a model of ambulance personnel experiences, preparation and support. Emerg Med Australas Ema. 2021;33:697–702.
Leemeyer AMR, Van Lieshout EMM, Bouwens M, Breeman W, Verhofstad MHJ, Van Vledder MG. Decision making in prehospital traumatic cardiac arrest; a qualitative study. Injury. 2020;51:1196–202.
Ebben RHA, Vloet LCM, Speijers RF, Tönjes NW, Loef J, Pelgrim T, et al. A patient-safety and professional perspective on non-conveyance in ambulance care: a systematic review. Scand J Trauma Resusc Emerg Med. 2017;25:71.
O’Hara R, Johnson M, Siriwardena AN, Weyman A, Turner J, Shaw D, et al. A qualitative study of systemic influences on paramedic decision making: Care transitions and patient safety. J Health Serv Res Policy. 2015;20:45–53.
Paulin J, Kurola J, Koivisto M, Iirola T. EMS non-conveyance: a safe practice to decrease ED crowding or a threat to patient safety? BMC Emerg Med. 2021;21:115.
Oosterwold J, Sagel D, Berben S, Roodbol P, Broekhuis H. Factors influencing the decision to convey or not to convey elderly people to the emergency department after emergency ambulance attendance: a systematic mixed studies review. BMJ Open. 2018;8.
Jones CMC, Cushman JT, Lerner EB, Fisher SG, Seplaki CL, Veazie PJ, et al. Prehospital Trauma Triage Decision-making: a model of what happens between the 9-1-1 call and the hospital. Prehosp Emerg Care. 2016;20:6–14.
Lokerman RD, Waalwijk JF, van der Sluijs R, Houwert RM, Leenen LPH, van Heijl M, et al. Evaluating pre-hospital triage and decision-making in patients who died within 30 days post-trauma: a multi-site, multi-center, cohort study. Injury. 2022;53:1699–706.
Erbay H. Some ethical issues in Prehospital Emergency Medicine. Turk J Emerg Med. 2014;14:193–8.
Waldrop DP, McGinley JM, Dailey MW, Clemency B. Decision-making in the moments before death: Challenges in Prehospital Care. Prehospital Emerg Care Off J Natl Assoc EMS Physicians Natl Assoc State EMS Dir. 2019;23:356–63.
Gugiu MR, McKenna KD, Platt TE, Panchal AR. A proposed theoretical Framework for Clinical Judgment in EMS. Prehosp Emerg Care. 2022. https://doi.org/10.1080/10903127.2022.2048756.
Perona M, Rahman MA, O’Meara P. Paramedic judgement, decision-making and cognitive processing: a review of the literature. Australas J Paramed. 2019;16.
Vuilleumier S, Fiorentino A, Dénéréaz S, Spichiger T. Identification of new demands regarding prehospital care based on 35,188 missions in 2018. BMC Emerg Med. 2021;21:63.
Neeki MM, Dong F, Avera L, Than T, Borger R, Powell J, et al. Alternative destination transport? The role of paramedics in optimal use of the Emergency Department. West J Emerg Med. 2016;17:690–7.
Willmore R. Cardiac arrest secondary to Accidental Hypothermia: who should we resuscitate? Air Med J. 2020;39:205–11.
Zajic P, Zoidl P, Deininger M, Heschl S, Fellinger T, Posch M, et al. Factors associated with physician decision making on withholding cardiopulmonary resuscitation in prehospital medicine. Sci Rep. 2021;11:5120.
Kamphausen A, Roese H, Oechsle K, Issleib M, Zöllner C, Bokemeyer C, et al. Challenges faced by Prehospital Emergency Physicians providing Emergency Care to patients with Advanced Incurable Diseases. Emerg Med Int. 2019;2019:3456471.
Wiese CHR, Bartels UE, Ruppert DB, Graf BM, Hanekop GG. Prehospital emergency physicians’ experiences with advance directives in Germany: a questionnaire-based multicenter study. Minerva Anestesiol. 2011;77:172–9.
Schuster M, Pints M, Fiege M. Duration of mission time in prehospital emergency medicine: effects of emergency severity and physicians level of education. Emerg Med J. 2010;27:398–403.
Sedlár M, Kaššaiová Z. Markers of cognitive skills important for team leaders in emergency medical services: a qualitative interview study. BMC Emerg Med. 2022;22:80.
Myers JA, Powell DMC, Psirides A, Hathaway K, Aldington S, Haney MF. Non-technical skills evaluation in the critical care air ambulance environment: introduction of an adapted rating instrument - an observational study. Scand J Trauma Resusc Emerg Med. 2016;24:24.
Clarke V, Braun V. Successful Qualitative Research: A Practical Guide for Beginners. 2013.
Aubin and King. The Healthcare Environment: a perfect ecosystem for growing shame. Healthc Q. 2018;20:31–6.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care J Int Soc Qual Health Care. 2007;19:349–57.
Dzakula A, Vočanec D, Banadinovic M, Vajagić M, Loncarek K, Lukačević Lovrenčić I, et al. Croatia: Health System Review Health Syst Transit. 2021;23:1–146.
Ministry of Health. Ordinance on conditions, organization, and manner of provision of emergency medicine (OG 71/16). Croatia: Croatian Ministry of Health; 2016.
Bolderston A. Conducting a research interview. J Med Imaging Radiat Sci. 2012;43:66–76.
Saunders B, Sim J, Kingstone T, Baker S, Waterfield J, Bartlam B, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant. 2018;52:1893–907.
Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24:105–12.
Vogt EE, Brown J, Isaacs D. The art of powerful questions: catalyzing, insight, innovation, and action. Mill Valley. Calif., Waltham, Mass.: Whole Systems Associates; Pegasus Communications [distributor]; 2003.
Gunnarsson B-M, Warrén Stomberg M. Factors influencing decision making among ambulance nurses in emergency care situations. Int Emerg Nurs. 2009;17:83–9.
Gregov L, Kovačević A, Slišković A. Stress among croatian physicians: comparison between physicians working in emergency medical service and health centers: pilot study. Croat Med J. 2011;52:8–15.
Stehman CR, Testo Z, Gershaw RS, Kellogg AR, Burnout. Drop out, suicide: physician loss in Emergency Medicine, Part I. West J Emerg Med. 2019;20:485–94.
Polanyi M. The Tacit Dimension. Chicago, IL: University of Chicago Press; 2009.
Dreyfus SE. The five-stage model of adult Skill Acquisition. Bull Sci Technol Soc. 2004;24:177–81.
Fraser SW, Greenhalgh T. Coping with complexity: educating for capability. BMJ. 2001;323:799–803.
Weick KE. In: Sutcliffe KM, editor. Managing the unexpected: assuring high performance in an age of complexity. 1st ed. Jossey-Bass; 2008.
Braithwaite J, Wears RL, Hollnagel E. Resilient health care: turning patient safety on its head. Int J Qual Health Care J Int Soc Qual Health Care. 2015;27:418–20.
Ivers N, Jamtvedt G, Flottorp S, Young JM, Odgaard-Jensen J, French SD et al. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2012;:CD000259.
Choi B, Tsai D, McGillivray CG, Amedee C, Sarafin J-A, Silver B. Hospital-directed feedback to Emergency Medical Services improves prehospital performance. Stroke. 2014;45:2137–40.
Rehn M, Krüger AJ. Quality improvement in pre-hospital critical care: increased value through research and publication. Scand J Trauma Resusc Emerg Med. 2014;22:34.
Stevanovic A, Beckers SK, Czaplik M, Bergrath S, Coburn M, Brokmann JC, et al. Telemedical support for prehospital Emergency Medical Service (TEMS trial): study protocol for a randomized controlled trial. Trials. 2017;18:43.
Schröder H, Beckers SK, Ogrodzki K, Borgs C, Ziemann S, Follmann A, et al. Tele-EMS physicians improve life-threatening conditions during prehospital emergency missions. Sci Rep. 2021;11:14366.
Kolb D. Experiential Learning: Experience As The Source Of Learning And Development. 1984.
Pourshaikhian M, Abolghasem Gorji H, Aryankhesal A, Khorasani-Zavareh D, Barati A. A systematic literature review: Workplace Violence against Emergency Medical Services Personnel. Arch Trauma Res. 2016;5:e28734.
Savoy S, Carron P-N, Romain-Glassey N, Beysard N. Self-reported violence experienced by swiss Prehospital Emergency Care Providers. Emerg Med Int. 2021;2021:e9966950.
Seys D, Wu AW, Van Gerven E, Vleugels A, Euwema M, Panella M, et al. Health care professionals as second victims after adverse events: a systematic review. Eval Health Prof. 2013;36:135–62.
Perea-Pérez B, Garrote Díaz JM, Hernández Gil Á, Martínez Hernández S. García Martín ÁF, Santiago-Sáez A. [Defensive medicine in hospital emergency services]. Rev Esp Salud Publica. 2021;95:e202106080.
Raposo VL. Defensive medicine and the imposition of a more demanding Standard of Care. J Leg Med. 2019;39:401–16.
Edmondson AC. The Fearless Organization: creating Psychological Safety in the Workplace for Learning, Innovation, and growth. Hoboken, NJ: John Wiley & Sons; 2018.
Kerner T, Schmidbauer W, Tietz M, Marung H, Genzwuerker HV. Use of checklists improves the quality and safety of prehospital emergency care. Eur J Emerg Med Off J Eur Soc Emerg Med. 2017;24:114–9.
Balakrishnan MP, Herndon JB, Zhang J, Payton T, Shuster J, Carden DL. The Association of Health literacy with preventable ED visits: a cross-sectional study. Acad Emerg Med Off J Soc Acad Emerg Med. 2017;24:1042–50.
Filippatos G, Evridiki K. The effect of emergency department crowding on patient outcomes. Health Sci J. 2015;9:1–6.
Carpenter CR, Platts-Mills TF. Evolving prehospital, emergency department, and “inpatient” management models for geriatric emergencies. Clin Geriatr Med. 2013;29:31–47.
Mazzocato P, Unbeck M, Elg M, Sköldenberg OG, Thor J. Unpacking the key components of a programme to improve the timeliness of hip-fracture care: a mixed-methods case study. Scand J Trauma Resusc Emerg Med. 2015;23:93.
Savage C, Bjessmo S, Borisenko O, Larsson H, Karlsson J, Mazzocato P. Translating “See-and-Treat” to primary care: opening the gates does not cause a flood. Int J Qual Health Care J Int Soc Qual Health Care. 2019;31:30–6.
Garton S, Copland F. I like this interview; I get cakes and cats!’: the effect of prior relationships on interview talk. Qual Res. 2010;10:533–51.
Mitchell J, Boettcher-Sheard N, Duque C, Lashewicz B. Who do we think we are? Disrupting notions of quality in qualitative research. Qual Health Res. 2018;28:673–80.
Bodenheimer T, Sinsky C. From triple to Quadruple Aim: care of the patient requires care of the provider. Ann Fam Med. 2014;12:573–6.
Acknowledgements
The authors would like to thank the participants for sharing their time and reflections, the Clinical Management research group at the Medical Management Centre, KI, for comments on previous drafts and Dr. Jan Jakobsson for feedback on the original master’s thesis.
Funding
No funding was obtained for this study.
Open access funding provided by Karolinska Institute.
Author information
Authors and Affiliations
Contributions
CS, VV, HL, KPH, and EK designed the study. VV, CS, and EK developed the interview guide. CS and VV trained EK in the interview techniques and VV coached EK through the reflexivity exercise. EK recruited participants and collected the data. EK, CS, MMC, and JLL conducted the analyses. EK drafted the master’s thesis upon which this article is based, under the supervision of CS, MMC, and JLL. EK, CS, MMC, and JLL drafted and with HL and VV revised the manuscript. All authors read, contributed to, and approved the final version prior to submission. CS was the PI.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study was vetted and approved by the Ethical Board of the Institute of Emergency medicine of the City of Zagreb (nr. 892). Participants provided their informed consent prior to commencement of the interviews after receiving written and oral information about the study. We explained we would strive to pseudonymize the results, especially considering the delicate and confidential nature of the topic. No experiments were conducted on humans or animals. All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Karmelić, E., Lindlöf, H., Luckhaus, J.L. et al. Decision-making on the fly: a qualitative study of physicians in out-of-hospital emergency medical services. BMC Emerg Med 23, 65 (2023). https://doi.org/10.1186/s12873-023-00830-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12873-023-00830-w