Abstract
Background
World Health Organization (WHO) consultation experts recommend countries to have guidance to identify public health action points suitable for their country. The objective of the study was to evaluate different obesity indices to predict high blood pressure and its optimal cutoff values among the adult population.
Method
A total of 3368 individuals age from 25 to 64 years were included in this study. Data was collected based on the WHO Stepwise approach. Body mass index (BMI), waist circumference (WstC), waist to hip ratio (WHpR) and waist to height ratio (WHtR) were measured and calculated. High blood pressure was considered for those with systolic blood pressure above 135 mmHg, diastolic blood pressure above 85 mmHg or taking antihypertensive medications. To generate cutoff values, the receiver operator characteristic curve was generated with the maximum Youden index.
Result
Women had a significantly higher hip circumference (P = 0.003), BMI (P = 0.036) and WHtR (P < 0.001) than men. Men had significantly higher WHpR (P = 0.027) than women. There were significantly higher BMI, WstC, WHpR, and WHtR among those with high blood pressure. The cutoff values for BMI, WstC, WHpR and WHtR were 22.86 kg/m2, 84.05 cm, 0.91 and 0.50 for men and 24.02 kg/m2, 79.50 cm, 0.91 and 0.51 for women, respectively.
Conclusion
BMI, WstC, WHpR, and WHtR are a useful predictor of high blood pressure among adults’ rural residents of southern Ethiopia. As the sensitivity for the cutoff values of most of indices were low, further surveys in different settings may need to be done before a conclusion can be drawn on whether or not to review the anthropometric cut offs for high blood pressure in Ethiopia.
Similar content being viewed by others
Background
Anthropometric parameters that assess body fat are broadly utilized to foretell the increased risk of chronic disease both at individual and population levels [1]. Body mass index (BMI) has been used by the World Health Organization (WHO) to define the risk of metabolic syndrome, especially the severity of overweight and obesity [2]. In addition to BMI, determinants of central adiposity like waist circumference (WstC) and waist-to-hip ratio (WHpR) were adopted as accurate predictors of these syndromes [3]. Recently literature started to include waist to height ratio (WHtR) as an additional anthropometric indicator for assessment of overweight and obesity-related syndromes including hypertension [4].
Hypertension is regarded as one of the major contributing factors for the global burden of diseases and a cardiovascular risk factor [5]. Physiologically, weight gain is the most common cause of hypertension [6]. Studies indicate that there is an association between anthropometric indicators and adverse cardiovascular and metabolic outcomes, including hypertension [6,7,8,9,10]. This relationship is also seen among studies conducted in Ethiopia [11, 12]. The most frequently used anthropometric indices are BMI and WstC [13].
WHO identified a cutoff value for these anthropometric indicators commonly based on the body fat level. The risks of certain diseases are notably higher in some populations than would be expected [2, 14]. Again, literature identified that the capacity of anthropometric indicators for predicting risk factors and diseases differ based on sex, ethnicity and other factors [2, 15,16,17,18,19,20,21]. WHO consultation experts also recommend countries to have guidance to identify public health action points suitable for their country [2]. An urgency was recognized to develop and share best practices, including affordable and effective community-based programs to screen and treat hypertension during a meeting held in African Union member states in Addis Ababa. During the meeting, it was stated that hypertension as one of the continent’s greatest health challenges after HIV/AIDS [22]. Anthropometric indicators may be an efficient strategy for the detection and control of high blood pressure mainly because these measures can be implemented without specialized technical apparatus and easy to set goals for interventions [23, 24]. Therefore, the objective of the study was to evaluate different obesity indices (BMI, WstC, WHpR, and WHtR) to predict high blood pressure and its related sex-specific cutoff values among the adult population of southern Ethiopia.
Methods
Participants
The study was carried at Arba Minch Health and Demographic Surveillance System (HDSS) which is located in Arba Minch Zuria district Southern Ethiopia. Arba Minch, the administrative town of the district, located 505 km south from the capital city, Addis Ababa. Arba Minch HDSS includes nine Kebeles (the lowest administrative unit of Ethiopia) of Arba Minch Zuria District. Eight of the nine HDSS Kebeles are rural and one is semi-urban.
A community-based cross-sectional survey was conducted from April to June 2017. The source population was adult residents (25–64 years old). Based on the 2016 Arba Minch HDSS site report, 24,800 (11,854 Male and 12,946 Female) eligible individuals, which was 33.5% of the total population, were included as source population. Pregnant mothers or women who have a history of recent delivery up to 8 weeks were excluded from the study [25].
The sample size was determined based on the WHO stepwise (STEPS) approach to surveillance of chronic non-communicable disease risk [25]. The estimated sample size for a sex-age group was 421 and the final sample size was 3368. The sampling frame was extracted from the Arba Minch HDSS database using sex, date of birth, individual and household identifications as extraction variables. A simple random sampling technique using Stata version 14 was implemented to select the study participants from the Arba Minch HDSS database.
Data collection procedure and instruments
Data collection instruments were adapted from STEPS instruments. From three levels of STEPS approach, only step one and two were applied in this study. Interview and measurement were conducted at the participants’ dwelling. Step one of the STEPS instruments is the questionnaire-based, which was designed to obtain core data on socio-demographic information with appropriate modifications in accordance with the STEPS manual [25]. Blood pressure measurements were taken using an Omron T9P digital automatic blood pressure monitor. Three blood pressure readings were taken on the left upper arm with the participant in a seated position following at least 15 min of rest. The participants rested for three minutes between each of the readings. The mean value of the three measurements was used as a final measurement of the blood pressure. Body weight (to the nearest 0.5 kg) was taken with the participant in bare feet with light clothing using SECA digital scale (model number 877). Height (to the nearest 1 cm) was measured using a stadiometer with participants wearing no shoes and without headwear. WstC measured at the midpoint between the palpable rib and the iliac crest. For measuring the hip circumference, the greatest posterior protuberance of the buttocks with a constant tension tape was used while the subject stands with arms at the sides, feet positioned close together, and weight evenly distributed across the feet.
Data quality control
Training was given for three days on data collection material and measurement procedures for 20 data collectors and four supervisors. The pre-test was conducted on 2% of the sample size and the finding was used to adjust the content and approach of the tools. Supervisors had monitored the whole data collection process and checked the data for completeness every day during the data collection time. To increase the response rate, the data collectors repeatedly visited (at least three times) those participants who were not present at the house during data collection time.
Definitions
BMI was generated by computing weight in kg per height in meter squared. WHpR and WHtR were computed by dividing the waist circumference by hip circumference and height, respectively. High blood pressure was considered for those with systolic blood pressure above 135 mmHg, diastolic blood pressure above 85 mmHg or if the participant reported that he/she is taking antihypertensive medications [26].
Data processing and analysis
EPI-data version 3.1 statistical software was used for data entry and the data was exported to Stata version 14 for further management and analysis. Descriptive statistical analyses like mean, standard deviation, frequencies & percentages were computed. Pearson’s partial correlation coefficients were calculated to reflect the relationships between four obesity indexes, and to characterize how these indexes correlated with high blood pressure. The receiver operator characteristic (ROC) curve was generated to identify optimal cutoff values with the maximum Youden index (sensitivity plus specificity-1) for anthropometric indexes to blood pressure measurements and to determine the ability of anthropometric variables to discriminate high blood pressure. The area under the curve (AUC) was calculated to compare the effectiveness of the different indexes and P-value < 0.05 was considered significant.
Results
A total of 3345 adults (50.0% were men) participated in the study with a response rate of 99.3%. The mean (SD) age of the participants was 44.59 (11.17) years and there was no significant difference in age between both sexes (P = 0.283). In addition, there was no significant difference between men and women concerning WstC (P = 0.406), systolic blood pressure (P = 0.837) and diastolic blood pressure (P = 8.99). However, women had a significantly higher hip circumference (P = 0.003), BMI (P = 0.036) and WHtR (P < 0.001) than men. Men had significantly higher WHpR (P = 0.027) than women (Table 1).
Significantly higher BMI, WstC, WHpR and WHtR were observed among those with high blood pressure, systolic blood pressure above 135 mmHg and diastolic blood pressure above 85 mmHg for men and total participants (for all P values were less than 0.05). For women, there were significantly higher BMI, WstC, WHpR and WHtR among those with high blood pressure and diastolic blood pressure above 85 mmHg. Only significantly higher WHpR and WHtR was observed in systolic blood pressure above 135 mmHg in women (Table 2).
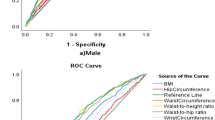
Among men, WstC had the highest AUC followed by WHtR, WHpR and BMI for high blood pressure. All of the anthropometric indicators were significant for AUC for high blood pressure among men. For women, WHtR had a higher AUC and followed by WstC, WHpR and BMI for high blood pressure. Like men, all anthropometric indicators showed significant for AUC for high blood pressure for women. In the case of AUC for systolic blood pressure above 135 mmHg, WstC for men and WHtR for women were the highest AUC. The AUC was significant for all anthropometric indicators for men, whereas only WHtR and WHpR for women. In the case of diastolic blood pressure above 85 mmHg, WstC for men and WHtR for women had the highest AUC. All anthropometric indicators for diastolic blood pressure above 85 mmHg had a significant AUC for both men and women (Table 3 and Figs. 1, 2, and 3).
For high blood pressure among male, the cutoff value for BMI was 22.86 kg/m2, with 35.7% sensitivity and 78.8% specificity at maximum Youden index. For females, the cutoff values was 24.02 kg/m2 with 26.4% sensitivity and 85.4% specificity. The sensitivity and specificity for high blood pressure for the traditional cutoff value, which is 25 kg/m2, were 14 and 94% for men, and 20 and 90% for women, respectively. Regarding waist circumference, the cutoff values, for men and women, was 84 cm and 79.5 cm, respectively. The sensitivity and specificity were 32.5 and 85.4% for men and 52.2 and 61.5% for women, respectively. WHO cutoff values for waist circumference were 94 cm for men and 80 cm for women [27]. At these cutoff values, the sensitivity and specificity for men were nearly 10 and 98% and for women 52 and 62%, respectively. Based on the highest Youden index, the cutoff value for WHpR were 0.91 for both sexes with 50.8% sensitivity and 62.5% specificity for men and 52.0% sensitivity and 61.5% specificity for women. According to the WHO cutoff value for sustainably increased risk of metabolic complications was 0.90 and 0.85 for men and women, respectively [27]. At these cutoff values, the sensitivity and specificity for men were 54 and 58% and for women were 78 and 25%, respectively. Regarding the cutoff values for WHtR for men and women was 0.50 and 0.51, respectively. The specificity and sensitivity were 41.9 and 74.0% for men and 56.4 and 58.7% for women, respectively (Table 3 & Figs. 1, 2, 3).
Discussion
This study showed that women had significantly higher mean BMI and WHtR compared to men. Men had significantly higher mean WHpR than women. Prior studies on the adult population in Ethiopia showed mean BMI ranges from 18.7 kg/m2 to 21.0 kg/m2, with higher among women [11, 28, 29], which is similar to the finding of this study. A cross-sectional community-based study among urban residents of Gondar, Northwest Ethiopia, showed that the mean WstC was 85.71 cm, with significantly higher among men participants [30]. A study in Gilgel Gibe Field Research Center, Southwest Ethiopia showed that the mean WstC was 75.2 cm and 73.8 cm for men and women, respectively, without significant difference [29]. Both studies conducted in the Gondor town and Gilgel Gibe Field Research Center are nearly similar mean WstC with this report. The report from Gilgel Gibe Field Research Center indicates that the mean WHpR was higher among men (0.90) compared to women (0.87) [29], which is similar to this finding regarding the difference between sex. Similarly, a study conducted at urban residents of Gondar was 0.89, with higher mean WHpR among men compared to women [30].
In this report, all the anthropometric indicators used (BMI, WstC, WHpR and WHtR) were apparently higher for high blood pressure. Similarly, a study conducted among 772 Chinese subjects showed that there was significantly higher mean value of BMI, WstC and WHtR for increased measurements of blood pressure. Contrary to the finding of this report, WHpR was not related [31]. A study among rural Wardha, India showed BMI and waist circumference had a strong correlation with increased blood pressure [8]. A study among 2097 adult Nigerian also showed that there was an association between BMI and blood pressure, which was with higher BMI there was an increased risk of hypertension [32]. A report from three different HDSS including from Ethiopia indicated that BMI was significantly correlated with both systolic blood pressure and diastolic blood pressure for the Ethiopian adult population [11]. As it is indicated in different literature, the association between obesity and hypertension is related to insulin resistance, sodium retention, increased sympathetic nervous system activity, activation of renin–angiotensin–aldosterone, and altered vascular function [33,34,35,36].
This study indicated that BMI, WstC, WHpR and WHtR useful indicators to identify the presence of high blood pressure in the adult population of the study setting. In addition, except BMI and WstC for systolic blood pressure above 135 mmHg for women, the other indicators showed that they had useful cutoff values for increased blood pressure measurements. Different studies showed the importance of these anthropometric indicators as a predictor of high blood pressure [31, 37, 38].
The cutoff value recommended by the WHO for BMI is 25 kg/m2. The present study revealed that 22.86 kg/m2 and 24.02 kg/m2 were the cutoff values for indicating the presence of high blood pressure for men and women, respectively. Other Studies in Ethiopia and Asian countries showed similarly lower cutoff value than indicated by WHO based on the Caucasian population [27]. For men, the cutoff value for the Chinese Liaoning Province, Hong Kong, and Western Ethiopia were 23.0 kg/m2, 23.8 kg/m2 and 23.5 kg/m2, respectively, which are nearly similar to this finding. Similarly, for women, the cutoff values were 23.3 kg/m2, 24.1 kg/m2 and 26.2 kg/m2 for the Chines population of Liaoning Province, Hong Kong and Western Ethiopia, respectively [31, 37, 39]. A study from Taiwanese and Shandong of China showed that the cutoff value of BMI was 25.74 kg/m2 and 25 kg/m2 for men and 23.46 kg/m2 and 24.5 kg/m2 for women, respectively [38, 40]. Finding from employees of Jimma University, Western Ethiopia showed a slightly higher BMI cutoff value than indicated for women by WHO based on the Caucasian population [27]. The higher cutoff values compared to WHO cutoff values for overweight might be related to urban society, which is the affiliated population in the case of Ethiopia. Studies conducted for assessing BMI cutoff values for determining high blood pressure have higher sensitivity and specificity than this finding for both men and women [31, 38,39,40].
The cutoff value for WstC to indicate high blood pressure of this study was lower than the cutoff value of WHO. The cutoff value by WHO is 94 cm for men and 80 cm for women [27]. A study on Taiwanese, Hong Kong, Shandong China and Western Ethiopia adults showed the cutoff value for WstC to predict high blood pressure was 87.9 cm, 82 cm, 88.5 cm and 89.2 cm for men and 76.4 cm, 78.4 cm, 83.5 cm and 93 cm for women [37,38,39,40]. The cutoff value for women WstC was similar to the WHO cutoff recommendation. For men, the cutoff value is lower than the recommended. Relatively the specificity for both men and women, and sensitivity for women is good, the sensitivity for the WstC cut-off value for men was by far lower even compared to other studies [31, 38,39,40].
The cutoff value to predict high blood pressure by using WHpR was 0.91 for both sexes from this finding. A cutoff value for WHpR as a predictor for high blood pressure in Southwest Ethiopia was 0.86 and 0.89 for men and women employees of the University [37]. Other studies, like Hong Kong, showed 0.89 for men and 0.84 for women as a predictor for high blood pressure [39]. Abdominal obesity is further defined as WHpR above 0.90 for males and above 0.85 for females [27]. The WHO recommendation is nearly similar for men but lower for women compared with this study. The sensitivity for the cutoff value of WHpR was lower than a study conducted in Liaoning Province and Hong Kong, China. The specificity was better for the study conducted Liaoning Province of China and nearly similar to the study conducted in Hong Kong, China [31, 39].
In this study, the WHtR cutoff value of identifying individuals with high blood pressure was nearly 0.50 for both sexes. A study among Hong Kong showed 0.50 for men and 0.55 for women as a cutoff value for WHtR as a predictor for high blood pressure among adult males [39]. A study among Taiwanese male adults showed that the cutoff value was 0.51 for men and 0.49 for women [40]. A study from Shandong of China showed that the cutoff value of WHtR was 0.53 for men and 0.52 for women [38]. A study among the employees of Jimma University, Western Ethiopia showed 0.47 for men and 0.51 for women as a cutoff value [37]. The specificity for the cutoff value for WHtR of this study was nearly similar to different studies. But the sensitivity was low for both men and women [38,39,40].
For this analysis, we consider measurements of blood pressure which is a part of metabolic syndrome. The data were collected mostly from rural residents within a district. As it is recommended to use different cutoff values for anthropometric indicators of metabolic syndrome, this finding gives a significant contribution.
Conclusions
In conclusion, BMI, WstC, WHpR and WHtR are useful predictors of high blood pressure among adults of rural residents of southern Ethiopia. This report found that the cutoff value of BMI for blood pressure measurements lower than that of the WHO’s recommendation for overweight based on the Caucasian population. But the sensitivity and specificity of BMI cutoff values for determining high blood pressure were low. Regarding WstC, the cutoff value is similar to the WHO cutoff value for women, but it is lower than the cutoff value of the men participants. In addition, the sensitivity for assessing high blood pressure using WstC was low for men. WHO recommended the cutoff value for WHpR was similar for men but lower for the women population of the study site. For most of the anthropometric indicators, the cutoff value as a predictor of high blood pressure was lower in this population compared with the international cutoff values. In addition, the sensitivity for determining the cutoff values for most of the indices was low. Further surveys in different settings may need to be done before a conclusion can be drawn on whether or not to review the anthropometric cutoffs for high blood pressure in Ethiopia.
Availability of data and materials
The datasets used and analyzed during the current study is available from Arba Minch Demographic Surveillance and Health Research Center, Arba Minch University and corresponding author on reasonable request. The survey tool/questionnaire are available as supplementary information files.
Abbreviations
- AUC:
-
Area under the curve
- BMI:
-
Body mass index;
- HDSS:
-
Health and demographic surveillance system
- ROC:
-
Receiver operator characteristic
- STEPS:
-
WHO stepwise
- WHO:
-
World Health Organization
- WHpR:
-
Waist to hip ratio
- WHtR:
-
Waist to height ratio
- WstC:
-
Waist circumference
References
Gibson RS. Principles of nutritional assessment. USA: Oxford university press; 2005.
expert consultation WHO. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63. https://doi.org/10.1016/S0140-6736(03)15268-3.
Zimmet P, Magliano D, Matsuzawa Y, Alberti G, Shaw J. The metabolic syndrome: a global public health problem and a new definition. J Atheroscler Thromb. 2005;12:295–300. https://doi.org/10.5551/jat.12.295.
Crystal Man Ying L, Rachel RH, Rachel PW, Mark W. Indices of abdominal obesity are better discriminators of cardiovascular risk factors than BMI: a meta-analysis. J Clin Epidemiol. 2008;61:646–53 http://linkinghub.elsevier.com/retrieve/pii/S0895435607003228?showall=true.
McMahan CA, Gidding SS, Fayad ZA, Zieske AW, Malcom GT, Tracy RE, et al. Risk scores predict atherosclerotic lesions in young people. Arch Intern Med. 2005;165:883–90.
Francischetti E, Genelhu V. Obesity-hypertension: an ongoing pandemic. Int J Clin Pract. 2007;61:269–80 http://search.ebscohost.com/login.aspx?direct=true&db=cin20&AN=105991474&site=ehost-live.
Klein S, Burke LE, Bray GA, Blair S, Allison DB, Pi-Sunyer X, et al. Clinical implications of obesity with specific focus on cardiovascular disease: a statement for professionals from the American Heart Association Council on nutrition, physical activity, and metabolism. Circulation. 2004;110:2952–67. https://doi.org/10.1161/01.CIR.0000145546.97738.1E.
Deshmukh PR, Gupta SS, Dongre AR, Bharambe MS, Maliye C, Kaur S, et al. Relationship of anthropometric indicators with blood pressure levels in rural Wardha. Indian J Med Res. 2006;123:657.
Al-Sharbatti SS, Shaikh RB, Mathew E, Sreedharan J, Muttappallymyalil J, Basha SA. The use of obesity indicators for the prediction of hypertension risk among youth in the United Arab Emirates. Iran J Public Health. 2011;40:33.
Deng W-W, Wang J, Liu M-M, Wang D, Zhao Y, Liu Y-Q, et al. Body mass index compared with abdominal obesity indicators in relation to prehypertension and hypertension in adults: the CHPSNE study. Am J Hypertens. 2012;26:58–67.
Tesfaye F, Nawi NG, Van Minh H, Byass P, Berhane Y, Bonita R, et al. Association between body mass index and blood pressure across three populations in Africa and Asia. J Hum Hypertens. 2007;21:28–37. https://doi.org/10.1038/sj.jhh.1002104.
Bonsa F, Gudina EK, Hajito KW. Prevalence of hypertension and associated factors in Bedele town, Southwest Ethiopia. Ethiop J Health Sci. 2014;24:21–6.
Goh LGH, Dhaliwal SS, Welborn TA, Lee AH, Della PR. Anthropometric measurements of general and central obesity and the prediction of cardiovascular disease risk in women: a cross-sectional study. BMJ Open. 2014;4:e004138.
World Health Organization, WHO. Physical status: the use of and interpretation of anthropometry, report of a WHO expert committee: World Health Organization; 1995.
Cheah WL, Chang CT, Hazmi H, Kho GWF. Using anthropometric Indicator to identify hypertension in adolescents: a study in Sarawak, Malaysia. Int J Hypertens. 2018;2018.
Okamkpa C, Nwankwo M, Danborno B. Predicting high blood pressure among adults in southeastern Nigeria using anthropometric variables. J Exp Clin Anat. 2016;15:111. https://doi.org/10.4103/1596-2393.200912.
Cassani RSL, Nobre F, Pazin-Filho A, Schmidt A. Relationship between blood pressure and anthropometry in a cohort of brazilian men: a cross-sectional study. Am J Hypertens. 2009;22:980–4.
Hunma S, Ramuth H, Miles-Chan JL, Schutz Y, Montani JP, Joonas N, et al. Body composition-derived BMI cut-offs for overweight and obesity in Indians and creoles of Mauritius: comparison with Caucasians. Int J Obes. 2016;40:1906–14.
Deurenberg P. Universal cut-off BMI points for obesity are not appropriate. Br J Nutr. 2001;85:135. https://doi.org/10.1079/BJN2000273.
Alberti KG, Zimmet P, Shaw J. The metabolic syndrome - a new worldwide definition. Lancet. 2005;366:1059–62.
Alberti K, Eckel R, Grundy S, Zimmet P, Cleeman J, Donato K, et al. Harmonizing the metabolic syndrome: a joint interim statement of the international diabetes federation task force on epidemiology and prevention; National Heart, Lung, and Blood Institute; American Heart Association; world heart federation; international. Circulation. 2009;120:1640–1645. doi:https://doi.org/10.1161/CIRCULATIONAHA.109.192644.
Dzudie A, Rayner B, Ojji D, Schutte AE, Twagirumukiza M, Damasceno A, et al. Roadmap to achieve 25% hypertension control in Africa by 2025. Glob Heart. 2018;13:45–59.
PAHO WHO. Protocol for the nutritional Management of Obesity, diabetes and hypertension in the Caribbean. Caribb Food Nutr Inst Jamaica. 2004.
Flores-Huerta S, Klünder-Klünder M, de la Cruz LR, Santos JI. Increase in body mass index and waist circumference is associated with high blood pressure in children and adolescents in Mexico City. Arch Med Res. 2009;40:208–15.
World Health Organization. The WHO STEPwise approach to noncommunicable disease risk factor surveillance. Geneva: World Health Organization; 2005.
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Böhm M, et al. 2013 ESH/ESC practice guidelines for the management of arterial hypertension: ESH-ESC the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Blood Press. 2014;23:3–16.
World Health Organization. Waist circumference and waist-hip ratio report of a WHO expert consultation: World Health; 2008. p. 8–11. https://doi.org/10.1038/ejcn.2009.139.
Girma T, Mossie A, Getu Y. Association between body composition and khat chewing in Ethiopian adults. BMC Res Notes. 2015;8:680.
Tessema F, Haileamlak AH, Muluneh AT, Alemseged F, Woldemichael K, Asefa M, et al. Physical measurement profile at Gilgel gibe field research center, Southwest Ethiopia. Ethiop J Health Sci. 2012;22:29–38.
Amare B, Moges B, Moges F, Fantahun B, Admassu M, Mulu A, et al. Nutritional status and dietary intake of urban residents in Gondar, Northwest Ethiopia. BMC Public Health. 2012;12:752.
Liu Y, Tong G, Tong W, Lu L, Qin X. Can body mass index, waist circumference, waist-hip ratio and waist-height ratio predict the presence of multiple metabolic risk factors in Chinese subjects? BMC Public Health. 2011;11(13 January 2011). https://doi.org/10.1186/1471-2458-11-35.
Adedoyin RA, Mbada CE, Bisiriyu LA, Adebayo RA, Balogun MO, Akintomide AO. Relationship of anthropometric indicators with blood pressure levels and the risk of hypertension in Nigerian adults. Int J Gen Med. 2009;1:33–40.
Landsberg L, Aronne LJ, Beilin LJ, Burke V, Igel LI, Lloyd-Jones D, et al. Obesity-related hypertension: pathogenesis, cardiovascular risk, and treatment: a position paper of the Obesity Society and the American Society of Hypertension. J Clin Hypertens. 2013;15:14–33.
Kotchen TA. Obesity-related hypertension: epidemiology, pathophysiology, and clinical management. Am J Hypertens. 2010;23:1170–8.
Hall JE, do Carmo JM, da Silva AA, Wang Z, Hall ME. Obesity-induced hypertension: interaction of neurohumoral and renal mechanisms. Circ Res. 2015;116:991–1006.
Vanecková I, Maletinska L, Behuliak M, Nagelová V, Zicha J, Kunes J. Obesity-related hypertension: possible pathophysiological mechanisms. J Endocrinol. 2014;223:R63–78.
Sinaga M, Worku M, Yemane T, Tegene E, Wakayo T, Girma T, et al. Optimal cut-off for obesity and markers of metabolic syndrome for Ethiopian adults. Nutr J. 2018;17:109. https://doi.org/10.1186/s12937-018-0416-0.
Dong X, Liu Y, Yang J, Sun Y, Chen L. Efficiency of anthropometric indicators of obesity for identifying cardiovascular risk factors in a Chinese population. Postgrad Med J. 2011;87:251–6.
Ko GTC, Chan JCN, Cockram CS, Woo J. Prediction of hypertension, diabetes, dyslipidaemia or albuminuria using simple anthropometric indexes in Hong Kong Chinese. Int J Obes. 1999;23:1136.
Li WC, Chen IC, Chang YC, Loke SS, Wang SH, Hsiao KY. Waist-to-height ratio, waist circumference, and body mass index as indices of cardiometabolic risk among 36,642 Taiwanese adults. Eur J Nutr. 2013;52:57–65.
Acknowledgements
We thank the respondents, field and data entry staffs of the Arba Minch HDSS for their contributions to the production of the data used in this study. Thank you to Arba Minch Demographic Surveillance and Health Research Center, Arba Minch University for supporting data collection, entry and analysis.
Funding
This study was funded by Arba Minch Demographic Surveillance and Health Research Center, Arba Minch University. The funder did not have a role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. Rather the funder covered the cost related to the data collection and analysis.
Author information
Authors and Affiliations
Contributions
This analysis was conceptualized by BT, with input from all co-authors. BT, AC, GA and AB facilitate data collection and entry. BT led the analysis design and BT, MB, MK, ND and AB prepared the draft manuscript. GA and AC provided comments towards the interpretation of results and drafted portions of the manuscript. BT organized and drafted the final manuscript with contributions from all co-authors. All authors read and approved the final manuscript
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical clearance was obtained from the Institutional Research Ethics Review Board of Arba Minch University. The informed consent obtained from study participants was verbal and approved by the ethical committee of the Institutional Research Ethics Review Board of Arba Minch University. The consent was obtained for the interview and physical measurements. Privacy of the study participants was maintained by interviewing the participants alone.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gutema, B.T., Chuka, A., Ayele, G. et al. Predictive capacity of obesity indices for high blood pressure among southern Ethiopian adult population: a WHO STEPS survey. BMC Cardiovasc Disord 20, 421 (2020). https://doi.org/10.1186/s12872-020-01686-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-020-01686-9