Abstract
Background
Obesity is one of the major determinants of blood pressure. This study aimed to determine the optimal sex- and age-specific cut-off points of anthropometric indices, including body mass index (BMI), waist circumference (WC), hip circumference (HC), wrist circumference (WrC), waist-hip ratio (WHR), and waist-height ratio (WHtR), to screen for hypertension (HTN) in a cohort of Iranian adults aged 35 to 70 years, and to compare the predictive performance of the indices based on receiver operating characteristic (ROC) curves.
Methods
This population-based study was carried out on the participants aged 35 to 70 years of the Bandare-Kong Non-Communicable Diseases (BKNCD) Cohort Study, a part of the Prospective Epidemiological Research Studies in IrAN (PERSIAN). Using the area under the receiver operating characteristic curve (AUC) and Youden's J index, optimal sex- and age-specific cut-off points of the anthropometric indices in association with HTN were calculated.
Results
This study included a total of 2256 females and 1722 males. HTN was diagnosed in 736 females (32.6%) and 544 males (31.6%). The optimal cut-off of WC for HTN was 90 cm in males and 95 cm in females, with an area under the ROC curve (AUROC) of 0.60 and 0.64, respectively. For HC, the optimal cut-off was 95 cm for males and 108 cm for females (AUROC = 0.54 for both). Moreover, WrC optimal cut-offs were 17 cm for males (AUROC = 0.56) and 15 cm for females (AUROC = 0.57). As for BMI, the optimal cut-off was 25 kg/m2 in males and 27 kg/m2 in females (AUROC of 0.59 and 0.60, respectively). Also, a cut-off of 0.92 was optimal for WHR in males (AUROC = 0.64) and 0.96 in females (AUROC = 0.67). On the other hand, WHtR optimal cut-offs were 0.52 for males and 0.60 for females (AUROC of 0.63 and 0.65, respectively).
Conclusions
WHR and WHtR, as anthropometric indices of obesity, were demonstrated to be significant predictors of HTN. Further, we suggest using WHR (cut-off point of 0.92 for males and 0.96 for females) and WHtR (cut-off point of 0.52 for males and 0.60 for females) as measures of preference to predict HTN among the southern Iranian population. Further multicenter longitudinal studies are recommended for a more accurate prediction of HTN.
Similar content being viewed by others
Background
Non-communicable diseases (NCDs) impose an enormous yet growing burden globally. The prevalence of NCDs has risen worldwide, affecting both males and females and all age groups [1]. Globally, NCDs account for 41 million annual deaths or approximately 71% of overall mortality; however, according to WHO, in 2019, this figure rose to 74% [2, 3]. NCDs claim the lives of over 15 million people from the ages of 30 to 69 every year; 85% of these deaths take place in countries with low and middle incomes. NCDs are responsible for 57% of deaths in the Eastern Mediterranean Region [4]. Hypertension (HTN) is one of NCDs' most critical risk factors [5]. It is highly prevalent globally, and by 2025, HTN is estimated to affect more than 1.56 billion people worldwide, up from 972 million in the year 2000 [6]. In 2019, HTN contributed to 10.8 million deaths worldwide [7]. Approximately two-thirds of patients with HTN live in developing countries [8, 9]. According to a recent meta-analysis conducted in Iran, a developing Eastern Mediterranean country, the prevalence of HTN was found to be 25% among females and 24% among males [10].
Obesity is one of the major determinants of blood pressure. There have been various explanations as to how body fat distribution affects blood pressure and HTN risk [11,12,13]. Anthropometric indices are essential for detecting obesity at an early stage. The anthropometric indices of obesity can be divided into two categories: measures of general obesity, including the body mass index (BMI), and measures of central obesity, such as waist circumference (WC), hip circumference (HC), and their ratios, waist-hip ratio (WHR) and waist-height ratio (WHtR). It is uncertain whether anthropometric indices of general or central obesity have a stronger correlation with blood pressure [14,15,16,17].
According to previous research [18], BMI used to be the primary determinant of HTN, as it was found to be more reliable than WC and WHtR. Some studies have found WC to be a more accurate screening tool than BMI, WHR, and WHtR [19,20,21,22,23]. Other studies have found WHR to be more reliable at predicting HTN than BMI, WC, and WHtR [24]. Furthermore, there have been several recent studies where WHtR has been found to have better predictive abilities than WHR, BMI, and WC among females and males [25,26,27,28,29,30,31].
Another noteworthy finding was that, in a recent systematic review conducted to assess the effectiveness of anthropometric indices in predicting cardiovascular diseases (CVDs), abdominal obesity indices, particularly WHR, led to a better prediction of CVD prevalence in adults [32]. Further, a study conducted among western Iranian adults proposed that BMI is a better predictor of metabolic syndrome than WC and WHR [33].
Given the existing controversy regarding the best anthropometric index for predicting HTN, this study aimed to determine the optimal sex- and age-specific cut-off points of anthropometric indices (BMI, WC, HC, WrC, WHR, and WHtR) to screen for HTN in a cohort of Iranian adults aged 35 to 70 years, and to compare the predictive performance of the indices based on receiver operating characteristic (ROC) curves.
Methods
Study design and sampling
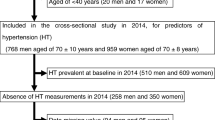
The dataset for this descriptive population-based cross-sectional study was obtained from the Bandare-Kong Non-Communicable Diseases (BKNCD) research (N = 4063), a large-scale prospective study conducted between November 2016 and November 2018, among people aged 35–70, as part of the Prospective Epidemiological Research Studies in Iran (PERSIAN). The precise study design and methodologies have already been discussed in depth [34]. Among the study subjects, pregnant women and incomplete data were excluded. In total, 3978 participants were analyzed in this study.
Data collection
The participants were interviewed by trained interviewers using a comprehensive standardized questionnaire for collecting demographics, medical and drug history.
Anthropometric measurements
A transportable weighing scale, with a precision of 0.01 kg was used to weigh the participants while minimally clothed and without shoes. The subjects' heights were measured using a height rod, with 0.5 cm precision, while standing barefoot and with shoulders relaxed and arms at sides. BMI was obtained by dividing the subjects' weight in kilograms by their height in meters square. WC was measured using a retractable tape in the horizontal plane halfway between the lowest rib and the top of the iliac crest, with an accuracy of 0.1 cm. HC was measured parallel to the floor, with the arms relaxed at the sides and the maximum circumference over the buttocks. Wrist circumference (WrC) was measured with subjects in a seated position from both wrists using a tape meter positioned over the Lister tubercle of the distal radius and over the distal ulna, and an average was taken. WHR and WHtR were obtained by dividing waist to hip and height, respectively.
Blood pressure measurement
A calibrated mercury sphygmomanometer was used to measure systolic and diastolic blood pressure (SBP, DBP). Prior to measurement, the participants rested for 5 min while seated. Blood pressure was measured twice at a 15-min interval from the right arm. The mean of the two consecutive blood pressure measurements was then utilized to compute the SBP and DBP that were used in the analysis. HTN was defined as SBP ≥ 140 mmHg and/or DBP ≥ 90 mmHg, self-reported HTN, as well as individuals those received HTN treatments [34].
Statistical analysis
It was assumed that the distribution was normal because of the large sample size. While continuous variables were described using means and standard deviations (SD), categorical variables were described using numbers and percentages (%). When comparing variables stratified by sex (male/female) or age (age < 50 / age ≥ 50), t-tests and chi-square tests were used to compare continuous variables and categorical variables, respectively.
Receiver operating characteristic (ROC) curves were used to determine the diagnostic accuracy of the anthropometric indices and their optimal cut-off values for each sex and age group (age < 50/age ≥ 50). The area under the ROC curve (AUC) was calculated to assess the diagnostic ability of the anthropometric indices to predict HTN. An anthropometric measure with AUC = 1 discriminated clearly between hypertensive and non-hypertensive individuals. However, an AUC of 0.5 indicated no difference in anthropometric values between the two groups, meaning the predictive power was invalid. Using Youden's J index, appropriate cut-off values were determined (maximum [sensitivity + specificity—1]).
Using the set cut-off values from the study, the anthropometric measures were dichotomized and assessed for their relationship with HTN using binary logistic regression following adjustment for age, physical activity, socio-economic status, smoking, and hookah consumption. Plus, all regression analyses were stratified according to sex. The ROC analysis was carried out using MedCalc software, and the other analyses were conducted by SPSS version 25. A P-value of 0.05 or lower was regarded as statistically significant.
Results
This study included 1722 (43.3%) males and 2256 (56.7%) females. Their age ranged from 35 to 70 years, with a mean (SD) of 48.3 (9.4) years. 544 males (31.6%) and 736 females (32.6%) were diagnosed with HTN. Table 1 displays the subjects' characteristics.
ROC analysis (Fig. 1) revealed that WHR and WHtR had better performance than other indices in females and males. According to Fig. 2, all anthropometric indices performed fairly similarly in predicting diagnosed HTN for age < 50 and age ≥ 50.
Table 2 displays the area under the ROC curve for males and females. WHR and WHtR showed better accuracy than other anthropometric indices in predicting HTN in females (AUC = 0.67 for WHR, AUC = 0.65 for WHtR) and males (AUC = 0.64 for WHR, AUC = 0.63 for WHtR).
Based on Table 3, anthropometric measures were more accurate in predicting HTN in people aged < 50 than those aged ≥ 50.
The optimal cut-off points for anthropometric indices were determined according to Youden's J statistic. The optimal cut-off points were developed for WC (90 cm for males and 96 cm for females), HC (95 cm for males and 108 cm for females), WrC (17 cm for males and 15 cm for females), BMI (25 kg/m2 for males and 27 kg/m2 for females), WHR (0.92 for males and 0.96 for females), and WHtR (0.52 for males and 0.60 for female) (Table 2).
The optimal cut-off values for screening hypertension were also determined based on age. The optimal cut-off points were developed for WC (92 cm for age < 50 and 90 cm for age ≥ 50), HC (99 cm for age < 50 and 95 cm for age ≥ 50), WrC (17 cm for age < 50 and 16 cm for age ≥ 50), BMI (25 kg/m2 for age < 50 and 26 kg/m2 for age ≥ 50), WHR (0.90 for age < 50 and 0.96 for age ≥ 50), and WHtR (0.60 for age < 50 and 0.60 for age ≥ 50) (Table 3).
After adjusting for the age, physical activity, socio-economic status, smoking, and hookah effects, the anthropometric indices were dichotomized using the defined cut-off points and then evaluated for their relationships with HTN (Table 4). The odds of HTN were significantly increased for all dichotomized measures. Among males, those who had increased WHR, WHtR, BMI, WC, HC, and WrC were 1.91, 2.24, 2.04, 2.16, 1.87, and 1.55 times respectively, more likely to be hypertensive than those with appropriate indices.
Whereas among females, those who had increased WHR, WHtR, BMI, WC, HC, and WrC were 2.10, 2.61, 2.14, 2.25, 1.66, and 1.84 times respectively, more likely to be hypertensive than those with appropriate indices.
Discussion
This population-based cross-sectional study aimed to determine optimal cut-off values of several anthropometric indices for the prediction of HTN among southern Iranian adults. Based on ROC analysis, our study demonstrated that WHR and WHtR, as abdominal obesity indices, provided better screening ability for hypertension compared to other measures among both sexes.
Consistently, Feldstein et al. demonstrated that WHR better predicts HTN compared to WC and BMI [35]. Also, Esmaillzadeh et al. concluded that WHR was a better screening measure for cardiovascular risk factors, especially HTN, than other anthropometric indices in adult men [20]. Evidence suggests that WHR is positively correlated with arterial stiffness [36], which plays a significant role in the pathogenesis of HTN and can predict the likelihood of cardiovascular events in hypertensive patients [37]. Moreover, excess abdominal fat deposition causes high-density lipoprotein (HDL) levels to decrease, and low-density lipoprotein (LDL) and triglyceride levels to increase, and a high LDL level is a well-established risk factor for HTN [38]. Additionally, the superiority of WHR may also be due to the fact that WHR incorporates a hip circumference measurement, which is inversely associated with HTN [39].
Furthermore, several studies have also shown that WHtR provides a more reliable prediction of HTN among different populations [29, 40, 41]. A potential explanation for the higher prediction power of WHtR could be that height may have an impact on how fat is distributed, making short individuals more likely to accumulate central fat and have greater SBP levels [42].
Inconsistent with our findings, some cross-sectional studies have indicated that other obesity indices better predict hypertension than WHR and WHtR. For instance, In some studies, BMI and WC have been suggested to better predict HTN [35, 43, 44]. BMI cannot distinguish between fat mass and muscle mass, leading to underestimating health risks; therefore, using only height and weight to screen for health risks is becoming obsolete [45]. On the other hand, although health risks are generally associated with central fat distribution [46], WC is collinear with BMI and weight, and has a limited ability to predict morbidity and mortality [47].
In the current study, the optimal cut-off values established for WHR to detect HTN were 0.92 in males and 0.96 in females, which are higher compared to the WHO-recommended sex-specific WHR cut-offs (0.90 in males and 0.85 in females) [48], and those estimated for an Ethiopian population [22]. Also, cut-off values of WHtR in our study were higher than in previous cross-sectional studies [41]. Additionally, cut-off points for WC to screen for HTN were determined to be 90.0 cm for males and 96.0 cm for females in the current study, while previously established cut-offs were 76–102 cm for males and 75–88 cm for females [24, 48, 49]. Furthermore, we found that BMI cut-offs were 25 kg/m2 for males and 27 kg/m2 for females. At the same time, cut-offs from other studies ranged from 22.2 to 24.6 for males and 24.3 to 27.7 for females [22, 50, 51]. The discrepancies between studies can be explained by ethnic and racial differences, as well as variations in body composition and fat distribution among different age and sex groups. Different research designs, measurement protocols, or criteria to define cardiometabolic outcomes may also make a difference.
Another noteworthy finding from this study is that anthropometric indices were generally more accurate in predicting HTN in individuals under 50 than those equal to or over 50, as well as females than males. One potential explanation can be the stronger correlation of these indices with HTN in females reflected in the generally higher odds of HTN than males in the logistic regression analysis, even after adjustment for age, physical activity, socio-economic status, smoking, and hookah consumption. Moreover, our previous research on the same population has shown that all metabolically unhealthy states were significantly higher in females than in males [52], and blood pressure is a component of metabolic health. The higher accuracy of indices in females, at least in part, can also account for the higher accuracy in those aged < 50 years since almost two-thirds of females were under 50.
Considering the results of the present study differed based on age and sex, the authors believe that there is a need to develop age and sex-specific cut-off values that are appropriate for different populations, as there is no consensus regarding these values in the literature when it comes to screening hypertension in adults. Furthermore, this study has significance for developing countries such as Iran because of the lifestyle changes caused by urbanization that may impact nutritional status and demographics. As a result of this condition, NCDs prevalence, like HTN and diabetes mellitus, has unexpectedly risen, which in turn leaves the country facing a heavy burden of non-communicable diseases [53]. Therefore, initiatives aiming at preventing NCDs like HTN can be developed using the findings from our study. The use of straightforward, non-invasive anthropometric indices in structured population-based or primary care facility-based HTN screening can easily achieve this.
There were several limitations to this study. Data for this study were taken from a cohort study conducted among southern Iranians aged between 35 and 70, which was a particular study group. It is uncertain if the same results hold true for other age groups or ethnicities. Additionally, due to the study's cross-sectional nature, we were unable to draw causal conclusions about the association between obesity indices and HTN. Another limitation may have been measurement error. Even though we attempted to reduce measurement errors, there is still a possibility of errors occurring. Despite these drawbacks, the results of this study are significant in terms of their implications for the prevention of HTN and the reduction in its occurrence among both males and females in the age group and population investigated. Thus, although the current study adds to the literature, future research that enables establishing a causal link between adiposity indices and HTN in other populations by multicenter longitudinal design is advised.
Conclusions
In a cohort of Iranian males and females aged 35–70, the measurement of WHR and WHtR, as anthropometric indices of obesity, were significantly indicative of the occurrence of HTN. The results of this study showed the significance of anthropometric obesity indices as predictors of HTN, despite the fact that the study was restricted to the middle-aged Iranian population and had some other limitations. Additionally, we propose using WHR (cut-off point of 0.92 for males and 0.96 for females) and WHtR (cut-off point of 0.52 for males and 0.60 for females) as the measures of preference to predict HTN in Iranians. Finally, we suggest that WHR and WHtR be regularly monitored in the healthcare system and utilized as indicators for evaluating the risk of HTN.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ADA:
-
American Diabetes Association
- AUROC:
-
Area Under the Receiver Operating Characteristic
- T2DM:
-
Type 2 diabetes mellitus
- FPG:
-
Fasting plasma glucose
- BMI:
-
Body mass index
- WC:
-
Waist circumference
- HP:
-
Hip Circumference
- WrC:
-
Wrist Circumference
- WHR:
-
Waist to Hip Ratio
- WHtR:
-
Waist to Height Ratio
- SBP:
-
Systolic Blood Pressure
- DBP:
-
Diastolic Blood Pressure
- BP:
-
Blood pressure
- HTN:
-
Hypertension
- CI:
-
Confidence interval
- WHO:
-
World Health Organization
- TG:
-
Triglyceride
- TC:
-
Total cholesterol
- HDL-C:
-
High-density lipoprotein cholesterol
- LDL-C:
-
Low-density lipoprotein cholesterol
- BKNCD:
-
Bandare-Kong Non-Communicable Disease
- PERSIAN:
-
Prospective Epidemiological Research Studies in IrAN
References
Beaglehole R, Bonita R, Horton R, Adams C, Alleyne G, Asaria P, et al. Priority actions for the non-communicable disease crisis. Lancet. 2011;377(9775):1438–47.
WHO. Noncommunicable diseases: Mortality 2021 [Available from: https://www.who.int/data/gho/data/themes/topics/topic-details/GHO/ncd-mortality].
WHO. The top 10 causes of death 2021 [Available from: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death].
Mediterranean WHO-ROftE. Library and information resources 2021 [Available from: http://www.emro.who.int/e-library/index.html].
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289(19):2560–71.
Chockalingam A, Campbell NR, Fodor JG. Worldwide epidemic of hypertension. Can J Cardiol. 2006;22(7):553–5.
Collaborators GBD, Ärnlöv J. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1223–49.
Faramarzi E, Ostadrahimi A, Nikniaz Z, Jafarabadi MA, Fakhari A, Somi M. Determination of the best anthropometric index of obesity for prediction of prehypertension and hypertension in a large population-based-study; the azar-cohort. Iran Red Crescent Med J. 2018;20(3):e59911.
Murray CJL, Lopez AD, World Health O. The global burden of disease: a comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020: summary: World Health Organization; 1996.
Oori MJ, Mohammadi F, Norozi K, Fallahi-Khoshknab M, Ebadi A, Gheshlagh RG. Prevalence of HTN in Iran: meta-analysis of published studies in 2004–2018. Curr Hypertens Rev. 2019;15(2):113–22.
Timpson NJ, Harbord R, Davey Smith G, Zacho J, Tybjærg-Hansen A, Nordestgaard BG. Does greater adiposity increase blood pressure and hypertension risk? Mendelian randomization using the FTO/MC4R genotype. Hypertension. 2009;54(1):84–90.
Hall JE, do Carmo JM, da Silva AA, Wang Z, Hall ME. Obesity-induced hypertension: interaction of neurohumoral and renal mechanisms. Circ Res. 2015;116(6):991–1006.
Dorresteijn JAN, Visseren FLJ, Spiering W. Mechanisms linking obesity to hypertension. Obes Rev. 2012;13(1):17–26.
Chakraborty R, Bose K, Bisai S. Body mass index and blood pressure among adult Bengalee male slum dwellers of Kolkata, India. J Public Health. 2009;17(5):301–8.
Deshmukh PR, Gupta SS, Dongre AR, Bharambe MS, Maliye C, Kaur S, et al. Relationship of anthropometric indicators with blood pressure levels in rural Wardha. Indian J Med Res. 2006;123(5):657.
Ghosh JR, Bandyopadhyay AR. Comparative evaluation of obesity measures: relationship with blood pressures and hypertension. Singapore Med J. 2007;48(3):232.
Venkatramana P, Reddy PC. Association of overall and abdominal obesity with coronary heart disease risk factors: comparison between urban and rural Indian men. Asia Pac J Clin Nutr. 2002;11(1):66–71.
Li N, Yang T, Yu W-Q, Liu H. Is waist-to-height ratio superior to body mass index and waist circumference in predicting the incidence of hypertension? Ann Nutr Metab. 2019;74(3):215–23.
Dobbelsteyn CJ, Joffres MR, MacLean DR, Flowerdew G. A comparative evaluation of waist circumference, waist-to-hip ratio and body mass index as indicators of cardiovascular risk factors. The Canadian Heart Health Surveys. Int J Obes. 2001;25(5):652–61.
Esmaillzadeh A, Mirmiran P, Azizi F. Comparative evaluation of anthropometric measures to predict cardiovascular risk factors in Tehranian adult women. Public Health Nutr. 2006;9(1):61–9.
Nyangasa MA, Buck C, Kelm S, Sheikh MA, Brackmann KL, Hebestreit A. Association between cardiometabolic risk factors and body mass index, waist circumferences and body fat in a Zanzibari cross-sectional study. BMJ Open. 2019;9(7):e025397.
Sinaga M, Worku M, Yemane T, Tegene E, Wakayo T, Girma T, et al. Optimal cut-off for obesity and markers of metabolic syndrome for Ethiopian adults. Nutr J. 2018;17(1):1–12.
Wai WS, Dhami RS, Gelaye B, Girma B, Lemma S, Berhane Y, et al. Comparison of measures of adiposity in identifying cardiovascular disease risk among Ethiopian adults. Obesity. 2012;20(9):1887–95.
Dutra MT, Reis DBV, Martins KG, Gadelha AB. Comparative evaluation of adiposity indices as predictors of hypertension among Brazilian adults. Int J Hypertens. 2018;2018:8396570.
Ashwell M, Gibson S. A proposal for a primary screening tool: Keep your waist circumference to less than half your height’. BMC Med. 2014;12(1):1–6.
Ashwell M, Gunn P, Gibson S. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: systematic review and meta-analysis. Obes Rev. 2012;13(3):275–86.
Deng G, Yin L, Liu W, Liu X, Xiang Q, Qian Z, et al. Associations of anthropometric adiposity indexes with hypertension risk: a systematic review and meta-analysis including PURE-China. Medicine. 2018;97(48):e13262.
Dereje R, Hassen K, Gizaw G. Evaluation of Anthropometric Indices for Screening Hypertension Among Employees of Mizan Tepi University, Southwestern Ethiopia. Integrated Blood Pressure Control. 2021;14:99.
Khader Y, Batieha A, Jaddou H, El-Khateeb M, Ajlouni K. The performance of anthropometric measures to predict diabetes mellitus and hypertension among adults in Jordan. BMC Public Health. 2019;19(1):1–9.
Minh QN, Vo MHN. Anthropometric indexes for predicting high blood pressure in Vietnamese adults: a cross-sectional study. Integrated Blood Pressure Control. 2020;13:181.
Saeed AA, Al-Hamdan NA. Anthropometric risk factors and predictors of hypertension among Saudi adult population–A national survey. J Epidemiol Global Health. 2013;3(4):197–204.
Darbandi M, Pasdar Y, Moradi S, Mohamed HJJ, Hamzeh B, Salimi Y. Discriminatory capacity of anthropometric indices for cardiovascular disease in adults: a systematic review and meta-analysis. Prev Chronic Dis. 2020;17:E131.
Hamzeh B, Bagheri A, Pasdar Y, Darbandi M, Rezaeian S, Najafi F, et al. Predicting metabolic syndrome by anthropometric measures among adults 35–65 years in the west of Iran; a cross sectional study from an Iranian RaNCD cohort data. Diabetes Metab Syndr. 2020;14(5):1293–8.
Chalmers J, MacMahon S, Mancia G, Whitworth J, Beilin L, Hansson L, et al. 1999 World Health Organization-International Society of Hypertension Guidelines for the management of hypertension. Guidelines sub-committee of the World Health Organization. Clin Exp Hypertens (New York, NY: 1993). 1999;21(5–6):1009–60.
Feldstein CA, Akopian M, Olivieri AO, Kramer AP, Nasi M, Garrido D. A comparison of body mass index and waist-to-hip ratio as indicators of hypertension risk in an urban Argentine population: a hospital-based study. Nutr Metab Cardiovasc Dis. 2005;15(4):310–5.
Hu F, Yu R, Han F, Li J, Zhou W, Wang T, et al. Does body mass index or waist-hip ratio correlate with arterial stiffness based on brachial-ankle pulse wave velocity in Chinese rural adults with hypertension? BMC Cardiovasc Disord. 2021;21(1):1–11.
Carey RM, Whelton PK, Committee* AAHGW. Prevention, detection, evaluation, and management of high blood pressure in adults: synopsis of the 2017 American College of Cardiology/American Heart Association Hypertension Guideline. Ann Int Med. 2018;168(5):351–8.
Ebbert JO, Jensen MD. Fat depots, free fatty acids, and dyslipidemia. Nutrients. 2013;5(2):498–508.
Seidell JC, Pérusse L, Després J-P, Bouchard C. Waist and hip circumferences have independent and opposite effects on cardiovascular disease risk factors: the Quebec Family Study. Am J Clin Nutr. 2001;74(3):315–21.
Alzeidan R, Fayed A, Rabiee F, Hersi A, Elmorshedy H. Diagnostic performance of waist-to-height ratio in identifying cardiovascular risk factors and metabolic syndrome among adult Saudis: a cross-sectional study. Saudi Med J. 2020;41(3):253.
Yang H, Xin Z, Feng J-P, Yang J-K. Waist-to-height ratio is better than body mass index and waist circumference as a screening criterion for metabolic syndrome in Han Chinese adults. Medicine. 2017;96(39):e8192.
Stefan N, Häring H-U, Hu FB, Schulze MB. Divergent associations of height with cardiometabolic disease and cancer: epidemiology, pathophysiology, and global implications. Lancet Diabetes Endocrinol. 2016;4(5):457–67.
Wang Q, Wang Z, Yao W, Wu X, Huang J, Huang L, et al. Anthropometric indices predict the development of hypertension in normotensive and Pre-Hypertensive middle-aged women in Tianjin, China: a prospective cohort study. Med Sci Monit. 2018;24:1871.
Gupta S, Kapoor S. Optimal cut-off values of anthropometric markers to predict hypertension in North Indian population. J Community Health. 2012;37(2):441–7.
Buss J. Limitations of body mass index to assess body fat. Workplace Health Safety. 2014;62(6):264.
Program NH. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114(2 Suppl 4th Report):555–76.
Chung W, Park CG, Ryu O-H. Association of a new measure of obesity with hypertension and health-related quality of life. PLoS One. 2016;11(5):e0155399.
Nishida C, Ko GT, Kumanyika S. Body fat distribution and noncommunicable diseases in populations: overview of the 2008 WHO Expert Consultation on Waist Circumference and Waist-Hip Ratio. Eur J Clin Nutr. 2010;64(1):2–5.
Chua EY, Zalilah MS, Haemamalar K, Norhasmah S, Geeta A. Obesity indices predict hypertension among indigenous adults in Krau Wildlife Reserve, Peninsular Malaysia. J Health Popul Nutr. 2017;36(1):1–7.
Park S-H, Choi S-J, Lee K-S, Park H-Y. Waist circumference and waist-to-height ratio as predictors of cardiovascular disease risk in Korean adults. Circ J. 2009;73(9):1643–50.
Lam BCC, Koh GCH, Chen C, Wong MTK, Fallows SJ. Comparison of body mass index (BMI), body adiposity index (BAI), waist circumference (WC), waist-to-hip ratio (WHR) and waist-to-height ratio (WHtR) as predictors of cardiovascular disease risk factors in an adult population in Singapore. PLoS One. 2015;10(4):e0122985.
Zoghi G, Shahbazi R, Mahmoodi M, Nejatizadeh A, Kheirandish M. Prevalence of metabolically unhealthy obesity, overweight, and normal weight and the associated risk factors in a southern coastal region, Iran (the PERSIAN cohort study): a cross-sectional study. BMC Public Health. 2021;21(1):1–8.
Zoghi G, Kheirandish M. Prevalence of type 2 diabetes, obesity, central obesity, and metabolic syndrome in a South Coastal Region, Iran, the PERSIAN Bandare Kong cohort study: a brief report. Hormozgan Medical Journal. 2020;25(1):42–4.
Acknowledgements
BKNCD is a part of PERSIAN national cohort and we would like to appreciate Professor Reza Malekzadeh, Deputy of Research and Technology at the Ministry of Health and Medical Education of Iran and Director of the PERSIAN cohort, and also Dr. Hossein Poustchi, Executive Director of the PERSIAN cohort and Dr. Azim Nejatizadeh Director of BKNCD for all their supports during design and running of BKNCD. We would also like to express our thanks to Bandare-kong cohort members, especially Mr. Mehdi Shahmoradi.
Funding
The Iranian Ministry of Health and Medical Education has funded the study in the PERSIAN Cohort through grant number 700/534.
Author information
Authors and Affiliations
Contributions
MK designed and wrote the manuscript. SR supervised the study and performed the statistical analysis. TA & AA wrote the manuscript. AG was consulted on the possible associated factors to be taken into account. SMH and HZ revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The cohort study received ethical approval from the Ethics Committee of Hormozgan University of Medical Sciences and it was conducted in accordance with the Declaration of Helsinki statements. The associated ethics code is IR.HUMS.REC.1400.347. Informed consent was obtained from all subjects.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Azarbad, A., Aghnia, T., Gharibzadeh, A. et al. Cut-off points for anthropometric indices to screen for hypertension among Iranian adults of the Bandare-Kong cohort: a cross-sectional study. BMC Public Health 22, 2064 (2022). https://doi.org/10.1186/s12889-022-14489-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-022-14489-8