Abstract
Background
The purpose of this study was to analyze cardiopulmonary fitness in Phase I cardiac rehabilitation on the prognosis of patients with ST-Elevation Myocardial Infarction (STEMI) after percutaneous coronary intervention (PCI).
Methods
The study enrolled a total of 499 STEMI patients treated with PCI between January 2015 and December 2015. Patients were assigned to individualized exercise prescriptions (IEP) group and non-individualized exercise prescriptions (NIEP) group according to whether they accept or refuse individualized exercise prescriptions. We compared the incidence of major cardiovascular events between the two groups. IEP group were further divided into two subgroups based on prognosis status, namely good prognosis (GP) group and poor prognosis (PP) group. Key cardio-pulmonary exercise testing (CPX) variables that may affect the prognosis of patients were identified through comparison of the cardio-respiratory fitness (CRF).
Results
There is no significant difference in the incidence of cardio-genetic death, re-hospitalization, heart failure, stroke, or atrial fibrillation between the IEP and the NIEP group. But the incidence of total major adverse cardiac events (MACE) was significantly lower in the IEP group than in the NIEP group (P = 0.039). The oxygen consumption (VO2) at ventilation threshold (VT), minute CO2 ventilation (E-VCO2), margin of minute ventilation carbon dioxide production (△CO2), rest partial pressure of end-tidal carbon dioxide(R-PETCO2), exercise partial pressure of end-tidal carbon dioxide(E-PETCO2) and margin of partial pressure of end-tidal carbon dioxide(△PETCO2) were significantly higher in the GP subgroup than in the PP subgroup; and the slope for minute ventilation/carbon dioxide production (VE/VCO2) was significantly lower in GP subgroup than in PP subgroup (P = 0.010). The VO2 at VT, VE/VCO2 slope, E-VCO2, △CO2, R-PETCO2, E-PETCO2 and margin of partial pressure of end-tidal carbon dioxide CO2 (△PETCO2) were predictive of adverse events. The VO2 at VT was an independent risk factor for cardiovascular disease prognosis.
Conclusions
Individualized exercise prescription of Phase I cardiac rehabilitation reduced the incidence of cardiovascular events in patients with STEMI after PCI. VO2 at VT is an independent risk factor for cardiovascular disease prognosis, and could be used as an important evaluating indicator for Phase I cardiac rehabilitation.
Similar content being viewed by others
Background
Acute STEMI is a leading cause of mortality and morbidity globally. STEMI leads to fatal conditions such as heart failure and sudden cardiac death, and results in an enormous psychological and financial burden on patients and the society [1]. Medication, coronary artery bypass grafting, and percutaneous coronary intervention (PCI) can reduce the morbidity and mortality in patients with STEMI [2, 3]. Medication is a basic treatment for patients before/after PCI. Compared with coronary artery bypass grafting, PCI provides an effective treatment for coronary artery stenosis. However, PCI operation may lead to coronary spasm, endothelial cell injury, and even restenosis or thrombus; moreover, a poor prognosis may still exist in patient with STEMI after PCI [4].
Cardiac rehabilitation (CR) has been found to improve the prognosis for patients with STEMI after PCI [5]. CR includes nutritional therapies, weight loss programs, management of lipid abnormalities with diet and medication, blood pressure control, diabetes management, stress management and physical exercise, and can help the recovery of physical function in patients with cardiac disease or recent cardiac surgeries. Therefore, PCI associated with CR have been recognised internationally as the preferred treatment of STEMI, now PCI combined with CR has become the internationally recognized effective treatment for patients with STEMI. Exercise training is an important part of CR, which not only improves cardiopulmonary fitness and physical activity, but also reduces the morbidity and mortality in patients with STEMI. However, as physical exercise intensifies, it also comes with certain risk. Currently, there is no specific aim for cardiopulmonary fitness in Phase I cardiac rehabilitation according to the American Heart Association (AHA) guidelines [6, 7]. The purpose of this study is to analyze cardiopulmonary fitness in Phase I cardiac rehabilitation on the prognosis of patients with STEMI after PCI, we reviewed all the information and CPX results of STEMI patients after PCI before the discharge and analyze long term prognosis of STEMI patients based on the exercise tolerance.
Methods
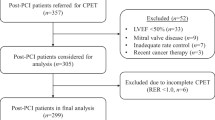
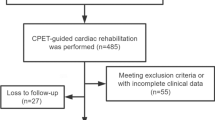
Patients
This retrospective study included a total of 586 STEMI patients treated with PCI in the Department of Cardiology at the First Hospital of Jilin University, between January 2015 and December 2015. After excluding 46 patients who were lost to follow-up and 41 patients who were not administrated with exercise prescription (Table 1), data from 499 STEMI patients were used in the final analyses. The study protocol was approved by the Institutional Review Board of each hospital.
Patients data including age, sex, cardiac function and test indices were collected, including white blood cell (WBC), hemoglobin (HGB), creatinine (Cr), glutamic pyruvic transaminase (AST), glutamic pyruvic aminotransferase (ALT), total cholesterol (TC); high-density lipoprotein cholesterol (HDL-C) and low-density lipoprotein cholesterol (LDL-C). All 499 patients had no contraindication of cardiopulmonary exercise testing. Depending on whether patients accepted or refused individualized exercise prescriptions based on cardio-pulmonary exercise testing (CPX) in Phase I cardiac rehabilitation, they were assigned to the individualized exercise prescriptions (IEP) group (n = 118) or the non-individualized exercise prescriptions (NIEP) group (n = 381). In the IEP group, the intensity of exercise was formulated base on each patient’s cardio-respiratory fitness (CRF) from CPX data [7]. In the NIEP group, the intensity of exercise was limited to Borg 11–13 by subjective sensation [7]. We compared the incidence of major cardiovascular events (MACE) between the two groups. IEP group were further divided into two subgroups based on prognosis status, namely the good prognosis (GP) group (n = 88) and the poor prognosis (PP) group (n = 30). By comparing the CRF between the two groups, we identify key CPX variables that may affect the prognosis of patients.
Quantification of CRF
To accurately quantify CRF, we used CPX which is a widely accepted evaluation tool in both the United States (US) and Europe.[8, 9]. The measurement of ventilatory gas exchange was used for function-based prognostic stratification [9,10,11]. In the IEP group, oxygen consumption (VO2), carbon dioxide production (VCO2), minute ventilation (VE), partial pressure of end-tidal carbon dioxide (PETCO2), and respiratory exchange ratio (RER) were measured in standard exercise testing using Cardio-respiratory instrumentation Medisoft (MS, made in Belgium, SN:130619–05-1470, Model: E100000011000001). The exercise tolerance was estimated from bicycle cycle ergometer work rate. The use of CPX during progressive exercise (10 watts per minute) is based on measurement of exercise gas exchange. The exercise test was terminated if any of the following occurred: abnormal hemodynamic or ECG exercise response or other reasons (i.e., lower extremity muscle fatigue, angina and dyspnoea).
Clinical follow-up
Major adverse cardiac events (MACE) included cardio-genic death, re-hospitalization, heart failure, stroke, and atrial fibrillation. Follow-up data were collected through hospital records and telephone interviews which was conducted every 3 months after discharge until death or December 1, 2017, whichever came first. Mortality data for patients who were lost to telephone follow up were obtained from the population registry bureau. The average follow-up time was 2.5 years.
Statistical analysis
For continuous variables, depending on whether a variable follows a normal distribution, the mean or median was reported and the t-test or nonparametric Wilcoxon’s rank sum test was applied for group comparison. The Chi-square tests were used for categorical variables. Multivariable logistic regression, in which we included age, cardiac function, test indices and variables showing a p-value< 0.05 in the univariate analysis, was used to identify independent risk factors for prognosis. The ROC curve was used to evaluate the predictive value of the model for MACE. All statistical analyses were done using SPSS 19 software (IBM Corp., Armonk, NY, USA).
Results
Incidence of major cardiovascular events
The patients’ clinical data are shown in Table 2. No significant difference in demographics was found between the IEP group and the NIEP group.
The results of adverse events are shown in Table 3. There was no significant difference in the incidence of cardio-genetic death (3 vs. 18, P = 0.442), re-hospitalization (27 vs. 109, P = 0.270), heart failure (3 vs. 13, P = 0.865), stroke (1 vs. 10, P = 0.429), or atrial fibrillation (0 vs. 2, P = 1.000) between the IEP and the NIEP groups. But the incidence of total MACE was significantly lower in the IEP group than in the NIEP group (34 vs. 152, P = 0.039; Fig. 1).
The key CPX variables affecting prognosis
The clinical data of the patients in the IEP group are summarized in Table 4. No significant difference was found between the GP subgroup and the PP subgroup.
The VO2 at VT, E-VCO2, △CO2, R-PETCO2, E-PETCO2 and △PETCO2 were significantly higher in the GP subgroup than in the PP subgroup (P = 0.006, P = 0.017, P = 0.018, P = 0.045, P = 0.005 and P = 0.022, respectively; Table 5). The VE/VCO2 slope was significantly lower in the GP subgroup than in the PP subgroup (P = 0.010). There were no statistically significant differences in other parameters.
We found that VO2 at VT, VE/VCO2 slope, E-VCO2, △CO2, R-PETCO2, E-PETCO2 and △PETCO2 to be predictive of adverse events (the areas under the curve being 0.666, 0.658, 0.646, 0.636, 0.623, 0.670 and 0.638, respectively), and the optimal cut-off point was 10.5 ml/kg/min, 33.4, 0.635 L/min, 0.345 L/min, 30.5 mmHg, 32.5 mmHg, and 2.5 mmHg, respectively (Figs. 2 and 3, Table 6). The VO2 at VT was an independent risk factor for cardiovascular disease prognosis (OR = 0.732, 95% CI: 0.541–0.988, P = 0.042; Table 7). The incidence of cardio-genetic death (0 vs. 3, P = 0.037), re-hospitalization (11 vs. 16, P = 0.033), and total MACE (13 vs. 21, P = 0.005) was significantly lower when the VO2 at VT was greater than 10.5 ml/kg/min (Table 8, Fig. 4).
The ROC curve of VO2 at VT, E-VCO2, △CO2, R-PETCO2, E-PETCO2, and △PETCO2. VO2 at VT: Oxygen consumption per kilogram of weight per minute at anaerobic threshold; E-VCO2: Exercise carbon dioxide production; △CO2: Margin of Minute ventilation carbon dioxide production; R-PETCO2: Rest partial pressure of end-tidal carbon dioxide; E-PETCO2: Exercise partial pressure of end-tidal carbon dioxide; △PETCO2: Margin of partial pressure of end-tidal carbon dioxide
Discussion
This study found that individualized exercise prescription of Phase I cardiac rehabilitation reduced the incidence of cardiovascular events in patients with STEMI after PCI. The key CPX variables, including VO2 at VT, VE/VCO2 slope, E-VCO2, △CO2, R-PETCO2, E- PETCO2 and △PETCO2 were predictive of these adverse events. Furthermore, the VO2 at VT was an independent risk factor for prognosis of cardiovascular disease.
Cardiac rehabilitation is a comprehensive treatment program that includes multiple components such as drug therapy, smoking cessation, exercise, psychology and nutrition. Phase I cardiac rehabilitation is in-hospital rehabilitation, which involves educating patients to recognize disease, prevent disease, and self-management. It can improve the prognosis of patients with unstable angina, acute myocardial infarction and heart failure [10, 11]. A large cohort study found that, in patients with coronary heart disease after revascularization, postoperative cardiac rehabilitations significantly reduced the mortality rate 1–5 years after operation [12]. Our study extends the prior finding by showing that individualized exercise prescription of Phase I cardiac rehabilitation can improve the total MACE of patients than traditional Phase I cardiac rehabilitation. It is somehow disappointing that we did not find significant differences between IEP and NIEP groups, regarding incidence of cardio-genetic death, re-hospitalization, heart failure, stroke, or atrial fibrillation. The reasons are as follows: first, cardiac rehabilitation include patient education, nutrition guidance, medication guidance, smoking cessation and psychological prescription, etc. except for exercise prescription. It shows that other Phase I cardiac rehabilitation parts also plays an important role in cardio-genetic death, re-hospitalization, heart failure, stroke, or atrial fibrillation [13]. Second, our study showed that cardio-genetic death, re-hospitalization, and total MACE decrease significantly when the VO2 at VT was greater than 10.5 ml/kg/min. Our results showed that pre-discharge cardiopulmonary fitness in Phase I cardiac rehabilitation could improve the long term prognosis of the STEMI patients. In addition, other study [14] also show that individualized exercise could not give any major advantage. These findings, taken together, suggest that individualized exercise prescription based on cardiopulmonary fitness was not only effective but also safe.
Exercise prescription guidance can be based on CPX or 6 min walk test (6MWT) [7]. This study adopted the CPX method, which was well recognized as the gold standard aerobic exercise assessment. The use of CRF has many utilizations in clinical, including measuring therapy progress and diagnosis. Although exercise tolerance normally came from the measurement of bicycle cycle ergometer work rate or treadmill, CPX is a more accurate tool to measure CRF. The measurement of CPX depends on the exchange of gases throughout exercise. CPX has got recognition not only it can give accurate measurement of patients with cardiovascular and pulmonary disease, but also it was easier to use because of technological progress, rapid response analyzers and computer-assisted data processing [7]. The 2016 EACPR/AHA scientific statement has indicated that peak VO2, VO2 at VT, and the minute ventilation/carbon dioxide production (VE/VCO2) relationship (VE/VCO2 slope) have prognostic significance [15].
Peak VO2 is defined as the highest O2 uptake obtained during exercise. Its response is resulting from central and peripheral functions, and widely indicates disease seriousness. Lots of studies have demonstrated that noninvasively determined peak cardiac output was regarded as a separate predictor of outcomes that improves the prognostic benefit of Peak VO2 [16,17,18,19]. Present evidence shows that if predicted peak VO2 value is below 50%, patients with heart failure (HF) have a poor prognosis in [20]. The prognostic value of VO2 at VT has been regarded to be a significant prognostic marker when evaluating pre-surgical risk using CPX [21, 22]. Importantly, an accurate and predictable recognition of VO2 at VT is not always possible which has been shown in patients with HF. If VO2 at VT is not predictable, the validity of the CPX should be accepted by providing that the subject attempt to reach an acceptable level (i.e., peak respiratory exchange ratio ≥ 1.00). The present study only uses this index to formulate exercise prescriptions. While the 2016 AHA guide pointed out that VO2 at VT is an independent risk factor for the prognosis of postoperative patients, it did not mention the implication of the index in STEMI patients.
In this study, we found that VO2 at VT is positively correlated with the prognosis of STEMI patients such that patients with VO2 at VT < 10.5 had poor cardiovascular prognosis. Therefore, VO2 at VT can be used as an important evaluation index of Phase I cardiac rehabilitation. It is safe and effective to formulate exercise prescription according to blood pressure, heart rate and watt under VO2 at VT. Large-scale randomized controlled trials are needed to confirm this.
VE/VCO2 slope represents matching of ventilation and perfusion within the pulmonary system, and broadly reflects disease severity as well as prognosis in several patient populations including HF, hypertrophic cardiomyopathy (HCM), pulmonary arterial hypertension (PAH)/secondary pulmonary hypertension (PH), chronic obstructive pulmonary disease (COPD), and interstitial lung Disease (ILD). A VE/VCO2 slope < 30 is considered normal while slight increase is possible with advanced age [7]. The index is usually used to assess the efficiency of ventilation, and involves in detecting high pulmonary pressures [23, 24]. Because pulmonary hypertension is often a consequence of left-sided valvular heart disease [25], the estimate of the VE/VCO2 slope may be particularly helpful. In many asymptomatic patients with severe aortic stenosis, it was found that elevated VE/VCO2 slope could be a significant predictor of decompensated HF or mortality [26]. Studies also showed that measures of ventilator efficiency, specifically the VE/VCO2 slope and PETCO2, may be valuable in patients with HCM as these measures are implicated in increased pulmonary pressures [27, 28]. In this study, we found that VE/VCO2 slope was also a predictor of prognosis in STEMI patients after PCI, with a cut-off point value of 33.4, suggesting that patients with VE/VCO2 slope over 33.4 tended to have poorer prognosis. Impaired cardiac output leads to decreased aerobic metabolism, increased anaerobic metabolism, and decreased VCO2 emissions, which may result in increased VE/VCO2 slope.
In all the CPX variables in patients with systolic HF, peak VO2 and the VE/VCO2 slope have been shown stable separate prognostic significance. While VE/VCO2 slope is a stronger predictive marker in the univariate model compared with peak VO2, there is strong evidence that indicates that a multivariate approach may improve prognostic accuracy [7]. With current healthy management strategies, a VE/VCO2 slope ≥ 45, and a peak VO2/ kg/ min < 10.0 ml are indicative of poorer prognosis over a 4-year period following CPX [27]. In this study, likely because all the patients had acute STEMI, and most of them did not have respiratory dysfunction, the cut-off point of VE/VCO2 slope differed, but the cut-off point of VO2/kg/min was the same as the study of Arena, R. et al. [27].
As VE/VCO2 slope, PETCO2 widely reflects disease severity in lots of patient with HF, HCM, PAH/secondary PH, COPD, and ILD. Both exercise oscillatory ventilation and PETCO2 during rest and exercise have been shown to be of prognostic value in patients with systolic HF [29, 30]. Abnormalities in the VE/VCO2 slope and PETCO2 have been thought to be pulmonary vasculopathy. We found that PETCO2 was also a predictor of the prognosis of patients with STEMI after PCI, such that increased PETCO2 was associated with a better prognosis. The difference in the heart function in the quiet/movement and PETCO2 might be due to difference in infarct area of the patients.
Conclusion
This study found that individualized exercise prescription of Phase I cardiac rehabilitation reduced the incidence of cardiovascular events in patients with STEMI after PCI, and long term prognosis of patients based on their pre-discharge cardiopulmonary fitness. The key CPX variables, including VO2 at VT, VE/VCO2 slope, E-VCO2, △CO2, R-PETCO2, E-PETCO2 and △PETCO2, are predictive of MACE. VO2 at VT was an independent risk factor for cardiovascular disease prognosis and could be used as an important evaluating indicator for Phase I cardiac rehabilitation. Future studies with larger sample sizes are warranted to validate these findings.
Availability of data and materials
The data used to support the findings of this study are available from the corresponding author upon request.
Abbreviations
- △CO2 :
-
Margin of minute ventilation carbon dioxide production
- △PETCO2 :
-
Margin of partial pressure of end-tidal carbon dioxide
- 6MWT:
-
6 min walk test
- AHA:
-
American Heart Association
- ALT:
-
Glutamic pyruvic aminotransferase
- AST:
-
Glutamic pyruvic transaminase
- COPD:
-
Chronic obstructive pulmonary disease
- CPX:
-
Cardio-pulmonary exercise testing
- CR:
-
Cardiac rehabilitation
- Cr:
-
Creatinine
- CRF:
-
Cardio-respiratory fitness
- E-VCO2 :
-
Exercise carbon dioxide production
- GP:
-
Good prognosis
- HCM:
-
Hypertrophic cardiomyopathy
- HDL-C:
-
High-density lipoprotein cholesterol
- HF:
-
Heart failure
- HGB:
-
Hemoglobin
- IEP:
-
Individualized exercise prescriptions
- ILD:
-
Interstitial lung disease
- LDL-C:
-
Low-density lipoprotein cholesterol
- MACE:
-
Major adverse cardiac events
- NIEP:
-
Non-individualized exercise prescriptions
- PAH:
-
Pulmonary arterial hypertension
- PCI:
-
Percutaneous coronary intervention
- PETCO2 :
-
Exercise partial pressure of end-tidal carbon dioxide
- PETCO2 :
-
Partial pressure of end-tidal carbon dioxide
- PETCO2 :
-
Rest partial pressure of end-tidal carbon dioxide
- PH:
-
Pulmonary hypertension
- PP:
-
Poor prognosis
- RER:
-
Respiratory exchange ratio
- STEMI:
-
ST-segment elevation myocardial infarction
- TC:
-
Total cholesterol
- VCO2 :
-
Carbon dioxide production
- VE :
-
Minute ventilation
- VE/VCO2 slope:
-
Slope for minute ventilation/carbon dioxide production
- VO2 at VT:
-
Oxygen consumption per kilogram of weight per minute at anaerobic threshold
- VO2 :
-
Oxygen consumption
- VT:
-
Ventilation threshold
- WBC:
-
White blood cell
References
Mozaffarian D, et al. Heart disease and stroke statistics--2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29–322.
Yusuf S, et al. Global burden of cardiovascular diseases: part I: general considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation. 2001;104(22):2746–53.
Smith SC Jr, et al. ACC/AHA guidelines of percutaneous coronary interventions (revision of the 1993 PTCA guidelines)--executive summary. A report of the American College of Cardiology/American Heart Association task force on practice guidelines (committee to revise the 1993 guidelines for percutaneous transluminal coronary angioplasty). J Am Coll Cardiol. 2001;37(8):2215–39.
Zhang Y, Ma XJ, Shi DZ. Effect of Trimetazidine in patients undergoing percutaneous coronary intervention: a meta-analysis. PLoS One. 2015;10(9):e0137775.
Zhang Y, et al. Cardiac rehabilitation in acute myocardial infarction patients after percutaneous coronary intervention: a community-based study. Medicine (Baltimore). 2018;97(8):e9785.
Fletcher GF, et al. Exercise standards for testing and training: a scientific statement from the American Heart Association. Circulation. 2013;128(8):873–934.
Guazzi M, et al. EACPR/AHA scientific statement. Clinical recommendations for cardiopulmonary exercise testing data assessment in specific patient populations. Circulation. 2012;126(18):2261–74.
Arena R, Myers J, Guazzi M. The future of aerobic exercise testing in clinical practice: is it the ultimate vital sign? Futur Cardiol. 2010;6(3):325–42.
Lauer M, et al. Exercise testing in asymptomatic adults: a statement for professionals from the American Heart Association Council on clinical cardiology, subcommittee on exercise, cardiac rehabilitation, and prevention. Circulation. 2005;112(5):771–6.
Balady GJ, et al. Clinician’s guide to cardiopulmonary exercise testing in adults: a scientific statement from the American Heart Association. Circulation. 2010;122(2):191–225.
Kaminsky LA, Arena R, Myers J. Reference standards for cardiorespiratory fitness measured with cardiopulmonary exercise testing: Data From the Fitness Registry and the Importance of Exercise National Database. Mayo Clin Proc. 2015;90(11):1515–23.
Suaya JA, et al. Cardiac rehabilitation and survival in older coronary patients. J Am Coll Cardiol. 2009;54(1):25–33.
Pavy B, et al. Therapeutic education in coronary heart disease: position paper from the working Group of Exercise Rehabilitation and Sport (GERS) and the therapeutic education Commission of the French Society of cardiology. Arch Cardiovasc Dis. 2013;106(12):680–9.
Powell R, et al. Is exercise-based cardiac rehabilitation effective? A systematic review and meta-analysis to re-examine the evidence. BMJ Open. 2018;8(3):e019656.
Guazzi M, et al. Focused update: clinical recommendations for cardiopulmonary exercise testing data assessment in specific patient populations. Circulation. 2016;133(24):e694–711.
Miki K, et al. Impairments and prognostic factors for survival in patients with idiopathic pulmonary fibrosis. Respir Med. 2003;97(5):482–90.
Colice GL, et al. Physiologic evaluation of the patient with lung cancer being considered for resectional surgery: ACCP evidenced-based clinical practice guidelines (2nd edition). Chest. 2007;132(3 Suppl):161S–77S.
Torchio R, et al. Exercise ventilatory inefficiency and mortality in patients with chronic obstructive pulmonary disease undergoing surgery for non-small-cell lung cancer. Eur J Cardiothorac Surg. 2010;38(1):14–9.
Holverda S, et al. Cardiopulmonary exercise test characteristics in patients with chronic obstructive pulmonary disease and associated pulmonary hypertension. Respiration. 2008;76(2):160–7.
Arena R, et al. Determining the preferred percent-predicted equation for peak oxygen consumption in patients with heart failure. Circ Heart Fail. 2009;2(2):113–20.
Hennis PJ, Meale PM, Grocott MP. Cardiopulmonary exercise testing for the evaluation of perioperative risk in non-cardiopulmonary surgery. Postgrad Med J. 2011;87(1030):550–7.
Smith TB, et al. Cardiopulmonary exercise testing as a risk assessment method in non cardio-pulmonary surgery: a systematic review. Anaesthesia. 2009;64(8):883–93.
Guazzi M, Myers J, Arena R. Cardiopulmonary exercise testing in the clinical and prognostic assessment of diastolic heart failure. J Am Coll Cardiol. 2005;46(10):1883–90.
Guazzi M, et al. Cardiopulmonary exercise testing variables reflect the degree of diastolic dysfunction in patients with heart failure-normal ejection fraction. J Cardiopulm Rehabil Prev. 2010;30(3):165–72.
Guazzi M, et al. Exercise oscillatory breathing in diastolic heart failure: prevalence and prognostic insights. Eur Heart J. 2008;29(22):2751–9.
Giardini A, et al. Ventilatory efficiency and aerobic capacity predict event-free survival in adults with atrial repair for complete transposition of the great arteries. J Am Coll Cardiol. 2009;53(17):1548–55.
Arena R, et al. Defining the optimal prognostic window for cardiopulmonary exercise testing in patients with heart failure. Circ Heart Fail. 2010;3(3):405–11.
Arena R, et al. Ventilatory efficiency and resting hemodynamics in hypertrophic cardiomyopathy. Med Sci Sports Exerc. 2008;40(5):799–805.
Corra U, et al. Oscillatory ventilation during exercise in patients with chronic heart failure: clinical correlates and prognostic implications. Chest. 2002;121(5):1572–80.
Task Force of the Italian Working Group on Cardiac Rehabilitation, P, et al. Statement on cardiopulmonary exercise testing in chronic heart failure due to left ventricular dysfunction: recommendations for performance and interpretation. Part I: definition of cardiopulmonary exercise testing parameters for appropriate use in chronic heart failure. Eur J Cardiovasc Prev Rehabil. 2006;13(2):150–64.
Acknowledgements
We thank Dr. Jingyun Yang for the help in editing the manuscript.
Funding
This assessment is funded by National Key R&D Program of China:NO. 2016YFC0900903. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
PC and YZ conceived and designed the study. HC, ZL, XZ, RL, WS, LW and LZ performed the experiments and statistical analysis. HC wrote the paper. PC and YZ reviewed and edited the manuscript. All authors read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Approved by Medical Ethics Committee of The First Hospital of Jilin University. Approval Number: 2016–281.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests, and all authors should confirm its accuracy.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Cai, H., Zheng, Y., Liu, Z. et al. Effect of pre-discharge cardiopulmonary fitness on outcomes in patients with ST-elevation myocardial infarction after percutaneous coronary intervention. BMC Cardiovasc Disord 19, 210 (2019). https://doi.org/10.1186/s12872-019-1189-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-019-1189-x