Abstract
In countries where headache services exist at all, their focus is usually on specialist (tertiary) care. This is clinically and economically inappropriate: most headache disorders can effectively and more efficiently (and at lower cost) be treated in educationally supported primary care. At the same time, compartmentalizing divisions between primary, secondary and tertiary care in many health-care systems create multiple inefficiencies, confronting patients attempting to navigate these levels (the “patient journey”) with perplexing obstacles.
High demand for headache care, estimated here in a needs-assessment exercise, is the biggest of the challenges to reform. It is also the principal reason why reform is necessary.
The structured headache services model presented here by experts from all world regions on behalf of the Global Campaign against Headache is the suggested health-care solution to headache. It develops and refines previous proposals, responding to the challenge of high demand by basing headache services in primary care, with two supporting arguments. First, only primary care can deliver headache services equitably to the large numbers of people needing it. Second, with educational supports, they can do so effectively to most of these people. The model calls for vertical integration between care levels (primary, secondary and tertiary), and protection of the more advanced levels for the minority of patients who need them. At the same time, it is amenable to horizontal integration with other care services. It is adaptable according to the broader national or regional health services in which headache services should be embedded.
It is, according to evidence and argument presented, an efficient and cost-effective model, but these are claims to be tested in formal economic analyses.
Similar content being viewed by others
Introduction
Governments, politicians and health-service managers concerned about the cost of headache care for very large numbers of people fail to recognize a fundamentally important aspect of the economics of headache disorders: untreated, they are a huge financial drain. The high levels of disability repeatedly attributed to headache, and migraine in particular [1,2,3,4,5,6,7,8,9], are expressed not only as lost health but also in lost productivity [10,11,12,13,14,15] and detriments to gross domestic product (GDP) [16,17,18,19].
In an enlightened view, this is an opportunity. A wealth of evidence attests the efficacy of treatments for migraine and other primary headache disorders that can well be provided by non-specialists [20]. In a reasonable expectation, good health care delivering these treatments efficiently to those who will benefit from them will substantially reduce the ill-health burden of headache. The costs may be high – because there are very many such people – but, again in a reasonable expectation, interventions achieving this purpose will be cost-effective [21]. In many economies they may be cost saving, through the recovery of lost work time [22].
Regrettably, throughout the world, the opportunity is missed: health-care systems that ought to provide this care either do not exist or, where they do, fail to reach many who need it [23, 24].
In this manuscript, a product of the Global Campaign against Headache [24,25,26], we aim to show the solid basis of these expectations. In so doing, we aim, more pertinently, to generate political recognition of the need to address this health-care failure and the educational failures lying behind it [22]. Further, by setting out a model of how they can be addressed, we lay the foundations for economic analyses demonstrating the value of treating headache.
Methods
Experts from all world regions, in headache, health service organization or health-technology assessment, were brought together to contribute to these proposals through email correspondence. The group was diverse, with members drawn from high-, middle- and low-income countries.
They took evidence from the published literature and, using this, built a headache-care model by developing and refining previous proposals for headache service organisation [27,28,29] put forward by Lifting The Burden (LTB) [26] and the European Headache Federation (EHF) [30]. They extended the applicability of the model beyond Europe through their own expertise and local knowledge and by drawing from experience and understanding gained by the Global Campaign against Headache during its 16 years of activities worldwide [26].
The problems
The challenge of numbers
Headache disorders are common, and, although most are episodic, in many cases they are lifelong conditions. They are also acknowledged to be among the top three causes of disability in the world [5,6,7,8,9]. Three – migraine, tension-type headache (TTH) and medication-overuse headache (MOH) – account for almost all headache-attributed burden [1, 5,6,7,8]: burden expressed in personal suffering, disability, impaired quality of life and financial cost as well as impact extending beyond those immediately affected [10].
Given all of this, it is unsurprising that large numbers of people with headache seek health care [31,32,33]. For example, in a United Kingdom (UK) study based in primary care 20 years ago, 17% of registered patients aged 16–65 years had consulted a general practitioner (GP) because of headache [33]. This is a good example because, in the UK, virtually everyone is registered with a GP.
However, existence of a health disorder, even one that is manifestly burdensome, does not translate directly into need for professional health care. Need in the context of health economics and policy is defined with regard to potential for benefit. Effective treatments exist [20, 34], but the proposal that everyone with headache has need for professional care is not arguable in a resource-limited world. Need is predicated on anticipated benefit, but this must rise above a threshold of benefit, itself judged against benefit achievable by other means (cost-effectiveness).
Headache-related health care needs assessment
Thresholds are hard to set objectively, although needs assessments are highly sensitive to them.
A previous estimate – essentially based on expert opinion – is that 50% of people with headache can manage themselves, using, if necessary, simple over-the-counter (OTC) medications [28]. They do not, or rather should not, need professional health care. While this estimate reflects the proportion of successful outcomes in clinical trials of OTC medications, these have almost all been conducted in patients, who are not the relevant denominator.
Many people do manage themselves, a large proportion through necessity, others from choice, none of them necessarily effectively. Those who choose self-management are not only the less severely affected [35]: they include a number who, for whatever reason and despite significant disability [36, 37], expect the marginal benefit of professional involvement in their care to be small (sub-threshold benefit negates need). Here is a problem, because expectations are quite often unrealistic – too high, or sometimes too low – so that needs assessment based on what people currently do [31,32,33, 35,36,37,38,39,40,41,42,43,44,45,46,47] has very questionable validity. This is more so when service improvement is planned: a better service – if “better” means delivering enhanced benefit – should see greater usage than a poor service it replaces (discovered need). While planning must factor this in, it is difficult to estimate.
Aside from these consumer-driven issues, another is also threshold-dependent. Cash-limited health services seek value for money: they will discount assessed needs, however great, whenever utility gain per unit of health-care resource consumption will be low. In headache medicine, the potential for benefit from professional health care is generally greatest among those worst affected, so that health policy might reasonably focus on these. Further, both migraine and MOH can, in most cases, be treated not only effectively but also at rather low cost [20, 21].
What follows – an assessment of how much professional headache care should be provided as a matter of policy – updates earlier estimates [27,28,29]. The approach adopted is conservative: it will under- rather than overestimate need. As will become apparent, any other approach would be unhelpful.
As with all economic assessments, there are many assumptions.
The first is that only those with disabling headache need professional care. The implication that others can adequately look after themselves is possibly unfair, but the assumption respects a reasonable view of priority. It effectively and helpfully removes most people with episodic TTH from consideration, this disorder generally (again perhaps unfairly [48]) being regarded as not significantly disabling [49] (There is also little that professional care can do for most episodic TTH beyond offering OTC medications [20]).
About two thirds (66%) of the world’s population are aged 15–64 years [50], these being the years during which headache disorders tend to be troublesome. About 25% are aged 14 or under [51]. Thus, with regional variations, in every million people living in the world there are 660,000 and 250,000 in these age groups respectively. Primary headache is less common, and less troublesome, in older people [1], who therefore contribute negligibly to expected numbers.
Best current epidemiological evidence suggests that a global average of about 15% of adults aged 15–64 have migraine [1, 6]. Further evidence is that 80% of these 15% (ie, 12%) are significantly disabled through pain and associated symptoms [52]. In every million people in the world, therefore, there are 80,000 adults (12% of the 660,000 aged 15–64 years) who need care because of migraine-attributed disability. A small proportion of adults have chronic TTH. While this is likely to be disabling, their numbers are not reliably known, partly because epidemiological data are limited and partly because conflation with MOH makes these data unreliable. As for MOH, the proportion varies greatly from country to country, with the best and most recent estimate suggesting a global mean prevalence of 1.5% [53]: another 10,000 (1.5% of the 660,000) needing care for two reasons. MOH is rated as highly disabling [49, 54], not surprisingly since it is frequently recurring by definition and very painful when present [55]. Although medication overuse may be the means by which many people with MOH nonetheless remain (partly) functional, it always requires professional care because it will not otherwise resolve.
The total of 90,000 per million (13.5% of the 660,000), which ignores TTH for reasons stated, is only one third of the estimated prevalence of all headache including TTH [1, 6] – substantially less than the 50% proposed earlier as being the proportion in need of professional care [28]. It may be over-conservative: it is somewhat below the UK finding (above) that 17% of GP-registered adults consult for headache [33], but this, although essentially a population-based observation, was a reflection of demand, not need. These, as we argue below, are not the same.
Needs arise in the child and adolescent populations also, but are more difficult to quantify, partly because there are fewer data – and none that are reliable in very young children (below 6 years) [1, 56]. In the age range 6–14 years, headache is apparently as common as in adults [1, 56, 57], but it has different characteristics. While migraine prevalence is lower, dependent upon age and reaching adult levels during the course of adolescence, undifferentiated headache (UdH) largely fills its place, albeit with less disabling consequences [57]. Furthermore, even migraine in these age groups tends to be short-lasting. In the absence of better data, a conservative but reasonable working basis is that headache-care needs in these age groups, in terms of numbers, are, proportionately, half those of adults [28, 29]: another 17,000 (0.5*13.5% of the 250,000 aged 14 or under) in each million of the population.
Service provision requirement
From these statistics, with some further assumptions, we can make arguably fair estimates of service requirements.
First is an assumption about demand. Need and demand overlap, but are not the same – each can exist without the other. Need for professional headache care, defined as above (ie, with regard to potential for benefit), becomes demand only in those who seek care. On the other hand, care may also be sought in the absence of need (as defined). Complex and poorly understood factors govern health-care seeking behaviour and care utilization by people with headache [35]. On the negative side are the obstacles to care described below (see The “patient journey”, and “care pathway”), which act as deterrents. Failed self-management is a positive driver. False expectations – too high or too low - have positive or negative influences accordingly. Evidence suggesting that demand for headache care is expressed by as few as half of those who might be considered in need [33, 35, 36, 58] is unreliable, because studies reporting this were not well able to judge need for care. Further, it is uncertain whether needs assessment for the purpose of service provision should reflect needs expression rather than a more objective assessment of need (as we wrote earlier, needs assessment based on what people currently do has very questionable validity). But we will adopt this estimate, pragmatically, because no other exists. If demand is indeed suppressed by barriers to care, better and more accessible services, dismantling these barriers, will generate increase. We assume that take-up of improved services will still not be 100%, but 75%, representing a closure of half the currently estimated gap [21].
Second are multiple assumptions about time (Table 1). These are based on expert views of requirement [21, 28, 29] but tempered with conservatism. They consider only ambulatory care: inpatient management is ignored in view of the minimal requirement for it. Admission is sometimes good practice, because of comorbidities or for detoxication in MOH, but only in a tiny percentage of patients.
Notwithstanding the conservatism pervading the assumptions, Table 2 sets out very challenging estimates of service requirement. We say more about this below (see The health-care solution).
The failing status quo: inefficient and inequitable services, and not only in low-income countries
The “patient journey”, and “care pathway”
Evidence from throughout the world is that headache care reaches a minority of those who need it [22, 35,36,37,38,39,40] (to say nothing about its quality).
The primary reason is a worldwide context of low priority accorded to headache disorders in the queue for health-care resources, evident for over 20 years [59]. A decade ago, the World Health Organization (WHO) published its Atlas of Headache Disorders and Resources in the World 2011, recording the worldwide ill health caused by headache [22]. Noting that this was mostly untreated, WHO called for change, in a message distributed to the health ministries of every country [22]. In the 10 years since, change has not been in evidence [9, 23], although attention among WHO’s member states is beginning now to fall on neurological diseases (including headache) [60].
We estimated above that two thirds of people with headache could manage themselves, needing no more than advice from pharmacists [36]. As we will show, keeping these people out of the health-care system is crucial to efficient and equitable implementation of care. But many people who might succeed in self-management lack the small amount of knowledge on which success depends, and receive neither educational nor practical support to help them. Instead, they join the queue for health care, thus, unnecessarily, embarking upon the “patient journey”.
The one third who do need professional care are likely to find the patient journey overcrowded and frustrating, with headache services fragmentary or difficult to access and the “care pathway” a mere misnomer – winding and beleaguered by culs-de-sac and poor signposting [61]. One consequence is direct presentation to emergency departments, without justifying medical need but benefiting the patient (at high cost) by bypassing the care pathway altogether [62, 63].
“Headache services”, if existing at all, are too often equated with headache clinics, usually located sporadically and in big urban centres according more to market forces than objective assessment of need. Public perception is often the driver, encouraged by policies in many countries that allow direct (and often unguided) self-referral to specialists. Iran, a country with well-developed health services, is a good example, with many people taking fruitless paths to neurosurgeons, otorhinolaryngologists, ophthalmologists or pain clinics (the poorly signposted care pathway [61]). In Russia, one in every three people receiving care for migraine have gone directly to neurologists [18]. In Estonia, also a country of the former USSR but with well-developed primary care and a referral system, the proportion sent by GPs to neurologists prior to an educational intervention was a not dissimilar 39.5% [64]. In Western Europe, also one in three people treated for headache in Spain, and one in four in Luxembourg, see specialists for this purpose [40]. In Greece, only one fifth of people with headache seek professional care, but most of these do so from private neurologists [65]. In the UK, where GPs maintain a gatekeeper role as an essential feature of the national health service, the proportion (9%) referred to secondary care [33] was in line with reasonable expectation (see below: Division of caseload). Neurologists, however, receiving most of these referrals, reported that up to a third of all their patients consulted for headache, more than for any other neurological condition [31].
Of course, specialist clinics are needed [66], but only by those with complex disorders requiring high-end multidisciplinary care, who are a small minority [28, 29]. If specialist clinics with their very limited capacity are at the centre rather than the apex of headache services, this purpose is likely to be thwarted by the overload of patients whose needs should be met elsewhere. Most people with headache have one of only a few very common disorders, which ought to be wholly familiar to primary-care providers and only rarely present diagnostic or management difficulties [20, 28]. But the underlying problem is that non-specialist care for headache is variable at best.
There are illustrative and revealing studies. To begin in high-income countries [67], in a population-based study in United States of America (USA) and UK, only two thirds of adults with migraine were found to be correctly diagnosed [35]. Half were consulting health-care providers (HCPs) – too many according to our earlier (conservative) estimate – but over 60% of those not consulting exhibited high migraine-related disability [35]. There was probable ascertainment bias in this study, but nonetheless it was indicative of malfunctioning care pathways in both countries. More recently, the Eurolight study in 10 European Union (EU) countries found that, among participants with frequent migraine and an unambiguous need for preventative medication (more than five headache days per month), fewer than 20% had received medical care at any level [68, 69]. Incorporating indices of adequacy of care, this study identified adequate acute treatment in barely half of these (ie, fewer than 10% in most of the countries) and even smaller proportions with the preventative medication for which they were clearly eligible [40]. In upper-middle-income Russia [67], again in a population-based survey, only 15% nationwide of people with headache were consulting, one third, as noted, with specialists [18, 41]. In lower-middle-income Nepal [67], also in a population-based survey, a much higher 58% of participants with headache had consulted a professional HCP in the previous year, and 8% had seen a specialist of some sort [42]. While these findings suggest better availability of health care in Nepal than in many other, much wealthier countries (Japan [38] and Taiwan [43], EU countries [40, 44] and UK and North America [35, 45, 46, 52]), all is not as it seems. The count of “medical consultations” in Nepal included a very wide range of HCPs, some with no counterparts or who would not be accredited as health professionals in other countries [42]. With pharmacist consultations (15%) excluded, the consulting proportion fell to 43% [42], similar to the 47% in China [47]. In the most salient comparison, with only physician-consultations considered, the proportion fell further to 19% (GPs 11%, specialists 8% [42]), much lower than those elsewhere [35, 38, 43, 45,46,47, 52] – except for Russia [18, 41]. Further, since there are no headache specialists and few neurologists in Nepal, “specialist” consultations were mostly with ophthalmologists, otorhinolaryngologists or psychiatrists [42]. In other words, these findings reflected high demand without indicating good care: on the contrary, headache-attributed burden in Nepal remains egregiously high [70].
Educational failures – the root of the problem
The origins of these health-care failures are clearly traceable to educational failures, occurring at every level [22].
On the political level, few governments appear willing to take concerted action against headache [9, 23, 71]. This is puzzling [8, 22]. It indicates a lack of awareness either of its substantial population ill-health burden (increasingly unlikely, since the Global Burden of Disease [GBD] study repeatedly affirms this [2,3,4,5,6,7,8]) or of its equally substantial but potentially reversible economic burdens on society [11,12,13,14,15,16,17,18,19, 21].
Among HCPs, very limited training in headache [22] does little to engender interest, good outcomes or, ultimately, satisfaction among themselves or their patients. For doctors this is a problem sewn in medical schools, the consequence, again, of low priority: worldwide, only 4 h are committed to headache disorders in 4–6 years of formal undergraduate medical training [22].
Among the general public, headaches – neither fatal nor contagious, and often invisible – are trivialized as “normal”, and, far worse, seen by some, in those who complain of them, as no more than an excuse to avoid responsibility [23, 72].
All of these need to change.
The health-care solution
The numbers estimated above (see Service provision requirement) cannot be regarded as precise: they are sensitive to the multiple assumptions, particularly those related to time (Table 1). But, from them, two conclusions are certain.
First of these is that specialist care, with its very limited capacity, cannot meet all needs, or even a substantial part of them. Systems or practice that lead to large numbers of headache referrals to neurologists or other specialists must be questioned.
Second, and the corollary to this, is that headache care in the main belongs and must be delivered in primary care. This is not undesirable for two principal reasons (others have to do with efficiency and cost containment). On a neutral level there is, as noted, no clinical objection to it: education may be required, but the necessary skills exist in primary care [20, 28]. On the plus side, since WHO’s Declaration of Alma-Ata of over 40 years ago [73], wherever health-care reform is in progress there is emphasis on strengthening primary care, with its benefits of continuity and care in the community [60, 73,74,75,76,77]. While models of health care vary throughout the world, whatever the overarching system of care, primary care has a recognized and important role nearly everywhere. In highly rural regions, those of sub-Saharan Africa, for example, primary care in whatever form it takes is the only point of contact for most patients.
Structured headache services
Systems approach to health care
Drawing from engineering theory, a systems approach to a problem or need first identifies it (“understanding the problem space” – which the foregoing has done) and then pulls together system elements that, working together, will resolve the problem or meet the need (“the solution space”) [78]. There are steps in the process, working from needs to requirements and from design to integration to delivery [78], but these do not need to be detailed here. The key feature shared by all well-functioning systems – in health care as much as in engineering – is that “their elements together produce results not obtainable by the same elements alone” [78]. Applicable particularly to health care, a systems approach involves “integrating the necessary disciplines into a team who then use a structured process to deliver a system” [78]. The health-care solution to headache is envisioned through applying this approach to headache care.
Nationwide structured and educationally supported headache services embedded and integrated within a country’s health-care system are the means of efficiently, effectively and equitably mitigating the personal and societal burdens of headache to the greatest extent possible with resources available, a proposition put forward by LTB and endorsed by WHO a decade ago [22]. Structured headache services pull elements together from primary, secondary and specialist (tertiary) care, and, importantly, from pharmacy services. Equally importantly, they also harness self-management. Educational supports are an additional element, required at all system levels and including public education on when and how to make correct use of these services. Integration within the broader health-care system is crucial: if headache services merely develop ad hoc, driven not by coherent policy but opportunistically by interested individuals, as is now the case in most countries providing any service at all, they can be neither efficient nor equitable.
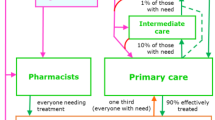
The essential purposes of headache-service organization are two-fold: to create capacity matched to need, and to divide service provision rationally between provider levels. The guiding principle in both purposes is that management of patients should be at the lowest level commensurate with good care. Achieving this makes most efficient use of allocated resources. Basing headache services in primary care (Fig. 1) extends reach and affords ease of access [60, 73,74,75,76,77]. Higher levels are reserved for those with high-frequency, complex or rare headache disorders, perhaps complicated by comorbidities that require multidisciplinary care [28, 29, 66].
Graphic depiction of headache services organized on three levels, but based in primary care, with predicted caseloads (see text and Table 3 for explanation). Inset: arguably a better depiction
A model of headache-service organization
The focus of headache services should be on migraine and MOH (see above: Headache-related health care needs assessment [27,28,29]). This does not exclude other headache disorders, but TTH, the most prevalent headache, is almost always self-manageable [20, 28, 79] while other primary headaches are far less common. As for secondary headaches, their management is of the causative disorder, and therefore, with a few exceptions (notably MOH), outside the ambit of headache services. But provision is needed for their recognition, since this is the responsibility of the services to which affected patients present – most likely to be headache services when headache is the symptom.
While organized headache services, if they are to be efficient and equitable, must be embedded in national or regional health services, these vary throughout the world, differently structured and not always adequately resourced. The model proposed (Fig. 2; Table 3), incorporating three interdependent levels with facilitated but controlled pathways between them while expanding the contribution from primary care, is a general guide and template adaptable to these variations. It is the interventional model adopted as the health-care solution to headache by the Global Campaign against Headache [24, 25]. The account here develops and refines earlier proposals [27,28,29].
Level 1. General primary care
Primary care is the front line of headache services (Figs. 1 and 2), available locally and accessible to all who need them. This is not everyone with headache: the estimated two thirds able to manage themselves (see above: Headache-related health care needs assessment) should do so, with advice from pharmacists and guidance from public educational programmes built into the model (see below: Educational implications).
Pharmacy services (perhaps level 0) need to be highlighted here. They are often greatly underutilized. Pharmacists are experts in the effects (wanted and unwanted) and uses of medications and generally the most easily accessible of all HCPs. Pharmacists can give guidance and advice not only on self-management but also on when further professional care should be sought [36].
Level 1 is provided by non-specialist HCPs, not necessarily physicians in a health-care system more dependent on other practitioners (clinical officers, nurses or community health workers, for example), although authority to prescribe is a requirement for non-OTC medications. Occupational health services can be a helpful adjunct, also provided in proximity to need (especially given the impact of headache on work). Whatever their background, HCPs providing level-1 care will need basic knowledge and understanding of headache disorders for this purpose, and many will therefore require some training in headache (see below: Educational implications). But the model does not require every HCP in primary care to offer headache services if they can share caseload between themselves according to their skills and interests, an arrangement that may be administratively easy in group practices or health centres.
Management aids designed to facilitate non-expert care are an important support to level 1 [20]. With these and the educational supports, this level should competently meet the needs of most people needing professional care for headache [28, 80]: most cases of migraine (and almost all of TTH, if needing care) can be diagnosed and managed here by HCPs who should be familiar with recommended acute and preventative drugs [30] and aware of the constraints in managing fertile women (important since these are a high proportion of people with migraine). Cluster headache, MOH and some other common secondary headache disorders listed in Table 4 should be recognized but not necessarily managed, and red-flag warnings of serious secondary headaches should also be recognized and duly acted upon [20]. Channels for referral to levels 2 and 3, urgently when necessary, should be in place for these cases, and for other patients who are diagnostically complex or difficult to manage [28, 29].
Level 1 therefore controls flow to higher levels. There is more to be said about this (see below: The gatekeeper role within the model).
Finally, this level should continue the long-term care of patients discharged with treatment plans (as they should be) from levels 2 or 3 [28, 29, 66, 82].
Level 2. Special-interest headache care
Level 2 may be in primary care, provided by HCPs (usually but not essentially GPs), but in many countries it is more likely to be offered in secondary-care polyclinics or district hospitals and by neurologists (sometimes general physicians, specialists in other fields of internal medicine or psychiatrists). Either fits the model, with training in headache to a more advanced but not specialist level (see below: Educational implications).
Level 2 provides more skilled ambulatory care, and has capacity only for the relatively small proportion of patients needing this (Figs. 1 and 2, and see below: Division of caseload). Competence should embrace the diagnosis and management of more difficult cases of primary headache, with experience in using the full range of medications. It should extend to some secondary headache disorders, though not those that are very rare [66]. Ideally, HCPs at level 2 should have access to other services such as neuroimaging, psychology and physiotherapy. Where this is not possible, and anyway for the minority of their patients outside their competence (Table 5), they require a referral channel to level 3 [28, 29].
To maintain efficiency, level 2 should repatriate patients to level 1, with management plans, as soon as is clinically appropriate.
Level 3. Headache specialist centres
Specialized headache centres sit at the apex of structured headache services (Fig. 1) [66].
In many countries, they remain an unfulfilled aspiration; in others, they exist – disadvantageously to them – without the lower levels in place, or are inequitably distributed. As an example of the last, a survey in Brazil identified 243 “headache specialists” in 2004/2005. These were more than twice the number estimated to be needed for Brazil’s 198 million people [83] in a well-functioning 3-level system (see below: Division of caseload), but 68% were in the south-east region catering for only 42.6% of the country’s population; by contrast, 12.4% were in the north-east for 28.1%, and five of Brazil’s 27 States had none [84].
The first and foremost role of specialized headache centres, as tertiary referral centres, is to manage the very small proportions of patients with primary headache disorders that are especially difficult to diagnose or treat, or with secondary headaches requiring multidisciplinary management [81], and those who for other reasons, such as comorbidities, need specialist intervention [28, 66, 82, 85, 86] (Figs. 1 and 2; Table 5). For this role, they employ accredited headache specialists or neurologists, and concentrate experience in the rare headache disorders and cranial neuralgias [28, 66]. They have access to equipment and specialists in other disciplines for the diagnosis and management of the underlying causes of all secondary headache disorders [66]. They provide limited but full-time inpatient facilities (see below: Division of caseload). Specialized headache centres are therefore situated within or closely affiliated (with access rights) to a university or other major hospital [66].
In their second role, level-3 centres support non-specialists at levels 1 and 2 through clinical advice, training and development of national management guidelines [66]. Sustained through bidirectional links, this is a symbiotic relationship: well-functioning lower levels reduce demand on the very limited capacity at level 3. In this role, level 3 both maintains standards throughout the system and protects its ability to perform its first role.
Repatriation of patients to level 1 (or 2) as soon as is clinically appropriate also protects this ability. Again, this should be with management plans.
Less essential additional roles, including locally mandated or broader-based research, have been described [66].
Provision for children and adolescents
Although their needs may differ, the model of care is the same for these age groups, with front-line services (level 1) in primary care. To the extent that neurological services provide higher levels of care, these may be replaced by child neurology or paediatric services. The latter, in some countries, are better developed than neurological services.
Division of caseload
Quantitative estimates of the proportions of patients with care needs at each level are largely based on expert opinion [27,28,29], but with some empirical support [33]. They shape the model as a broad-based pyramid with a narrow apex (Fig. 1). Assuming all levels are in place and functioning efficiently, they predict 90% managed at level 1 and about 10% at higher levels, with no more than 1% of all headache patients at level 3 [28] (Fig. 2).
On these estimates and the earlier assumptions about consultation times (Table 1), one full-time equivalent (FTE) HCP at levels 1, 2 or 3 can provide care at those levels to populations no larger than 25,000, 200,000 and 2 million respectively [28, 29]. (One FTE HCP does not necessarily imply one engaged full-time in headache services; it could, for example, be two HCPs engaged half time in headache, or ten engaged for 10% of full time.)
For inpatients – the very few with difficult comorbidities, or with MOH requiring detoxication – a recommended minimum is two beds per million population [28].
The gatekeeper role within the model
The model expands the role of primary care, and shifts demand in structured services downwards towards it – a move that is both clinically appropriate and economically efficient [60, 73,74,75,76,77]. This brings into focus the gatekeeper role of primary care as an organizational element of the model [74, 82, 87,88,89]. It is a controversial role.
On the one hand, patients cannot be blamed for seeking direct access to perceived experts, and gatekeeping is not a norm in many countries’ health systems. On the other, ostensibly, gatekeeping guides patients along the “care pathway”, efficiently and in their best interests through the health system according to their needs, not their demands [87]. This is a well-intentioned purpose, although arguably somewhat paternalistic. In truth, gatekeeping is the means of preventing overload in specialist services, which would deny access to some who really need it. This is a more defensible consideration. But gatekeeping is also a means of cost containment, because specialist care is costly (especially when unnecessary). Gatekeeping therefore attracts a hostile perception as a means of rationing [87,88,89].
How essential is it? Health systems in which gatekeeping is the norm will accommodate it easily within headache services; others may not. More important in all cases, both to effectiveness of the model [88] and to the equity of it, is efficiency at the interfaces between levels (“seams in service continuity” [82, 89]), so that no delays are system-created against those who do need specialist care. Efficient interfaces are matters of implementation, best determined in the context of local health services. If the model is implemented well, with all levels in place and adequate provision at each, demand within the levels is likely to be self-regulating, effectively governed by waiting lists.
Flexibility of the model
Two principal factors determine how this model might be implemented in a country (or region or district): the resources allocated to headache services and the structure of the health service accommodating them. The model has considerable flexibility, allowing adaptations in many ways without altering its intrinsic structure (Table 6).
Layered (above) and hub-and-spoke (below) structures. The bi-directional arrows indicate patient flows from lower levels to higher, and clinical and educational supports from higher to lower. Each structure is amenable to top-down or bottom-up organization for integration within existing health services, although bottom-up is more likely in layered structures and top-down in hub-and-spoke. Hybrid structures are possible
Table 7 provides illustrations of how, with these adaptations, it might be implemented in various countries.
Educational implications
Public education has three main purposes. Firstly, it is needed to improve people’s understanding of headache. Secondly, it should explain the use and limitations of OTC medication [79] while warning against self-mismanagement, the attendant dangers of medication overuse and the unsupervised purchase of analgesics from supermarkets and other unlicensed outlets rather than from pharmacists. Thirdly, it should explain how to make appropriate use of headache services, what to expect from them and, in this context, the likely futility of non-adherence [105, 106].
WHO identified professional education as the most pressing requirement in headache services improvement [22]. Separate educational initiatives are required at each level. Pharmacists are not generally expected to diagnose, having neither the training nor the facilities required, but they should have the knowledge to recognise treatment failures and incipient or established medication overuse [79]. Limited knowledge is required at level 1 [28, 64], but better than usually exists. Enhanced but still non-specialist knowledge is needed in level 2 [28]. In both, education should be coupled with availability – and use – of evidence-based guidelines [20, 64, 107, 108] adapted to local resource availability. Specialist expertise and competence are expected in level 3, gained through high-level training and maintained through practice, continuous professional development and participation in professional networks (national or international) allowing exchange of ideas and experience [66]. In the USA, the United Council for Neurologic Subspecialities (UCNS) offers examination-based certification (and recertification) in headache medicine as a subspecialty [109], although there is no requirement for a physician practising as a “headache specialist” to be certified [110]. For some countries, training at this level will require attendance at specialist centres abroad. Several schemes exist for this. The University of Copenhagen and Danish Headache Centre, and Sapienza University in Rome, both offer Master degree courses in headache medicine, open to students from all countries [111, 112]. Training scholarships are offered by the International Headache Society (IHS) [113] and EHF (EHF-SAS [114]).
The major political and logistic implications of these requirements, especially at level 1 in view of the numbers of HCPs who need training, are probably the greatest barrier to nationwide implementation. Far-reaching national training must be part and parcel of effective headache-service reform, and it needs to commence in medical schools. Within the 3-level care system proposed, a training role for each higher level towards the level below can be envisaged (Fig. 2). The entire structure may depend upon these roles being developed.
A comment on service quality
Effective service implementation does not of itself guarantee quality of care. Quality-assurance measures are necessary, as in all fields of medicine.
Standards and indicators exist for headache service quality evaluation (SQE), developed by LTB specifically to support implementation of structured headache services [108]. They are themselves undergoing evaluation at the various levels [66, 115,116,117,118].
A comment on cost
Headache services delivering care equitably and nationwide to large numbers of people will undoubtedly enhance the headache patients’ journey and improve outcomes. They will also consume substantial health-care resources, and require major up-front investment. Cost-effectiveness becomes a key consideration. While preliminary economic analyses are highly favourable [21], there is a cost incurred by doing nothing.
There is promise of even greater savings to offset the cost – if improvements to services recover the lost productivity due to headache, or even a small part of it [11,12,13,14,15,16,17,18,19, 22]. This promise needs testing in formal economic analyses. If it proves to be sound, these savings foregone as a result of doing nothing become the financial penalty of inaction [29].
Concluding remarks
Many problems beset the current compartmentalized division of headache services between primary, secondary and tertiary care. The model described seeks vertical integration. It recognizes that the demand for headache care dictates delivery for the most part in primary care, and that this is a perfectly good way forward in terms of accessibility and effectiveness of care. The model is amenable to horizontal integration with other care services, and capable of adaptation to suit local cultures and health-care systems.
The need for better – and better resourced – headache services exists in all countries, differing only quantitatively. At a time when momentum is again developing for health-service reform diverting resources from secondary to primary care [60, 77], there is opportunity for change. In low- and middle-income countries in particular, the growing shift of emphasis in health policy towards chronic non-communicable diseases [119] creates a fair climate for change.
Political will, needed for change to happen [9, 22, 60], will be driven by economic (cost-effectiveness) analyses. These, so far, have been highly encouraging [21], but more thorough evaluations are needed.
Availability of data and materials
Not applicable.
Abbreviations
- EHF:
-
European Headache Federation
- EU:
-
European Union
- FTE:
-
Full-time equivalent
- GBD:
-
Global burden of disease (study)
- GDP:
-
Gross domestic product
- GP:
-
General practitioner
- HCP:
-
Health-care provider
- ICHD:
-
International classification of headache disorders
- IHS:
-
International Headache Society
- LTB:
-
Lifting The Burden
- MOH:
-
Medication-overuse headache
- OTC:
-
Over-the-counter
- TTH:
-
Tension-type headache
- UdH:
-
Undifferentiated headache
- UK:
-
United Kingdom
- USA:
-
United States of America
- USSR:
-
Union of Soviet Socialist Republics
- WHO:
-
World Health Organization
References
Stovner LJ, Hagen K, Jensen R, Katsarava Z, Lipton R, Scher AI, Steiner TJ, Zwart J-A (2007) The global burden of headache: a documentation of headache prevalence and disability worldwide. Cephalalgia 27(3):193–210. https://doi.org/10.1111/j.1468-2982.2007.01288.x
Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, Shibuya K, Salomon JA, Abdalla S, Aboyans V, Abraham J, Ackerman I, Aggarwal R, Ahn SY, Ali MK, Alvarado M, Anderson HR, Anderson LM, Andrews KG, Atkinson C, Baddour LM, Bahalim AN, Barker-Collo S, Barrero LH, Bartels DH, Basáñez MG, Baxter A, Bell ML, Benjamin EJ, Bennett D, Bernabé E, Bhalla K, Bhandari B, Bikbov B, Bin Abdulhak A et al (2012) Years lived with disability (YLD) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the global burden of disease study 2010. Lancet 380(9859):2163–2196. https://doi.org/10.1016/S0140-6736(12)61729-2
Vos T, Barber RM, Bell B, Bertozzi-Villa A, Biryukov S, Bolliger I, Charlson F, Davis A, Degenhardt L, Dicker D, Duan L, Erskine H, Feigin VL, Ferrari AJ, Fitzmaurice C, Fleming T, Graetz N, Guinovart C, Haagsma J, Hansen GM, Hanson SW, Heuton KR, Higashi H, Kassebaum N, Kyu H, Laurie E, Liang X, Lofgren K, Lozano R, MacIntyre MF, Moradi-Lakeh M, Naghavi M, Nguyen G, Odell S, Ortblad K et al (2015) Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the global burden of disease study 2013. Lancet 386(9995):743–800. https://doi.org/10.1016/S0140-6736(15)60692-4
GBD 2015 Disease and Injury Incidence and Prevalence Collaborators (2016) Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the global burden of disease study 2015. Lancet 388(10053):1545–1602. https://doi.org/10.1016/S0140-6736(16)31678-6
Vos T, Abajobir AA, Abate KH, Abbafati C, Abbas KM, Abd-Allah F, Abdulkader RS, Abdulle AM, Abebo TA, Abera SF, Aboyans V, Abu-Raddad LJ, Ackerman IN, Adamu AA, Adetokunboh O, Afarideh M, Afshin A, Agarwal SK, Aggarwal R, Agrawal A, Agrawal S, Ahmadieh H, Ahmed MB, Aichour MTE, Aichour AN, Aichour I, Aiyar S, Akinyemi RO, Akseer N, Al Lami FH, Alahdab F, Al-Aly Z, Alam K, Alam N, Alam T et al (2017) Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the global burden of disease study 2016. Lancet 390(10100):1211–1259. https://doi.org/10.1016/S0140-6736(17)32154-2
Stovner LJ, Nichols E, Steiner TJ, Abd-Allah F, Abdelalim A, Al-Raddadi RM, Ansha MG, Barac A, Bensenor IM, Doan LP, Edessa D, Endres M, Foreman KJ, Gankpe FG, Gururaj G, Goulart AC, Gupta R, Hankey GJ, Hay SI, Hegazy MI, Hilawe EH, Kasaeian A, Kassa DH, Khalil I, Khang Y-H, Khubchandani J, Kim YJ, Kokubo Y, Mohammed MA, Moradi-Lakeh M, Nguyen HLT, Nirayo YL, Qorbani M, Ranta A, Roba KT et al (2018) Global, regional, and national burden of migraine and tension-type headache, 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet Neurol 17(11):954–976. https://doi.org/10.1016/S1474-4422(18)30322-3
GBD 2017 Disease and Injury Incidence and Prevalence Collaborators (2018) Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet 392:1789–1858
GBD 2019 Diseases and Injuries Collaborators (2020) Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet 396:1204–1222
Steiner TJ, Stovner LJ, Vos T, Jensen R, Katsarava Z (2018) Migraine is first cause of disability in under 50s: will health politicians now take notice? [editorial]. J Headache Pain 19(1):17. https://doi.org/10.1186/s10194-018-0846-2
Steiner TJ, Gururaj G, Andrée C, Katsarava Z, Ayzenberg I, Yu SY, Al Jumah M, Tekle-Haimanot R, Birbeck GL, Herekar A, Linde M, Mbewe E, Manandhar K, Risal A, Jensen R, Queiroz LP, Scher AI, Wang SJ, Stovner LJ (2014) Diagnosis, prevalence estimation and burden measurement in population surveys of headache: presenting the HARDSHIP questionnaire. J Headache Pain 15(1):3. https://doi.org/10.1186/1129-2377-15-3
Hu XH, Markson LE, Lipton RB, Stewart WF, Berger ML (1999) Burden of migraine in the United States: disability and economic costs. Arch Intern Med 159(8):813–818. https://doi.org/10.1001/archinte.159.8.813
Selekler MH, Gökmen G, Steiner TJ (2013) Productivity impact of headache on a heavy-manufacturing workforce in Turkey. J Headache Pain 14(1):88. https://doi.org/10.1186/1129-2377-14-88
Linde M, Gustavsson A, Stovner LJ, Steiner TJ, Barré J, Katsarava Z, Lainez JM, Lampl C, Lantéri-Minet M, Rastenyte D, Ruiz de la Torre E, Tassorelli C, Andrée C (2012) The cost of headache disorders in Europe: the Eurolight project. Eur J Neurol 19(5):703–711. https://doi.org/10.1111/j.1468-1331.2011.03612.x
Raggi A, Leonardi M (2015) Burden and cost of neurological diseases: a European north-south comparison. Acta Neurol Scand 132(1):16–22. https://doi.org/10.1111/ane.12339
Raggi A, Leonardi M (2020) Burden of brain disorders in Europe in 2017 and comparison with other non-communicable disease groups. J Neurol Neurosurg Psychiatry 91(1):104–105. https://doi.org/10.1136/jnnp-2019-320466
Steiner TJ, Rao GN, Kulkarni GB, Gururaj G, Stovner LJ (2016) Headache yesterday in Karnataka state, India: prevalence, impact and cost. J Headache Pain 17(1):74. https://doi.org/10.1186/s10194-016-0669-y
Yu S, Liu R, Zhao G, Yang X, Qiao X, Feng J, Fang Y, Cao X, He M, Steiner T (2012) The prevalence and burden of primary headaches in China: a population-based door-to-door survey. Headache 52(4):582–591. https://doi.org/10.1111/j.1526-4610.2011.02061.x
Ayzenberg I, Katsarava Z, Sborowski A, Chernysh M, Osipova V, Tabeeva G, Steiner TJ (2014) Headache-attributed burden and its impact on productivity and quality of life in Russia: structured healthcare for headache is urgently needed. Eur J Neurol 21(5):758–765. https://doi.org/10.1111/ene.12380
Mbewe E, Zairemthiama P, Paul R, Birbeck GL, Steiner TJ (2015) The burden of primary headache disorders in Zambia: national estimates from a population-based door-to-door survey. J Headache Pain 16(1):36. https://doi.org/10.1186/s10194-015-0513-9
Steiner TJ, Jensen R, Katsarava Z, Linde M, MacGregor EA, Osipova V, Paemeleire K, Olesen J, Peters M, Martelletti P, on behalf of the European Headache Federation and Lifting The Burden: the Global Campaign against Headache (2019) Aids to management of headache disorders in primary care (2nd edition). J Headache Pain 20:57
Linde M, Steiner TJ, Chisholm D (2015) Cost-effectiveness analysis of interventions for migraine in four low- and middle-income countries. J Headache Pain 16(1):15. https://doi.org/10.1186/s10194-015-0496-6
World Health Organization and Lifting The Burden (2011) Atlas of headache disorders and resources in the world 2011. WHO, Geneva Available at: http://www.who.int/mental_health/management/atlas_headache_disorders/en/2011
Katsarava Z, Steiner TJ (2012) Neglected headache: ignorance, arrogance or insouciance? [editorial]. Cephalalgia 32(14):1019–1020. https://doi.org/10.1177/0333102412459478
Steiner TJ (2004) Lifting the burden: the global campaign against headache. Lancet Neurol 3(4):204–205. https://doi.org/10.1016/S1474-4422(04)00703-3
Steiner TJ (2005) Lifting The Burden: the global campaign to reduce the burden of headache worldwide. J Headache Pain 6(5):373–377. https://doi.org/10.1007/s10194-005-0241-7
Lifting The Burden. The global campaign against headache. http://www.l-t-b.org. Accessed 6 June 2021
Antonaci F, Valade D, Lanteri-Minet M, Láinez JM, Jensen J, Steiner TJ (2008) Proposals for the organisation of headache services in Europe. Intern Emerg Med 3:S25–S28
Steiner TJ, Antonaci F, Jensen R, Lainez MJ, Lanteri-Minet M, Valade D (2011) Recommendations for headache service organisation and delivery in Europe. J Headache Pain 12(4):419–426. https://doi.org/10.1007/s10194-011-0320-x
Steiner TJ, Jensen R, Katsarava Z, Uluduz D, Tinelli M, Thomas H, Stovner LJ (2019) The healthcare solution to headache. Ch 15. In: Steiner TJ, Stovner LJ (eds) Societal impact of headache. Burden, costs and response. Springer Nature, Cham, pp 203–224
European Headache Federation. https://ehf-org.org. Accessed 6 June 2021
Hopkins A, Menken M, De Friese GA (1989) A record of patient encounters in neurological practice in the United Kingdom. J Neurol Neurosurg Psychiatry 52(4):436–438. https://doi.org/10.1136/jnnp.52.4.436
Wiles CM, Lindsay M (1996) General practice referrals to a department of neurology. J Roy Coll Physicians 30:426–431
Laughey WF, Holmes WF, MacGregor AE, Sawyer JPC (1999) Headache consultation and referral patterns in one UK general practice. Cephalalgia 19:328–329
Tfelt-Hansen P (2020) Review. Pharmacological strategies to treat attacks of episodic migraine in adults. Exp Opin Pharmacother 22(3):305–316. https://doi.org/10.1080/14656566.2020.1828347
Lipton RB, Scher AI, Steiner TJ, Kolodner K, Liberman J, Stewart WF (2003) Patterns of health care utilization for migraine in England and in the United States. Neurology 60(3):441–448. https://doi.org/10.1212/WNL.60.3.441
Mehuys E, Paemeleire K, Van Hees T, Christiaens T, Van Bortel LM, Van Tongelen I, De Bolle L, Remona J-P, Boussery K (2012) Self-medication of regular headache: a community pharmacy-based survey. Eur J Neurol 19(8):1093–1099. https://doi.org/10.1111/j.1468-1331.2012.03681.x
Edmeads J (2006) Understanding the needs of migraine patients. Drugs 66:1–8
Takeshima T, Ishizaki K, Fukuhara Y, Ijiri T, Kusumi M, Wakutani Y, Mori M, Kawashima M, Kowa H, Adachi Y, Urakami K, Nakashima K (2004) Population-based door-to-door survey of migraine in Japan: the Daisen study. Headache 44(1):8–19. https://doi.org/10.1111/j.1526-4610.2004.04004.x
Radtke A, Neuhauser H (2009) Prevalence and burden of headache and migraine in Germany. Headache 49(1):79–89. https://doi.org/10.1111/j.1526-4610.2008.01263.x
Katsarava Z, Mania M, Lampl C, Herberhold J, Steiner TJ (2018) Poor medical care for people with migraine in Europe – evidence from the Eurolight study. J Headache Pain 19(1):10. https://doi.org/10.1186/s10194-018-0839-1
Ayzenberg I, Katsarava Z, Sborowski A, Obermann M, Chernysh M, Osipova V, Tabeeva G, Steiner TJ (2015) Headache yesterday in Russia: its prevalence and impact, and their application in estimating the national burden attributable to headache disorders. J Headache Pain 16(1):7. https://doi.org/10.1186/1129-2377-16-7
Manandhar K, Risal A, Linde M, Steiner TJ (2018) Health-care utilization for headache disorders in Nepal: a population-based door-to-door survey. J Headache Pain 19(1):116. https://doi.org/10.1186/s10194-018-0942-3
Wang SJ, Fuh JL, Young YH, Lu SR, Shia BC (2001) Frequency and predictors of physician consultations for headache. Cephalalgia 21(1):25–30. https://doi.org/10.1046/j.1468-2982.2001.00138.x
Lampl C, Buzath A, Baumhackl U, Klingler D (2003) One-year prevalence of migraine in Austria: a nation-wide survey. Cephalalgia 23(4):280–286. https://doi.org/10.1046/j.1468-2982.2003.00509.x
Lipton RB, Scher AI, Kolodner K, Liberman J, Steiner TJ, Stewart WF (2002) Migraine in the United States: epidemiology and patterns of health care use. Neurology 58(6):885–894. https://doi.org/10.1212/WNL.58.6.885
Edmeads J, Findlay H, Tugwell P, Pryse-Phillips W, Nelson RF, Murray TJ (1993) Impact of migraine and tension-type headache on life-style, consulting behaviour, and medication use: a Canadian population survey. Can J Neurol Sci 20(2):131–137. https://doi.org/10.1017/S0317167100047697
Liu R, Yu S, He M, Zhao G, Yang X, Qiao X, Feng J, Fang Y, Cao X, Steiner TJ (2013) Health-care utilization for primary headache disorders in China: a population-based door-to-door survey. J Headache Pain 14(1):47. https://doi.org/10.1186/1129-2377-14-47
Steiner T, Lange R, Voelker M (2003) Episodic tension-type headache (ETTH): evidence of prolonged disability from a placebo-controlled comparison of aspirin and paracetamol. Cephalalgia 23:630
Salomon JA, Haagsma JA, Davis A, de Noordhout CM, Polinder S, Havelaar AH, Cassini A, Devleesschauwer B, Kretzschmar M, Speybroeck N, Murray CJ, Vos T (2015) Disability weights for the global burden of disease 2013 study. Lancet Glob Health 3(11):e712–e723. https://doi.org/10.1016/S2214-109X(15)00069-8
World Bank. https://data.worldbank.org/indicator/SP.POP.1564.TO.ZS. Accessed 6 June 2021
World Bank. https://data.worldbank.org/indicator/SP.POP.0014.TO.ZS. Accessed 6 June 2021
Lipton RB, Diamond S, Reed M, Diamond ML, Stewart WF (2001) Migraine diagnosis and treatment: results from the American migraine study II. Headache 41(7):638–645. https://doi.org/10.1046/j.1526-4610.2001.041007638.x
Westergaard ML, Hansen EH, Glumer C, Olesen J, Jensen RH (2014) Definitions of medication-overuse headache in population-based studies and their implications on prevalence estimates: a systematic review. Cephalalgia 34(6):409–425. https://doi.org/10.1177/0333102413512033
Togha M, Nadjafi-Semnani F, Martami F, Mohammadshirazi Z, Vahidpour N, Akbari-sari A, Daroudi R (2020) Economic burden of medication-overuse headache in Iran: direct and indirect costs. Neurol Sci 42(5):1869–1877. https://doi.org/10.1007/s10072-020-04716-8
Lauwerier E, Paemeleire K, Van Damme S, Goubert L, Crombez G (2011) Medication use in patients with migraine and medication-overuse headache: the role of problem-solving and attitudes about pain medication. Pain 152(6):1334–1339. https://doi.org/10.1016/j.pain.2011.02.014
Kyu HH, Pinho C, Wagner JA, Brown JC, Bertozzi-Villa A, Charlson FJ, Coffeng LE, Dandona L, Erskine HE, Ferrari AJ, Fitzmaurice C, Fleming TD, Forouzanfar MH, Graetz N, Guinovart C, Haagsma J, Higashi H, Kassebaum NJ, Larson HJ, Lim SS, Mokdad AH, Moradi-Lakeh M, Odell SV, Roth GA, Serina PT, Stanaway JD, Misganaw A, Whiteford HA, Wolock TM, Wulf Hanson S, Abd-Allah F, Abera SF, Abu-Raddad LJ, AlBuhairan FS, Amare AT et al (2016) Global and national burden of diseases and injuries among children and adolescents between 1990 and 2013: findings from the global burden of disease 2013 study. JAMA Pediatr 170(3):267–287. https://doi.org/10.1001/jamapediatrics.2015.4276
Wöber C, Wöber-Bingöl C, Uluduz D, Aslan TS, Uygunoglu U, Tüfekçi A, Alp SI, Duman T, Sürgün F, Emir GK, Demir CF, Balgetir F, Özdemir YB, Auer T, Siva A, Steiner TJ (2018) Undifferentiated headache: broadening the approach to headache in children and adolescents, with supporting evidence from a nationwide school-based cross-sectional survey in Turkey. J Headache Pain 19(1):18. https://doi.org/10.1186/s10194-018-0847-1
Lyngberg AC, Rasmussen BK, Jørgensen T, Jensen R (2005) Secular changes in health care utilization and work absence for migraine and tension-type headache: a population based study. Eur J Epidemiol 20(12):1007–1014. https://doi.org/10.1007/s10654-005-3778-5
American Association for the Study of Headache, International Headache Society (1998) Consensus statement on improving migraine management. Headache 38(10):736. https://doi.org/10.1046/j.1526-4610.1998.t01-1-3810736.x
World Health Assembly (2020) Synergies in addressing the burden of epilepsy and other neurological disorders. WHA73_5_en WHO 2020
Davies PTG, Lane RJM, Astbury T, Fontebasso M, Murphy J, Matharu M (2019) The long and winding road: the journey taken by headache sufferers in search of help. Prim Health Care Res Dev 20:e4. https://doi.org/10.1017/S1463423618000324
Doretti A, Shestaritc I, Ungaro D, Lee J-I, Lymperopoulos L, Kokoti L, Guglielmetti M, Mitsikostas DD, Lampl C, on behalf of the School of Advanced Studies of the European Headache Federation (EHF-SAS) (2019) Headaches in the emergency department –a survey of patients’ characteristics, facts and needs. J Headache Pain 20:100
Southwell J, Afridi SK (2021) The burden of migraine on acute and emergency services in a London teaching hospital. Cephalalgia 18:333102420981734. https://doi.org/10.1177/0333102420981734 (online ahead of print)
Braschinsky M, Haldre S, Kals M, Iofik A, Kivisild A, Korjas J, Koljal S, Katsarava Z, Steiner TJ (2016) Structured education can improve primary-care management of headache: the first empirical evidence, from a controlled interventional study. J Headache Pain 17(1):24. https://doi.org/10.1186/s10194-016-0613-1
Constantinidis T, Arvaniti A, Fakas N, Rudolf J, Kouremenos E, Giannouli E, Mitsikostas DD, on behalf of the Hellenic Headache Society (2021) A population-based survey for disabling headaches in Greece: prevalence, burden and treatment preferences. Cephalalgia 41(7):810–820. https://doi.org/10.1177/0333102421989630
Steiner TJ, Göbel H, Jensen R, Lampl C, Paemeleire K, Linde M, Braschinsky M, Mitsikostas D, Gil-Gouveia R, Katsarava Z, on behalf of the European Headache Federation and Lifting The Burden: the Global Campaign against Headache (2019) Headache service quality: the role of specialized headache centres within structured headache services, and suggested standards and criteria as centres of excellence. J Headache Pain 20:24
World Bank (2020) World bank country and lending groups – country classification. At: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups
Andrée C, Stovner LJ, Steiner TJ, Barré J, Katsarava Z, Lainez JM, Lair M-L, Lanteri-Minet M, Mick G, Rastenyte D, Ruiz de la Torre E, Tassorelli C, Vriezen P, Lampl C (2011) The Eurolight project: the impact of primary headache disorders in Europe. Description of methods. J Headache Pain 12(5):541–549. https://doi.org/10.1007/s10194-011-0356-y
Steiner TJ, Stovner LJ, Katsarava Z, Lainez JM, Lampl C, Lantéri-Minet M, Rastenyte D, Ruiz de la Torre E, Tassorelli C, Barré J, Andrée C (2014) The impact of headache in Europe: principal results of the Eurolight project. J Headache Pain 15(1):31. https://doi.org/10.1186/1129-2377-15-31
Manandhar K, Risal A, Linde M, Steiner TJ (2016) The burden of headache disorders in Nepal: estimates from a population-based survey. J Headache Pain 17:3
Martelletti P, Steiner TJ, Bertolote JM, Dua T, Saraceno B (2007) The definitive position of headache among the major public health challenges. An end to the slippery slope of disregard [editorial]. J Headache Pain 8(3):149–151. https://doi.org/10.1007/s10194-007-0382-y
Steiner TJ, Olesen J (2019) Advocacy for patients with headache. Ch 30. In: Grisold W, Struhal W, Grishold T (eds) Advocacy in neurology. Oxford University Press, Oxford, pp 339–346
World Health Organization International Conference on Primary Health Care (1978) Declaration of Alma-Ata. WHO, Geneva
Tarino E, Webster EG (1995) Primary health care concepts and challenges in a changing world. Alma-Ata revisited. WHO, Geneva
Coulter A (1995) Shifting the balance from secondary to primary care. BMJ 311(7018):1447–1448. https://doi.org/10.1136/bmj.311.7018.1447
Walley J, Lawn JE, Tinker A, de Francisco A, Chopra M, Rudan I, Bhutta ZA, Black RE, the Lancet Alma-Ata Working Group (2008) Primary health care: making Alma-Ata a reality. Lancet 372:1001–1007
World Health Organization and United Nations Children’s Fund (UNICEF) Global Conference on Primary Health Care (2018) Declaration of Astana. From Alma-Ata towards universal health coverage and the sustainable development goals. WHO/UNICEF, Astana
Clarkson J, Dean J, Ward J, Komashie A, Bashford T (2018) A systems approach to healthcare: from thinking to practice. Future Healthcare J 5(3):151–155. https://doi.org/10.7861/futurehosp.5-3-151
Haag G, Diener H-C, May A, Meyer C, Morck H, Straube A, Wessely P, Evers S (2011) Self-medication of migraine and tension-type headache: summary of the evidence-based recommendations of the Deutsche Migräne und Kopfschmerzgesellschaft (DMKG), the Deutsche Gesellschaft für Neurologie (DGN), the Österreichische Kopfschmerzgesellschaft (ÖKSG) and the Schweizerische Kopfwehgesellschaft (SKG). J Headache Pain 12(2):201–217. https://doi.org/10.1007/s10194-010-0266-4
World Health Organization (2000) Headache disorders and public health. Education and management implications. WHO (WHO/MSD/MBD/00.9), Geneva
Headache Classification Committee of the International Headache Society (2018) The international classification of headache disorders, 3rd edition. Cephalalgia 38:1–211
Steiner TJ (2003) Health-care systems for headache: patching the seam between primary and specialist care. J Headache Pain 4(suppl 1):S70–S74
Populationpyramid.net. https://www.populationpyramid.net/brazil/2010. Accessed 6 June 2020
Masruha MR, Souza JA, Barreiros H, Piovesan EJ, Kowacs F, Queiroz LP, Ciciarelli MC, Peres MFP (2007) Distribution of “Brazilian headache specialists”. Analyses of Brazilian Headache Society members. Einstein 5:48–50
Harpole LH, Samsa GP, Jurgelski AE, Shipley JL, Bernstein A, Matchar DB (2003) Headache management program improves outcome for chronic headache. Headache 43(7):715–724. https://doi.org/10.1046/j.1526-4610.2003.03128.x
Diener H, Gaul C, Jensen R, Göbel H, Heinze A, Silberstein S (2011) Integrated headache care. Cephalalgia 31(9):1039–1047. https://doi.org/10.1177/0333102411409075
Ferris TG, Chang Y, Blumenthal D, Pearson SD (2001) Leaving gatekeeping behind – effects of opening access to specialists for adults in a health maintenance organization. NEJM 345(18):1312–1317. https://doi.org/10.1056/NEJMsa010097
Jones R, Lamont T, Haines A (1995) Setting priorities for research and development in the NHS: a case study on the interface between primary and secondary care. BMJ 311(7012):1076–1080. https://doi.org/10.1136/bmj.311.7012.1076
Preston C, Cheater F, Baker R, Hearnshaw H (1999) Left in limbo: patients views on care across the primary/secondary interface. Qual Health Care 8(1):16–21. https://doi.org/10.1136/qshc.8.1.16
Peres MF, Amado DK, Gonçalves AL, Ribeiro R, Pagura JR, Queiroz LP (2011) The need for preventive therapy in primary headaches. Headache Med 2:46–49
Yu S, Zhang M, Zhou J, Liu R, Wan Q, Li Y (2014) Headache care in China. Headache 54(4):601–609. https://doi.org/10.1111/head.12330
Restrepo Miranda D, Ortiz Monsalve L (2017) Aproximaciones a la estimación de la oferta y la demanda de médicos especialistas en Colombia, 2015–2030. Observatorio De Talento Humano En Salud. Retrieved 1 November 2020 from https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/VS/TH/Especialistas-md-oths.pdf
Muñoz Cerón J (2011) A survey about neurology practice in Colombia. Acta Neurol Colomb 28:180–186 Retrieved 1 November 2020 from http://www.scielo.org.co/scielo.php?script=sci_arttext&pid=S0120-87482012000400003
Ministerio de Salud y Seguridad Social (2016) Resolución 0256 de 2016. Boletín Judicial N° 2. Retrieved 1 November 2020 from https://www.minsalud.gov.co/Normatividad_Nuevo/Bolet%C3%ADn%20Jur%C3%ADdico%20No%202%20Febrero%202016.pdf
Giorgadze G, Mania M, Kukava M, Dzagnidze A, Mirvelashvili E, Steiner TJ, Katsarava Z (2018) Implementation of effective, self-sustaining headache services in the Republic of Georgia: evaluation of their impact on headache-related disability and quality of life of people with headache. Cephalalgia 38(4):639–645. https://doi.org/10.1177/0333102417702131
Hellenic Headache Society. http://www.kefalalgia.gr/index.php/el/. Accessed 6 June 2021
Gazzetta Ufficiale della Repubblica Italiana. LEGGE 14 luglio 2020, n. 81. Disposizioni per il riconoscimento della cefalea primaria cronica come malattia sociale. At https://www.gazzettaufficiale.it/eli/id/2020/07/28/20G00100/SG. Accessed 6 June 2021
Risal A, Manandhar K, Steiner TJ, Holen A, Koju R, Linde M (2014) Estimating prevalence and burden of major disorders of the brain in Nepal: cultural, geographic, logistic and philosophical issues of methodology. J Headache Pain 15(1):51. https://doi.org/10.1186/1129-2377-15-51
Federal Office for State Statistics, Government of the Russian Federation (EMISS). Number of doctors of all specialties (individuals) in organizations providing medical services to the population at the end of the reporting year. https://www.fedstat.ru/indicator/31547. Accessed 6 June 2021
Lebedeva ER, Kobzeva NR, Gilev DV, Olesen J (2017) The quality of diagnosis and management of migraine and tension-type headache in three social groups in Russia. Cephalalgia 37(3):225–235. https://doi.org/10.1177/0333102416642603
Osipova VV, Azimova JE, Tabeeva GR, Tarasova SV, Amelin AV, Kutsemelov IB, Moldovanu IV, Odobesku SS, Naumova GI (2012) Diagnosis of headache disorders in Russia and in post-Soviet countries: state of the problem and ways to solve it (in Russian). Ann Clin Exp Neurol 6:16–21
Osipova VV, Filatova EG, Artemenko AR, Lebedeva ER, Azimova YY, Latysheva NV, Sergeev AV, Amelin AV, Koreshkina MI, Skorobogatyh KV, Ekusheva EV, Naprienko MV, Isaguljan YD, Rachin AP, Danilov AB, Kurushina OV, Parfenov VA, Tabeeva GR, Gekht AB, Yahno NN (2017) Diagnosis and treatment of migraine: recommendations of the Russian experts. Zh Nevrol Psikhiatr Im S S Korsakova 117(1. Vyp. 2):28–42. https://doi.org/10.17116/jnevro20171171228-42
Lebedeva ER, Olesen J, Osipova VV, Volkova LI, Tabeeva GR, Steiner TJ (2013) The Yekaterinburg headache initiative: an interventional project, within the global campaign against headache, to reduce the burden of headache in Russia. J Headache Pain 14(1):101. https://doi.org/10.1186/1129-2377-14-101
UK Department of Health (2003) Guidelines for the appointment of general practitioners with special interests in the delivery of clinical services: headaches. Department of Health, London
Hedenrud T, Jonsson P, Linde M (2008) Beliefs about medicines and adherence among Swedish migraineurs. Ann Pharmacother 42(1):39–45. https://doi.org/10.1345/aph.1K354
Mulleners WM, Whitmarsh TE, Steiner TJ (1998) Noncompliance may render migraine prophylaxis useless, but once-daily regimens are better. Cephalalgia 18(1):52–56. https://doi.org/10.1046/j.1468-2982.1998.1801052.x
Braschinsky M, Haldre S, Kals M, Arge M, Saar B, Niibek M, Katsarava Z, Steiner TJ (2018) Structured education to improve primary-care management of headache: how long do the benefits last? A follow-up observational study. Eur J Neurol 25(3):497–502. https://doi.org/10.1111/ene.13524
Peters M, Jenkinson C, Perera S, Loder E, Jensen R, Katsarava Z, Gil Gouveia R, Broner S, Steiner T (2012) Quality in the provision of headache care. 2: defining quality and its indicators. J Headache Pain 13(6):449–457. https://doi.org/10.1007/s10194-012-0465-2
United Council for Neurologic Subspecialities (2020) Headache medicine certification. https://www.ucns.org/Online/Certification/Headache_Cert.aspx
American Headache Society (2020) Tool kit for UCNS headache board certification. https://americanheadachesociety.org/tool-kit-for-ucns-headache-board-certification/
University of Copenhagen (2020) Master of Headache Disorders. https://mhd.ku.dk/
Sapienza Università di Roma (2020) Master in Headache Medicine. https://web.uniroma1.it/masterheadache/
International Headache Society (2020) Grants, awards and training programmes. https://ihs-headache.org/en/resources/grants-awards-and-training-programmes/
European Headache Federation (2020). https://ehf-org.org/educational-activities/. Accessed 6 June 2021
Katsarava Z, Gil Gouveia R, Jensen R, Gaul C, Schramm S, Schoppe A, Steiner TJ (2015) Evaluation of headache service quality indicators: pilot implementation in two specialist-care centres. J Headache Pain 16(1):53. https://doi.org/10.1186/s10194-015-0537-1
Schramm S, Uluduz D, Gil Gouveia R, Jensen R, Siva A, Uygunoglu U, Gvantsa G, Mania M, Braschinsky M, Filatova E, Latysheva N, Osipova V, Skorobogatykh K, Azimova J, Straube A, Emre Eren O, Martelletti P, De Angelis V, Negro A, Linde M, Hagen K, Radojicic A, Zidverc-Trajkovic J, Podgorac A, Paemeleire K, De Pue A, Lampl C, Steiner TJ, Katsarava Z (2016) Headache service quality: evaluation of quality indicators in 14 specialist-care centres. J Headache Pain 17(1):111. https://doi.org/10.1186/s10194-016-0707-9
Pellesi L, Benemei S, Favoni V, Lupi C, Mampreso E, Negro A, Paolucci M, Steiner TJ, Ulivi M, Cevoli S, Guerzoni S (2017) Quality indicators in headache care: an implementation study in six Italian specialist-care centres. J Headache Pain 18(1):55. https://doi.org/10.1186/s10194-017-0762-x
Steiner TJ, Jensen R, Gil-Gouveia R, Katsarava Z (2019) Evaluation: quality in headache services. Ch 16. In: Steiner TJ, Stovner LJ (eds) Societal impact of headache. Burden, costs and response. Springer Nature, Cham, pp 225–236
World Health Organization (2018) Noncommunicable diseases. http://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases
Acknowledgements
Not applicable.
Funding
None.
Author information
Authors and Affiliations
Consortia
Contributions
TJS, RJ, ZK and LJS developed the model from earlier proposals, with contributory input from DU, MLi, JO, KP and MTi, as a product of the Global Campaign against Headache conducted by LTB. All other authors contributed to its refinement. ZK, LJS, DU, LA, MAlJ, AMAlK, MA, MB, SB, JHE, RG-G, JBG-G, LSG, AAH, NKa, NKi, GBK, ERL, MLe, OL, YM, IM, DDM, TM, VO, KP, MFPP, GQ, GNR, AR, ERdlT, DS, MTo, S-YY, MZ, YZZ and JZ-T provided input based on local knowledge and expertise into adaptations of the model for various countries. TJS drafted the manuscript. All authors contributed to manuscript revision and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
TJS, RJ, ZK, LJS and DU are the Directors and Trustees of Lifting The Burden. Otherwise, no author declares a conflict of interest in relation to the content of this manuscript.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Steiner, T.J., Jensen, R., Katsarava, Z. et al. Structured headache services as the solution to the ill-health burden of headache: 1. Rationale and description. J Headache Pain 22, 78 (2021). https://doi.org/10.1186/s10194-021-01265-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s10194-021-01265-z