Abstract
Introduction
Ventilator-associated pneumonia (VAP) is associated with increased medical resource utilization, but few randomized studies have been conducted to evaluate the effect of initial antibiotic therapy. To assess medical resource utilization in patients with VAP, we conducted a pooled analysis of two prospective, randomized, open-label, multicenter, phase III studies, which also showed that doripenem was clinically noninferior to comparators.
Methods
We assessed durations of mechanical ventilation, intensive care unit (ICU) stay, and hospitalization in patients with VAP who received at least 1 dose of doripenem or a comparator in the phase III studies. Comparators were piperacillin/tazobactam (study 1) and imipenem (study 2). We analyzed between-group differences in medical resource utilization endpoints by comparison of Kaplan-Meier curves with generalized Wilcoxon test and in microbiologic eradication rates by two-sided Fisher's exact test.
Results
625 patients with VAP were evaluated and received at least 1 dose of doripenem (n = 312) or a comparator (n = 313). Median durations of mechanical ventilation (7 versus 10 days; P = 0.008) and hospitalization (22 versus 26 days; P = 0.010) were shorter for doripenem than comparators; corresponding ICU stays were 12 and 13 days (P = 0.065). All-cause, overall mortality rates were similar (51/312 [16%] versus 47/313 [15%]; P = 0.648). MIC90 values against Pseudomonas aeruginosa for doripenem versus imipenem were 4 versus 16 μg/mL in study 2. P. aeruginosa was eradicated from 16/24 (67%) doripenem recipients and 10/24 (42%) comparator recipients (P = 0.147). In patients with P. aeruginosa at baseline, median durations of mechanical ventilation (7 versus 13 days; P = 0.031) and ICU stay (13 versus 21 days; P = 0.027) were shorter for doripenem; corresponding hospital stays were 24 and 35 days (P = 0.129).
Conclusions
Doripenem was associated with lower medical resource utilization than comparators. Differences in antipseudomonal activity may have contributed to these findings.
Trial registration
ClinicalTrials.gov number NCT00211003 (study 1) and NCT00211016 (study 2).
Similar content being viewed by others
Introduction
Ventilator-associated pneumonia (VAP) imposes a burden on medical resources, with attributable hospital costs ranging from $10,000 to $12,000 per episode [1–3]. Length of stay (LOS) is an important component of hospital costs. VAP adds five days to the duration of mechanical ventilation [1], four to six days to LOS in the ICU [2, 4], and seven days to overall duration of hospitalization [1]. LOS is even longer in patients with VAP due to microorganisms that are more virulent, such as Pseudomonas aeruginosa[4–6], or that are resistant to imipenem [7] or multiple drugs [8, 9].
Appropriate initial antibiotic therapy is vital because delayed treatment is associated with increased risk of mortality [4, 10–15]. The choice of therapy depends on the presence of risk factors for multidrug-resistant pathogens and time of VAP onset. Patients with risk factors or late-onset VAP are at increased risk of infection due to P. aeruginosa and are therefore candidates for an antipseudomonal carbapenem [16].
Doripenem is a broad-spectrum carbapenem with activity against P. aeruginosa[17]. In phase III studies, doripenem was clinically noninferior compared with piperacillin/tazobactam in patients with nosocomial pneumonia (study 1) [18] and with imipenem in patients with VAP (study 2) [19]. Additionally, doripenem was associated with shorter durations of mechanical ventilation and hospitalization than was imipenem in study 2; between-group differences in ICU LOS were not significant [20].
Few randomized studies have been conducted to prospectively evaluate the effect of initial antibiotic therapy on medical resource utilization, such as duration of mechanical ventilation, ICU LOS, and hospital LOS. To compare medical resource utilization for doripenem with that for comparators, we conducted a pooled analysis of studies 1 [18] and 2 [19]. Considering the added burden of P. aeruginosa on resource utilization [4–6], we also evaluated between-group differences in microbiologic outcome and medical resource utilization in patients with P. aeruginosa at baseline.
Materials and methods
Data for this pooled analysis were obtained from two prospective, randomized, open-label, multicenter, phase III studies, which were conducted between June 2004 and October 2006 to evaluate whether doripenem was noninferior to comparator drugs. Study 1 was conducted at 24 centers in North America, 18 in South America, and 26 in Europe; study 2 was conducted at 37 centers in North America, 33 in Western Europe, 11 in Australia, and 3 in other parts of the world. Study designs have been previously reported [18–20] and were similar, unless otherwise indicated. Adults were eligible for study 1 if they had clinical and radiologic criteria for nosocomial pneumonia and early-onset VAP, defined as less than five days of mechanical ventilation and a Luna Clinical Pulmonary Infection Score of 5 or more [21]; the pooled analysis included only the subset with VAP. Adults were eligible for study 2 if they had VAP as previously defined. Study protocols and informed consent forms were reviewed and approved by an institutional review board or ethics committee at each study center. All patients or their legally appointed representatives provided written informed consent.
Eligible patients were stratified by non-VAP and early VAP in study 1, early and late VAP in study 2 (onset <5 versus ≥5 days), geographic region, and Acute Physiology and Chronic Health Evaluation (APACHE) II scores (≤15 versus >15). After stratification, patients were randomly assigned to receive doripenem 500 mg every eight hours or a comparator, each intravenously. Doripenem was infused over one hour in study 1 and over four hours in study 2. In study 1, the comparator was piperacillin/tazobactam 4.5 g every six hours infused over 30 minutes; patients who were clinically improved after at least 72 hours of intravenous therapy could be switched to oral levofloxacin 750 mg daily. In study 2, the comparator was imipenem 500 mg every six hours infused over 30 minutes or 1000 mg every eight hours infused over one hour. Both studies allowed adjunctive therapy with vancomycin for suspected methicillin-resistant Staphylococcus aureus (MRSA) or an aminoglycoside for suspected P. aeruginosa. All antibiotic dosages were adjusted for renal function; antibiotic concentrations were not collected.
Endpoints were prospectively defined in the phase III study protocols. Medical resource utilization, which was retrospectively analyzed from prospectively collected data in the pooled analysis, included durations of mechanical ventilation, ICU stay, and hospitalization. Duration of mechanical ventilation was defined as stop date - maximum (start date or randomization date) + 1. If the stop date was not available, the minimum of the following was used for censoring: death, ICU discharge, hospital discharge, or late follow-up, which occurred 28 to 35 days after the end of intravenous therapy. Duration of ICU stay was defined as ICU discharge date - maximum (ICU admit date or randomization date) + 1. Nine patients were excluded from ICU analysis because they had valid ICU admittance dates but no valid ICU discharge dates and had hospital discharge dates (doripenem, 3; comparator, 6). Duration of hospitalization was defined as (discharge date or death date) - randomization date + 1. If discharge date was not available, patients were censored at late follow up. In addition, all-cause overall mortality and, in patients with P. aeruginosa at baseline, minimal inhibitory concentrations (MIC), eradication rate, and resource utilization were evaluated.
Statistical analyses
Medical resource utilization endpoints were analyzed in all patients who received at least one dose of study drug, defined as the intent-to-treat (ITT) population, and who met the clinical definition of VAP (clinical modified ITT) [19]. Microbiologic endpoints were analyzed in patients from whom P. aeruginosa alone or with other microorganisms had been isolated at baseline from the lower respiratory tract.
Between-group differences in medical resource utilization endpoints were analyzed by comparison of Kaplan-Meier curves with Gehan's generalization of the Wilcoxon test [22], whose weighting scheme reduces the relative contribution of patients with prolonged LOS due to other (non-VAP) conditions by placing more weight on early versus later discharges. Between-group differences in microbiologic eradication rates were analyzed by two-sided Fisher's exact test and in LOS by generalized Wilcoxon test.
Effect of covariates on outcome variables, as well as treatment effect after controlling for important covariates, was examined with Cox proportional hazards regression model. Variables were selected by the best-subsets model-selection method, where the smallest model with statistically significant variables was included; the P value for inclusion in the model was less than 0.05. In addition, baseline microbiology of P. aeruginosa or MRSA was included as a clinically important variable. Assumption of proportional hazards was tested in each case by examining the effect-by-time interaction effect jointly for all covariates, and individually for each covariate entered into the model. The proportional hazards assumption was validated for each model.
Statistical Analysis Software version 9.1.3 (SAS Institute, Inc., Cary, NC, USA) was used for statistical analyses. P values less than 0.05 were considered statistically significant.
Results
Of 979 patients randomized to receive doripenem (n = 489) or a comparator (n = 490) in studies 1 and 2 (Figure 1), 354 were excluded from the pooled analysis because they did not receive the study drug (n = 10) or did not meet clinical diagnostic criteria for VAP (n = 344). Most of these exclusions occurred in patients enrolled in study 1 who had nosocomial pneumonia but not VAP. In the remaining 625 patients, none of the tests for between-group differences in demographics, clinical characteristics, and adjunctive medication use yielded statistically significant results (Table 1). All remaining patients were included in the pooled analysis except four who received comparators and did not have valid medical resource utilization data.
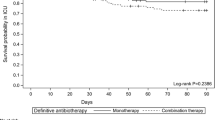
Durations of mechanical ventilation and hospitalization were shorter among patients treated with doripenem than among those treated with a comparator; between-group differences in ICU stay were not statistically significant (Table 2). For example, median duration of mechanical ventilation was 7 days for doripenem and 10 days for comparators; the P value for the Kaplan-Meier curve comparison was 0.008 (Figure 2). Similar trends were seen for the subset of patients who either survived or died seven or more days after stopping mechanical ventilation. All-cause, overall mortality occurred in 51 (16%) of 312 patients in the doripenem group and in 47 (15%) of 313 patients in the comparator group (P = 0.648).
In the Cox proportional hazards model, patients in the doripenem group were 1.3 times more likely to be weaned from mechanical ventilation (P = 0.005) or discharged from the hospital (P = 0.004) than those in the comparator group (Table 3). Hazard ratios for treatment with doripenem versus comparators corresponding to risk of stopping mechanical ventilation (P = 0.006) and hospital discharge (P = 0.004) remained significantly above one after adjusting for other significant covariates, such as presence of P. aeruginosa. The hazard ratio corresponding to risk of ICU discharge was not significantly different from one before (P = 0.079) or after (P = 0.122) adjusting for significant covariates.
In the subset of patients with P. aeruginosa at baseline, this pathogen was eradicated or presumed eradicated from 16 (67%) of 24 patients in the doripenem group and from 10 (42%) of 24 patients in the comparator group (P = 0.147; Table 4). In study 1, MIC50 values were 0.5 μg/mL for doripenem and 4.0 μg/mL for piperacillin/tazobactam, and corresponding MIC90 values were 1 and 128 μg/mL (Figure 3). In study 2, MIC50 values were 0.25 μg/mL for doripenem and 2.0 μg/mL for imipenem, and corresponding MIC90 values were 4 and 16 μg/mL. Median durations of mechanical ventilation (7 versus 13 days; generalized Wilcoxon P = 0.031) and ICU stay (13 versus 21 days; P = 0.027) were shorter for doripenem; between-group differences in hospital stay were not statistically significant.
Discussion
The results of this pooled analysis of two phase III studies indicated that initial use of doripenem in patients with VAP was associated with shorter durations of mechanical ventilation and hospitalization than was use of comparator antibiotics. Between-group differences in hospital LOS remained significant in the subset of patients who survived or died seven or more days after stopping mechanical ventilation, suggesting that the difference was not due to an imbalance in mortality. Treatment group was associated with durations of mechanical ventilation and hospitalization after adjusting for other significant covariates in the regression analysis. Median duration of mechanical ventilation in the comparator group (10 days) was generally consistent with that in previous cohort studies of patients with VAP (10 to 14 days) [1, 23]. Similarly, duration of hospitalization (26 days) was within the range in previous studies (15 to 38 days) [1, 3, 23].
To further elucidate our findings, we evaluated patients with P. aeruginosa at baseline. Microbiologic eradication rates were 67% for doripenem and 42% for comparators; however, the between-group difference was not statistically significant, presumably because of the limited number of patients in this subset. We also found that doripenem had lower MIC values than did imipenem. Comparison of MIC values among different antibiotic classes are not an indication of clinical efficacy; however, free time above MIC in serum (f T>MIC) can be used as a surrogate for comparison. This pharmacokinetic/pharmacodynamic index correlates with clinical efficacy and bactericidal activity and is used to determine antibiotic dosage regimens [24, 25]. Pharmacodynamic modeling reveals that the doripenem dosages would have a 99 to 100% probability of achieving a target f T>MIC for the MIC90 values in study 1 (1 μg/mL) and study 2 (4 μg/mL) [26]. In contrast, the piperacillin/tazobactam dosage would have a very low probability of achieving a target f T>MIC for the MIC90 (128 μg/mL) in study 1 [27].
Finally, we found significant between-group differences in medical resource utilization favoring doripenem in patients with P. aeruginosa at baseline for duration of mechanical ventilation and also for ICU LOS, whereas that for hospital LOS was not significant. As expected, each measure of medical resource utilization was greater for patients in the comparator group with P. aeruginosa at baseline than for those without P. aeruginosa. For example, median duration of mechanical ventilation was 10 days for all patients with VAP and 13 days for the subset with P. aeruginosa at baseline. Vidaur and colleagues [5] reported that, when patients were treated with inappropriate antibiotics, clinical resolution occurred more slowly if VAP was due to P. aeruginosa than due to other pathogens. Interestingly, each measure of medical resource utilization was nearly identical for patients in the doripenem group, regardless of whether P. aeruginosa was present. Therefore, these findings suggest that doripenem may have prevented the increased medical resource utilization associated with P. aeruginosa at baseline reported in other studies [4–6] because of activity against key pathogens. Consideration of the influence of appropriateness of empiric therapy against subsequently identified pathogens was beyond the scope of this economic analysis and merits further evaluation.
The lack of statistically significant between-group difference in one of three measures of medical resource utilization is puzzling, given the relation between the outcome measures. In the subset with P. aeruginosa at baseline, the absolute difference in hospital LOS was nine days. The absolute difference in ICU stay was only one day in all patients and is more difficult to explain. During acute critical illness requiring ICU stay of more than 48 hours, health-related quality of life (HRQOL) declines rapidly. After patients are discharged from the ICU, HRQOL begins to recover and reaches near pre-ICU admission levels by the time of hospital discharge [28]. Therefore, an intervention with a more rapid effect on VAP may allow patients to recover more quickly on the ward and to be discharged from the hospital more quickly. This hypothesis requires further evaluation with repeated assessment of HRQOL throughout hospitalization and after discharge.
Our findings address a gap in the literature regarding the effect of initial antibiotic therapy on medical resource utilization in patients with VAP. The larger, combined sample provided a sufficient number of patients with P. aeruginosa at baseline to show a statistically significant difference between those who received doripenem and those who received a comparator, which was not detected in a previous study containing only a portion of the combined sample [20]. These between-group differences may have clinical implications. Specifically, shortening LOS may decrease the cost of hospitalization as demonstrated in a recent economic analysis of studies 1 and 2 [29]. Using discrete event simulation, Kongnakorn and colleagues [29] estimated that use of doripenem instead of imipenem for treatment of VAP would yield a per-patient saving of approximately $12,260 primarily due to reduced durations of mechanical ventilation, ICU stay, and hospitalization. In addition, shortening LOS may decrease the risk of nosocomial complications, such as exposure to resistant microorganisms and recurrent VAP. Carmeli and colleagues [30] were among the first to report the economic burden of antibiotic resistance in P. aeruginosa. Emergence of resistance during hospitalization was associated with longer hospital LOS and increased risk of secondary bacteremia in their cohort study [30].
Our study had several limitations. First, this was a post hoc analysis, although data were collected prospectively and analysis of medical resource utilization was intended for the individual studies. Second, both study designs were open label, which may have affected medical resource utilization; however, bias should be minimal because the decision of whether to discharge patients or discontinue mechanical ventilation was likely to be based on overall health and predefined institutional procedures rather than treatment assignment, and the number of investigators was large.
Third, the studies were not identical, but they were similar except for the following. Study 1 excluded patients with late-onset VAP; study 2 included patients with early- and late-onset VAP. Study 1 (n = 123) had fewer patients than study 2 (n = 501). Doripenem was infused over one hour in study 1 and four hours in study 2. Comparators were piperacillin/tazobactam in study 1 and imipenem in study 2. Fourth, excluding patients without VAP from study 1 may have partially offset the benefits of randomization in that study; however, all patients in the clinically modified ITT population were included from study 2, which was larger than study 1.
Fifth, not all LOS was attributable to VAP. Patients could have been admitted for other reasons and subsequently acquired VAP. Furthermore, patients with VAP are critically ill and have other comorbidities that contribute to LOS. Additionally, we did not capture data needed to eliminate the possibility that social circumstances or other factors led to earlier discharge of patients who received doripenem, but randomization should have offset any between-group differences. Also, we used a statistical test that places more weight on early discharges than on late discharges and did not consider ICU readmissions. Sixth, the analyses do not prove a cause-and-effect relation between doripenem and shorter LOS, but statistical models were used to address covariates likely to influence treatment and outcome.
Conclusions
This pooled analysis of two prospectively randomized phase III studies suggests that doripenem use for the treatment of VAP was associated with shorter durations of mechanical ventilation and hospitalization. Differences in antipseudomonal activity may have contributed to these findings. Our economic findings, combined with previous clinical findings, suggest that doripenem may be considered an alternative for empirical treatment of VAP, especially when P. aeruginosa is suspected or prevalent. More studies are needed to confirm these preliminary findings and to define the clinical and economic value of doripenem in patients with VAP.
Key messages
-
Initial doripenem use in patients with VAP was associated with statistically significant shorter durations of mechanical ventilation (median, 7 versus 10 days) and hospitalization (median, 22 versus 26 days) than was use of comparator antibiotics (piperacillin/tazobactam or imipenem) in a pooled analysis of two phase III studies.
-
Initial doripenem use was also associated with statistically significant shorter durations of mechanical ventilation (median, 7 versus 13 days) and ICU stay (median, 13 versus 21 days) in the subset with P. aeruginosa at baseline.
-
The economic findings from this paper, combined with previous clinical findings, suggest that doripenem may be considered an alternative for empirical treatment of VAP, especially when P. aeruginosa is suspected or prevalent.
Abbreviations
- APACHE:
-
Acute Physiology and Chronic Health Evaluation
- HRQOL:
-
health-related quality of life
- ITT:
-
intent to treat
- LOS:
-
length of stay
- MIC:
-
minimal inhibitory concentration
- MRSA:
-
methicillin-resistant Staphylococcus aureus
- VAP:
-
ventilator-associated pneumonia.
References
Hugonnet S, Eggimann P, Borst F, Maricot P, Chevrolet JC, Pittet D: Impact of ventilator-associated pneumonia on resource utilization and patient outcome. Infect Control Hosp Epidemiol 2004, 25: 1090-1096. 10.1086/502349
Safdar N, Dezfulian C, Collard HR, Saint S: Clinical and economic consequences of ventilator-associated pneumonia: a systematic review. Crit Care Med 2005, 33: 2184-2193. 10.1097/01.CCM.0000181731.53912.D9
Warren DK, Shukla SJ, Olsen MA, Kollef MH, Hollenbeak CS, Cox MJ, Cohen MM, Fraser VJ: Outcome and attributable cost of ventilator-associated pneumonia among intensive care unit patients in a suburban medical center. Crit Care Med 2003, 31: 1312-1317. 10.1097/01.CCM.0000063087.93157.06
Heyland DK, Cook DJ, Griffith L, Keenan SP, Brun-Buisson C: The attributable morbidity and mortality of ventilator-associated pneumonia in the critically ill patient. The Canadian Critical Trials Group. Am J Respir Crit Care Med 1999, 159: 1249-1256.
Vidaur L, Planas K, Sierra R, Dimopoulos G, Ramirez A, Lisboa T, Rello J: Ventilator-associated pneumonia: impact of organisms on clinical resolution and medical resources utilization. Chest 2008, 133: 625-632. 10.1378/chest.07-2020
Bou R, Lorente L, Aguilar A, Perpinan J, Ramos P, Peris M, Gonzalez D: Hospital economic impact of an outbreak of Pseudomonas aeruginosa infections. J Hosp Infect 2009, 71: 138-142. 10.1016/j.jhin.2008.07.018
Lautenbach E, Weiner MG, Nachamkin I, Bilker WB, Sheridan A, Fishman NO: Imipenem resistance among Pseudomonas aeruginosa isolates: risk factors for infection and impact of resistance on clinical and economic outcomes. Infect Control Hosp Epidemiol 2006, 27: 893-900. 10.1086/507274
Giske CG, Monnet DL, Cars O, Carmeli Y: Clinical and economic impact of common multidrug-resistant gram-negative bacilli. Antimicrob Agents Chemother 2008, 52: 813-821. 10.1128/AAC.01169-07
Shorr AF: Review of studies of the impact on Gram-negative bacterial resistance on outcomes in the intensive care unit. Crit Care Med 2009, 37: 1463-1469. 10.1097/CCM.0b013e31819ced02
Alvarez-Lerma F: Modification of empiric antibiotic treatment in patients with pneumonia acquired in the intensive care unit. ICU-Acquired Pneumonia Study Group. Intensive Care Med 1996, 22: 387-394. 10.1007/BF01712153
Iregui M, Ward S, Sherman G, Fraser VJ, Kollef MH: Clinical importance of delays in the initiation of appropriate antibiotic treatment for ventilator-associated pneumonia. Chest 2002, 122: 262-268. 10.1378/chest.122.1.262
Kollef MH, Ward S: The influence of mini-BAL cultures on patient outcomes: implications for the antibiotic management of ventilator-associated pneumonia. Chest 1998, 113: 412-420. 10.1378/chest.113.2.412
Luna CM, Vujacich P, Niederman MS, Vay C, Gherardi C, Matera J, Jolly EC: Impact of BAL data on the therapy and outcome of ventilator-associated pneumonia. Chest 1997, 111: 676-685. 10.1378/chest.111.3.676
Rello J, Gallego M, Mariscal D, Sonora R, Valles J: The value of routine microbial investigation in ventilator-associated pneumonia. Am J Respir Crit Care Med 1997, 156: 196-200.
Luna CM, Aruj P, Niederman MS, Garzon J, Violi D, Prignoni A, Rios F, Baquero S, Gando S: Appropriateness and delay to initiate therapy in ventilator-associated pneumonia. Eur Respir J 2006, 27: 158-164. 10.1183/09031936.06.00049105
Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia Am J Respir Crit Care Med 2005, 171: 388-416. 10.1164/rccm.200405-644ST
Jones RN, Sader HS, Fritsche TR: Comparative activity of doripenem and three other carbapenems tested against Gram-negative bacilli with various beta-lactamase resistance mechanisms. Diagn Microbiol Infect Dis 2005, 52: 71-74. 10.1016/j.diagmicrobio.2004.12.008
Réa-Neto A, Niederman M, Lobo SM, Schroeder E, Lee M, Kaniga K, Ketter N, Prokocimer P, Friedland I: Efficacy and safety of doripenem versus piperacillin/tazobactam in nosocomial pneumonia: a randomized, open-label, multicenter study. Curr Med Res Opin 2008, 24: 2113-2126. 10.1185/03007990802179255
Chastre J, Wunderink R, Prokocimer P, Lee M, Kaniga K, Friedland I: Efficacy and safety of intravenous infusion of doripenem versus imipenem in ventilator-associated pneumonia: a multicenter, randomized study. Crit Care Med 2008, 36: 1089-1096. 10.1097/CCM.0b013e3181691b99
Merchant S, Gast C, Nathwani D, Lee M, Quintana A, Ketter N, Friedland I, Ingham M: Hospital resource utilization with doripenem versus imipenem in the treatment of ventilator-associated pneumonia. Clin Ther 2008, 30: 717-733. 10.1016/j.clinthera.2008.04.001
Luna CM, Blanzaco D, Niederman MS, Matarucco W, Baredes NC, Desmery P, Palizas F, Menga G, Rios F, Apezteguia C: Resolution of ventilator-associated pneumonia: prospective evaluation of the clinical pulmonary infection score as an early clinical predictor of outcome. Crit Care Med 2003, 31: 676-682. 10.1097/01.CCM.0000055380.86458.1E
Gehan EA: A generalized two-sample Wilcoxon test for doubly censored data. Biometrika 1965, 52: 650-653.
Rello J, Ollendorf DA, Oster G, Vera-Llonch M, Bellm L, Redman R, Kollef MH: Epidemiology and outcomes of ventilator-associated pneumonia in a large US database. Chest 2002, 122: 2115-2121. 10.1378/chest.122.6.2115
Craig WA: Interrelationship between pharmacokinetics and pharmacodynamics in determining dosage regimens for broad-spectrum cephalosporins. Diagn Microbiol Infect Dis 1995, 22: 89-96. 10.1016/0732-8893(95)00053-D
Vogelman B, Gudmundsson S, Leggett J, Turnidge J, Ebert S, Craig WA: Correlation of antimicrobial pharmacokinetic parameters with therapeutic efficacy in an animal model. J Infect Dis 1988, 158: 831-847.
Bhavnani SM, Hammel JP, Cirincione BB, Wikler MA, Ambrose PG: Use of pharmacokinetic-pharmacodynamic target attainment analyses to support phase 2 and 3 dosing strategies for doripenem. Antimicrob Agents Chemother 2005, 49: 3944-3947. 10.1128/AAC.49.9.3944-3947.2005
Shea KM, Cheatham SC, Smith DW, Wack MF, Sowinski KM, Kays MB: Comparative pharmacodynamics of intermittent and prolonged infusions of piperacillin/tazobactam using Monte Carlo simulations and steady-state pharmacokinetic data from hospitalized patients. Ann Pharmacother 2009, 43: 1747-1754. 10.1345/aph.1M304
Hofhuis JG, Spronk PE, van Stel HF, Schrijvers GJ, Rommes JH, Bakker J: The impact of critical illness on perceived health-related quality of life during ICU treatment, hospital stay, and after hospital discharge: a long-term follow-up study. Chest 2008, 133: 377-385. 10.1378/chest.07-1217
Kongnakorn T, Mwamburi M, Merchant S, Akhras K, Caro JJ, Nathwani D: Economic evaluation of doripenem for the treatment of nosocomial pneumonia in the US: discrete event simulation. Curr Med Res Opin 2010, 26: 17-24. 10.1185/03007990903358980
Carmeli Y, Troillet N, Karchmer AW, Samore MH: Health and economic outcomes of antibiotic resistance in Pseudomonas aeruginosa . Arch Intern Med 1999, 159: 1127-1132. 10.1001/archinte.159.10.1127
Acknowledgements
Funding/support. This study, including the statistical analysis and manuscript preparation, was supported by a research grant from Johnson and Johnson Pharmaceutical Services, LLC.
Role of the sponsor. SM, AQ, and NK of Johnson and Johnson met authorship criteria by participating in the study design, analysis of results, interpretation of findings, and drafting of the paper.
Independent statistical analysis. The accuracy of the data analysis was independently verified by William Shannon, PhD, Associate Professor of Biostatistics in Medicine, Department of Medicine, Washington University School of Medicine wshannon@wustl.edu. Dr Shannon received the raw database and statistical analysis plan, reviewed and replicated all analyses, and discovered no discrepancies. All reported analyses are those performed by Dr Shannon. Dr Shannon received compensation from the sponsor.
Additional contributions. We thank Cindy W. Hamilton, PharmD, ELS (Hamilton House, Virginia Beach, Virginia) for assisting with manuscript preparation. Hamilton House received compensation from Johnson and Johnson Pharmaceutical Services, LLC for its contributions.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
This study, including statistical analysis and manuscript preparation, was supported by a grant from Johnson and Johnson Pharmaceutical Services, LLC. MK reported receiving a consulting fee from Kimberly Clark and lecture fees and grant support from Bard, Elan, Merck, Ortho-McNeil (lecture fees only), and Pfizer. DN reported receiving speaking fees and honoraria for meetings and advisory boards supported by Astellas, Wyeth, Bayer, Pfizer, and Johnson and Johnson (J&J). MK and DN have not received any fees for involvement in this study or manuscript. SM, AQ, and NK are employed by Johnson and Johnson. CG is employed by Axio, which received payment from Johnson and Johnson for its services.
Authors' contributions
MK had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. MK contributed to study concept and design, to analysis and interpretation of data and to drafting of the manuscript and critical revision for important intellectual content. DN contributed to study concept and design, to analysis and interpretation of data and to drafting of the manuscript and critical revision for important intellectual content. SM contributed to study concept and design, to analysis and interpretation of data and to drafting of the manuscript and critical revision for important intellectual content. CG contributed to study concept and design, to analysis and interpretation of data, to drafting of the manuscript and critical revision for important intellectual content and to statistical analysis. AQ contributed to study concept and design, to analysis and interpretation of data and to drafting of the manuscript and critical revision for important intellectual content. NK contributed to study concept and design, to analysis and interpretation of data and to drafting of the manuscript and critical revision for important intellectual content.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Kollef, M.H., Nathwani, D., Merchant, S. et al. Medical resource utilization among patients with ventilator-associated pneumonia: pooled analysis of randomized studies of doripenem versus comparators. Crit Care 14, R84 (2010). https://doi.org/10.1186/cc9012
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/cc9012