Abstract
Use of helium-oxygen (He/O2) mixtures in critically ill patients is supported by a reliable and well understood theoretical rationale and by numerous experimental observations. Breathing He/O2 can benefit critically ill patients with severe respiratory compromise mainly by reducing airway resistance in obstructive syndromes such as acute asthma and decompensated chronic obstructive pulmonary disease. However, the benefit from He/O2 in terms of respiratory mechanics diminishes rapidly with increasing oxygen concentration in the gaseous mixture. Safe use of He/O2 in the intensive care unit requires specific equipment and supervision by adequately experienced personnel. The available clinical data on inhaled He/O2 mixtures are insufficient to prove that this therapy has benefit with respect to outcome variables. For these reasons, He/O2 is not currently a standard of care in critically ill patients with acute obstructive syndromes, apart from in some, well defined situations. Its role in critically ill patients must be more precisely defined if we are to identify those patients who could benefit from this therapeutic approach.
Similar content being viewed by others
Introduction
Use of helium-oxygen (He/O2) mixtures in clinical practice is not a new concept. Before the advent of bronchodilatators, Barach [1, 2], in the early 1930s, advocated use of helium because of its respiratory benefits, particularly with respect to obstructive syndromes. Following a brief primer of the basic theory supporting use of He/O2 mixtures, this short review details its potential indications in critically ill patients, technical aspects, and costs associated with its administration.
Theoretical considerations
Helium is an odourless, colourless and biologically inert gas. Clinically, it is only its physical properties that are interesting and may be exploited. Helium is less dense but more viscous than air, oxygen, or nitrogen. Helium also has a high thermal conductivity [3, 4]. Its physical properties relative to those of air, nitrogen and oxygen are summarized in the Table 1.
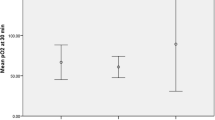
The physical properties of a gaseous mixture containing helium depend on the concentration of helium in the mixture. Because the density of helium is almost an order of magnitude less than that of oxygen or nitrogen, He/O2 mixtures are always less dense than nitrogen-oxygen mixtures (Figure 1). He/O2 mixtures are also more viscous than nitrogen-oxygen mixtures, but this effect is less pronounced than that for density. Similar observations can be made with respect to thermal conductivity.
Density of He/O2 versus nitrogen-oxygen mixture at 20°C and 765 mmHg atmospheric pressure. One can observe that the two densities are quite different and increase progressively with FiO2, especially in the case of helium-oxygen mixtures. FiO2, fractional inspired oxygen; He/O2, helium-oxygen mixture.
Consonant with the physical properties of helium, inhaling He/O2 will influence respiratory mechanics by altering gas convection in the airways. Gas enters the alveoli because of modification to the transpulmonary pressure gradient, which permits gas convection in the airways and renews the alveolar gas. Gas convection is highly dependent on airway resistances. The resistances of the airways mainly result from their anatomical configuration (diameter, number of connections and length), the physical properties of the inhaled gas and the flow rate. Human airways can be compared with pipes in which several types of flow patterns can be distinguished: laminar, turbulent and rough [3–5]. The crossing from one flow type to another is not instantaneous but rather occurs progressively. The flow that occurs between two flow types is referred to as 'transitional' [3, 4]. The flow type can be predicted based on the Reynolds number (R) [3]. This number, without physical dimension, corresponds to the ratio of the inertial forces to the viscous forces, and it is caculated as follows:
Where V is flow (ml/s), ρ is the gas density (g/l), r is the pipe radius (cm), and μ the gas viscosity (micropoises). A Reynolds number under about 2000 suggests a laminar type of flow, and a Reynolds number above 4000 suggests turbulent flow. Under physiological conditions the flow type in the upper airways is not laminar but is at best transitional and may even be turbulent. As the gas approaches the alveoli the flow becomes increasingly laminar because of the decreased gas flow.
The pressure necessary to generate a gas flow in pipes depends on the flow rate and on the flow type. If the flow type is laminar, then the relationship between pressure and flow may be defined as follows:
This is the classic Hagen-Poiseuille law. It shows that the pressure necessary to generate a given gas flow is proportional to the flow (V), the length of the pipe (l) and the gas viscosity (μ), and is inversely proportional to the radius (r) of the pipe to the power of four. Note that the loss of charge is proportional to the viscosity but not the gas density in the case of a laminar type flow [3, 4]. The term 8lμ/πr4 represents the resistance to gas flow for a laminar-type flow. In case of transitional or turbulent flow, the flow resistance becomes dependent on the density of the gas (ρ) [3, 4], as indicated by the following general equation developed by Wood and coworkers [6], which describes the pressure-flow relationship throughout the airway system:
ΔP = Kμ2-aρa-1
In this equation, K is a constant and the value of a varies between 1 and 2 as Reynold's number increases from very low to very high values. This equation allows for continuous modifications to flow type along the tracheobronchial tree [6]. Based on these equations, breathing He/O2 decreases the Reynolds number and favours laminar-type flow. Laminar flow is associated with lower resistance. In the case of turbulent-type flow, the use of He/O2 reduces resistance to flow.
In the clinic, breathing He/O2 can decrease the pulmonary resistance during inspiration and expiration. This decrease reduces the respiratory resistive work of breathing (WOB) and the energy cost of ventilation. Indications thus far identified for use of He/O2 mixtures are obstructive syndromes. Finally, He/O2 mixtures improve gaseous convection [4] in the case of obstructive syndromes, and so they can be used to improve aerosol delivery.
Clinical indications
Upper airway obstruction
In the 1930s, Barach [1, 2] used He/O2 in the context of acute obstruction of the upper airways. For some time thereafter authors advocated use of He/O2 to manage paediatric laryngitis or obstruction of the upper airways by tumours. Some reports showed spectacular clinical improvement in some patients [7–14]. In a randomized, prospective trial conducted in children, Weber and coworkers [15] demonstrated benefit from from use of He/O2 to manage acute laryngitis. In patients with moderate to severe croup, He/O2 administration resulted in improvements in croup score similar to those in patients given racemic adrenaline (epinephrine).
In such situations, if the obstruction of the upper airways is quickly reversible either medically or surgically, then use of He/O2 as a symptomatic treatment is justified; it can be used as a therapeutic bridge until definitive treatment takes effect. At present this is probably one of the best indications for He/O2, with the important caveat that one should be careful not to misinterpret the ensuing improvement as reflecting an improvement in the underlying process. This indication for He/O2 has never undergone rigorous investigation in a large randomized trial because of the considerable heterogeneity in patients and technical problems.
Status asthmaticus
The vast majority of patients with acute asthma are successfully treated with routine therapy based on β2-agonists and corticosteroids. Some patients fail to respond to conventional therapy and may require intubation or even mechanical ventilation, which is associated with increased morbidity under these circumstances. Some case studies have suggested that a small subgroup of patients with status asthmaticus may benefit from breathing He/O2 until definitive therapies take hold [16–20]. Effectively, He/O2 has a potential benefit in reducing airway resistance, and consequently respiratory burden, by reducing dyspnoea and respiratory rate with spontaneous ventilation; in improving aerosol delivery (see below); and in reducing the insufflation pressure and the phenomenon of dynamic hyperinflation during mechanical ventilation.
Ten patients with status asthmaticus and respiratory acidosis or combined respiratory and metabolic acidosis were treated by Shiue and Gluck [21] with He/O2, in addition to usual bronchodilator therapy and corticosteroids. A significant reversal ini acidosis was noted within the first 20 min and no patient required subsequent intubation. The He/O2 treatment was started after the aerosolized and subcutaneous bronchodilators but before intravenous corticosteroids and aminophylline had achieved their peak effects. There were no untoward reactions, and most of the patients sensed an immediate reduction in their dyspnoea with the onset of He/O2 therapy. Shiue and Gluck concluded that He/O2 may be a useful adjunct to the usual medications employed in the treatment of status asthmaticus, and may allow some patients to avoid intubation and mechanical ventilation. In 2003, Sattonnet and coworkers [22] included 203 patients with severe asthmatic crisis in a multicentre, randomized study. They found that early administration of He/O2 in association with inhaled β2-agonist therapy reduced the intubation rate and length of stay in the intensive care unit (ICU). This study has been published only in abstract form.
In 2003, Rodrigo and coworkers [23] conducted a meta-analysis including seven prospective controlled studies: six involving adults and one including children only. This meta-analysis included a total of 392 patients, and the main outcome variable was spirometric measurements (peak expiratory flow rate or forced expiratory volume in 1 s [FEV1]). Those investigators found that use of heliox (He/O2) to treat asthma crises did not improve respiratory function, and the existing evidence does not support administration of He/O2 to patients with moderate-to-severe acute asthma in the emergency department. However, as mentioned by Rodrigo and coworkers, these conclusions are based on between group comparisons and small studies. Moreover, the seven studies were heterogeneous in a number of areas, including technique used to administer helium; concentration of helium administered; severity of illness; dosage of bronchodilator administered; the method used to measure FEV1; and the correction applied to FEV1 to account for the use of He/O2 (without which FEV1 measurement is known to be imprecise). For these reasons, the findings of the meta-analysis should be interpreted with caution.
Kass [24] suggested that use of heliox should be reserved for the unstable asthmatic patient who does not quickly respond to inhaled β2-agonist therapy and who has any of the following characteristics: severe airflow obstruction (peak expiratory flow rate <30% predicted) and an acute exacerbation of symptoms (over a period of under 24 hours but no longer than 72 hours); history of labile asthma and/or previous tracheal intubation for asthma; and failure of a mechanical ventilator to achieve adequate ventilation.
Acute respiratory failure in chronic obstructive pulmonary disease
In the setting of acute respiratory failure, patients with chronic obstructive pulmonary disease (COPD) are at considerable risk for respiratory distress because of the huge ventilatory burden resulting from high respiratory resistance. The increase in respiratory WOB can lead to failure of the respiratory muscles and require management with invasive mechanical ventilation. Once intubated, these patients need prolonged mechanical ventilation.
He/O2, by reducing respiratory resistance, is a potential but controversial therapeutic tool in such patients, and could confer the following benefits. First, He/O2 reduces the burden imposed on respiratory muscles during spontaneous ventilation and can buy time until other treatments exert their beneficial effects. Second, He/O2 improves the efficiency of and optimizes results with noninvasive positive pressure ventilation (NIPPV), and so it reduces the burden imposed on the respiratory muscles; it also improves tolerance to NIPPV by allowing better synchronization to be acheived between patient and ventilator. Achieving an optimal patient-ventilator interaction is probably key to the success of noninvasive ventilation during decompensated COPD. Finally, He/O2 reduces the impact of the dynamic hyperinflation phenomenon by increasing expiratory flow. Dynamic hyperinflation contributes to increased alveolar pressure and results in high levels of intrinsic positive end-expiratory pressure (PEEPi), which also increases the WOB and can have deleterious haemodynamic effects.
In addition to the potential benefits of He/O2 during spontaneous ventilation and NIPPV, its use to wean patients from mechanical ventilation is also an interesting potential application.
Decompensated chronic obstructive pulmonary disease under spontaneous ventilation
Several impressive case reports have been published on the use of heliox in patients with decompensated COPD who are ventilating spontaneously [25, 26], but there is just one reported study on use of He/O2 in such patients [27]. This retrospective study was conducted in 81 patients with decompensated COPD who underwent management in the emergency department; 42 patients received air-oxygen and 39 received He/O2 in the emergency ward and during their hospitalization. The two patient groups had similar clinical and therapeutic characteristics. The intubation and mortality rates were significantly lower in the He/O2 group than in the air-oxygen group (intubation: 50% versus 8%, P = 0.01; mortality: 24% versus 1%, P = 0.01). These spectacular results must be considered with caution because of weak methodology resulting from the retrospective nature of the study.
Decompensated chronic obstructive pulmonary disease under noninvasive positive pressure ventilation
For the past 10 years it has become the standard of care to manage patients with decompensated COPD using NIPPV. Many authors have demonstrated that NIPPV tends to reduce intubation rate, morbidity, mortality and length of stay in the ICU during acute respiratory failure in patients with COPD [28, 29]. As mentioned above, in this setting He/O2 can enhance the benefits of NIPPV.
Jolliet and coworkers [30] were the first to conduct a randomized prospective trial of He/O2 during NIPPV in 20 patients with decompensated COPD. Those investigators found that He/O2 improves respiratory comfort, reduces the sensation of dyspnoea and decreases arterial carbon dixoide tension. Jaber and colleagues [31] conducted a pathophysiological study in 10 COPD patients suffering an exacerbation. They found that He/O2 can reduce the WOB and the pressure-time index in COPD patients receiving NIPPV under pressure support mode.
In a later randomized, prospective, multicentre study, Jolliet and coworkers [32] evaluated the effect of He/O2 on outcomes in patients with decompensated COPD. A total of 123 patients were included in the study and randomly assigned to either an air-oxygen group (n = 64) or a HeO2 group (n = 59). The intubation rate was lower in the He/O2 group than in the air-oxygen group (13% versus 20%), but this difference was not statistically significant. Length of stay in the ICU was similar between the two groups (5.1 ± 4 days in the He/O2 group versus 6.2 ± 5.6 days in the air-oxygen group). The duration of post-ICU hospital stay was shorter in the He/O2 than in the air-oxygen group (13 ± 6 days in the He/O2 group versus 19 ± 12 days in the air-oxygen group; P < 0.002).
The most recent randomized, prospective, multicentre clinical trial is that conducted by Maggiore and coworkers [33]. The aim of this multicentre randomized trial was to determine whether the NIPPV failure rate can be reduced with He/O2 in comparison with air-oxygen in COPD patients suffering an acute exacerbation. The main efficacy criterion was need for endotracheal intubation at 28 days. A total of 204 patients with decompensated COPD were included in the study, but only 195 patients were analyzed on an intention-to-treat basis. The intubation rates were 20.8% in the He/O2 group (n = 96) and 30.3% in the air-oxygen group (n = 99), but the difference was not statistically significant. Differences between groups in duration of NIPPV and death rate were not statistically significant. This study has not yet been published in full.
Interpretation of these two multicentre studies [32, 33] is difficult largely because they are underpowered, but also because it is not possible to achieve blinding in a study of NIPPV combined with He/O2 inhalation because of modification to the patient's voice (squeaky or 'Donald Duck' voice resulting from inhalation of He/O2). It is evident that He/O2 can improve respiratory comfort in the setting of decompensated COPD under NIPPV, and so He/O2 may be used instead of air-oxygen in order to enhance patient comfort during NIPPV.
Chronic obstructive pulmonary disease under mechanical ventilation
PEEPi occurs as a consequence of the dynamic hyperinflation phenomenon. It is frequently observed during mechanical ventilation in COPD patients [34, 35]. He/O2 could be used during mechanical ventilation in COPD patients to decrease levels of PEEPi. Three studies have attested to the efficiency of He/O2 in this setting.
First, in 23 decompensated, sedated and mechanically ventilated COPD patients, Tassaux and coworkers [36] demonstrated that He/O2 significantly reduced trapped volume and PEEPi (trapped volume: 215 ± 125 ml versus 99 ± 15 ml; PEEPi: 9 ± 2.5 cmH2O versus 5 ± 2.7 cmH2O: P < 0.05 for both comparisons). These effects disappeared rapidly when He/O2 was interrupted.
A second, similar study conducted by Gainnier and colleagues [37] corroborated these findings in a similar number of mechanically ventilated COPD patients. In this study the ventilator WOB was also measured, and all of its components were found to decrease with He/O2 use: total WOB decreased from 2.34 ± 1.04 J/l to 1.85 ± 1.01 J/l (P < 0.001), elastic WOB from 1.02 ± 0.61 J/l to 0.87 ± 0.47 J/l (P < 0.01), WOB due to PEEPi from 0.77 ± 0.38 J/l to 0.54 ± 0.38 J/l (P < 0.001), and resistive WOB from 0.55 ± 0.19 J/l to 0.44 ± 0.24 J/l (P < 0.05).
In the third study, Lee and coworkers [38] evaluated 25 consecutive mechanically ventilated patients with COPD and acute respiratory failure who had systolic pressure variations greater than 15 mmHg. Compared with air-oxygen, He/O2 ventilation decreased PEEPi (13 ± 4 cmH2O versus 5 ± 2 cmH2O; P < 0.05), trapped lung volume (362 ± 67 ml versus 174 ± 86 ml; P < 0.05), and respiratory changes in systolic pressure variation (29 ± 5% versus 13 ± 7%; P < 0.05). The authors concluded that He/O2 may be a useful adjunct in patients with severe COPD during acute respiratory failure who exhibit PEEPi-induced haemodynamic changes. Currently, the likelihood of high PEEPi levels are marginal if the recommended ventilatory settings are applied in such patients (low frequency, low tidal volume, and inspiratory:expiratory ratio >1:4). In the case of conventional mechanical ventilation, our policy restricts the use of He/O2 in COPD to just those patients with high levels of PEEPi with haemodynamic or respiratory consequences despite adequate ventilator settings.
During weaning from mechanical ventilation, Diehl and coworkers [39] demonstrated in 13 patients that use of He/O2 reduced the respiratory WOB and PEEPi during the weaning process, especially in patients with the greatest WOB (1.442 ± 0.7 versus 1.133 ± 0.500 J/l; P < 0.05). This reduction was accounted for by a reduction in the resistive component of the WOB. These findings are similar to those reported by Jaber and colleagues [40]. They observed 18 non-COPD patients after extubation and found that He/O2 reduced the transdiaphragmatic pressure-time index and improved respiratory comfort. Those authors concluded that He/O2 could be used during the postextubation period in association with NIPPV, especially if upper obstruction is the main cause of acute respiratory failure, in order to avoid reintubation. More recently, Tassaux and coworkers [41] showed that He/O2 reduces PEEPi, the number of ineffective breaths, the magnitude of inspiratory effort and the WOB in intubated COPD patients. This could be useful during weaning from mechanical ventilation.
Despite all of these findings, the use of He/O2 remains controversial in patients with decompensated COPD because of the low level of evidence supporting its use.
Aerosol delivery
He/O2 has the potential benefit of allowing aerosols to be carried deeper into the distal airways during severe airway obstruction than is possible with air or oxygen. The mechanisms underlying the improved aerosol delivery with He/O2 are as follows [42]: He/O2 allows greater flow through the airways; it ameliorates the reduction in flow speed in the most obstructed regions of the respiratory system; it prevents transition from laminar to turbulent flow, which can affect aerosol deposition; it favours higher minute ventilation, which may enhance aerosol delivery to the distal airways; and, finally, it reduces particle impaction within the delivery system.
In 1993, Anderson and coworkers [43] evaluated aerosol delivery in 10 asthmatic patients using an inhaled radionuclide aerosol with He/O2 as the driving gas, and found that particle deposition in the airways was improved. These findings were corroborated by Goode and coworkers [44] in the setting of mechanical ventilation. These investigators, using an in vitro model of mechanical ventilation, observed an improvement in aerosol deposition in the distal airways when He/O2 was used as the driving gas at various various inspired fractions of helium. The improvement was similar whatever aerosol technique was used (metered dose inhalers or jet nebulizers). It is important to note that it was necessary to operate the jet nebulizer at a flow rate of 15 l/min (for an various inspired fraction of helium at 70%) to obtain aerosol delivery equivalent to that obtained with pure oxygen at a flow rate of 6 l/min. Diagrams with conversion factors are available that allow the operating flow rate to be set at a level appropriate for use of He/O2 with jet nebulizers [45]. This is important because use of an inadequate operating flow with He/O2 prevents aerosolization of drug particles [44].
He/O2 has been evaluated for use as the driving gas for nebulizing β2-agonists in the setting of asthma crisis [22, 46–52] and in COPD exacerbations [53]. There were some discrepancies between the findings of these studies because of differences in methods employed, severity of illness, aerosol delivery technique and duration of therapy [42]. The use of He/O2 in such circumstances probably requires the use of specific devices that can exploit the properties of He/O2 during nebulization. The use of a large volume nebulizer and reservoir may also be important when using He/O2 to deliver aerosol drugs, particularly in teenagers and adults, who may have minute ventilation requirements that exceed the output rate of small volume nebulizers [54]. Corcoran and Gamard [45] stressed that the use of He/O2 for nebulization requires a large volume nebulizer and reservoir to prevent entrainment of room air.
Cost and technical problems with the use of helium-oxygen mixtures
Equipment and costs
He/O2 is provided in tanks of various sizes. Tanks containing 50 l are most frequently used. They contain 78% helium and 22% oxygen, and are pressurized at approximately 200 bars. Some manufacturers provide a mixture that includes less helium (70% helium and 30% oxygen). The 50 l tank (78% helium/22% oxygen) costs approximately 200 euros. Air regulators can be screwed onto the tank and then connected to the ventilator or flow meter using the appropriate connectors. However, He/O2 regulators and flow meters are commercially available and should be used when possible. It is difficult to estimate the daily consumption of a patient because of heterogeneity in the conditions of use (spontaneous or mechanical ventilation), ventilator settings (in the setting of mechanical ventilation) and duration of use. In our experience in the setting of continuous use, daily consumption and cost vary between one and three tanks and from 200 to 600 euros, respectively. Based on the only available study in which a cost evaluation was done, that conducted by Jolliet and coworkers [32], the daily cost of He/O2 use amounted to US$69 ± 46 in the setting of discontinuous use during NIPPV. In that study, because of the reduced length of stay of decompensated COPD patients in the ICU with He/O2 use, total hospitalization costs were reduced by US$3348 per patient with He/O2. However, the findings of that study reflect the practice of short discontinuous trials of NIPPV, as were used in the participating centres, and so more prolonged use of He/O2 will incur greater costs.
Technical problems with mechanical ventilators
Only gaseous He/O2 with fractional inspired oxygen similar to that in air may be used clinically; this avoids any risk that a gas without sufficient oxygen will be administered. The physical properties of helium can interfere with mechanical ventilator functions such as gas mixing, inspiratory and expiratory valve accuracy, flow measurement, volume delivery, triggering and automatic leakage compensation. This has been evaluated in several reports of ventilator functioning with He/O2 in the ICU [55–58].
The ventilator currently marketed that permits safe use of He/O2 for both invasive and noninvasive ventilation is the Avea™ ventilator (VIASYS Health Care, Conshohocken, Pennsylvania, USA). This ventilator can deliver He/O2 appropriately by changing a connector on the back panel. All volumes are automatically compensated with He/O2. Perino and coworkers [59] evaluated this ventilator in different modes in a lung model. They concluded that volume delivery is clinically acceptable with this ventilator. Ventilators designed specifically for NIPPV such as BiPAPVision™ Respironics, Pitsburgh, Pennsylvania, USA) are not accurate with He/O2 [60]. GE Healthcare recently developed the Aptaér™ heliox delivery system (GE Healthcare, Madison, Wisconsin, USA). The sole ventilatory mode available on this ventilator is the pressure support mode. It incorporates the Aeroneb™ Professional Nebulizer System (Aerogen Pro, Nektar Therapeutics, Moutain View, California, USA). The Aeroneb™ Professional Nebulizer System is an aerosol generator that creates a fine droplet, low velocity aerosol of specific particle size, with very low residual volume. Operation of the aerosol generator is independent of gas density or flow rate [61]. Little has been published on the performance of this device.
Finally, helium have a high thermal conductivity (352 μcal/cm/s/°K). This physical property explains why helium affects the hotwire flow sensors used in some ventilators. Humidification and warming of helium may cause problems, particularly during mechanical ventilation. To our knowledge there are no studies addressing this problem in the literature. The ideal technique for conditioning He/O2 (heated humidifier or heat-moisture exchanger) is not known. We use a heated humidifier. Less heat is lost during breathing because the thermal capacity of He/O2 is less than that of the same volume of air. If He/O2 is administered via a face mask, then the face may feel cool [62].
Hypothermia has been associated with hood administration of He/O2 to infants with bronchiolitis. Heat loss occurs if the body is surrounded by He/O2 rather than by air because heat conductance is the major factor in loss of heat from the skin [62].
Safe use of He/O2 requires specific equipment and investment. He/O2 is expensive and He/O2 tanks are relatively cumbersome for use out of a hospital. Because of the lack of high level evidence for use of He/O2 in clinical practice, many intensive care physicians do not wish to invest in the equipment necessary to use He/O2 except in certain centres for research purposes.
Conclusion
Reliable physical and physiological theories support the assertion that helium can improve ventilatory function, essentially by reducing the resistance of the airways, which is considered the main physiopathological element of obstructive syndromes. However, the level of evidence does not permit a formal recommendation to be made regarding the use of He/O2 in the ICU. Numerous questions remain unanswered concerning the use of He/O2 and must be addressed. For instance, which patients may benefit from He/O2 use, in the setting of COPD or asthma? Is He/O2 useful in combination with noninvasive mechanical ventilation or with aerosol delivery? What is the role of He/O2 in mechanically ventilated patients? Finally, what is the best delivery system for He/O2?
Until these questions are answered, the specific role for He/O2 as a therapeutic tool in the ICU remains to be defined.
Abbreviations
- COPD:
-
chronic obstructive pulmonary disease
- FEV1:
-
forced expiratory volume in 1 s
- He/O2:
-
helium-oxygen
- ICU:
-
intensive care unit
- NIPPV:
-
noninvasive positive pressure ventilation
- PEEPi:
-
intrinsic positive end-expiratory pressure
- WOB:
-
work of breathing.
References
Barach AL: Use of helium as a new therapeutic gas. Proc Soc Exp Biol Med 1934, 32: 462.
Barach AL: The use of helium in the treatment of asthma and obstructive lesions in the larynx and trachea. Ann Intern Med 1935, 9: 739-765.
Douglas F, Gasiorek JM, Swaffield JA: Fluid Mechanics. Harlow, UK: Prentice Hall; 2001.
Papamoschou D: Theoretical validation of the respiratory benefits of helium-oxygen mixtures. Respir Physiol 1995, 99: 183-190. 10.1016/0034-5687(94)00071-7
Drazen JM, Loring SH, Ingram RH Jr: Distribution of pulmonary resistance: effects of gas density, viscosity, and flow rate. J Appl Physiol 1976, 41: 388-395.
Wood LD, Engel LA, Griffin P, Despas P, Macklem PT: Effect of gas physical properties and flow on lower pulmonary resistance. J Appl Physiol 1976, 41: 234-244.
Myers TR: Therapeutic gases for neonatal and pediatric respiratory care. Respir Care 2003, 48: 399-422. discussion: 423–395
Ho AM, Dion PW, Karmakar MK, Chung DC, Tay BA: Use of heliox in critical upper airway obstruction. Physical and physiologic considerations in choosing the optimal helium:oxygen mix. Resuscitation 2002, 52: 297-300. 10.1016/S0300-9572(01)00473-7
Khanlou H, Eiger G: Safety and efficacy of heliox as a treatment for upper airway obstruction due to radiation-induced laryngeal dysfunction. Heart Lung 2001, 30: 146-147. 10.1067/mhl.2001.112026
Grosz AH, Jacobs IN, Cho C, Schears GJ: Use of helium-oxygen mixtures to relieve upper airway obstruction in a pediatric population. Laryngoscope 2001, 111: 1512-1514. 10.1097/00005537-200109000-00004
Mizrahi S, Yaari Y, Lugassy G, Cotev S: Major airway obstruction relieved by helium/oxygen breathing. Crit Care Med 1986, 14: 986-987. 10.1097/00003246-198611000-00016
Curtis JL, Mahlmeister M, Fink JB, Lampe G, Matthay MA, Stulbarg MS: Helium-oxygen gas therapy. Use and availability for the emergency treatment of inoperable airway obstruction. Chest 1986, 90: 455-457.
Skrinskas GJ, Hyland RH, Hutcheon MA: Using helium-oxygen mixtures in the management of acute upper airway obstruction. CMAJ 1983, 128: 555-558.
Lu TS, Ohmura A, Wong KC, Hodges MR: Helium-oxygen in treatment of upper airway obstruction. Anesthesiology 1976, 45: 678-680. 10.1097/00000542-197612000-00020
Weber JE, Chudnofsky CR, Younger JG, Larkin GL, Boczar M, Wilkerson MD, Zuriekat GY, Nolan B, Eicke DM: A randomized comparison of helium-oxygen mixture (Heliox) and racemic epinephrine for the treatment of moderate to severe croup. Pediatrics 2001, 107: E96. 10.1542/peds.107.6.e96
Abd-Allah SA, Rogers MS, Terry M, Gross M, Perkin RM: Helium-oxygen therapy for pediatric acute severe asthma requiring mechanical ventilation. Pediatr Crit Care Med 2003, 4: 353-357. 10.1097/01.PCC.0000074267.11280.78
Gluck EH, Onorato DJ, Castriotta R: Helium-oxygen mixtures in intubated patients with status asthmaticus and respiratory acidosis. Chest 1990, 98: 693-698.
Kass JE, Castriotta RJ: Heliox therapy in acute severe asthma. Chest 1995, 107: 757-760.
Kass JE, Terregino CA: The effect of heliox in acute severe asthma: a randomized controlled trial. Chest 1999, 116: 296-300. 10.1378/chest.116.2.296
Manthous CA, Hall JB, Caputo MA, Walter J, Klocksieben JM, Schmidt GA, Wood LD: Heliox improves pulsus paradoxus and peak expiratory flow in nonintubated patients with severe asthma. Am J Respir Crit Care Med 1995, 151: 310-314.
Shiue ST, Gluck EH: The use of helium-oxygen mixtures in the support of patients with status asthmaticus and respiratory acidosis. J Asthma 1989, 26: 177-180.
Sattonnet P, Plaisance P, Lecourt L, Vicaut E, Adnet P, Goldstein P, Marx JS, Ecollan P, Ricard-Hibon A, Bagou G, et al.: The efficacy of continuous administration of helium-oxygen mixture (65%–35%) in acute asthma exacerbation [abstract; in French]. Réanimation 2003, (Suppl 3):128s-129s.
Rodrigo GJ, Rodrigo C, Pollack CV, Rowe B: Use of helium-oxygen mixtures in the treatment of acute asthma: a systematic review. Chest 2003, 123: 891-896. 10.1378/chest.123.3.891
Kass JE: Heliox redux. Chest 2003, 123: 673-676. 10.1378/chest.123.3.673
Gerbeaux P, Boussuges A, Torro D, Jean P: Heliox in the treatment of obstructive hypoventilation. Am J Emerg Med 1998, 16: 215-216. 10.1016/S0735-6757(98)90051-1
Polito A, Fessler H: Heliox in respiratory failure from obstructive lung disease. N Engl J Med 1995, 332: 192-193. 10.1056/NEJM199501193320318
Gerbeaux P, Gainnier M, Boussuges A, Rakotonirina J, Nelh P, Torro D, Arnal JM, Jean P: Use of heliox in patients with severe exacerbation of chronic obstructive pulmonary disease. Crit Care Med 2001, 29: 2322-2324. 10.1097/00003246-200112000-00015
Brochard L, Mancebo J, Wysocki M, Lofaso F, Conti G, Rauss A, Simonneau G, Benito S, Gasparetto A, Lemaire F, et al.: Noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary disease. N Engl J Med 1995, 333: 817-822. 10.1056/NEJM199509283331301
Plant PK, Owen JL, Elliott MW: Early use of non-invasive ventilation for acute exacerbations of chronic obstructive pulmonary disease on general respiratory wards: a multicentre randomised controlled trial. Lancet 2000, 355: 1931-1935. 10.1016/S0140-6736(00)02323-0
Jolliet P, Tassaux D, Thouret JM, Chevrolet JC: Beneficial effects of helium:oxygen versus air:oxygen noninvasive pressure support in patients with decompensated chronic obstructive pulmonary disease. Crit Care Med 1999, 27: 2422-2429. 10.1097/00003246-199911000-00017
Jaber S, Fodil R, Carlucci A, Boussarsar M, Pigeot J, Lemaire F, Harf A, Lofaso F, Isabey D, Brochard L: Noninvasive ventilation with helium-oxygen in acute exacerbations of chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2000, 161: 1191-1200.
Jolliet P, Tassaux D, Roeseler J, Burdet L, Broccard A, D'Hoore W, Borst F, Reynaert M, Schaller MD, Chevrolet JC: Helium-oxygen versus air-oxygen noninvasive pressure support in decompensated chronic obstructive disease: A prospective, multicenter study. Crit Care Med 2003, 31: 878-884. 10.1097/01.CCM.0000055369.37620.EE
Maggiore S, Richard JC, Abroug F, Diehl JL, Sauder P, Mancebo J, Ferrer M, Bonmarchand G, Breton L, Lecourt L, et al.: Efficacy assessment of helium-oxygen mixture (Oxhel) in association with non invasive positive pressure ventilation during acute exacerbation of chronic obstructive pulmonary disease [abstract; in French]. Réanimation 2005,14(Suppl 1):SO77. 45s–46s
Poggi R, Polese G, Morandini GC, Rossi A: COPD patients and mechanical ventilation with positive end expiratory pressure (PEEP). Monaldi Arch Chest Dis 1994, 49: 40-42.
Rossi A, Ganassini A, Polese G, Grassi V: Pulmonary hyperinflation and ventilator-dependent patients. Eur Respir J 1997, 10: 1663-1674. 10.1183/09031936.97.10071663
Tassaux D, Jolliet P, Roeseler J, Chevrolet JC: Effects of helium-oxygen on intrinsic positive end-expiratory pressure in intubated and mechanically ventilated patients with severe chronic obstructive pulmonary disease. Crit Care Med 2000, 28: 2721-2728. 10.1097/00003246-200008000-00006
Gainnier M, Arnal JM, Gerbeaux P, Donati S, Papazian L, Sainty JM: Helium-oxygen reduces work of breathing in mechanically ventilated patients with chronic obstructive pulmonary disease. Intensive Care Med 2003, 29: 1666-1670. 10.1007/s00134-003-1911-z
Lee DL, Lee H, Chang HW, Chang AY, Lin SL, Huang YC: Heliox improves hemodynamics in mechanically ventilated patients with chronic obstructive pulmonary disease with systolic pressure variations. Crit Care Med 2005, 33: 968-973. 10.1097/01.CCM.0000163403.42842.FE
Diehl JL, Mercat A, Guerot E, Aissa F, Teboul JL, Richard C, Labrousse J: Helium/oxygen mixture reduces the work of breathing at the end of the weaning process in patients with severe chronic obstructive pulmonary disease. Crit Care Med 2003, 31: 1415-1420. 10.1097/01.CCM.0000059720.79876.B5
Jaber S, Carlucci A, Boussarsar M, Fodil R, Pigeot J, Maggiore S, Harf A, Isabey D, Brochard L: Helium-oxygen in the postextubation period decreases inspiratory effort. Am J Respir Crit Care Med 2001, 164: 633-637.
Tassaux D, Gainnier M, Battisti A, Jolliet P: Helium-oxygen decreases inspiratory effort and work of breathing during pressure support in intubated patients with chronic obstructive pulmonary disease. Intensive Care Med 2005, 31: 1501-1507. 10.1007/s00134-005-2796-9
Kim IK, Saville AL, Saville AL, Corcoran TE: Heliox-driven albuterol nebulization for asthma exacerbations: an overview. Respir Care 2006, 51: 613-618.
Anderson M, Svartengren M, Bylin G, Philipson K, Camner P: Deposition in asthmatics of particles inhaled in air or in helium-oxygen. Am Rev Respir Dis 1993, 147: 524-528.
Goode ML, Fink JB, Dhand R, Tobin MJ: Improvement in aerosol delivery with helium-oxygen mixtures during mechanical ventilation. Am J Respir Crit Care Med 2001, 163: 109-114.
Corcoran TE, Gamard S: Development of aerosol drug delivery with helium oxygen gas mixtures. J Aerosol Med 2004, 17: 299-309. 10.1089/jam.2004.17.299
Bag R, Bandi V, Fromm RE Jr, Guntupalli KK: The effect of heliox-driven bronchodilator aerosol therapy on pulmonary function tests in patients with asthma. J Asthma 2002, 39: 659-665. 10.1081/JAS-120014931
Henderson SO, Acharya P, Kilaghbian T, Perez J, Korn CS, Chan LS: Use of heliox-driven nebulizer therapy in the treatment of acute asthma. Ann Emerg Med 1999, 33: 141-146. 10.1016/S0196-0644(99)70386-0
Kim IK, Phrampus E, Venkataraman S, Pitetti R, Saville A, Corcoran T, Gracely E, Funt N, Thompson A: Helium/oxygen-driven albuterol nebulization in the treatment of children with moderate to severe asthma exacerbations: a randomized, controlled trial. Pediatrics 2005, 116: 1127-1133. 10.1542/peds.2004-2136
Kress JP, Noth I, Gehlbach BK, Barman N, Pohlman AS, Miller A, Morgan S, Hall JB: The utility of albuterol nebulized with heliox during acute asthma exacerbations. Am J Respir Crit Care Med 2002, 165: 1317-1321. 10.1164/rccm.9907035
Lee DL, Hsu CW, Lee H, Chang HW, Huang YC: Beneficial effects of albuterol therapy driven by heliox versus by oxygen in severe asthma exacerbation. Acad Emerg Med 2005, 12: 820-827. 10.1197/j.aem.2005.04.020
Rivera ML, Kim TY, Stewart GM, Minasyan L, Brown L: Albuterol nebulized in heliox in the initial ED treatment of pediatric asthma: a blinded, randomized controlled trial. Am J Emerg Med 2006, 24: 38-42. 10.1016/j.ajem.2005.06.007
Rose J, Panacek E, Miller P: Prospective randomized trial of heliox-driven continuous nebulizers in the treatment of asthma in the emergency department. J Emerg Med 2002, 22: 133-137. 10.1016/S0736-4679(01)00454-1
deBoisblanc BP, DeBleiux P, Resweber S, Fusco EE, Summer WR: Randomized trial of the use of heliox as a driving gas for updraft nebulization of bronchodilators in the emergent treatment of acute exacerbations of chronic obstructive pulmonary disease. Crit Care Med 2000, 28: 3177-3180. 10.1097/00003246-200009000-00009
Corcoran TE, Shortall BP, Kim IK, Meza MP, Chigier N: Aerosol drug delivery using heliox and nebulizer reservoirs: results from an MRI-based pediatric model. J Aerosol Med 2003, 16: 263-271. 10.1089/089426803769017631
Brown MK, Willms DC: A laboratory evaluation of 2 mechanical ventilators in the presence of helium-oxygen mixtures. Respir Care 2005, 50: 354-360.
Oppenheim-Eden A, Cohen Y, Weissman C, Pizov R: The effect of helium on ventilator performance: study of five ventilators and a bedside Pitot tube spirometer. Chest 2001, 120: 582-588. 10.1378/chest.120.2.582
Tassaux D, Jolliet P, Thouret JM, Roeseler J, Dorne R, Chevrolet JC: Calibration of seven ICU ventilators for mechanical ventilation with helium-oxygen mixtures. Am J Respir Crit Care Med 1999, 160: 22-32.
Berkenbosch JW, Grueber RE, Dabbagh O, McKibben AW: Effect of helium-oxygen (heliox) gas mixtures on the function of four pediatric ventilators. Crit Care Med 2003, 31: 2052-2058. 10.1097/01.ccm.0000084804.15352.48
Perino C, Hess D: Heliox delivery using the AVEA ventilator [abstract]. Respir Care 2003, 48: 1093.
Chatmongkolchart S, Kacmarek RM, Hess DR: Heliox delivery with noninvasive positive pressure ventilation: a laboratory study. Respir Care 2001, 46: 248-254.
Fink J, Heramia M, Bathe D, Watson A: Heliox improves aerosol deposition and tidal volume in a model of acute airway obstruction [abstract]. Critical Care 2003,7(Suppl 2):P157. 10.1186/cc2046
Myers TR: Use of heliox in children. Respir Care 2006, 51: 619-631.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
About this article
Cite this article
Gainnier, M., Forel, JM. Clinical review: Use of helium-oxygen in critically ill patients. Crit Care 10, 241 (2006). https://doi.org/10.1186/cc5104
Published:
DOI: https://doi.org/10.1186/cc5104