Abstract
Background
Oxygen therapy is essential in the management of patients with respiratory problem, including after endotracheal extubation. Conventional oxygen devices may be inadequate in patients requiring high inspiratory flow. HFNC has a growing place in the repertoire of respiratory therapies. The purpose of this study was to compare the efficiency, tolerability, and outcome of HFNC in patients with respiratory failure and post-mechanical ventilation patients in comparison to NIV and conventional oxygen devices.
Results
In case of respiratory failure patients, there was non-significant statistical difference between HFNC, conventional oxygen therapy and NIV, regarding the difference in ABGs, vital data, and dyspnea scores, at successive time points, except for PO2 after 30 min in patients received NIV, which was significantly higher. There was non-significant statistical difference between the three mentioned modalities of oxygen therapy regarding comfort and clinical outcome.
In case of post-extubation patients, there was non-significant statistical difference between the HFNC and conventional oxygen therapy regarding clinical parameters, comfort and outcome.
Conclusions
HFNC is comparable to conventional oxygen therapy in respiratory failure and post-extubation patients. HFNC is comparable to NIV in respiratory failure patients.
Similar content being viewed by others
Background
Respiratory failure is a condition in which the respiratory system fails in one or both of its gas-exchanging functions—i.e., oxygenation of, and carbon dioxide elimination from, mixed venous (pulmonary arterial) blood [1].
Administration of oxygen is an essential support measure to maintain proper tissue oxygenation in patients with acute respiratory failure [2].
Oxygen therapy can be delivered—depending on the severity of the patient’s respiratory distress—during either unassisted (via nasal cannulas or facemasks) or assisted breathing with non-invasive or invasive mechanical ventilation [3].
Oxygen therapy is essential in the management of patients who have a respiratory problem, including after endotracheal extubation. Oxygen supply via face mask with bag is routinely used in these patients, but this method may be inadequate in some patients, especially if they require a high inspiratory flow [4].
Oxygen delivery via high-flow nasal cannula (HFNC) has a growing place in the repertoire of respiratory therapies available in the intensive care environment [5].
HFNC is a new technological device in a high-flow oxygen system that consists of an air-oxygen blender, which allows from 0.21 to 1.00 FIO2and which generates a gas flow of up to 55 L/min, and a heated humidification system [6].
The beneficial effects of HFNC have been widely reported: heated humidification during HFNC improves patient comfort [7]; flushing of anatomical dead space reduces CO2 level [8]; and the expiratory resistance produced by the continuous high flow causes a low level of positive oropharyngeal airway pressure [9].
HFNC has been evaluated in many groups, including healthy subjects, patients with acute respiratory failure, and patients recovering from post-cardiac surgery. Extubated patients will need a high inspiratory flow and adequate oxygen supplementation, so after extubation, a high flow of oxygen may be necessary to compensate for the work of breathing; thus, HFNC may have a role in this situation [10].
Methods
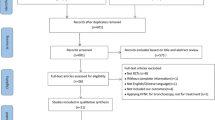
This was a prospective study conducted upon 115 patients at the Respiratory Intensive Care Unit of a tertiary Chest Hospital in the period between June 2015 and September 2018.
The patients were classified into two groups; group A included 69 patients with respiratory failure not candidate for intubation and invasive mechanical ventilation and were assigned to receive either HFNC (The Optiflow™ system, Fisher and Paykel Healthcare Limited, Auckland, New Zealand), conventional oxygen therapy or non-invasive mechanical ventilation, equally allocated, 23 patients to each subgroup. Group B included 46 extubated post-mechanical ventilation patients and were assigned to receive either HFNC or conventional oxygen therapy, equally allocated, 23 patients to each subgroup. Allocation to each subgroup was done by simple randomization using random allocation software.
Patients fulfilling the criteria for immediate mechanical ventilation were excluded form group A. Patients who failed weaning in the same admission were excluded from group B.
All patients were subjected to the following:
-
1.
Detailed medical history taking and clinical examination.
-
2.
Routine laboratory investigations, plain chest X-ray postero–anterior view and electrocardiography.
-
3.
Serial arterial blood gases:
-
For group A: at baseline, 30 min and 120 min following the application of oxygen intervention and at the end of first day of oxygen intervention.
-
For group B: at baseline, 30 min, 120 min, and 48 h after extubation, where at 48 h, the patient is considered successfully weaned from mechanical ventilation.
-
4.
Serial subjective assessments of patients:
-
a.
Patient’s comfort by direct “yes” or “no” answer.
-
b.
Borg dyspnea scale [11]: at baseline, 30 min, 120 min, and end of day of oxygen intervention for group A and at baseline, 30 min, 120 min, and 48 hours after extubation for group B.
-
a.
-
5.
Serial objective assessments of patients:
-
a.
Vital data: blood pressure, pulse and respiratory rate.
-
b.
Respiratory Distress Observation Scale (RDOS) [12] at baseline, 30 min, 120 min, and end of day of oxygen intervention for group A and at baseline, 30 min, 120 min, and 48 h after extubation for group B.
-
c.
Several demographic data: the need for intubation and mechanical ventilation, days on mechanical ventilation, duration of ICU stay, morbidity
-
a.
-
6.
The outcome: mortality or improvement and discharge.
Statistical analysis
The collected data was revised, coded, tabulated and introduced to a personal computer (PC) using Statistical package for Social Science (IBM Corp. Released 2011. IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp.). Data was presented and suitable analysis was done according to the type of data obtained for each parameter. Descriptive statistics were described as mean, standard deviation (±SD) and range for parametric numerical data, and Frequency and percentage of non-numerical data. Analytical statistics described as Student’s t test used to assess the statistical significance of the difference between two study group means, ANOVA test used to assess the statistical significance of the difference between more than two study group means, correlation analysis to assess the strength of association between two quantitative variables. The correlation coefficient denoted symbolically “r” defines the strength and direction of the linear relationship between two variables, and chi-square test used to examine the relationship between two qualitative variables. The results were considered to be statistically significant at a p value less than 0.05, highly significant at a p value less than 0.01, and insignificant at a p value more than 0.05.
Results
Sixty-nine patients were enrolled in group A; their demographic and clinical characteristics are shown in (Table 1).
In group A, regarding the difference in ABGs, vial data, RDOS, and Borg dyspnea scale across the three subgroups, there was non-significant statistical difference between the HFNC, conventional oxygen therapy, and NIV subgroups at successive time points, except for PO2 after 30 min in the NIV subgroup, which was significantly higher than the HFNC and conventional subgroups, but it is worth mentioning, that this statistically significant difference was not detected after 120 min and 24 h of therapy (Fig. 1). There was statistically significant difference regarding PCOs between NIV and conventional subgroups, being higher in the NIV subgroup, but this difference was observed at the start of the oxygen therapy as well as after 30 min, 120 min, and 24 h from therapy (Tables 2, 3, and 4). (Figs. 2, 3 and 4).
Regarding the tolerability and outcome in group A, there was non-significant statistical difference between the HFNC, conventional oxygen therapy and NIV subgroups in comfort, intubation, duration of mechanical ventilation, duration of ICU stay, and mortality.
Forty-six patients were enrolled in group B; their demographic and clinical characteristics are shown in (Table 5).
In group B, regarding the difference in ABGs, vial data, RDOS, and Borg dyspnea scale across the subgroups, there was non-significant statistical difference between the HFNC and conventional oxygen therapy subgroups as regards all ABG parameters (pH, PCO2, PO2, HCO3, Be, and O2Sat), respiratory rate, blood pressure, pulse rate, RDOS, and Borg scale after 30 min, 120 min, and 48 h of starting oxygen therapy (Table 6, 7, and 8).
Regarding the tolerability and outcome in group B, there was non-significant statistical difference between the HFNC and conventional oxygen therapy in comfort, re-intubation, duration of mechanical ventilation, duration of ICU stay, and mortality (Table 5).
In comparison of both HFNC subgroups between group A and B, as regards the ABGs, vital data, RDOS, and Borg dyspnea scale, there was statistically significant difference regarding respiratory rate, RDOS and Borg scale at start of oxygen therapy as well as, after 30 min, 120 min, and at end of follow-up period of oxygen therapy, being higher in group A. There was non-significant statistical difference regarding ABG parameters, blood pressure, and pulse rate after 30 min, 120 min, and at end of follow-up period of oxygen therapy (Table 9).
Regarding tolerability and outcome in both HFNC subgroups between group A and B, there was non-significant statistical difference between both subgroups in comfort, intubation, and mechanical ventilation, duration of mechanical ventilation, duration of ICU stay, and mortality (Table 10).
Discussion
The aim of this study was to compare the efficiency, tolerability, and outcome of oxygen therapy using HFNC in patients with acute respiratory failure and post-mechanical ventilation patients in comparison to NIV and conventional oxygen devices. To achieve this aim, the study enrolled two groups, group A consists of 69 respiratory failure patients assigned to receive either; HFNC, conventional oxygen therapy or NIV (23 patients each) , and group B consists of 46 post-extubation patients assigned to receive either HFNC or conventional oxygen therapy (23 patients each).
The current study proved that HFNC has comparable efficiency versus conventional oxygen devices and NIV in respiratory failure patients. In group A, regarding the difference in ABGs, vial data, RDOS and Borg dyspnea scale across the three subgroups, there was non-significant statistical difference between the HFNC, conventional oxygen therapy, and NIV subgroups at successive time points, except for PO2 after 30 min in the NIV subgroup, which was significantly higher than the HFNC and conventional subgroups. These results were in agreement with Schwabbauer et al. (2014) [13] where they compared the short-term effects of oxygen therapy via a HFNC in comparison to NIV and standard treatment. In Schwabbauer et al. [13] study, PO2 with NIV was significantly higher than PO2 with HFNC after 30 min of oxygen therapy. On the other hand, the results in the current study were partially consistent with Rittayami et al. (2015) [14], where they investigated the effects of HFNC in terms of physiologic, adverse events, and hospitalization rate compared with conventional oxygen therapy in subjects with acute dyspnea and hypoxemia. Similar to the current study, Rittayami et al. (2015) [14] found no statistical significant difference between both HFNC and conventional oxygen groups regarding blood pressure and PO2. Meanwhile, they found that respiratory rate at 30 min and heart rate at end of study as well as the dyspnea score at end of study period were significantly less in the HFNC than the conventional group. However, the study by Rittayami et al. (2015) [14] was conducted in the emergency department rather than the ICU with the trial period over 60 min only. Meanwhile, the results in the current study were comparable to Lemiale et al. (2015) [15], where they studied the effects of a two-hour trial of HFNC versus Venturi mask in immunocompromised patients with hypoxemic acute respiratory failure. They found no significant difference in heart rate, respiratory rate, or dyspnea score between the two study groups.
The current study proved that HFNC has comparable tolerability as well as similar clinical outcome versus conventional oxygen devices and NIV in respiratory failure patients. In group A, there was non-significant statistical difference between the HFNC, conventional oxygen therapy, and NIV subgroups in comfort, intubation, duration of mechanical ventilation, duration of ICU stay, and mortality. However, Rittayami et al. (2015) [14], the aforementioned study, found significant better comfort with HFNC as compared to the conventional oxygen therapy. But it is worth mentioning that the study by Rittayami et al. (2015) [14] conducted a short period of 60 min trials of oxygen therapy. Meanwhile, the previously mentioned study by Schwabbauer et al. (2014) [13] found better comfort with HFNC as compared with NIV, but the oxygen therapy trials were conducted over a 30-min period and recruited type I respiratory failure patients only. On the other hand, the results of the current study were in agreement with Lemiale et al. (2015) [15] the aforementioned study, where there was no significant difference between the HFNC and Venturi mask groups regarding the need for mechanical ventilation during the study period.
The current study proved that HFNC has comparable efficiency versus conventional oxygen devices in post-extubation patients. In group B, regarding the difference in ABGs, vial data, RDOS, and Borg dyspnea scale across the subgroups, there was non-significant statistical difference between the HFNC and conventional oxygen therapy subgroups as regards all ABG parameters, respiratory rate, blood pressure, pulse rate, RDOS, and Borg scale after 30 min, 120 min, and 24 h of starting oxygen therapy. These results were in agreement with the study by Fernandez et al. (2017) [16], where they conducted a trial in patients who passed a spontaneous breathing trial to be assigned to receive HFNC or conventional oxygen for 24 h after extubation. Fernandez et al. (2017) [16] observed no significant difference in oxygenation, respiratory acidosis, or respiratory rate between the two groups. Rittayami et al. (2014) [17] compared the short-term benefit of HFNC with non-rebreathing mask in terms of change in dyspnea, physiologic variables, and patient comfort in subjects after endotracheal extubation. Similar to the current study, there was no significant difference in SPO2 and BP between HFNC and conventional oxygen therapy, but on the other hand, they observed better heart rate, respiratory rate, and dyspnea score with the HFNC in comparison to conventional therapy. However, Rittayami et al. (2014) [17] applied HFNC and conventional oxygen to the patients in sequential matter 30 min each to same patients’ subset, where the use of one oxygen device could affect the outcome of the other device whomever were used first, and this is clearly different than the current study design.
The current study proved that HFNC has comparable tolerability as well as similar clinical outcome versus conventional oxygen devices in post-extubation patients. In group B, there was non-significant statistical difference between the HFNC and conventional oxygen therapy in comfort, re-intubation, duration of mechanical ventilation, duration of ICU stay, and mortality. These results were similar to the previously mentioned study by Rittayami et al. (2014) [17]. The results in the current study were also in agreement with Fernandez et al. (2017) [16], the aforementioned study, where they found no significant difference between HFNC and conventional oxygen after extubation regarding rate of re-intubation, duration of ICU stay, and mortality.
In comparison of both HFNC subgroups between group A and B, as regards the ABGs, vital data, RDOS, and Borg dyspnea scale, there was statistically significant difference regarding respiratory rate, RDOS, and Borg scale at start of oxygen therapy as well as, after 30 min, 120 min, and at end of follow-up period of oxygen therapy, being higher in group A. There was non-significant statistical difference regarding ABG parameters, blood pressure, and pulse rate after 30 min, 120 min, and at end of follow-up period of oxygen therapy.
Regarding tolerability and outcome in both HFNC subgroups of both groups A and B, there was non-significant statistical difference between both subgroups in comfort, intubation and mechanical ventilation, duration of mechanical ventilation, duration of ICU stay, and mortality.
Conclusion
-
Conventional oxygen devices remain the standard methods in respiratory failure patients with the advantage of being cheap, available, and easy to use.
-
HFNC proved to be an accepted alternative to conventional oxygen devices, with similar physiological effects, tolerability, and clinical outcome.
-
HFNC is a comparable method of oxygen therapy to different conventional oxygen devices in variable diagnoses and variable clinical situations.
-
HFNC is also comparable to conventional oxygen devices in post-extubation patients with respiratory failure.
-
HFNC is comparable to NIV in respiratory failure patients. This is particularly useful because NIV setting is more expensive, more resource-intensive, and more difficult to monitor and maintain.
Availability of data and materials
Tables included.
Abbreviations
- ABG:
-
Arterial blood gases
- ANOVA:
-
Analysis of variance
- BE:
-
Base excess
- CO2:
-
Carbon dioxide
- COPD:
-
Chronic obstructive pulmonary disease
- DBP:
-
Diastolic blood pressure
- DVT:
-
Deep venous thrombosis
- FIO2:
-
Fraction of inspired oxygen
- HCO3:
-
Bicarbonate
- HFNC:
-
High-flow nasal cannula
- ICU:
-
Intensive care unit
- Max:
-
Maximum
- Min:
-
Minimum
- N:
-
Number
- NIV:
-
Non-invasive ventilation
- PC:
-
Personal computer
- PCO2:
-
Partial pressure of carbon dioxide
- PO2:
-
Partial pressure on oxygen
- RDOS:
-
Respiratory distress observation scale
- RICU:
-
Respiratory intensive care unit
- RR:
-
Respiratory rate
- SBP:
-
Systolic blood pressure
- SD:
-
Standard deviation
- SPO2:
-
Oxygen saturation of hemoglobin
References
Michael AG (2008) Respiratory failure: an overview. In: Alfred PF, Jack AE, Jay AF, Michael AG, Robert MS, Allan IP (eds) Fishman’s pulmonary diseases and disorders, vol 2, 4th edn. New York, USA, McGraw-Hill Medical, pp 2509–21.
Oriol R, Jordi R, Ferran T et al (2010) High-flow oxygen therapy in acute respiratory failure. Respir Care 55(4):408–413
Hugo L, Benjamin S, Christophe L et al (2012) Humidified high flow nasal oxygen during respiratory failure in the emergency department: feasibility and efficacy. Respir Care 57(11):1873–1878
L’Her E, Deye N, Lellouche F et al (2005) Physiologic effects of non invasive ventilation during acute lung injury. Am J Respir Crit Care Med 172(9):1112–1118
Rachael LP, Shay PM, Michelle LE (2011) A preliminary randomized controlled trial to assess effectiveness of nasal high-flow oxygen in intensive care patients. Respir Care 56(3):265–270
Ricard JD (2012) High flow nasal oxygen in acute respiratory failure. Minerva Anestesiol 78(7):836–841
Dysart K, Miller TL, Wolfson MR et al (2009) Research in high flow therapy: mechanisms of action. Respir Med 103(10):1400–1405
Lee JH, Rehder KJ, Williford L et al (2013) Use of high flow nasal cannula in critically ill infants, children, and adults: a critical review of the literature. Intensive Care Med 39(2):247–257
Parke RL, Eccleston ML, McGuinness SP (2011) The effects of flow onairway pressure during nasal high-flow oxygen therapy. Respir Care 56(8):1151–1155
Nuttapol R, Jamsak T, Pitchayapa R (2014) High-flow nasal cannula versus conventional oxygen therapy after endotracheal extubation: a randomized crossover physiologic study. Respir Care 59(4):485–490
Borg GA (1982) Psychophysical bases of perceived exertion. Med SciSports Exerc 14:377–381
Campbell (2007) Psychometric testing of a respiratory distress observation scale. J Palliat Med 11(1):44–50
Schwabbauer N, Berg B, Blumenstock G et al (2014) Nasal high–flow oxygen therapy in patients with hypoxic respiratory failure: effect on functional and subjective respiratory parameters compared to conventional oxygen therapy and non-invasive ventilation (NIV). BMC Anesthesiol 14:66
Rittayamai N, Tscheikuna J, Praphruetkit N et al (2015) Use of high-flow nasal cannula for acute dyspnea and hypoxemia in the emergency department. Respir Care 60(10):1377–1382
Lemiale V, Mokart D, Mayaux J et al (2015) The effects of a 2-h trial of high-flow oxygen by nasal cannula versus Venturi mask in immunocompromised patients with hypoxemic acute respiratory failure: a multicenter randomized trial. Crit Care 2(19):380
Fernandez R, Subira C, Frutos-Vivar F et al (2017) High-flow nasal cannula to prevent postextubation respiratory failure in high-risk non-hypercapnic patients: a randomized multicenter trial. Ann Intensive Care 7(1):47
Rittayamai N, Tscheikuna J, Rujiwit P (2014) High-flow nasal cannula versus conventional oxygen therapy after endotracheal extubation: a randomized crossover physiologic study. Respir Care 59(4):485–490
Acknowledgements
Not applicable
Funding
No funding was used in the current research.
Author information
Authors and Affiliations
Contributions
MMAA: choosing the research subject and revising the manuscript. IHEG: choosing the research subject, revising the manuscript, and follow-up the patient data collection. EBA: choosing the research subject, writing the manuscript, and follow up the patient data collection. BBMK: writing the manuscript, follow-up the patient data collection, practical part of the research. The authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Informed written consent was taken from all patients (or their legal guardians) who were invited to participate in the research as regards confidentiality, right to refuse or withdraw, and in case of refusing to participate in the research, the patient will be followed up and will receive his treatment as planned. The study protocol and the written consent were revised and approved by the ethical committee of scientific research, Faculty of Medicine, Ain Shams University (committee’s reference number: MD 204/2015).
Consent for publication
Not applicable
Competing interests
There are no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Abo-Galala, M.M.A., Galal, I.H.E., Abdel-Fattah, E.B. et al. High-flow nasal oxygen therapy versus conventional oxygen therapy and non-invasive mechanical ventilation in patients with acute respiratory failure and post-mechanical ventilation. Egypt J Bronchol 14, 42 (2020). https://doi.org/10.1186/s43168-020-00036-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43168-020-00036-9