Abstract
Introduction
The diagnosis of invasive pulmonary aspergillosis, according to the criteria as defined by the European Organisation for the Research and Treatment of Cancer/Mycoses Study Group (EORTC/MSG), is difficult to establish in critically ill patients. The aim of this study is to address the clinical significance of isolation of Aspergillus spp. from lower respiratory tract samples in critically ill patients on the basis of medical and radiological files using an adapted diagnostic algorithm to discriminate proven and probable invasive pulmonary aspergillosis from Aspergillus colonisation.
Methods
Using a historical cohort (January 1997 to December 2003), all critically ill patients with respiratory tract samples positive for Aspergillus were studied. In comparison to the EORTC/MSG criteria, a different appreciation was given to radiological features and microbiological data, including semiquantitative cultures and direct microscopic examination of broncho-alveolar lavage samples.
Results
Over a 7 year period, 172 patients were identified with a positive culture. Of these, 83 patients were classified as invasive aspergillosis. In 50 of these patients (60%), no high risk predisposing conditions (neutropenia, hematologic cancer and stem cell or bone marrow transplantation) were found. Typical radiological imaging (halo and air-crescent sign) occurred in only 5% of patients. In 26 patients, histological examination either by ante-mortem lung biopsy (n = 10) or necropsy (n = 16) was performed, allowing a rough estimation of the predictive value of the diagnostic algorithm. In all patients with histology, all cases of clinical probable pulmonary aspergillosis were confirmed (n = 17). Conversely, all cases classified as colonisation had negative histology (n = 9).
Conclusion
A respiratory tract sample positive for Aspergillus spp. in the critically ill should always prompt further diagnostic assessment, even in the absence of the typical hematological and immunological host risk factors. In a minority of patients, the value of the clinical diagnostic algorithm was confirmed by histological findings, supporting its predictive value. The proposed diagnostic algorithm needs prospective validation.
Similar content being viewed by others
Introduction
Aspergillus is a saprophytic filamentous fungus widespread in the environment. Although Aspergillus can affect any organ system, the respiratory tract is involved in more than 90% of affected patients. Inhalation of Aspergillus spores or conidia can give rise to various clinical conditions, depending essentially on the host's immunological status [1, 2]. In immunocompetent patients, pulmonary aspergilloma, allergic bronchopulmonary aspergillosis and obstructive bronchial aspergillosis are described. In immunocompromised patients, especially with prolonged neutropenia, Aspergillus fumigatus can invade the pulmonary parenchyma, resulting in invasive pulmonary aspergillosis, a disease with a high lethality. More recently, a locally invasive form called necrotizing pulmonary aspergillosis has been described in patients with mild immunosuppression [1, 3–5]. Recent data indicate that invasive aspergillosis must be considered as an emerging and devastating infectious disease in intensive care unit (ICU) patients even in the absence of an apparent predisposing immunodeficiency. In a carefully designed study in a medical ICU, the incidence of invasive aspergillosis was 5.8% ; the majority of these patients did not have a history of hematological malignancy. [6]. In an autopsy study of ICU patients, 2.7% of patients were found to have invasive aspergillosis. Chronic obstructive pulmonary disease (COPD) and advanced liver cirrhosis were recognised as potential risk factors [7].
The significance of isolation of Aspergillus from respiratory cultures has been studied extensively in immunocompromised hosts who develop invasive pulmonary aspergillosis [8–10]. On the other hand, little is known about the significance of isolation of Aspergillus from respiratory specimens of apparently immunocompetent or mildly immunocompromised patients. Because species of Aspergillus are ubiquitous, one must be cautious in ascribing a pathogenic role to the fungus obtained from a nonsterile site. Therefore, diagnosis of invasive pulmonary aspergillosis on the basis of an Aspergillus positive culture from tracheal aspirates remains most difficult in patients with intermediate risk [5], or in patients without currently recognized risk factors. The golden standard for the definite diagnosis of proven invasive pulmonary aspergillosis remains histopathological lung tissue examination. In clinical practice, the diagnosis of proven invasive pulmonary aspergillosis is rarely established ante-mortem, because of the critical condition of the patients, excluding invasive procedures. Since no non-invasive diagnostic test is sensitive or specific enough to establish definite diagnosis, the diagnostic categories of 'probable' and 'possible invasive pulmonary aspergillosis' have been developed, based on the combination of host risk factors, clinical symptoms and distinct radiological and microbiological criteria [11]. These diagnostic criteria were originally developed for clinical trials in patients with bone marrow transplants and cancer. However, in ICU patients, clinical signs and symptoms are often non-specific, and except for neutropenia and a congenital or acquired immunocompromised state, it is not feasible to define particular host risk factors, or combinations of risk factors, for the acquisition of invasive fungal disease, since there are no large epidemiological studies in this special patient population.
The aim of the present study is to assess the clinical relevance of Aspergillus positive respiratory tract samples in ICU patients, based upon a diagnostic algorithm derived from the European Organisation for the Research and Treatment of Cancer/Mycosis Study Group (EORTC/MSG) criteria for invasive fungal disease [11] with a modified interpretation of medical imaging data and microbiological findings. The validity of the diagnostic criteria was assessed if biopsy or necropsy data were available.
Materials and methods
Setting
The present study was conducted in the Ghent University Hospital, a 1,060 bed primary care and referral centre with a 54 bed ICU including a surgical and medical ICU, an ICU for cardiac surgery and a unit for severely burned patients. Approximately 3,800 patients are admitted to the ICU each year. The surgical ICU serves all kinds of surgery with the need for intensive care management, including multiple trauma and solid organ transplantations. During the study period, 910 patients received a solid organ transplant (kidney, pancreas, liver and heart).
The medical ICU serves all patients with internal diseases requiring intensive care, including patients with haematological malignancies and bone marrow transplant recipients; a total of 270 haematological patients was admitted during the study period. For immunocompromised patients or patients colonized or infected with epidemiologically important microorganisms, each unit is equipped with several isolation rooms. The burns unit consists of six separated isolation rooms with shower and bath installations within.
Study design
The study is designed as a historical cohort study (retrospective analysis of prospectively gathered data), including all patients admitted to the ICUs during the period January 1997 through December 2003. The sole criterion for entry in the study is a lower respiratory tract culture positive for Aspergillus spp. As a routine practice, all intubated patients in the ICU receive surveillance cultures of endotracheal aspirate thrice weekly. Otherwise, respiratory specimens from all patients, including pulmonary biopsy and specimens of normally sterile sites, are obtained according to the instructions of the attending physicians. The local Center for Hospital Hygiene and Infection Control prospectively files all patient records with any positive culture for Aspergillus spp., hence all relevant data could be retrieved.
Patients admitted to the ICU with prior diagnosis of invasive Aspergillus disease were not included in the analysis.
Data collection and processing, and patient anonymisation were done according to legal regulations and local Ethics Committee requirements. Given the non-interventional design, the Ethics Committee of the Ghent University Hospital waived informed consent.
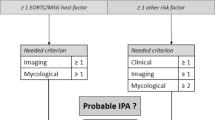
Definitions of definite or probable invasive pulmonary aspergillosis and Aspergilluscolonisation
An adapted clinical algorithm considering clinical status, host factors, microbiological data, bronchoscopy with broncho-alveolar lavage, medical imaging and cytological examination of smears of broncho-alveolar lavage fluid results was used to discriminate colonisation from invasive infection. These criteria for defining cases of invasive pulmonary aspergillosis are summarized in Table 1. For the diagnosis of probable invasive pulmonary aspergillosis, all criteria needed to be fulfilled (1 + 2 + 3 + either 4a or 4b). This algorithm is in part derived from the EORTC/MSG consensus data concerning opportunistic invasive fungal infections in immunocompromised patients with cancer and hematopoetic stem cell transplants [11]. The circulating galactomannan test for Aspergillus antigen was not routinely available in our institution during the study period, and was hence not taken into the diagnostic elaboration. Patients not fullfilling the criteria for invasive pulmonary aspergillosis were classified as colonized. Autopsy was performed at the request of the attending physician after consent of the family.
Data collection
The following data relevant to patient characteristics were collected: age, Acute Physiology and Chronic Health Evaluation (APACHE) II score [12], comorbidities and underlying diseases, and treatment with systemic and inhalation corticosteroids. Data collected concerning ICU treatment and outcome were ICU stay, ventilator dependence, need for vasopressor or inotropic treatment, need for renal replacement therapy, and antifungal therapy. Outcome was described as in-hospital mortality, defined as death within the same hospital episode as the ICU admission.
Classification of radiological findings
Results of chest X-ray and thoracic CT scan were described as normal, acute respiratory distress syndrome (ARDS)-like, non-specific infiltrates and consolidation, pleural fluid, nodular lesion(s), halo sign, air-crescent sign, and cavitation. The CT halo sign is described as a mass-like infiltrate with a surrounding halo of ground glass attenuation. The halo lesion was shown to correspond to a central fungal nodule surrounded by a rim of hemorrhage and coagulative necrosis. The air-crescent sign is described as a pulmonary cavitation [13, 14].
Other definitions
Acute renal failure is defined as the need for renal replacement therapy, acute respiratory failure as the need for acute mechanical ventilation and cardiovascular failure as the need for inotropic or vasopressive support despite adequate fluid resuscitation [15–18].
Statistics
Continuous variables are described as median (interquartile range). Comparative analyses were performed with the Mann-Whitney U or Chi-square test when appropriate. Survival curves were prepared by means of the Kaplan-Meier method and univariate survival distributions were compared with use of the Log rank test. Statistical analyses were performed with SPSS 11.0 (SPSS Inc., Chicago, IL, USA). All used tests are two-tailed and statistical significance is defined as P < 0.05.
Results
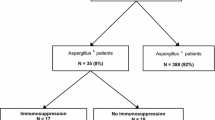
During the observation period, 25,216 patients were admitted to the ICU. Respiratory tract samples were positive for Aspergillus in 172 patients (incidence: 6.8/1,000 ICU admissions). The diagnostic breakdown of the cohort is illustrated in Figure 1. According to the predefined criteria, 83 cases (48.3%) were classified as invasive pulmonary aspergillosis (17 definite, 68 probable). In the remaining 89 patients (51.7%), the presence of Aspergillus was considered as colonisation. Pulmonary biopsy was performed in ten patients. Biopsy was positive in seven patients, who were classified as documented invasive aspergillosis ante-mortem. In three patients, classified clinically as colonisation, lung biopsy showed no fungal disease. Autopsy in patients with an Aspergillus positive respiratory tract specimen was performed in 16 patients. Ten of these patients fullfilled the predefined criteria of probable invasive pulmonary aspergillus ante-mortem; since lung necropsy specimens confirmed the diagnosis, they were subsequently classified as definite invasive pulmonary aspergillosis. In six patients who were considered as colonized ante-mortem, the autopsy did not reveal invasive Aspergillus disease.
In Table 2, underlying conditions of patients with invasive pulmonary aspergillosis and colonisation are summarized. Of the patients diagnosed with invasive pulmonary aspergillosis, 40% of patients had a high risk profile (neutropenia, hematological cancer, bone marrow or stem cell transplant). Patient characteristics and outcome are summarised in Table 3. Thoracic medical imaging (Table 4) shows that nodular lesions were almost exclusively found in invasive pulmonary aspergillosis (30% versus 2%; P < 0.001). The halo and air-crescent sign were evident in only three patients. Most patients classified as invasive pulmonary aspergillosis had non-specific radiological findings.
Appropriate antifungal treatment was given to 71 (85.5%) patients with invasive pulmonary aspergillosis. All patients classified with invasive pulmonary aspergillosis in whom no antifungal therapy was started died (n = 12). When these patients were excluded, the mortality rate was 73%. Figure 2 shows the survival curves of patients categorised as invasive aspergillosis and colonisation.
Discussion
Until recently, research on epidemiology and risk factors for the acquisition of Aspergillus infection and treatment of invasive disease has almost enterily focused on severely immunocompromised patients with hematological malignancy and solid organ recipients. However, recent literature indicates an expanding spectrum of patients at risk for invasive aspergillus disease. These are categorised into high risk (allogeneic bone marrow transplant, neutropenia and hematological cancer), intermediate risk (autologous bone marrow transplant, malnutrition, corticosteroids, HIV, solid organ transplant, diabetes, underlying pulmonary disease and solid organ cancer) and low risk (cystic fibrosis and connective tissue disease) [5]. Furthermore, case reports and papers about invasive pulmonary aspergillosis in COPD patients and apparently non-immunocompromized patients [19–26] have been published.
Hence, it seems worthwile to address the question of diagnosis of invasive pulmonary aspergillosis in ICU patients. The lack of validated and stringent criteria for case definitions in patient categories, other than hemato-oncological and solid organ transplant, hampers diagnostic assessment. The ante-mortem diagnosis of proven invasive aspergillosis is extremely difficult to establish in ICU patients as hemodynamic and/or respiratory insufficiency and coagulopathy often preclude invasive tissue sampling. Because of these diagnostic limitations, a feasible diagnostic approach was developed. As in the EORTC/MSG definitions, host factors for the acquisition of invasive disease were taken into account. For patients who did not meet the criteria for high-risk host, the Aspergillus spp. positive tracheal aspirate had to be corroborated with a positive semi-quantitative culture and a positive cytological examination of broncho-alveolar lavage fluid. This is in part endorsed by the observations of Greub and Bille [27] in a case-definition study in immunocompromised patients: compared to those from patients considered to be colonised, cultures of lower respiratory tract specimens from patients with proven invasive pulmonary aspergillosis showed a significant difference in the total number of Aspergillus colonies recovered from culture per episode; for BAL (broncho-alveolar lavage), the number of Aspergillus colonies per agar plate was also significantly higher in the proven aspergillosis group. Furthermore, many authors consider the visualisation of the characteristic septate hyphae in bronchial washings as a confirmatory finding of invasive disease in the presence of a compatible clinical picture [8, 28–32]. False-positive results appear to be unusual, since patients without chronic lung diseases rarely show colonisation of the lower tracheobronchial tree with Aspergillus [33]. Compared to the EORTC/MSG diagnostic criteria, the interpretation of radiological data in the algorithm is also less strict, as any major radiological sign of pneumonia is taken into consideration. Medical imaging of the thorax in ICU patients is less pathognomonic due to many confounding factors such as ventilator associated pneumonia, atelectasis, and pleural fluid effusions in critically ill ventilated patients; furthermore, it can be speculated that typical radiological lesions may be less apparent because of the difference in severity and nature of the immune derangements. Typical lesions for invasive aspergillosis, such as the halo and the air-crescent sign, were only found in 5% of patients. This is in agreement with the low sensitivity of 24% in patients without hematological malignancy compared with 82% in patients with neutropenic hematological malignancy [34].
Since the modified clinical diagnosis of probable invasive aspergillosis is less stringent than the EORTC/MSG criteria, a lower specificity may be of concern. However, in a limited number of patients, histopathological specimens were available in order to check the validity of the clinical assumption. Samples for histology were available in 26 patients. Of these, 13 fullfilled the EORTC/MSG criteria for host risk factors. Ten patients underwent pulmonary biopsy. Seven of these met the criteria of probable aspergillosis prior to biopsy, and could be reclassified ante-mortem as definite invasive pulmonary aspergillosis because of a positive histopathological examination. In three other patients, classified as colonized, lung biopsy showed no evidence of fungal infection. Furthermore, autopsy data were available in 16 patients, of whom 10 were classified as probable invasive pulmonary aspergillosis ante-mortem, and the other six patients as colonized. Necropsy findings histologically confirmed the clinical diagnosis in all these patients. These data are in support of a high positive predictive value of the criteria for the diagnosis of invasive pulmonary aspergillosis. Nevertheless, the number of patients with histological confirmation was low. The true predictive value of the proposed diagnostic algorithm needs to be assessed prospectively.
In this study, using an entry criterion of an Aspergillus positive respiratory specimen and an adapted diagnostic algorithm, an incidence of invasive pulmonary aspergillosis of 3.2/1,000 ICU admissions was found. In the subgroup of medical patients, the incidence was three times as high (10.2/1,000). In a recent retrospective study in a medical ICU, an incidence of invasive aspergillosis of even 5.8% was found, with, in most cases, pulmonary involvement [6]. In a study considering autopsies of patients from a mixed medical-surgical ICU, an incidence of 2.7% of proven invasive aspergilosis was found [7]. In general, the autopsy rate is low in our institution (<5%) because of local ethical regulations. It can not be excluded that patients classified as colonized indeed had invasive disease, and that other patients with negative surveillance cultures suffered from invasive disease since respiratory tract cultures lack sensitivity. It is clear that a stringent protocol for post-mortem examination is necessary for a truthful estimation of the epidemiology and incidence of invasive aspergillosis in ICU patients [6, 7]. Furthermore, prospective research should include non-culture methods for diagnosis, such as the detection of galactomannan, PCR, and beta-D-glucan in non-neutropenic patients [35, 36]. At this time, it is unclear if these non-invasive methods are of any diagnostic value in critically ill patients without the EORTC/MSG host risk factors.
An important finding is that the majority of the patients classified as having invasive pulmonary aspergillosis did not belong to the well known high-risk group (neutropenia, bone marrow transplant, hematological cancer); this is in accordance with the data provided in the study by Meersseman and colleagues [6]. Underlying conditions, such as COPD, chronic lung disease, non-hematological malignancy, HIV infection, diabetes mellitus, liver failure, chronic alcohol abuse, malnutrition and extensive burns, have been described in association with invasive aspergillosis [5, 7, 37, 38]. In the EORTC/MSG diagnostic criteria, the use of corticosteroids for more than three weeks is considered a predisposing host factor [11]. In the setting of persistent septic shock, steroids are frequently used since a beneficial effect has been demonstrated [39]. Corticosteroids substantially impair macrophage killing of Aspergillus spores and mononuclear cell killing of Aspergillus hyphae [40]. In the setting of underlying lung disease, there is a risk factor for invasive aspergillosis at much lower doses and shorter courses of steroids [41, 42]. This should be taken into account in the clinical assessment of an Aspergillus spp. positive respiratory tract sample. Steroid treatment has also been given important weight in a recently described point-score system for assessment of positive cultures [43]. It has been speculated that patients with normal immune function prior to ICU admission may be at risk for invasive aspergillosis due to a temporary immunoparalysis in the context of the multiple organ dysfunction syndrome [44].
Hospital mortality of patients with invasive pulmonary aspergillosis in this study was high (77%), but in accordance with previous reports describing dramatic fatality rates [22, 24, 45, 46]. When comparing the survival curves of the group of patients with invasive aspergillosis with the group of patients classified as colonised, a clear difference is observed during the first 15 days after positive respiratory Aspergillus culture and fullfillment of the diagnostic criteria for invasive disease. The initial decline of the curve of patients with invasive disease is more pronounced, reflecting an acute mortality probably due to Aspergillus infection. This fits well with the generally accepted time frame of the development of invasive Aspergillus disease until demise. This observation is an indirect argument in favour of the value of the diagnostic algorithm.
Conclusion
The finding of an Aspergillus positive respiratory tract sample in an ICU patient cannot be discarded and must trigger further diagnostic exploration using BAL, with semiquantitative culture and cytological examination, as well as CT scan and pulmonary biopsy if possible. Adapted clinical diagnostic criteria should be used in order not to miss a critical window of therapeutic opportunity.
The proposed diagnostic algorithm for the diagnosis of invasive pulmonary aspergillosis is supported by histopathological data from a subgroup of patients. An important finding is that not only patients with severe hematological disease are afflicted: the majority of patients has an intermediate risk for the acquisition of invasive disease. Radiological features are often non-specific. The associated mortality is high in spite of appropriate treatment.
Key messages
-
The finding of Aspergillus spp. in respiratory tract samples in critically ill patients should not be routinely discarded as colonisation, even in presumably immunocompetent hosts.
-
Clinical signs and symptoms of invasive pulmonary aspergillosis and radiographic features are often non-specific in ICU patients
-
Risk factors for the development of invasive aspergillosis in critically ill patients include neutropenia, haematological malignancy and immunosuppressive treatment. However, invasive disease can occur in the absence of these risk factors.
-
In the presence of clinical features of unresolving pneumonia, appropriate antifungal therapy should be considered carefully when Aspergillus spp. is isolated from respiratory tract specimens, in patients with COPD, after corticosteroid exposure even in moderate dose, and in other patients with severe underlying disease and critical illness induced immunoparalysis.
Abbreviations
- COPD:
-
chronic obstructive pulmonary disease
- EORTC/MSG:
-
European Organisation for the Research and Treatment of Cancer/Mycoses Study Group
- ICU:
-
intensive care unit.
References
Sharma OP, Chwogule R: Many faces of pulmonary aspergillosis. Eur Respir J. 1998, 12: 705-715. 10.1183/09031936.98.12030705.
Barnes AJ, Denning DW: Aspergilli – significance as pathogens. Rev Med Microbiol. 1993, 4: 176-180.
Denning DW: Invasive aspergillosis. Clin Infect Dis. 1998, 26: 781-803.
Saraceno JL, Phelps DT, Ferro TJ, Futerfas R, Schwartz DB: Chronic necrotizing pulmonary aspergillosis: approach to management. Chest. 1997, 112: 541-548.
Perfect JR, Cox GM, Lee JY, Kauffman CA, de Repentigny L, Chapman SW, Morrison VA, Pappas V, Hiemenz JW, Stevens DA: The impact of culture isolation of Aspergillus species: a hospital-based survey of aspergillosis. Clin Infect Dis. 2001, 33: 1824-1833. 10.1086/323900.
Meersseman W, Vandecasteele SJ, Wilmer A, Verbeken E, Peetermans WE, Van Wijngaerden E: Invasive aspergillosis in critically ill patients without malignancy. Am J Respir Crit Care Med. 2004, 170: 621-625. 10.1164/rccm.200401-093OC.
Dimopoulos G, Piagnerelli M, Berre J, Eddafali B, Salmon I, Vincent JL: Disseminated aspergillosis in intensive care unit patients: an autopsy study. J Chemother. 2003, 15: 71-75. 10.1159/000070766.
Levy H, Horak DA, Tegtmeier BR, Yokota SB, Forman SJ: The value of bronchoalveolar lavage and bronchial washings in the diagnosis of invasive pulmonary aspergillosis. Respir Med. 1992, 86: 243-248.
Yu VL, Muder RR, Poorsattar A: Significance of isolation of Aspergillus from the respiratory tract in diagnosis of invasive pulmonary aspergillosis. Results from a three-year prospective study. Am J Med. 1986, 81: 249-254. 10.1016/0002-9343(86)90259-7.
Horvath JA, Dummer S: The use of respiratory-tract cultures in the diagnosis of invasive pulmonary aspergillosis. Am J Med. 1996, 100: 171-178. 10.1016/S0002-9343(97)89455-7.
Ascioglu S, Rex JH, de Pauw B, Bennett JE, Bille J, Crokaert F, Denning DW, Donnelly JP, Edwards JE, Erjavec Z, et al: Defining opportunistic invasive fungal infections in immunocompromised patients with cancer and hematopoietic stem cell transplants: an international consensus. Clin Infect Dis. 2002, 34: 7-14. 10.1086/323335.
Knaus WA, Draper EA, Wagner DP, Zimmerman JE: APACHE II: a severity of disease classification system. Crit Care Med. 1985, 13: 818-829.
Caillot D, Casasnovas O, Bernard A, Couaillier JF, Durand C, Cuisenier B, Solary E, Piard F, Petrella T, Bonnin A, et al: Improved management of invasive pulmonary aspergillosis in neutropenic patients using early thoracic computed tomographic scan and surgery. J Clin Oncol. 1997, 15: 139-147.
Kuhlman JE, Fishman EK, Siegelman SS: Invasive pulmonary aspergillosis in acute leukemia: characteristic findings on CT, the CT halo sign, and the role of CT in early diagnosis. Radiology. 1985, 157: 611-614.
Blot S, Vandewoude K, Colardyn F: Nosocomial bacteremia involving Acinetobacter baumannii in critically ill patients: a matched cohort study. Intensive Care Med. 2003, 29: 471-475.
Blot SI, Vandewoude KH, Colardyn FA: Evaluation of outcome in critically ill patients with nosocomial enterobacter bacteremia: results of a matched cohort study. Chest. 2003, 123: 1208-1213. 10.1378/chest.123.4.1208.
Groeneveld AB, Tran DD, van der Meulen J, Nauta JJ, Thijs LG: Acute renal failure in the medical intensive care unit: predisposing, complicating factors and outcome. Nephron. 1991, 59: 602-610.
Noble JS, MacKirdy FN, Donaldson SI, Howie JC: Renal and respiratory failure in Scottish ICUs. Anaesthesia. 2001, 56: 124-129. 10.1046/j.1365-2044.2001.01841.x.
Fisher JR, Conway MJ, Takeshita RT, Sandoval MR: Necrotizing fasciitis. Importance of roentgenographic studies for soft-tissue gas. JAMA. 1979, 241: 803-806. 10.1001/jama.241.8.803.
Lewis M, Kallenbach J, Ruff P, Zaltzman M, Abramowitz J, Zwi S: Invasive pulmonary aspergillosis complicating influenza A pneumonia in a previously healthy patient. Chest. 1985, 87: 691-693.
Pittet D, Huguenin T, Dharan S, Sztajzel-Boissard J, Ducel G, Thorens JB, Auckenthaler R, Chevrolet JC: Unusual cause of lethal pulmonary aspergillosis in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1996, 154: 541-544.
Bulpa PA, Dive AM, Garrino MG, Delos MA, Gonzalez MR, Evrard PA, Glupczynski Y, Installe EJ: Chronic obstructive pulmonary disease patients with invasive pulmonary aspergillosis: benefits of intensive care?. Intensive Care Med. 2001, 27: 59-67. 10.1007/s001340000768.
Karam GH, Griffin FM: Invasive pulmonary aspergillosis in nonimmunocompromised, nonneutropenic hosts. Rev Infect Dis. 1986, 8: 357-363.
Rello J, Esandi ME, Mariscal D, Gallego M, Domingo C, Valles J: Invasive pulmonary aspergillosis in patients with chronic obstructive pulmonary disease: report of eight cases and review. Clin Infect Dis. 1998, 26: 1473-1475.
Rolando N, Harvey F, Brahm J, Philpott-Howard J, Alexander G, Casewell M, Fagan E, Williams R: Fungal infection: a common, unrecognised complication of acute liver failure. J Hepatol. 1991, 12: 1-9. 10.1016/0168-8278(91)90900-V.
Garnacho-Montero J, Amaya-Villar R, Ortiz-Leyba C, Leon C, Alvarez-Lerma F, Nolla-Salas J, Iruretagoyena JR, Barcenilla F: Isolation of Aspergillus spp. from the respiratory tract in critically ill patients: risk factors, clinical presentation and outcome. Crit Care. 2005, 9: R191-R199. 10.1186/cc3488.
Greub G, Bille J: Aspergillus species isolated from clinical specimens: suggested clinical and microbiological criteria to determine significance. Clin Microbiol Infect. 1998, 4: 710-716.
Aisner J, Murillo J, Schimpff SC, Steere AC: Invasive aspergillosis in acute leukemia: correlation with nose cultures and antibiotic use. Ann Intern Med. 1979, 90: 4-9.
Fisher BD, Armstrong D, Yu B, Gold JW: Invasive aspergillosis. Progress in early diagnosis and treatment. Am J Med. 1981, 71: 571-577. 10.1016/0002-9343(81)90208-4.
Burton JR, Zachery JB, Bessin R, Rathbun HK, Greenough WB, Sterioff S, Wright JR, Slavin RE, Williams GM: Aspergillosis in four renal transplant recipients. Diagnosis and effective treatment with amphotericin B. Ann Intern Med. 1972, 77: 383-388.
Albelda SM, Talbot GH, Gerson SL, Miller WT, Cassileth PA: Role of fiberoptic bronchoscopy in the diagnosis of invasive pulmonary aspergillosis in patients with acute leukemia. Am J Med. 1984, 76: 1027-1034. 10.1016/0002-9343(84)90853-2.
Uffredi ML, Mangiapan G, Cadranel J, Kac G: Significance of Aspergillus fumigatus isolation from respiratory specimens of nongranulocytopenic patients. Eur J Clin Microbiol Infect Dis. 2003, 22: 457-462. 10.1007/s10096-003-0970-y.
Nalesnik MA, Myerowitz RL, Jenkins R, Lenkey J, Herbert D: Significance of Aspergillus species isolated from respiratory secretions in the diagnosis of invasive pulmonary aspergillosis. J Clin Microbiol. 1980, 11: 370-376.
Greene RE, Schlamm HT, Stark P, Oestman JW, Troke P, Patterson TF, Herbrecht R, Wingard J, Bennett JE, Lortholary O, et al: Radiological findings in acute invasive pulmonary aspergillosis: utility and reliability of halo sign and air-crescent sign for diagnosis and treatment of invasive pulmonary aspergillosis in high-risk patients. Clin Microbiol Infect. 2003, 9 (Suppl 1): O397-
Maertens J, Verhaegen J, Lagrou K, Van Eldere J, Boogaerts M: Screening for circulating galactomannan as a noninvasive diagnostic tool for invasive aspergillosis in prolonged neutropenic patients and stem cell transplantation recipients: a prospective validation. Blood. 2001, 97: 1604-1610. 10.1182/blood.V97.6.1604.
Ostrosky-Zeichner L, Alexander BD, Kett DH, Vazquez J, Pappas PG, Saeki F, Ketchum PA, Wingard J, Schiff R, Tamura H, et al: Multicenter clinical evaluation of the (1-->3) beta-D-glucan assay as an aid to diagnosis of fungal infections in humans. Clin Infect Dis. 2005, 41: 654-659. 10.1086/432470.
Rees JR, Pinner RW, Hajjeh RA, Brandt ME, Reingold AL: The epidemiological features of invasive mycotic infections in the San Francisco Bay area, 1992–1993: results of population-based laboratory active surveillance. Clin Infect Dis. 1998, 27: 1138-1147.
Vandewoude K, Blot S, Benoit D, Depuydt P, Vogelaers D, Colardyn F: Invasive aspergillosis in critically ill patients: analysis of risk factors for acquisition and mortality. Acta Clin Belg. 2004, 59: 251-257.
Annane D, Sebille V, Charpentier C, Bollaert PE, Francois B, Korach JM, Capellier G, Cohen Y, Azoulay E, Troche G, et al: Effect of treatment with low doses of hydrocortisone and fludrocortisone on mortality in patients with septic shock. JAMA. 2002, 288: 862-871. 10.1001/jama.288.7.862.
Lionakis MS, Kontoyiannis DP: Glucocorticoids and invasive fungal infections. Lancet. 2003, 362: 1828-1838. 10.1016/S0140-6736(03)14904-5.
Palmer LB, Greenberg HE, Schiff MJ: Corticosteroid treatment as a risk factor for invasive aspergillosis in patients with lung disease. Thorax. 1991, 46: 15-20.
Kontoyiannis DP, Bodey GP: Invasive aspergillosis in 2002: an update. Eur J Clin Microbiol Infect Dis. 2002, 21: 161-172. 10.1007/s10096-002-0699-z.
Bouza E, Guinea J, Pelaez T, Perez-Molina J, Alcala L, Munoz P: Workload due to Aspergillus fumigatus and significance of the organism in the microbiology laboratory of a general hospital. J Clin Microbiol. 2005, 43: 2075-2079. 10.1128/JCM.43.5.2075-2079.2005.
Hartemink KJ, Paul MA, Spijkstra JJ, Girbes AR, Polderman KH: Immunoparalysis as a cause for invasive aspergillosis?. Intensive Care Med. 2003, 29: 2068-2071. 10.1007/s00134-003-1778-z.
Janssen JJ, Strack van Schijndel RJ, van der Poest Clement EH, Ossenkoppele GJ, Thijs LG, Huijgens PC: Outcome of ICU treatment in invasive aspergillosis. Intensive Care Med. 1996, 22: 1315-1322.
Vandewoude KH, Blot SI, Benoit D, Colardyn F, Vogelaers D: Invasive aspergillosis in critically ill patients: attributable mortality and excesses in length of ICU stay and ventilator dependence. J Hosp Infect. 2004, 56: 269-276. 10.1016/j.jhin.2004.01.006.
Acknowledgements
The authors thank Prof. Dr G Verschraegen, MD, and Mr P Dewaegemaeker, MA, from the Hospital Hygiene Team of the Ghent University Hospital, for kindly providing data from the Aspergillus registry. This paper has been partially presented at the 44th Interscience Conference on Antimicrobial Agents and Chemotherapy, Washington, USA, 30 October to 2 November, 2004.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
KV, WT and DV conceived and designed the study. Acquisition of the data was performed by KV and WT. Statistical analysis was performed by SB and PD. Interpretation of the results was done by KV, SB, DV, FC and PD. KV and SB drafted the manuscript, after which it was revised by DV, PD, FC and DB.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Vandewoude, K.H., Blot, S.I., Depuydt, P. et al. Clinical relevance of Aspergillus isolation from respiratory tract samples in critically ill patients. Crit Care 10, R31 (2006). https://doi.org/10.1186/cc4823
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/cc4823