Abstract
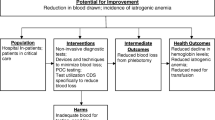
The quality and economy of critical care could both be improved if blood losses due to phlebotomy and sampling from indwelling catheters for unnecessary diagnostic testing were curtailed. Practice guidelines can help to break bad diagnostic 'habits', such as fever work-ups that require substantial blood to be drawn yet typically yield little useful information. Invasive hemodynamic monitoring is associated with morbidity due to blood loss as well as infection, and newer noninvasive technologies should be encouraged. Several devices allow blood that would otherwise be wasted during sampling to be returned to the patient aseptically. Point-of-care testing uses microliter quantities of blood, has acceptable precision, and can provide valuable diagnostic information while being minimally invasive.
Similar content being viewed by others
Introduction
The intensive care unit (ICU) is the epitome of resource-intensive health care settings. Critically ill patients are more numerous and more severely ill than ever before, and the demands upon resources for their care are commensurate. Integral to the care of these patients is appropriate physiologic monitoring, because it is more efficient to prevent morbidity or treat it at an early stage than to undertake a major resuscitation or other intervention for the full manifestations of a serious complication. Monitoring of blood flow, acid-base status, oxygen transport, coagulation, visceral organ function, and the development of nosocomial infection are a few of many aspects of the surveillance of such patients. Collection of blood for testing is an essential part of the monitoring of these patients, but it is increasingly recognized that excessive blood testing occurs, leading (only somewhat facetiously) to an 'anemia of chronic investigation'.
Cost and quality are inextricably linked, and can be defined in an optimal relation. Expenditure of additional resources decreases quality if there is no benefit to the patient. Increased ease of blood sampling occasioned by invasive monitoring catheters does not equate with expanded indications for blood testing. Blood removed from a critically ill patient for testing can average more than 70 ml/day for days or even weeks, depending on the nature and the severity of the illness [1]. The presence of an arterial catheter may increase blood testing by as much as one third [2]. Waste of blood occurs each time a catheter is aspirated and flushed [3], and the risk for nosocomial infection is increased both by catheter manipulation [4] and by transfusion of allogeneic packed red blood cell concentrates [5].
Avoidance of needless blood testing thus has both patient care and economic benefits. Several strategies can be employed to reduce blood testing while preserving optimal patient care, including noninvasive hemodynamic monitoring, adoption of practice parameters for diagnostic evaluation, and point-of-care (POC) testing. Equally important is the need for education to change attitudes toward blood testing. During residency training, a traditional hallmark of efficiency was to 'have all the data'; woe unto the house officer who did not have results available on demand. However, physicians and surgeons are trained to make decisions and intervene effectively based on incomplete data, and should be comfortable obtaining data as dictated by the clinical situation. Several studies [6, 7] demonstrate the lack of utility of routine preoperative blood testing. Studies performed in the surgical ICU at the author's institution demonstrated that blood testing can be reduced by at least 50% without an adverse effect on patient care [8, 9]. To the extent that attitudes and expectations must be adjusted, the adjustment process has been termed 'learning to not know' [8].
Noninvasive hemodynamic monitoring
The morbidity of invasive hemodynamic monitoring is substantial, including infection, vascular injury and other access-related complications, and inappropriate therapy as a result of poor quality control or misinterpretation of the data. Pulmonary artery catheterization is employed less frequently now as compared with as recently as 5 years ago, owing to increasing reliance on echocardiography and esophageal Doppler estimates of aortic blood flow, and to evidence that use of pulmonary artery catheters may be associated with increased mortality [10]. Noninvasive measurement of arterial blood pressure is accurate and the technology is widely available. New antihypertensive agents such as fenoldopam allow control of elevated blood pressure without the use of an indwelling catheter, even in emergencies [11].
Practice parameters for diagnostic evaluation
Practice parameters, sometimes referred to as guidelines, are increasingly recognized as valuable tools in medical practice. Far from being 'cookbook medicine' or 'a roadmap for the malpractice lawyers', these documents can be very informative, especially when they are evidence based rather than relying solely on expert opinion. Available evidence is graded for quality, recommendations are made based on the quality of the evidence, and areas where more data are needed become readily apparent. Practitioners should partner with their institutions to determine how published documents may be used to enhance care in the context of local patterns of practice.
One example relevant to the issue of reduced blood testing in the ICU is the practice parameter for the evaluation of fever in critically ill adults published jointly by the Society of Critical Care Medicine and the Infectious Diseases Society of America, with the endorsement of the Surgical Infection Society [12]. The yield of 'fever work-ups' in general, and blood cultures in particular, is very low in the early postoperative period (< 72 hours), and therefore evaluation is usually not indicated. Most of these episodes of fever are either non-infectious in origin or related to the diagnosed disease process that necessitated surgery in the first place.
Point-of-care testing
Point-of-care testing of blood samples occurs at or near the bedside. Initially slow to be accepted, largely because of regulatory concerns regarding quality control of the data, POC testing is now recognized to be accurate and to confer numerous advantages. Turnaround time is reduced, enhancing clinical care and reducing repetitive tests sent in frustration over the slow return of results from the initial sample sent to the main laboratory. Very small (i.e. microliter) blood samples are required, and in some cases are not even removed from the patient because indwelling sensors or a closed circuit extracorporeal sampling device is employed to permit return of the sample to the patient after analysis.
Perhaps the most prevalent example of POC testing is glucose monitoring [13], whereas the intracorporeal and closed circuit extracorporeal technologies are rare by comparison. Expected error tolerances for bedside glucose monitoring are ± 15%. In a paired study of 247 critically ill patients, 91–100% of bedside results were within the error tolerances compared with several reference laboratory analyzers. There was no impact of abnormal blood gas variables on the glucose results, but abnormal hematocrit values were associated with the variant results. Low hematocrit was associated with an overestimated bedside blood glucose concentration, whereas the converse was also true [13]. Blood gases and electrolyte concentrations can also be analyzed at the bedside with good precision across a range of concentrations for each analyte. In a recent comparison trial [14], precision studies performed at three different concentrations for each analyte demonstrated an intra-assay coefficient of variation of 2.5% or less and an interassay precision of 4% or less in all tests.
The value of POC testing has been demonstrated in the setting of trauma resuscitation. In a prospective study of 200 patients with major trauma [15], physicians were queried using a standardized set of questions as to their diagnostic and therapeutic management plan before and after a battery of POC tests (hemoglobin, electrolytes, glucose, blood gases and pH, base deficit, and lactate) became available. Although electrolytes and blood urea nitrogen never influenced management, each of the other tests had an impact in 6% of cases. As would be expected, POC hemoglobin and blood gas testing were most likely to influence management within the ensuing 30 min after test results became available.
Conclusion
Blood testing in the ICU is often excessive and unnecessary, may increase the risk for infection, and may lead to increased cost. Conservation of blood may be achieved by adhering to evidence-based guidelines, employing POC testing at the bedside, and by reducing needless blood testing, and increasingly is a part of quality patient care in the ICU.
Abbreviations
- ICU:
-
intensive care unit
- POC:
-
point of care.
References
Corwin HL, Parsonnet KC, Gettinger A: RBC transfusion in the ICU. Is there a reason?. Chest. 1995, 108: 767-771.
Low LL, Harrington GR, Stoltzfus DP: The effect of arterial lines on blood-drawing practices and costs in intensive care units. Chest. 1995, 108: 216-219.
Lin JC, Strauss RG, Kulhavy JC, Johnson KJ, Zimmerman MB, Cress GA, Connolly NW, Widness JA: Phlebotomy overdraw in the neonatal intensive care nursery. Pediatrics. 2000, 106: E19-
Adal KA, Farr BM: Central venous catheter-related infections: a review. Nutrition. 1996, 12: 208-213. 10.1016/S0899-9007(96)91126-0.
Ottino G, De Paulis R, Pansini S, Rocca G, Tallone MV, Comoglio C, Costa P, Orzan F, Morea M: Major sternal wound infection after open-heart surgery: a multivariate analysis of risk factors in 2,579 consecutive operative procedures. Ann Thorac Surg. 1987, 44: 173-179.
Kaplan EB, Sheiner LB, Boeckmann AJ, Roizen MF, Beal SL, Cohen SN, Nicoll CD: The usefulness of preoperative laboratory screening. JAMA. 1985, 253: 3576-3581. 10.1001/jama.253.24.3576.
Houry S, Georgeac C, Hay J-M, Fingerhut A, Boudet M-J: A prospective multicenter evaluation of preoperative hemostatic screening tests. Am J Surg. 1995, 170: 19-23. 10.1016/S0002-9610(99)80245-1.
Barie PS, Hydo LJ: Learning to not know: results of a program for ancillary cost reduction in surgical critical care. J Trauma. 1996, 41: 714-720.
Barie PS, Hydo LJ: Lessons learned: durability and progress of a program for ancillary cost reduction in surgical critical care. J Trauma. 1997, 43: 590-594.
Connors AF, Speroff T, Dawson NV, Thomas C, Harrell FE, Wagner D, Desbiens N, Goldman L, Wu AW, Califf RM, Fulkerson WJ, Vidaillet H, Broste S, Bellamy P, Lynn J, Knaus WA: The effectiveness of right heart catheterization in the initial care of critically ill patients. JAMA. 1996, 276: 889-897. 10.1001/jama.276.11.889.
Tumlin JA, Dunbar LM, Oparil S, Buckalew V, Ram CV, Mathur V, Ellis D, McGuire D, Fellmann J, Luther RR: Fenoldopam, a dopamine agonist, for hypertensive emergency: a multicenter randomized trial. Fenoldopam Study Group. Acad Emerg Med. 2000, 7: 653-662.
O'Grady NP, Barie PS, Bartlett J, Bleck T, Garvey G, Jacobi J, Linden P, Maki DG, Nam M, Pasculle W, Pasquale MD, Tribett DL, Masur H: Practice parameters for evaluating new fever in critically ill adult patients. Crit Care Med. 1998, 26: 392-408. 10.1097/00003246-199802000-00046.
Louie RF, Tang Z, Sutton DV, Lee JH, Kost GJ: Point-of-care glucose testing: effects of critical care variables, influence of reference instruments, and a modular glucose meter design. Arch Pathol Lab Med. 2000, 124: 257-266.
Chance JJ, Li DJ, Sokoll LJ, Silberman MA, Engelstad ME, Nichols JH, Liu X, Mohammad AA, Petersen JR, Okorodudu AO: Multiple site analytical evaluation of a portable blood gas/electrolyte analyzer for point of care testing. Crit Care Med. 2000, 28: 2081-2085. 10.1097/00003246-200006000-00069.
Asimos AW, Gibbs MA, Marx JA, Jacobs DG, Erwin RJ, Norton HJ, Thomason M: Value of point-of-care blood testing in emergent trauma management. J Trauma. 2000, 48: 1101-1108.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
PSB is a consultant for Ortho Biotech Products, L.P.
Rights and permissions
About this article
Cite this article
Barie, P.S. Phlebotomy in the intensive care unit: strategies for blood conservation. Crit Care 8 (Suppl 2), S34 (2004). https://doi.org/10.1186/cc2454
Published:
DOI: https://doi.org/10.1186/cc2454