Abstract
Background
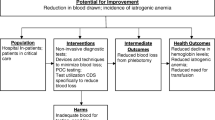
Diagnostic laboratory tests are an integral part of managing hospitalized patients. In particular, patients in the intensive care units (ICUs) can experience a concerning amount of blood loss due to diagnostic testing, which can increase the risk developing iatrogenic anemia. Several interventions exist to curtail avoidable blood loss, for example computerized decision support, smaller phlebotomy tubes, and other blood conservation devices. Nevertheless, use of these interventions is not standardized. Therefore, the objective of our study was to quantify the daily phlebotomy volume taken from patients who had undergone major cardiac or vascular surgery.
Methods
We estimated the number of blood analyses and volumes of drawn blood of 400 consecutive patients (≥ 18 yr) undergoing major cardiac or vascular surgery. The amount of blood saved using small-volume tubes and in combination with blood conservation device rather than standard-volume tubes was estimated for serum chemistry (serum), ethylenediaminetetraacetic acid (EDTA) tubes, sodium citrate coagulation (SCC) tubes, and arterial blood gas (ABG) analysis.
Results
The mean total blood loss due to phlebotomy drawing using standard-volume tubes during hospitalization was 167.9 mL (95% confidence interval [CI], 158.0 to 177.8), 255.6 mL (95% CI, 226.5 to 284.6), and 695.3 mL (95% CI, 544.1 to 846.4) for patients undergoing cardiac surgery with a hospital length of stay (LOS) of 0–10, 11–20, and ≥ 21 days, respectively. The mean total blood loss due to phlebotomy during hospitalization was 80.5 mL (95% CI, 70.5 to 90.6), 225.0 mL (95% CI, 135.1 to 314.8 mL) and 470.3 mL (95% CI, 333.5 to 607.1) for vascular surgery patients with LOS 0–10, 11–20, and ≥ 21 days, respectively. Patients with at least a two-day stay at the ICU had a mean blood loss of 146.6 mL (95% CI, 134.6 to 158.6 mL) and those with ≥ 11 days incurred a loss of 1,428 mL (95% CI, 1,117.8 to 1,739.2). The use of closed blood collection device and small-volume tubes (serum, EDTA, SCC, and ABG) reduced blood loss by 82.8 mL for patients with an ICU stay of 2 days and up to 824.0 mL for patients with a ICU stay of ≥ 11 days.
Conclusion
Diagnostic laboratory tests are associated with significant patient blood loss, but are a modifiable risk factor. The use of small-volume tubes and closed blood collection devices decreases the volume of patient blood drawn for analysis and prevents blood waste.
Résumé
Contexte
Les tests diagnostiques de laboratoire font partie intégrante de la prise en charge des personnes hospitalisées. Plus spécifiquement, la patientèle des unités de soins intensifs (USI) peut perdre une quantité inquiétante de sang en raison des tests de diagnostic, ce qui peut augmenter le risque d’anémie iatrogène. Plusieurs interventions existent pour réduire les pertes de sang évitables, par exemple une aide à la décision informatisée, des tubes de phlébotomie plus petits et d’autres dispositifs de conservation du sang. Néanmoins, le recours à ces interventions n’est pas normalisé. Par conséquent, l’objectif de notre étude était de quantifier le volume quotidien de phlébotomie prélevée chez des patient·es ayant bénéficié d’une chirurgie cardiaque ou vasculaire majeure.
Méthode
Nous avons estimé le nombre d’analyses sanguines et les volumes de sang prélevés de 400 personnes consécutives (≥ 18 ans) bénéficiant d’une chirurgie cardiaque ou vasculaire majeure. La quantité de sang économisée à l’aide de tubes de petit volume et en combinaison avec un dispositif de conservation du sang plutôt que des tubes de volume standard a été estimée pour la chimie sérique (sérum), les tubes d’acide éthylène-diamine-tétra-acétique (EDTA), les tubes de coagulation au citrate de sodium (CCS) et l’analyse des gaz du sang artériel (GSA).
Résultats
La perte sanguine totale moyenne due au prélèvement de phlébotomie à l’aide de tubes de volume standard pendant l’hospitalisation était de 167,9 mL (intervalle de confiance [IC] à 95 %, 158,0 à 177,8), 255,6 mL (IC 95 %, 226,5 à 284,6) et 695,3 mL (IC 95 %, 544,1 à 846,4) chez les patient·es bénéficiant d’une chirurgie cardiaque avec une durée de séjour à l’hôpital de 0 à 10, 11 à 20, et ≥ 21 jours, respectivement. La perte sanguine totale moyenne due à la phlébotomie pendant l’hospitalisation était de 80,5 mL (IC 95 %, 70,5 à 90,6), 225,0 mL (IC 95 %, 135,1 à 314,8 mL) et 470,3 mL (IC 95 %, 333,5 à 607,1) chez les patient·es ayant bénéficié d’une chirurgie vasculaire avec des durées de séjour de 0-10, 11-20 et ≥ 21 jours, respectivement. Les patient·es ayant séjourné au moins deux jours à l’USI ont eu une perte de sang moyenne de 146,6 mL (IC 95 %, 134,6 à 158,6 mL) et celles et ceux ayant séjourné ≥ 11 jours ont subi une perte de 1428 mL (IC 95 %, 1117,8 à 1739,2). L’utilisation d’un dispositif de prélèvement sanguin fermé et de tubes de petit volume (sérum, EDTA, SCC et gsa) a réduit la perte de sang de 82,8 mL pour les patient·es ayant séjourné à l’USI 2 jours et jusqu’à 824,0 mL pour les patient·es ayant séjourné en USI ≥ 11 jours.
Conclusion
Les tests de laboratoire diagnostiques sont associés à une perte de sang importante chez les patient·es, mais constituent un facteur de risque modifiable. L’utilisation de tubes de petit volume et de dispositifs fermés de prélèvement sanguin diminue le volume de sang prélevé pour analyse et prévient le gaspillage de sang.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Laboratory testing is an essential component of perioperative care. Nevertheless, clinicians are often unaware of the frequency of routine laboratory testing and the blood volume involved. Koch et al.1 assessed the number of performed laboratory tests in 1,894 patients undergoing cardiac surgery and found that, on average, 115 tests per patient were performed. Arterial blood gas (ABG) analysis was the most frequently performed (40%) followed by coagulation tests (18%), complete blood counts (14%), metabolic panels (13%), blood culture (5.3%), blood type and screen (3.8%), and potassium level tests (1.8%). On a regular ward, the median [interquartile range (IQR)] cumulative blood volume drawn was 118 mL [73 to 232] and on an intensive care unit (ICU), the median [IQR] blood drawn was 332 mL [197 to 619 mL].1 Excessive blood draws reduce hemoglobin (Hb) levels and may contribute to the development or progression of anemia. Furthermore, phlebotomy in intensive care patients contributes to the need for red blood cell (RBC) transfusions.2 Since the outbreak of the SARS-CoV-2 pandemic, the number of available RBC units has dramatically decreased in many countries, thus the safe handling of patient blood has become even more important. Several blood-saving measures exist, including in-line blood conservation devices, small-volume phlebotomy tubes, point-of-care testing, rational test ordering, and noninvasive methods. While several studies have shown that using small-volume phlebotomy tubes reduces blood loss caused by diagnostic sampling without increasing laboratory error,3,4 minimal volume sampling is not a standard practice in most hospitals. Therefore, in this study, we assessed the number of laboratory tests conducted in patients undergoing major or vascular surgery to estimate the effect of small-volume phlebotomy tubes on blood loss due to diagnostic sampling.
Material and methods
Setting
We collected data of 400 consecutive patients (age ≥ 18 yr) scheduled for major cardiac (n = 200; n = 100 with a cardiopulmonary bypass and n = 100 without a cardiopulmonary bypass) or vascular (n = 200) surgery between January 2019 and February 2020 at the University Hospital Frankfurt, retrospectively. Major surgery was defined as any cases with increased probability of an RBC transfusion.5,6 We manually extracted patient data and the number and types of performed laboratory tests from the hospital’s electronic database. Based on laboratory diagnostics, we identified the number of blood tests and the blood collection tubes used. We then used the data to quantify the amount of blood loss and to calculate the amount of reduced blood volume when using small-volume tubes. It is noteworthy to mention that small-volume tubes are used for the most part at the University Hospital Frankfurt. Standard-volume tubes are used for specific analyses or analyses performed at external laboratories. Briefly, use of small-volume tubes was part of the implementation of a Patient Blood Management program at the University Hospital Frankfurt.5 The exchange of the tubes was repeatedly announced to all employees by the head of the laboratory department through email, newsletters, and internal training. Small-volume sodium citrate coagulation [SCC] tubes were validated before implementation.3 Standard-volume tubes were replaced stepwise for each collection tube (serum, ethylenediaminetetraacetic acid [EDTA], SCC, and ABG) and for every hospital ward in close collaboration with medical staff. Handling and analyses of collected blood using small-volume tubes were closely controlled and analyzed.
The study protocol was approved by the ethics committee of the University Hospital Frankfurt (Ref. 318/17) and the requirement for written informed consent by patients was waived.
Sampling
The number of diagnostic samplings was evaluated for serum chemistry (serum), EDTA, SCC, ABG, blood culture (10.0 mL), thin capillary tubes (0.5 mL), point-of-care testing (POCT) (2.8 mL), and activated clotting time (ACT) (1.0 mL). The volume for standard and small-volume tubes were: 4.7 mL and 2.6 mL for serum, 2.7 mL and 1.8 mL for EDTA, 3.0 mL and 1.8 mL for SCC, and 2.0 mL and 1.0 mL for ABG, respectively. In addition, the placement of central venous catheter (CVCs) and arterial lines was noted.
Total blood loss for patients with ICU stays was calculated for both standard- and small-volume tubes based on the number of serum, EDTA, SCC, ABG, blood culture, thin capillary tubes, and POCT laboratory tests that were conducted. In the presence of a CVC or arterial line, 5 mL of blood was routinely discarded before blood was drawn for laboratory analysis and was included in the estimation of total blood loss. Closed blood conservation devices were used in the ICU only. In these patients, no blood was discarded during blood collection. Anemia was defined according to the World Health Organization criteria7 as Hb < 12.0 g·dL–1 for women and Hb < 13.0 g·dL–1 for men.
Statistical analysis
To investigate the volume of blood drawn for laboratory diagnostics, we estimated the number of blood tests taken and the number of collection tubes used. Based on laboratory profiles, the used collection tube was identified as 1) EDTA: small blood count including blood cells and Hb; 2) serum: creatinine, liver function, kidney function, and electrolyte; and 3) SCC: coagulation. Blood analyses performed with tubes for ABG were identified in the laboratory profiles. Next, the drawn blood volume was calculated using standard- and small-volume tubes for serum, EDTA, SCC, and ABG. Then, the total volume of blood drawn during a hospital stay was calculated for three conditions: 1) standard-volume tubes (serum [4.7 mL], EDTA [2.7 mL], SCC [3.0 mL], ABG [2.0 mL], blood culture [10.0 mL], thin capillary tubes [0.5 mL], POCT [2.8 mL], and amount of discarded blood [5.0 mL]); 2) small-volume tubes (serum [2.6 mL], EDTA [1.8 mL], SCC [1.8 mL], ABG [1.0 mL], blood culture [10 mL], thin capillary tubes [0.5 mL], POCT [2.8 mL], and amount of discarded blood [5.0 mL]); and 3) small-volume tubes and closed blood conservation devices (serum [2.6 mL], EDTA [1.8 mL], SCC [1.8 mL], ABG [1.0 mL], blood culture [10 mL], thin capillary tubes [0.5 mL], POCT [2.8 mL]).
We analyzed descriptive variables using means and standard deviations (SDs). Statistical significance was set at P < 0.05 and was determined using the Mann–Whitney U test, Student’s t test, or Fisher’s exact test. We used Spearman’s rank correlation rho to assess correlations between length of stay (LOS) and the number of laboratory tests performed. To assess the standardized mean difference, we calculated the absolute difference between saved blood volumes using small-volume tubes compared with standard-volume tubes. The number of performed laboratory tests with serum, EDTA, SCC, and ABG was used to calculate the saved blood volume. We performed a univariate linear regression model on the hospital stay and the volume of drawn blood volume for laboratory diagnostics. Prediction bands have been analyzed to take the variability of the data around the fitted curve into account. All analyses were conducted using R version 3.1 (R Foundation for Statistical Computing, Vienna, Austria) and Microsoft® Excel (Microsoft Corporation, Redmond, WA, USA).
Results
In total, 200 patients undergoing cardiac surgery and 200 patients undergoing vascular surgery were included in the analysis (Electronic Supplementary Material [ESM] eTable 1). Table 1 lists the patient characteristics including age, sex, Hb level at admission, and presence or absence of anemia. The mean (SD) total hospital LOS was 14.7 (10.7) days for patients undergoing cardiac surgery and 16.3 (16.9) days for patients undergoing vascular surgery. For cardiac surgery patients, the mean (SD) Hb level at discharge was 10.3 (1.6) g·dL–1, and 93.5% of patients had anemia. For vascular surgery patients, the Hb level at discharge was 10.4 (2.0) g·dL–1 and 86.5% were anemic (Table 2). In total, 85 (42.5%) cardiac surgery patients had a LOS of 0–10 days, 80 (40%) had a LOS of 10–20 days, and 35 (17.5%) had a LOS of > 21 days. Of the vascular surgery patients, 116 (58%) had a LOS of 0–10 days, 31 (15.5%) had a LOS of 10–20 days, and 53 (25.6%) had a LOS of > 21 days. Electronic Supplementary Material eTables 2 and 3 show Hb levels and hospital LOS for patients undergoing peripheral major vascular surgery, aortic surgery, vascular surgery, and cardiac surgery with or without cardiopulmonary bypass.
Blood volumes and the frequency of laboratory testing
The most commonly performed laboratory tests in patients undergoing cardiac surgery were ABG (n = 12,678; 56%) followed by SCC (n = 3,606; 16%), serum (n = 3,151; 14%), and EDTA (n = 3,106; 14%). For patients undergoing vascular surgery, the most common tests were ABG (n = 7,177; 48%) followed by EDTA (n = 2,725; 18%), serum (n = 2,635; 17%), and SCC (n = 2,444; 16%) (ESM eTable 4). In cardiac surgery patients, hospital LOS and the number of laboratory tests using serum, EDTA, and SCC were strongly correlated (ESM eTable 5). Similarly, in patients undergoing vascular surgery, LOS and the number of laboratory tests using serum and EDTA were strongly correlated (ESM eTable 5). Increasing hospital LOS during the postoperative period was associated with increased overall phlebotomy volumes (Fig. 1). For patients undergoing cardiac surgery, the mean total blood loss due to phlebotomy was 167.9 mL (95% confidence interval [CI], 158.0 to 177.8), 255.6 mL (95% CI, 226.5 to 284.6) and 695.3 mL (95% CI, 544.1 to 846.4) with a hospital LOS of 0–10, 11–20, and > 21 days, respectively. The mean total blood loss due to phlebotomy was 80.5 mL (95% CI, 70.5 to 90.6), 225.0 mL (95% CI, 135.1 to 314.8) and 470.3 mL (95% CI, 333.5 to 607.1) for vascular surgery patients with a hospital LOS of 0–10, 11–20, and > 21 days, respectively (Fig. 2, ESM eFig. 1). The linear regression analysis revealed that LOS was a significant predictor for drawn blood volume using serum, EDTA, SCC, and ABG blood collection tubes. The analysis also showed that most of the analyzed data reside within the margins of the predictive bands (ESM eFig. 2).
Number and volume of blood analysis per collection tube. The bubble plot shows for each collection tube the number and drawn blood volume per day. Bubble size represents the number of performed blood analyses.
ABG = arterial blood gas; EDTA = ethylenediaminetetraacetic acid; LOS = length of hospital stay; SCC = sodium citrate coagulation
Amount of potential blood saving using small-volume tubes
The absolute difference between saved blood volumes using small-volume tubes compared with standard-volume tubes increased with a longer hospital LOS (ESM eTables 6 and 7).
The mean amount of blood drawn can be significantly reduced using small-volume tubes compared with standard-volume tubes both in cardiac and vascular surgery patients (ESM eTables 6 and 7): 50% reduction using ABG, 45% reduction using serum, 33.4% reduction using EDTA, and 40% reduction using SCC.
Total blood loss during the intensive care unit stay
The total blood loss was highest for patients during their ICU stay and increased the longer they spent in the ICU. Patients with a two-day stay in the ICU had a mean blood loss of 146.6 mL (95% CI, 134.6 to 158.6) and with ≥ 11 days, this increased to a mean blood loss of 1,428 mL (95% CI, 1,117.8 to 1,739.2) (Table 3). By using small-volume tubes, the amount of blood loss could have been reduced by 51.3 mL for patients with an ICU stay of two days and up to 465.3 mL for patients with an ICU stay of ≥ 11 days. The combined use of small-volume tubes and closed blood conservation devices was associated with a blood loss reduction of 82.8 mL for patients with an ICU stay of two days and 824.0 mL for patients with an ICU stay of ≥ 11 days (Fig. 3 and ESM eTable 8).
Discussion
Iatrogenic blood loss is a key factor contributing to the development and worsening of hospital-acquired anemia (HAA). The etiology of anemia is multifactorial and includes iron deficiency, intestinal disorders, chronic conditions, pregnancy, menstruation, occult or procedural bleeding, hemodilution from intravenous fluid administration, blunted erythropoietin production, and laboratory diagnostics.8,9,10 Nevertheless, blood loss due to laboratory diagnostics is also associated with the development of HAA.11 There is evidence suggesting that HAA is associated with an increased risk for in-hospital mortality and prolonged hospital LOS.11,12,13 Koch et al. showed that, of 188,447 hospitalized patients, 74% developed HAA. Of these, 29% developed mild anemia, 41% experienced moderate anemia, and 30% had severe HAA. They further found that mortality risk significantly increased with the severity of HAA (OR, 1.51 for moderate HAA and OR, 3.28 for severe HAA).14 Blood transfusions are often used to reverse anemia and up to 53% of ICU patients receive a blood transfusion during their stay.15
Several strategies exist to reduce blood draws for diagnostic laboratory testing.16,17,18,19,20,21,22 For example, Riessen et al. showed that a combination of blood-saving bundles including closed-loop arterial blood sampling systems, smaller sampling tubes, fewer blood draws, and a reduction in sample numbers were associated with a significant reduction in mean blood loss (from 43.3 mL to 15.0 mL). Moreover, the authors found that transfused RBC units decreased from 7.0 to 2.3 units per 100 observation days, with the closed-loop arterial blood sampling system being the largest contributor to this effect.23
Major surgery is often associated with both intensive care and a prolonged hospital stay, particularly for patients undergoing invasive cardiac or vascular surgery who are prone to postoperative complications. Laboratory diagnostics during postoperative care are inevitable. Nevertheless, extensive bloodletting may drive HAA and impede surgical recovery. In our analysis, the mean (SD) hospital LOS was 14.7 (10.7) days and 16.3 (16.9) days for patients undergoing major cardiac and vascular surgery, respectively. Overall, 17.5% of the patients undergoing cardiac surgery and 25.6% of the patients undergoing vascular surgery had a hospital LOS > 21 days. Our analysis revealed that a prolonged LOS was associated with an increase in overall phlebotomy volume. In patients with a LOS of > 21 days, blood volume for serum, EDTA, SCC, and ABG was up to 695.3 mL (95% CI, 544.1 to 846.4) for patients undergoing cardiac surgery and 470.3 mL (95% CI, 333.5 to 607.1) for patients undergoing vascular surgery during their overall hospital stay. Remarkably, patients with a two-day stay in the ICU experienced a median blood loss of 146.6 mL (95% CI, 134.6 to 158.6) and with ≥ 11 days a median blood loss of 1,428.0 mL (95% CI, 1,117.8 to 1,739.2). By using small-volume tubes for serum, EDTA, SCC, and ABG as well as using closed blood collection tubes, the amount of blood loss could be reduced by 82.8 mL for patients with an ICU stay of two days and up to 824.0 mL for those with an ICU stay of ≥ 11 days.
Laboratory diagnostics can be divided into two categories: routine or screening and indicated or diagnostic. Recent findings suggest that, with the introduction of protocols for enhanced recovery after surgery, perioperative care pathways have improved. These improvements have led some to question whether the number of daily, routine blood draws can be reduced. Nevertheless, changing these routines is challenging as clinicians worry that, in case of complications or adverse events, the lack of testing will be challenged. In addition, while indwelling CVC or arterial lines simplify blood sampling, they contribute to iatrogenic anemia because the first few millilitres from each new blood draw are discarded. Mukhopadhyay et al. found that the use of a blood conservation device was associated with a significant reduction in Hb levels and transfusion requirements in ICU patients.24 Patients with reduced erythropoiesis capacity cannot sufficiently compensate for surgical blood loss or laboratory diagnostics. Therefore, attempts to ameliorate unnecessary blood loss should focus on modifiable procedures. Small-volume or pediatric tubes are helpful as they can be used to preserve patient blood.4 Moreover, Briggs et al. showed that small-volume tubes reduced sampling volume by 50% with no increase in laboratory error.25 In this study, we calculated the amount of saved blood volume using small-volume sampling tubes in patients undergoing major cardiac or vascular surgery. Our results indicate that using small-volume tubes could reduce the amount of blood drawn by 50% for ABG, by 45% for serum, by 33.4% for EDTA, and by 40% for SCC. Patients with intensive care needs would benefit the most, with blood reductions of 82.8 mL (for a two-day ICU stay) and up to 824.0 mL for ICU stays ≥ 11 days.
Laboratory diagnostics are essential components of medical diagnoses and therapies. Nevertheless, a significant proportion of blood tests are reflexive, and repetitive phlebotomy is associated with hematoma formation, nerve damage, pain extravasation, iatrogenic anemia, arterial punctures, petechiae, allergies, fear and phobias, infection, syncope and fainting, excessive bleeding, edema, and thrombus.2 Furthermore, repetitive phlebotomy may increase the risk for HAA,11,26 increase the need for RBC transfusion,2 and prolong hospital LOS.26 Insufficient knowledge of laboratory costs, fear of litigation, diagnostic uncertainty, absence of feedback on testing practices, and differing levels of health care professional training are common contributors to the problem and are difficult to address. Nevertheless, preserving patient blood reserves is becoming increasingly important and has been addressed by Choosing Wisely Canada recommendations,27 the American Association of Blood Banks,28 and the Society for the Advancement of Blood Management. While coordinated, multidisciplinary, and multimodal quality improvement initiatives have been recommended, they can be difficult to implement and sustain.20,29,30,31 Changing a long-standing work practice is challenging and often associated with resistance. Therefore, close cooperation with laboratories is required, who could then support the replacing collection tubes. Fewer blood specimens may also require more precise handling of samples. Nevertheless, companies provide small-volume tubes similar to standard ones, which do not require changing machines or centrifuge rotors, making the use of smaller-volume tubes a straightforward adjustment. Still, laboratories often require confirmation from their providers that the exchange of sampling tubes would not compromise the blood analyses. In addition, laboratories often request internal validation to show reliable results. Smaller volume tubes may also require adjustments to the hematology analyzer. For example, adapting the depth of needle immersion needs and storage places for tubes.
Limitations
This study had several limitations. First, a power analysis to estimate the smallest sample size needed for the study was not conducted. We cannot exclude that analyzing a higher number of patients may have revealed different amounts of saved blood volumes when using small-volume tubes. As our results showed that using small-volume tubes was feasible, future studies should prospectively assess the effect of these tubes during routine clinical practice. Second, confounding factors such as infection, bleeding, and bleeding disorders that may increase hospital LOS and would require additional laboratory blood analyses were not investigated. Nevertheless, HAA is associated with poor clinical outcomes and iatrogenic blood loss is one of the key contributing factors.32,33 Wu et al. found that implementing the use of small-volume tubes was associated with a reduction in the mean (SD) number of blood transfusions—from 60.0 (46.73) to 58.5 (44.77).34 Based on our study design, we were not able to assess the impact of small-volume blood tubes on blood transfusion. Fourth, the exact amount of discarded volume may vary between medical staff. The literature suggests that withdrawn and discarded blood volume should be between 3 and 5.3 mL.35,36,37,38 At our hospital, medical staff are requested to discard 5 mL of blood before a laboratory analysis is performed. Nevertheless, depending on which lumen of the CVC is used, the volume of discarded blood may be lower. Therefore, the estimated blood loss in our study may have been overestimated.
Conclusion
There is scant clinical awareness of the extent that excessive blood loss from laboratory diagnostic testing contributes to anemia and blood transfusions. Ideally, patient-individualized bloodletting for laboratory diagnostics is preferable, but difficult to implement. Small-volume tubes and closed blood conservation devices represent a valuable alternative to reducing blood loss due to laboratory diagnostics. This study shows that using small-volume tubes and closed blood conservation devices in daily clinical practice can reduce avoidable blood loss and potentially reduce the rate of HAA.
References
Koch CG, Reineks EZ, Tang AS, et al. Contemporary bloodletting in cardiac surgical care. Ann Thorac Surg 2015; 99: 779–84. https://doi.org/10.1016/j.athoracsur.2014.09.062
Chant C, Wilson G, Friedrich JO. Anemia, transfusion, and phlebotomy practices in critically ill patients with prolonged ICU length of stay: a cohort study. Crit Care 2006; 10: R140. https://doi.org/10.1186/cc5054
Adam EH, Zacharowski K, Hintereder G, Zierfuß F, Raimann F, Meybohm P. Validation of a new small-volume sodium citrate collection tube for coagulation testing in critically ill patients with coagulopathy. Clin Lab 2018; 64: 1083–9. https://doi.org/10.7754/clin.lab.2018.171008
Helmer P, Hottenrott S, Steinisch A, et al. Avoidable blood loss in critical care and patient blood management: scoping review of diagnostic blood loss. J Clin Med 2022; 11: 320. https://doi.org/10.3390/jcm11020320
Meybohm P, Herrmann E, Steinbicker AU, et al. Patient blood management is associated with a substantial reduction of red blood cell utilization and safe for patient's outcome: a prospective, multicenter cohort study with a noninferiority design. Ann Surg 2016; 264: 203–11. https://doi.org/10.1097/sla.0000000000001747
Triphaus C, Judd L, Glaser P, et al. Effectiveness of preoperative iron supplementation in major surgical patients with iron deficiency: a prospective observational study. Ann Surg 2021; 274: e212–9. https://doi.org/10.1097/sla.0000000000003643
World Health Organization. Nutritional anaemias: report of a WHO scientific group [meeting held in Geneva from 13 to 17 March 1967]; 1968. Available from URL: https://apps.who.int/iris/handle/10665/40707 (accessed July 2023).
Shander A, Corwin HL. A narrative review on hospital-acquired anemia: keeping blood where it belongs. Transfus Med Rev 2020; 34: 195–9. https://doi.org/10.1016/j.tmrv.2020.03.003
Shander A. Anemia in the critically ill. Crit Care Clin 2004; 20: 159–78. https://doi.org/10.1016/j.ccc.2004.01.002
Napolitano LM. Scope of the problem: epidemiology of anemia and use of blood transfusions in critical care. Crit Care 2004; 8: S1–8. https://doi.org/10.1186/cc2832
Salisbury AC, Reid KJ, Alexander KP, et al. Diagnostic blood loss from phlebotomy and hospital-acquired anemia during acute myocardial infarction. Arch Intern Med 2011; 171: 1646–53. https://doi.org/10.1001/archinternmed.2011.361
Makam AN, Nguyen OK, Clark C, Halm EA. Incidence, predictors, and outcomes of hospital-acquired anemia. J Hosp Med 2017; 12: 317–22. https://doi.org/10.12788/jhm.2712
Koch CG, Li L, Sun Z, et al. From bad to worse: anemia on admission and hospital-acquired anemia. J Patient Saf 2017; 13: 211–6. https://doi.org/10.1097/pts.0000000000000142
Koch CG, Li L, Sun Z, et al. Hospital-acquired anemia: prevalence, outcomes, and healthcare implications. J Hosp Med 2013; 8: 506–12. https://doi.org/10.1002/jhm.2061
Vincent JL, Piagnerelli M. Transfusion in the intensive care unit. Crit Care Med 2006; 34: S96–101. https://doi.org/10.1097/01.ccm.0000214314.57109.cd
Holland J, Peralta RM, Moss RL, Feane K, Uprichard J. A single-centre review of iatrogenic anaemia in adult intensive care. Transfus Med 2020; 30: 196–200. https://doi.org/10.1111/tme.12674
Sanchez-Giron F, Alvarez-Mora F. Reduction of blood loss from laboratory testing in hospitalized adult patients using small-volume (pediatric) tubes. Arch Pathol Lab Med 2008; 132: 1916–9. https://doi.org/10.5858/132.12.1916
Barreda Garcia J, Xian JZ, Pedroza C, et al. Pediatric size phlebotomy tubes and transfusions in adult critically ill patients: a pilot randomized controlled trial. Pilot Feasibility Stud 2020; 6: 112. https://doi.org/10.1186/s40814-020-00657-3
Dolman HS, Evans K, Zimmerman LH, et al. Impact of minimizing diagnostic blood loss in the critically ill. Surgery 2015; 158: 1083–7. https://doi.org/10.1016/j.surg.2015.05.018
Eaton KP, Levy K, Soong C, et al. Evidence-based guidelines to eliminate repetitive laboratory testing. JAMA Intern Med 2017; 177: 1833–9. https://doi.org/10.1001/jamainternmed.2017.5152
Jakacka N, Snarski E, Mekuria S. Prevention of iatrogenic anemia in critical and neonatal care. Adv Clin Exp Med 2016; 25: 191–7. https://doi.org/10.17219/acem/32065
Lyon AW, Chin AC, Slotsve GA, Lyon ME. Simulation of repetitive diagnostic blood loss and onset of iatrogenic anemia in critical care patients with a mathematical model. Comput Biol Med 2013; 43: 84–90. https://doi.org/10.1016/j.compbiomed.2012.11.008
Riessen R, Behmenburg M, Blumenstock G, et al. A simple "blood-saving bundle" reduces diagnostic blood loss and the transfusion rate in mechanically ventilated patients. PloS One 2015; 10: e0138879. https://doi.org/10.1371/journal.pone.0138879
Mukhopadhyay A, Yip HS, Prabhuswamy D, et al. The use of a blood conservation device to reduce red blood cell transfusion requirements: a before and after study. Crit Care 2010; 14: R7. https://doi.org/10.1186/cc8859
Briggs EN, Hawkins DJ, Hodges AM, Monk AM. Small volume vacuum phlebotomy tubes: a controlled before-and-after study of a patient blood management initiative in an Australian adult intensive care unit. Crit Care Resusc 2019; 21: 251–7.
Thavendiranathan P, Bagai A, Ebidia A, Detsky AS, Choudhry NK. Do blood tests cause anemia in hospitalized patients? The effect of diagnostic phlebotomy on hemoglobin and hematocrit levels. J Gen Intern Med 2005; 20: 520–4. https://doi.org/10.1111/j.1525-1497.2005.0094.x
Choosing Wisely Canada. Internal medicine: eleven tests and treatments to question; 2022. Available from URL: https://choosingwiselycanada.org/recommendation/internal-medicine/ (accessed July 2023).
Choosing Wisely. Five things physicians and patients should question; 2022. Available from URL: https://downloads.aap.org/AAP/PDF/Choosing%20Wisely/CWEmergencyMedicine.pdf (accessed July 2023).
Merkeley HL, Hemmett J, Cessford TA, et al. Multipronged strategy to reduce routine-priority blood testing in intensive care unit patients. J Crit Care 2016; 31: 212–6. https://doi.org/10.1016/j.jcrc.2015.09.013
Baird G. The laboratory test utilization management toolbox. Biochem Med (Zagreb) 2014; 24: 223–34. https://doi.org/10.11613/bm.2014.025
Cadamuro J, Ibarz M, Cornes M, et al. Managing inappropriate utilization of laboratory resources. Diagnosis (Berl) 2019; 6: 5–13. https://doi.org/10.1515/dx-2018-0029
Smoller BR, Kruskall MS. Phlebotomy for diagnostic laboratory tests in adults. Pattern of use and effect on transfusion requirements. N Engl J Med 1986; 314: 1233–5. https://doi.org/10.1056/nejm198605083141906
Mann SA, Williams LA 3rd, Marques MB, Pham HP. Hospital-acquired anemia due to diagnostic and therapy-related blood loss in inpatients with myasthenia gravis receiving therapeutic plasma exchange. J Clin Apher 2018; 33: 14–20. https://doi.org/10.1002/jca.21554
Wu Y, Spaulding AC, Borkar S, et al. Reducing blood loss by changing to small volume tubes for laboratory testing. Mayo Clin Proc Inn Qual Outcomes 2021; 5: 72–83. https://doi.org/10.1016/j.mayocpiqo.2020.08.007
Low LL, Harrington GR, Stoltzfus DP. The effect of arterial lines on blood-drawing practices and costs in intensive care units. Chest 1995; 108: 216–9. https://doi.org/10.1378/chest.108.1.216
Lew JK, Hutchinson R, Lin ES. Intra-arterial blood sampling for clotting studies. Effects of heparin contamination. Anaesthesia 1991; 46: 719–21. https://doi.org/10.1111/j.1365-2044.1991.tb09763.x
Woda RP, Dzwonczyk R, Buyama C, Bernacki BL, Kellly WB. On the dynamic performance of the Abbott Safeset blood-conserving arterial line system. J Clin Monit Comput 1999; 15: 215–21. https://doi.org/10.1023/a:1009936917049
Konopad E, Grace M, Johnston R, Noseworthy T, Shustack A. Comparison of PT and aPTT values drawn by venipuncture and arterial line using three discard volumes. Am J Crit Care 1992; 1: 94–101.
Author contributions
Suma Choorapoikayil, Vanessa Neef, Chantal Himmele, and Patrick Meybohm contributed to conception and study design. Suma Choorapoikayil, Vanessa Neef, Chantal Himmele, Patrick Meybohm, Florian Piekarski, Lea Valeska Blum, Lotta Hof, Tomas Holubec, and Wojciech Derwich contributed to writing the manuscript. Chantal Himmele contributed to data acquisition. Suma Choorapoikayil, Chantal Himmele, Vanessa Neef, and Patrick Meybohm contributed to data analysis and interpretation.
Acknowledgements
We would like to thank Dr. Gudrun Hintereder and Frank Zierfuss for supporting the implementation of small volume tubes at the University Hospital Frankfurt and for providing information. We would also like to thank Matthieu Poyer and Dr Oliver Old for statistical support and critical reading. Finally we would also like to thank Tobias Weitbrecht for critical discussion about the implementation of small-volume tubes.
Disclosures
Patrick Meybohm and/or the Department received research grants from the German Research Foundation (ME 3559/1-1, ME 3559/3-1), BMBF (01KG1815), BMG (ZMVI1-2520DAT10E); honoraria for scientific lectures from Abbott GmbH &Co KG, Aesculap Academy, B. Braun Melsungen, Biotest AG, Vifor Pharma, Ferring, CSL Behring, German Red Cross/ Institute of Transfusion Medicine, HCCM Consulting GmbH, Heinen&Löwenstein, Hemosonics, Pharmacosmos, and Siemens Healthcare. Florian Piekarski received honoraria from Pharmacosmos for scientific lectures. The remaining authors have nothing to declare concerning this study.
Funding statement
Not applicable.
Data availability
The data set supporting the conclusion of this article is available upon request.
Editorial responsibility
This submission was handled by Dr. Stephan K. W. Schwarz, Editor-in-Chief, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Patrick Meybohm and Suma Choorapoikayil share last authorship.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Neef, V., Himmele, C., Piekarski, F. et al. Effect of using smaller blood volume tubes and closed blood collection devices on total blood loss in patients undergoing major cardiac and vascular surgery. Can J Anesth/J Can Anesth 71, 213–223 (2024). https://doi.org/10.1007/s12630-023-02643-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-023-02643-8